·Clinical Research··Current Issue· ·Achieve· ·Search Articles· ·Online Submission· ·About IJO·
Indications
for and techniques of keratoplasty at Vietnam National Institute of
Ophthalmology
Pham
Ngoc Dong1, Truong Nhu Han1, Anthony J. Aldave2,
Hoang Thi Minh Chau1
1Vietnam
National Institute of Ophthalmology, Hanoi, Vietnam
2Stein
Eye Institute, the University of California, Los Angeles, CA 90095-7003, USA
Correspondence to: Pham Ngoc Dong. Vietnam National
Institute of Ophthalmology, Hanoi, Vietnam. dong69nam@yahoo.com
Received: 2015-05-01
Accepted: 2015-07-13
Abstract
AIM: To report the
indications for and techniques of corneal transplantation at Vietnam National
Institute of Ophthalmology (VNIO) over a period of 12y (2002-2013).
METHODS:
Records of patients who had undergone corneal transplantation at VNIO from
January 1, 2002 to January 1, 2014 were reviewed to determine the indication
for and type of corneal transplant performed. Patient age, gender, indication
for corneal transplantation and surgical technique were recorded and analyzed.
RESULTS:
Corneal transplantation were underwent in 1390 eyes of 1278
patients with a mean age of 44.9±18.1y during the period under review. The most
common indication was infectious corneal ulcer (n=670; 48.2%), followed by corneal scar (n=333, 24.0%),
corneal dystrophy (n=138, 9.9%) and
failed graft (n=112, 8.1%). Nearly
all procedures performed were penetrating keratoplasty (n=1300, 93.5%), with a few lamellar keratoplasty procedures
performed: lamellar keratoplasty (n=52,
3.7%), Descemet’s
stripping automated endothelial keratoplasty (n=27, 1.9%)
and deep anterior lamellar keratoplasty (n=11,
0.8%).
CONCLUSION: While the most common indication for keratoplasty
was infectious keratitis, nearly all
indications for corneal transplantation were managed with penetrating
keratoplasty. However, lamellar keratoplasty techniques, including deep
anterior lamellar keratoplasty and Descemet’s stripping automated
endothelial keratoplasty, are being performed with increasing frequency for
isolated stromal and endothelial disorders, respectively.
KEYWORDS:
penetrating keratoplasty; lamellar keratoplasty; endothelial keratoplasty;
indication for keratoplasty; technique of keratoplasty
DOI:10.18240/ijo.2016.03.09
Citation: Dong PN, Han TN, Aldave AJ, Chau HTM. Indications
for and techniques of keratoplasty at Vietnam National Institute of
Ophthalmology. Int J Ophthalmol 2016;9(3):379-383
INTRODUCTION
Keratoplasty is one of
the most successful forms of tissue transplantation performed worldwide. Since
the first keratoplasty was performed in 1905[1], keratoplasty has gained great progress both in
terms of quality and quantity. Currently, there are about 50 000 keratoplasty
performed in the United States each year[2].
Due to changes in disease profiles and advances in surgical techniques and
instrumentation, there have been many changes in the indications for and types
of corneal transplantation. In developed countries, the leading indications for
keratoplasty have been Fuchs endothelial dystrophy and pseudophakic corneal edema.
Therefore, endothelial keratoplasty (EK) has become the most commonly performed
type of corneal transplantation in the United States[2]. At the same time, the leading indications for
keratoplasty in developing countries have remained infectious keratitis and
corneal scarring, and thus penetrating keratoplasty (PK) remains the most
commonly performed technique of corneal transplantation[3-4].
In Vietnam, the first
keratoplasty was performed in 1950[5].
However, it was rarely performed during the war. Since the year 2000, using
both domestically and internationally recovered corneal tissue, keratoplasty
has been performed more regularly and has now became a routinely performed
ophthalmic surgery. While the number of cases is increasing and the indications
are expanding, keratoplasty is still only performed at major ophthalmology
institutions, such as the Vietnam National Institute of Ophthalmology (VNIO) in
Hanoi, where the majority of keratoplasty procedures in Vietnam are performed.
To date, there have been no published studies in the peer-reviewed literature
regarding keratoplasty in Vietnam. Therefore, to determine the indications for
and types of keratoplasty performed in Vietnam, we reviewed all keratoplasty
procedures performed at VNIO during the previous 12y.
SUBJECTs
and Methods
The medical records of
all patients who underwent keratoplasty at VNIO during the period from January
1, 2002 to January 1, 2014 were retrospectively reviewed. Data collection was
performed in a manner compliant with the Health Insurance Portability and
Accountability Act, and the described research adhered to the tenets of the
Declaration of Helsinki. The following data was collected for each keratoplaty
procedure: age, sex, indication for surgery, and type of keratoplasty procedure
performed. Keratoplasty procedures were classified as penetrating and lamellar,
which was subcategorized into anterior lamellar keratoplasty (ALK), deep
anterior lamellar keratoplasty (DALK) and Descemet’s stripping automated
endothelial keratoplasty (DSAEK). Indication for keratoplasty was defined as
the corneal pathology at time of keratoplasty as diagnosed clinically by the
surgeon. These indications were divided into 9 diagnostic categories:
infectious keratitis, corneal scar,
corneal dystrophy, regraft, aphakic/pseudophakic bullous keratopathy (ABK/PBK),
keratoconus, acute chemical or thermal injury, corneal degeneration and other
(trauma, Stevens Johnson syndrome and uncertain diagnosis).
Infectious keratitis was further classified according to the pathogenic species
(bacteria, fungus, Acanthamoeba, herpes simplex and unknown). Corneal scars
included scars secondary to infectious keratitis, prior chemical or thermal
injury, trauma and congenital opacity. Regraft was defined as a case in which a
failed prior corneal transplant was the indication.
The study period was
divided into two six year periods (January 1, 2002 to December 31, 2007 and
January 1, 2008 to January 1, 2014) for descriptive and analytical purposes. A
Chi-square (χ2)
contingency table testing of the frequency of types of keratoplasty in the two
time periods was performed. A P value
of <0.05 was considered statistically significant.
Results
Indications for Corneal
Transplantation During
the period from January 1, 2002 to January 1, 2014, 1390 corneal transplants
were performed for 1278 patients at VNIO. The mean age (±standard deviation) of
the recipients was 44.9±18.1y (range from 1 to 89y), with males accounting for
59.5% of the patients. A significant increase in the number of corneal
transplants performed was noted over the twelve-year period, with the
number of transplants almost doubling from 2002-2007 (n=486)
to 2008-2013
(n=904). During the
twelve-year period, the most common indication for
corneal transplantation was infectious keratitis (48.2%) (Table 1). Corneal
perforation and failure to respond to medical therapy were the most common reasons
why corneal transplantation was required in the management of infectious keratitis. The most common
etiology of infectious keratitis was fungal keratitis, which accounted for 56.9% (381/670) of cases (Table 2).
Table 1 Indications for corneal transplantation at Vietnam
National Instititute of Ophthalmology between 2002 and 2013 n (%)
|
Indications |
2002-2007 |
2008-2013 |
Total |
|
Infectious keratitis |
273 (56.2) |
397 (43.9) |
670 (48.2) |
|
Corneal scar |
78 (16.0) |
255 (28.2) |
333 (24.0) |
|
Corneal dystrophy |
42 (8.6) |
96 (10.6) |
138 (9.9) |
|
Regraft |
44 (9.1) |
68 (7.5) |
112 (8.1) |
|
ABK/PBK |
20 (4.1) |
52 (5.8) |
72 (5.2) |
|
Keratoconus |
12 (2.5) |
15 (1.7) |
27 (1.9) |
|
Acute eye burn |
3 (0.6) |
4 (0.4) |
7 (0.5) |
|
Corneal degeneration |
3 (0.6) |
5 (0.6) |
8 (0.6) |
|
Others |
11 (2.3) |
12 (1.3) |
23 (1.7) |
|
Total |
486 (100.0) |
904 (100.0) |
1390 (100.0) |
ABK/PBK: Aphakic/pseudophakic
bullous keratopathy.
Table 2 Etiology of keratitis and corneal scar in
recipients of corneal transplants at Vietnam National Instititute of
Ophthalmology between 2002 and 2013
n (%)
|
Etiology |
2002-2007 |
2008-2013 |
Total |
|
Infectious keratitis |
273 (100.0) |
397 (100.0) |
670 (100.0) |
|
Fungal keratitis |
145 (53.1) |
236 (59.4) |
381 (56.9) |
|
Bacterial keratitis |
91 (33.3) |
128 (32.2) |
214 (31.9) |
|
Viral keratitis |
23 (8.4) |
26 (6.5) |
48 (7.2) |
|
Acanthalmoebic keratitis |
6 (2.2) |
5 (1.3) |
11 (1.7) |
|
Others |
8 (2.9) |
2 (0.5) |
15 (2.3) |
|
Corneal scar |
115 (100.0) |
218 (100.0) |
333 (100.0) |
|
Infectious keratitis |
94 (81.7) |
179 (82.1) |
273 (82.0) |
|
Eye burn |
18 (15.7) |
29 (13.3) |
47 (14.1) |
|
Congenital pathology |
3 (2.6) |
10 (4.6) |
13 (3.9) |
During the period 2002-2007, 56.2% of corneal
transplants were performed for infectious keratitis, signifcantly greater than
the 43.9% performed in the years 2008-2013 (χ2=22.58;
P<0.0001). While the percentage of
corneal transplants performed each year for infetious keratitis increased
between 2002 and 2009, the percentage has decreased since, with 2013 being the
first year in which infectious keratitis was not the most common indication for
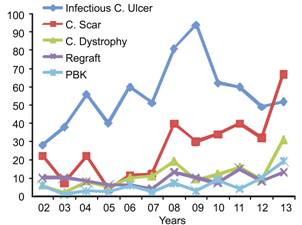
corneal transplantation (Figure 1).
Figure
1 The 5 most common indications for corneal transplant.
While the percentage of keratoplasty procedures peformed for other indications also differed between
the first and second time periods, corneal scarring, corneal dystrophy and
failed keratoplasty were the three most common indications, after infectious
keratitis, in both time periods (Table 1). The most common cause of corneal scarring necessitating
keratoplasty was resolved
infectious keratitis. Therefore, infectious keratitis necessitating either
early (n=670) or delayed (n=273) keratoplasty accounted for 67.8% of all keratoplasty
procedures performed at VNIO during the twelve-year
period under review (Table
2).
Technique of Corneal Transplantation Between 2002 and 2013, PK was the primary form of
keratoplasty performed at VNIO, accounting for 1300 of the 1390 (93.5%)
keratoplasties performed (Table 3). While ALK represents only a small
percentage of the keratoplasty procedures performed in both the first and
second periods, the percentage of ALK procedures more than tripled from 1.4% in
the first period to 5.0% in the second period. Similarly, endothelial
keratoplasty represents an infrequent but increasingly commonly performed
procedure at VNIO since the first DSAEK procedure was performed in October 2010
(Table 3).
Table
3 Types of keratoplaty procedures performed at Vietnam National Instititute of Ophthalmology
between 2002 and 2013 n (%)
|
Surgical
technique |
2002-2007 |
2008-2013 |
Total |
|
PK |
479 (98.6) |
821 (90.8) |
1300 (93.5) |
|
LK |
|
|
|
|
ALK |
7 (1.4) |
45 (5.0) |
52 (3.7) |
|
DALK |
0 |
11 (1.2) |
11 (0.8) |
|
DSAEK |
0 |
27 (3.0) |
27 (2.0) |
|
Total |
486 (100.0) |
904 (100.0) |
1390 (100.0) |
PK: Penetrating
keratoplasty; LK:
Lamellar keratoplasty; ALK: Anterior lamellar keratoplasty; DALK: Deep anterior
lamellar keratoplasty; DSAEK: Descemet’s stripping automated endothelial
keratoplasty.
Discussion
To the best of our knowledge, this study is the first to report the
indications for and types of keratoplasty performed in Vietnam. Similar to
reports of indications for keratoplasty from other developing countries,
infectious keratitis is the most common indication for keratoplasty in Vietnam.
In Shandong,
China during the period of 2005-2010, the leading indications for
corneal transplantation were infectious keratitis (37.1%), herpes simplex
keratitis (19.1%) and keratoconus (11.2%)[3]. Similarly, corneal scarring
following infectious keratitis is the most common indication for keratoplasty
in Southern India[6],
while keratitis, either active or healed, is the major indication for
keratoplasty in Nepal and Malaysia (Table 4)[4,7]. Corneal scarring is the second most common
indication for keratoplasty in Vietnam, accounting for approximately
one-quarter of the keratoplasty procedures performed. Similarly, other Asian
countries have reported a significant percentage of corneal transplants being
performed for corneal scarring, including China (55.9%)[8],
India (38.03%)[9] and Taiwan,
China
(27.9%)[10]. As has been reported in other Southeast Asian
countries such as Malaysia, the main causes of corneal scarring in Vietnam are
infectious keratitis and trauma[7]. We report that
approximately two-thirds of all keratoplasties performed in Vietnam are for
active or resolved infectious keratitis, indicative of the fact that infection
remains the leading cause of corneal pathology in Vietnam. As a consequence,
efforts to reduce the incidence of avoidable blindness and need for corneal
transplantation should focus on the prevention of corneal trauma and secondary
infectious keratitis.
Table 4 Indications for keratoplasty in published series across Asia
%
|
Indications |
Wang
et al[3] |
Bajracharya et
al[4] |
Dasar et al[6] |
Chaidaroon et
al[11] |
Present study |
|
China 2005-2010 |
Nepal 2005-2010 |
India 2002-2012 |
Thailand 1996-1999 |
Vietnam 2002-2013 |
|
|
Infectious keratitis |
56.2 |
40.9 |
2.94 |
17.8 |
48.2 |
|
Corneal scar |
4.8 |
26.8 |
60.7 |
22.2 |
24.0 |
|
Corneal dystrophy |
3.4 |
1.7 |
4.9 |
20.0 |
9.9 |
|
Regraft |
6.7 |
11.2 |
12.7 |
8.9 |
8.1 |
|
ABK/PBK |
8.5 |
9.0 |
8.8 |
28.9 |
5.2 |
|
Keratoconus |
11.2 |
7.0 |
- |
- |
1.9 |
ABK/PBK: Aphakic/pseudophakic
bullous keratopathy.
While infectious keratitis remains the most
common indication for corneal transplantation in Vietnam and other developing
countries in Asia, it is no longer a common indication in many developed
countries. Approximately fifty
years ago in Israel, infectious keratitis was the most common indication for
keratoplasty, accounting for 37.0% of procedures. As time passed, infectious
keratitis become a less common indication, accounting for only 6.3% of
procedures, while keratoconus and graft failure became more common indications
for keratoplasty in Israel[12]. In the majority of developed
countries, the main indications for keratoplasty are non-infectious disorders
such as keratoconus and bullous keratopathy[13-16]. In
Canada, from 1986-1995, the most frequent
indication for keratoplasty was bullous keratopathy (28.5%) and regraft (22.4%)
while keratitis (3.7%) and corneal scar (2.8%) are relatively uncommon
indications[17]. In Germany, among 1200 corneal transplants performed between 2001 and
2010, keratoconus was the main indication (25.5%), followed by corneal
dystrophy (23.3%) and corneal scarring (14.4%). In addition, the authors
reported a statistically significant increase in the number of corneal
transplants performed for keratoconus and Fuchs endothelial dystrophy and a
statistically significant decrease in the number performed for corneal scarring[18].
The percentage of corneal transplants
performed for prior failed graft at VNIO, 8.1%, is similar to that reported in
other Southeast Asian countries such as Thailand (8.9%)[11] and Nepal (11.2%)[4]. As the number of corneal
transplants performed annually in Vietnam continues to increase, the number of
procedures performed for graft failure will continue to increase as well, as
has been observed in developed countries. In fact, graft failure was the most
common indication for penetrating keratoplasty in the UK from 1990-1999, accounting for
40.9% of all cases in one published series[19]. While pseudophakic and aphakic bullous keratopathy
have been reported to be relatively common indications for keratoplasty in
other Southeast Asian countries, such as Thailand (28.9% of all penetrating
keratoplasties)[11] and
Singapore (26.3% of all penetrating keratoplasties)[20], they remain a relatively
uncommon indication in Vietnam, accounting for 5.2% of all cases. However, as
the number of cataract surgeries performed each year in Vietnam continues to
increase significantly, the incidence of post-cataract surgery corneal edema is
likely to increase as well.
Penetrating keratoplasty accounts for over 90% of the keratoplasties
performed at VNIO from 2002-2013, although an increasing number of selective
lamellar keratoplasty procedures have been performed over the last several
years. From 2008-2013, approximately 10% of all keratoplasties performed were anterior or
posterior lamellar procedures, as compared to just over 1% during the preceding
six years. Corneal surgeons around the world have recognized the myriad
advantages of lamellar keratoplasty, including more rapid visual recovery and
lower risk of rejection, leading to increased popularity of anterior and
posterior lamellar keratoplasty
worldwide[21-24]. In Iran, among 1859 corneal
transplantations performed from 2004 to 2009, the proportion of PKP, DALK, LKP,
and DSAEK was 70.9%, 20.1%, 4.4%, 2.3% respectively[25]. In
the West of Scotland, the percentage of lamellar keratoplasty procedures performed increased
from 14.1% between 2001 and 2005 to 40.4% between 2006 and 2010[14]. Similarly, in the United States, 24 987 endothelial keratoplasty procedures were
performed in 2013, accounting for a majority of the 48 229 keratoplasty procedures that were performed[2].
Reasons for significantly different
percentage of penetrating versus lamellar keratoplasty procedures performed in
Vietnam as compared to developed countries include differing indications for
keratoplasty, lack of microkeratome availability and lack of domestically
recovered, eye bank prepared, pre-cut tissue for DSAEK in Vietnam[24,26].
In summary, infectious
keratitis is the most common indication for keratoplasty, and penetrating
keratoplasty is the most common form of corneal
transplantation in Vietnam. However, non-infectious indications are becoming
more common as the number of corneal transplants and cataract surgeries
performed annually in Vietnam continue to increase. In recent years, a small
but increasing number of anterior and posterior lamellar keratoplasty
procedures is being performed, which we anticipate will improve the outcomes of
corneal transplantation in Vietnam.
ACKNOWLEDGEMENTS [Top]
This
work was accomplished with great supports of Dr. Rose Vo, Cornea and Refractive
Surgery, The Jules Stein Eye Institute,
100 Stein Plaza, UCLA, Los
Angeles, CA 90095-7003, USA; Dr. Alvin Young, Prince of
Wales Hospital, Department
of Ophthalmology & Visual Sciences, The Chinese University of Hong Kong, China.
Conflicts of Interest: Dong PN, None; Han
TN, None; Aldave AJ, None; Chau HTM, None.
REFERENCES
1 Zirm EK.
Eine erfolgreiche totale keratoplastik (A successful total keratoplasty).1906.
<ii>Refract Corneal Surg</ii> 1989;5(4): 258-261. [PubMed]
2 Eye bank Association of America. 2013 Eye banking statistical Report.
Washington, DC, 2014.
3 Wang JY, Xie LX, Song XS, Zhao J. Trends in the indications for penetrating
keratoplasty in Shandong, 2005-2010. <ii>Int J Ophthalmol</ii>
2011;4(5):492-497. [PMC free article]
[PubMed]
4 Bajracharya L, Gurung R, Demarchis EH, Oliva M, Ruit S, Tabin G.
Indications for keratoplasty in Nepal: 2005-2010. <ii>Nepal J
Ophthalmol</ii> 2013;5(2):207-214. [CrossRef]
5 Nguyen Dinh Cat, Nguyen Ngoc Kinh, Nguyen Duy Hoa. 46 cases of corneal
transplantation on Vietnamsese patients. <ii>Far East French Medical
Review </ii> 1952;5:33-36.
6 Dasar L, Pujar C, Gill KS, Patil M, Salagar M. Indications of
penetrating keratoplasty in southern India. <ii>J Clin Diagn
Res</ii> 2013;7(11):2505-2507. [CrossRef]
7 Reddy SC, Tajunisah I. Indications for penetrating keratoplasty in
west Malaysia. <ii>Int J Ophthalmol</ii> 2008;1(2):125-128.
8 Zhang C, Xu J. Indications for penetrating keratoplasty in East China,
1994-2003. <ii>Graefes Arch Clin Exp Ophthalmol</ii>
2005;243(10):1005-1009. [CrossRef]
[PubMed]
9 Sony P, Sharma N, Sen S, Vajpayee RB. Indications of penetrating
keratoplasty in northern India. <ii>Cornea</ii> 2005;24(8):989-991.
[CrossRef]
10 Chen WL, Hu FR, Wang IJ. Changing indications for penetrating
keratoplasty in Taiwan from 1987 to 1999. <ii>Cornea</ii>
2001;20(2):141-144. [CrossRef]
11 Chaidaroon W, Ausayakhun S, Ngamtiphakorn S, Prasitsilp J. Clinical
indications for penetrating keratoplasty in Maharaj Nakorn Chiang Mai Hospital,
1996-1999. <ii>J Med Assoc Thai</ii> 2003;86(3):206-211. [PubMed]
12 Frucht-Pery J, Shtibel H, Solomon A, Siganos CS, Yassur Y, Pe’er J.
Thirty years of penetrating keratoplasty in Israel. <ii>Cornea</ii>
1997;16(1):16-20. [CrossRef]
13 Galvis V, Tello A, Gomez AJ, Rangel CM, Prada4 AM, Camacho PA.
Corneal Transplantation at an ophthalmological referral center in Colombia:
indications and techniques (2004-2011). <ii>Open Ophthalmol J</ii>
2013;7:30-33. [CrossRef]
[PubMed] [PMC free article]
14 Ting DS, Sau CY, Srinivasan S, Ramaesh K, Mantry S, Roberts F.
Changing trends in keratoplasty in the West of Scotland: a 10-year review.
<ii>Br J Ophthalmol</ii> 2012;96(3):405-408. [CrossRef] [PubMed]
15 Ghosheh FR, Cremona F, Ayres BD, Hammersmith KM, Cohen EJ, Raber IM,
Laibson PR, Rapuano CJ. Indications for penetrating keratoplasty and associated
procedures, 2001-2005. <ii>Eye Contact Lens</ii>
2008;34(4):211-214. [CrossRef]
[PubMed]
16 Kanavi MR, Javadi MA, Sanagoo M. Indications for penetrating
keratoplasty in Iran. <ii>Cornea</ii> 2007;26(5):561-563. [PubMed]
17 Liu E, Slomovic AR. Indications for penetrating keratoplasty in
Canada, 1986-1995. <ii>Cornea</ii> 1997;16(4):414-419. [CrossRef]
18 Wang J, Hasenfus A, Schirra F, Bohle RM, Seitz B, Szentmary N.
Changing indications for penetrating keratoplasty in Homburg/Saar from 2001 to
2010-histopathology of 1200 corneal buttons. <ii>Graefes Arch Clin Exp
Ophthalmol</ii> 2013;251(3):797-802. [CrossRef] [PubMed]
19 Al-Yousuf N, Mavrikakis I, Mavrikakis E, Daya SM. Penetrating
keratoplasty: indications over a 10 year period. <ii>Br J
Ophthalmol</ii> 2004;88(8):998-1001. [CrossRef] [PubMed] [PMC free article]
20 Chan CM, Wong TY, Yeong SM, Lim TH, Tan DT. Penetrating keratoplasty
in the Singapore National Eye Centre and donor cornea acquisition in the
Singapore Eye Bank. <ii>Ann Acad Med Singapore</ii>
1997;26(4):395-400. [PubMed]
21 Ple-Plakon PA, Shtein RM. Trends in corneal transplantation:
indications and techniques. <ii>Curr Opin Ophthalmol</ii>
2014;25(4):300-305. [CrossRef]
[PubMed]
22 Tan JC, Holland SP, Dubord PJ, Moloney G, McCarthy M, Yeung SN.
Evolving indications for and trends in keratoplasty in British Columbia,
Canada, from 2002 to 2011: a 10-year review. <ii>Cornea</ii>
2014;33(3):252-256. [CrossRef]
23 Zare M, Javadi MA, Einollahi B, Baradaran-Rafii A, Zarei Ghanavati S,
Farsani MR, Mohammadi P, Feizi S. Indications for corneal transplantation at a
tertiary referral center in tehran. <ii>J Ophthalmic Vis Res</ii>
2010;5(2):82-86. [PMC
free article] [PubMed]
24 Keenan TD, Jones MN, Rushton S, Carley FM, National Health Service
Blood and Transplant Ocular Tissue Advisory Group and Contributing
Ophthalmologists (Ocular Tissue Advisory Group Audit Study 8). Trends in the
indications for corneal graft surgery in the United Kingdom: 1999 through 2009.
<ii>Arch Ophthalmol</ii> 2012;130(5):621-628. [CrossRef] [PubMed]
25 Zare M, Javadi MA, Einollahi B, Karimian F, Rafie AR, Feizi S, Azimzadeh
A. Changing indications and surgical techniques for corneal transplantation
between 2004 and 2009 at a tertiary referral center. <ii>Middle East Afr
J Ophthalmol</ii> 2012;19(3):323-329. [CrossRef] [PubMed] [PMC free article]
26 Zhang AQ, Rubenstein D, Price AJ, Cote E, Levitt M, Sharpen L,
Slomovic A. Evolving surgical techniques of and indications for corneal
transplantation in Ontario: 2000-2012. <ii>Can J Ophthalmol</ii>
2013;48(3):153-159. [CrossRef]
[PubMed]
[Top]