·Meta-Analysis··Current Issue· ·Achieve· ·Search Articles· ·Online Submission· ·About IJO·
Femtosecond laser capsulotomy versus manual capsulotomy:
a Meta-analysis
Dao-Wei Qian1,2,3, Hai-Ke Guo2,
Shang-Li Jin1,2, Hong-Yang Zhang2, Yuan-Cun Li1,2
1Southern
Medical University, Guangzhou 510515, Guangdong Province, China
2Department
of Ophthalmology, Guangdong General Hospital/Guangdong Academy of Medical
Sciences, Guangzhou 510080, Guangdong Province, China
3Department
of Ophthalmology, Pingshan New District People’s Hopital of Shenzhen, Shenzhen
518118, Guangdong Province, China
Correspondence to: Hai-Ke Guo. Department of Ophthalmology, Guangdong General
Hospital/Guangdong Academy of Medical Sciences, Guangzhou 510080, Guangdong Province, China. guohaike@medmail.com.cn
Received: 2015-01-14
Accepted: 2015-06-11
Abstract
AIM: To perform
a Meta-analysis on the precision and safety of femtosecond laser
(FSL) capsulotomy compared with manual continuous
curvilinear capsulotomy (CCC).
METHODS: We searched PubMed, EMBASE, Web of Science, the Cochrane Library databases, and Clinical Trials.gov that maintained our inclusion criteria.
Reference lists of retrieved articles were also reviewed. The effects of
morphology of capsulorhexis and the tears of anterior capsule were calculated
by using random-effect models.
RESULTS: We identified 4 randomized and 7 nonrandomized studies involving 2941 eyes. The
diameter of capsulotomy and the rates of anterior capsule tear showed no
statistically difference between FSL group and manual group (MD=0.03; 95%CI, -0.03 to 0.09, P=0.31), and (OR=1.40; 95%CI, 0.28 to
6.97, P=0.68) respectively. In terms of the circularity of capsulotomy, FSL
group had a more significant advantage than the manual CCC group (MD=0.09; 95%CI, 0.05 to
0.12, P<0.0001).
CONCLUSION: Our Meta-analysis shows
that FSL can perform a capsulotomy with more precision and higher reliability
than manual CCC. The results in diameter of capsulotomy and the rate of anterior
capsule tears was no significant difference between FSL and manual CCC groups.
However in terms of circularity, the FSL was superior to the manual procedure.
KEYWORDS: femtosecond laser; cataract surgery;
capsulotomy/capsulorhexis; phacoemulsification; Meta-analysis
DOI:10.18240/ijo.2016.03.23
Citation: Qian DW, Guo HK, Jin SL, Zhang HY, Li YC. Femtosecond laser capsulotomy versus
manual capsulotomy: a Meta-analysis. Int
J Ophthalmol 2016;9(3):453-458
INTRODUCTION
Cataract
surgery is one of the most successfully and commonly performed ophthalmic procedure worldwide[1]. As a critical step in the cataract procedure, the capsulorhexis
is making a window in anterior capsule wall, techniques employed for this task have
undergone sustained evolution[2]. Continuous curvilinear
capsulotomy (CCC) has been recongnized as the standard method of anterior
capsulectomy. The size, shape, and centration of capsulotomy is key determinants of the
positioning and refractive outcomes, too small or too large capsulotomies
caused intraocular lens (IOL) decentration or
tilting, fibrosis and hyperopic shift, posterior capsular opacification[3-6], even more profound in
patients undergoing surgery with toric, multifocal or accommodating IOLs.
Unfortunately, the CCC is still a manual procedure, the size, shape, and
centration of the capsulorhexis can be variable depending on the type of
cataract, even in the experience surgeons, these have implications for the
final refractive outcome, while also increasing the risk of aberrations such as
astigmatism, halo and coma.
Femtosecond lasers (FSL) use a shorter pulse time of 10-15s,
thus further decrease energy output for a given effect without collateral
damage[7]. FSL first
became available for refractive surgery in 2001, the flaps created by FSL
were more reproducible, uniform, closer to their intended thickness and
centration, had improved safety profiles compared with those made by manual
keratome[8]. FSL cataract
surgery witnessed increasing emerging evidence of reduced phacoemulsification
time, better wound architecture, greater precision and accuracy of the anterior
capsulotomy, as well as more stable and predictable positioning of the
intraocular lens[4,9-12].
In this study, we focus on capsulotomy, to review FSL capsulotomy versus
manual CCC in cataract surgery, and assessed the precision and safety of the
two techniques in a Meta-analysis approach.
MATERIALS AND METHODS
Search Strategy We searched PubMed, EMBASE, Web of Science, the
Cochrane Library databases for articles published between January 1, 2009 to
September 30, 2014, and Clinical Trials. gov. The database keywords were:
capsulorhexis/capsulotomy, CCC, FSL, laser capsulotomy , phacoemusification ,
cataract surgery. We manually searched the references of all potentially
relevant articles to identify studies not found by the electronic searches. We
did not contact authors of the primary studies for additional information. The
search strategy did not include language and FSL platforms restriction.
Searches were performed independently by 2 reviewers (Qian DW
and Jin SL).
Inclusion and Exclusion Criteria Two reviewers
(Qian DW and Jin SL) independently initially scanned the titles and abstracts
to identify those that fulfilled the inclusion criteria: randomized
controlled trials (RCTs) and non-RCTs that compared FSL capsulotomy versus
manual CCC: morphology (diameter and circular) of capsulotomy. The rate of
intraoperative
anterior capsule tears. Patients older than 18y with insertion of a
posterior chamber IOL in routine cataract surgery were enrolled in the study.
Exclusion criteria: case reports, case series and studies that do not report
primary data such as editorials and non-systematic reviews.
Data Collection Two reviewers (Qian DW
and Jin SL) independently performed the data extraction
that met the inclusion criteria. We removed duplicate records and obviously
irrelevant titles and abstracts at this stage. We obtained full-text copies of
any report referring to definitely or possibly relevant trials. Results were
compared and any discrepancies between the reviewers’ results were resolved by
discussion (Qian DW and Jin SL), and if disagreements between the 2 reviewers
arose, a third reviewer (Guo HK) was consulted. A customized form was used to record 1)
the author of each study; 2) year of publication; 3) the country in which the study was conducted; 4) the number of eyes;
5) diameter of capsulotomy; 6) circularity of capsulotomy; 7) tears of anterior
capsule.
Quality Assessment of the Retrieved Articles Studies were assessed for quality by means of the
Downs and Black checklist[13]. It has
been found to be valid and reliable for critically evaluating experimental and
nonexperimental studies[14-15]. The criteria of the study’s power was
omitted because few studies reported. Scoring on the modified version could
range between 0 and 27, with a higher score indicating higher methodological
quality. The quality of each study was considered excellent (21-23), good (15-20),
fair (10-14), and poor (≤9)[16]. Scoring was performed independently by two
researchers (Qian DW and Jin SL), and disagreements were resolved
through discussion with a third researcher (Guo HK).
Statistical Analysis The data of both FSL
capsulotomy and manual CCC on diameter, circularity and the rate of capsule
tears were aggregated , the means and standard deviations of diameter and
circularity were used to calculate the estimated mean difference (MD) between
groups, the pooled odds ratio (OR) and 95%CI were performed. Continuity
correction of 0.5 in studies with zero frequencies.
The Chi-square and I2 tests were used to assess the heterogeneity
of the studies[17]. A random effects model was chosen because
the trials with patients from the clinical centers have varying risk profiles
and selection criteria. The 11 studies in our Meta-analysis differed in design and FSL
platform, which was a potential source of heterogeneity between studies.
Potential publication bias was evaluated using the funnel graph. Asymmetry in such plots simplifies the existence of bias, which is
usually publication bias due to nonpublication of small studies with
negative results. Overall we considered the trials at risk of performance and
detection bias because it was difficult to mask patients and outcome assessors,
it was also difficult to assess the role of reporting bias. All analyses were
performed using STATA version 12.0 (StataCorp, College Station, Texas,
USA). A P value<0.05 was considered significant. Figures drafted using R
software (Version 3.1.2) [18].
RESULTS
Search Result and Study Characteristics The electronic searches yielded a total of 453
records. After adjusting for duplicates, 346 different studies were identified,
315 were excluded on the basis of their abstracts for not meeting the primary
inclusion criteria as described earlier. We obtained full-text copies of 31
records for further investigation. After assessing the full-text of the 31
potentially relevant articles. We identified 12 eligible
studies for analysis[4,11,12,19-27]:
two reporting on the same subjects[19,23], the report with higher
quality and the most recent publication was selected[19]. Of them, two studies were conducted in the
United States, five in Europe, three in Australia, and one in Mexico. These
studies comprised four RCTs[12,20,22,26], seven prospective nonrandomized comparative studies[4,11,19,21,24-25,27]. It involved altogether 2941 eyes, of
which 1527 (51.92%) underwent FSL capsulotomy and 1414
(48.08%) manual CCC. Five studies reported the diameter, six reported the
circularity of the capsulotomy, and six reported the rate of anterior capsule tears (complication),five did not mention any of them. The characteristics of the included studies are presented in Table
1.
Table 1 Characteristics of 11 includes
|
Study (first author, year) |
Country |
Study design |
n |
Diameter |
Circularity |
Tears |
||||
|
FSL |
CCC |
|
CCC |
FSL |
CCC |
|
CCC |
|||
|
Schultz T, 2014[25] |
Germany |
Case control |
50 |
50 |
0.99±0.03 |
0.98±0.34 |
0.95±0.02 |
0.81±0.07 |
- |
- |
|
Reddy KP, 2013[20] |
Germany |
RCT |
56 |
63 |
1.02±0.05 |
0.93±0.09 |
0.97±0.02 |
0.92±0.05 |
1 |
1 |
|
Tackman RN, 2011[21] |
Mexico |
Case control |
49 |
24 |
0.97±0.18 |
0.92±0.53 |
- |
- |
- |
- |
|
Kranitz K, 2011[11] |
Hungary |
Case control |
20 |
20 |
1.01±0.15 |
1.04±0.42 |
0.86±0.01 |
0.83±0.02 |
- |
- |
|
Friedman NJ, 2011[4] |
USA |
Case control |
39 |
23 |
0.99±0.03 |
0.93±0.26 |
0.94±0.04 |
0.80±0.15 |
0 |
0 |
|
Nagy ZZ, 2011[22] |
Hungary |
RCT |
54 |
57 |
- |
- |
0.86±0.04 |
0.85±0.03 |
- |
- |
|
Palanker DV, 2010[12] |
USA |
RCT |
29 |
30 |
- |
- |
0.95±0.04 |
0.77±0.15 |
- |
- |
|
Abell RG, 2014[19] |
Australia |
Case control |
804 |
822 |
- |
- |
- |
- |
15 |
1 |
|
Abell R, 2012[24] |
Australia |
Case control |
200 |
200 |
- |
- |
- |
- |
1 |
1 |
|
Conrad-Hengerer I, 2013[26] |
Germany |
RCT |
75 |
75 |
- |
- |
- |
- |
0 |
1 |
|
Abell RG, 2013[27] |
Australia |
Case control |
151 |
50 |
- |
- |
- |
- |
0 |
0 |
FSL: Femtosecond laser capsulotomy; CCC:
Manual continuous curvilinear capsulotomy; RCT: Randomized controlled trial; “-”:
Unrelated.
Table 2 summarizes the quality of the 11 studies. Their quality
scores ranged from 17 to 20, with an average of 18.27±0.90. Based on the
Quality Assessment Score (QAS), all studies were rated good. In surgical
research, it was difficult to mask patients and outcome assessors, the criteria
of blind and measuring were zero in all the included studies, which was a
potential heterogeneity between studies.
Table 2 Scores of Downs and
Black scale
|
Studies (first author, year) |
Reporting |
External
validity |
Internal
validity bias |
Internal
validity confounding |
Total scores |
|
Schultz T, 2014[25] |
9 |
3 |
4 |
2 |
18 |
|
Reddy KP, 2013[20] |
10 |
3 |
4 |
3 |
20 |
|
Tackman RN, 2011[21] |
8 |
3 |
4 |
2 |
17 |
|
Kranitz K, 2011[11] |
9 |
3 |
4 |
2 |
18 |
|
Friedman NJ, 2011[4] |
9 |
3 |
4 |
2 |
18 |
|
Nagy ZZ, 2011[22] |
9 |
3 |
4 |
3 |
19 |
|
Palanker DV, 2010[12] |
8 |
3 |
4 |
3 |
18 |
|
Abell RG, 2014[19] |
9 |
3 |
4 |
3 |
19 |
|
Abell R, 2012[24] |
8 |
3 |
4 |
2 |
17 |
|
Conrad-Hengerer I, 2013[26] |
9 |
3 |
4 |
3 |
19 |
|
Abell RG, 2013[27] |
9 |
3 |
4 |
2 |
18 |
Diameter Five studies provided data[4,11,20-21,25] for calculating the MD of capsulotomy diameter
(Figure 1). There was no statistically significant difference in the diameter
between FSL and manual CCC groups (MD=0.03; 95%CI, -0.03 to 0.09,P=0.31). The studies were
characterized by low heterogeneity (I2=0,
tau2=0, P=0.8869). The
funnel plot was symmetric, with no evidence of a relevant small study bias
(Figure 2).
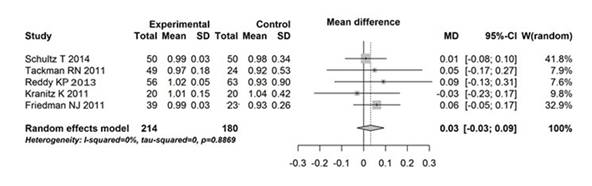
Figure 1 Forest plot comparing of diameter in
femtosecond laser capsulotomy (experimental) versus that in manual CCC (control).
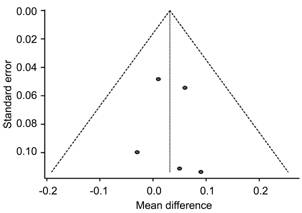
Figure 2 Funnel plot of publication bias of
diameter.
Circularity Six studies provided data[4,11-12,20,22,25] for calculating the MD of capsulotomy
circularity (Figure 3. There was a statistically significant difference in the
circular between FSL capsulotomy and manual CCC groups (MD=0.09; 95%CI,
0.05 to 0.12, P<0.0001). The
studies were characterized by high heterogeneity (I2=96.2%, tau2=0.0019,P<0.0001). A subgroup
analysis showed no significant differences in studies between RCTs studies and the case control
studies (P=0.56), still with high heterogeneity (I2=92.9% and 98%).
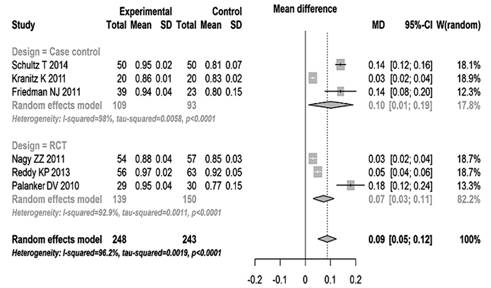
Figure 3 Forest plot comparing overall effect
of circularity with femtosecond laser capsulotomy (experimental) versus manual CCC (control).
Anterior Capsule Tear Six studies[4,19-20,24,26-27] reported capsule tears intraoperative (Figure
4). Two reported zero[4,27].
The incidence of
anterior capsule tear was 17 of 1325 eyes (1.28%) in FSL group compared with 4
of 1233 eyes (0.32%) in manual group. Meta-analysis shows no statistically significant difference
between the FSL and manual groups (OR=1.40; 95%CI, 0.28 to 6.97, P=0.68). Moderate heterogeneity was
identified in this analysis (I2=42.2%,
tau2=1.657, P=0.1235). A subgroup
analysis showed no significant differences between RCTs studies and the case control studies (P=0.52). The heterogeneity was moderate in case control (I2=56.1%) and low in RCTs studies (I2=0).
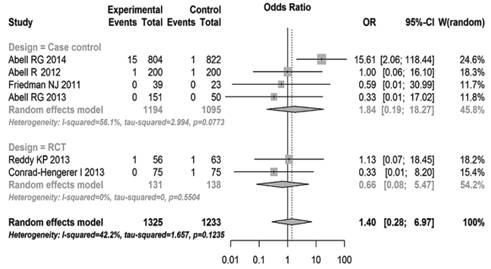
Figure 4 Conventional computation
overall effect of the OR and 95%CI on tears with femtosecond laser capsulotomy
(experimental events) versus manual CCC (control
events).
DISCUSSION
Femtosecond lasers
are able to create exquisitely precise, customizable incisions in ocular tissue
without collateral damage[28]. The results of FSL applications in cataract
surgery for more than 4y are promising[29-30]. Recently a study found a significantly
higher rate of anterior capsule tears in FSL capsulotomy[19], thus we performed a Meta-analysis to compare
the diameter and circularity of capsulotomy, and rate of anterior capsule tears
between FSL and manual CCC to assesse the new technology of FSL in capsulotomy.
A
precise and well-performed capsulotomy can improve the steps of cataract
extraction, and reduce complications[31]. Variations in size of the capsulorhexis can
result in aberrant IOL position[32]. The size and shape of the capsulorhexis
therefore are key determinants in both position and performance of IOL[25], but they can be variable. A 360° overlapping
capsular edge is thought to be an important factor for standardizing refractive
results by keeping the IOL in the desired center position. The overlap sets not
only the horizontal-vertical but also the anteroposterior positioning of the
IOL[32]. Because the data of diameter came from (dmajor/horizontal
+ dminor/vertical) /2, there was little diffculty for the
experienced surgeons to perform a capsulorhexis in order to attain the size and
shape that they want through manual technique. So in the fiver studies of
diameter, there was no statistical significant difference in diameter of
capsulotomy between FSL and manual CCC groups. The contour of the capsulorhexis
was ellipse and asymmetric in manual CCC. The mean deviation of capsule
diameter from intended diameter was 0.18±0.17 mm and significantly less in
buttons created using FSL compared with the mean deviation of 0.53±0.54 mm
among buttons constructed using manual CCC in Tackman’s study[21]. Friedman[4] demonstrated the deviation from the intended
diameter of capsule button was 29±26 μm using FSL and 337±258 μm using manual
CCC. So the overlap of the capsule on the IOL was better in FSL than in manual
CCC, the difference is significant (SMD=-1.29, P<0.0001).
Besides
the proper size, a perfect anterior capsule opening has to be resistant to
prevent capsular tears during surgery[33]. Circularity is a parameter used to determine the regularity of
the shape of the capsulotomy. In the six studies of circularity[4,11-12,20,22,25], the values of 1.0 indicate a perfect circle.
In Schultz et al’s[25] study, the capsule disk samples of the FSL
group were closer to an ideal roundness of 1. Very little variation was
observed in circularity in the FSL group and a greater variation in the manual
CCC groups. Palanker et al[12] reported similar results. An essential aspect
of the femtosecond laser cataract surgery is the integrated OCT that performs
3-D mapping of the cornea and lens. The system automatically aligns all
incision patterns in 3-D to follow the contour of ocular structures, which
minimizes the degree of required cutting overlaps and optimizes the safety zone
distances. This critical feature guarantees safe, precise, and reproducible
placement of the cutting patterns within the target tissue[4]. So the FSL may be able to provide a more
circular, stronger, precisely planned and executed capsulorhexis, which could
offer more control over capsulotomy unpredictability and more accurate
refractive outcomes than manual CCC[34]. Studies have demonstrated that a better
visual acuity was found in the patients treated with femtocataract comparing to
those treated with conventional cataract surgery in one year follow-up (P<0.05) [9]. Although, the other study found
post-operative CDVA was 0.97±0.08 in the FSL group and 0.97±0.06 in the
conventional group (P>0.05). But
the FSL group had significantly lower values of intraocular vertical tilt
(-0.50±0.36 vs 0.27±0.57) and coma
(-0.003±0.11 vs 0.1±0.15; P=0.006) [10].
Anterior
tear of the capsule is a significant complication in cataract surgery. Radial
tears in turn may lead to a series of complications such as zonular rupture,
posterior capsular tear, vitreous presentation, insufficient capsular support
for IOL implantation, or even nucleus drop during phacoemulsification[2]. Evidence-based guidelines for cataract surgery suggest a capsule
complication frequency of <2% should be possible and desirable to achieve[35]. In the included six studies of tear[4,19-20,24,26-27], the anterior capsule tear rates from 0 to
1.87% in FSL groups versus 0 to 1.6% in manual groups. Abell et al[19] reported 15 cases of anterior capsule tear, 7 anterior capsule
tear extended to the posterior capsule and required sulcus IOL implantation.
Five of these patients had no vitreous loss, whereas the remaining 2 patients
underwent an anterior and posterior vitrectomy, respectively. And 1 case in
manual CCC, the surgery procedure was evenly. During Roberts et al[30] early experiences, the anterior capsule tear
rates was 4%, and degraded to 0.31% when experienced. There was a clear
learning curve associated with the use of FSL for cataract surgery[36]. Study found that little manual manipulation
was needed in 96% of cases during removal of the capsule, indicating that a
free-floating capsule was generated by the FSL[21]. The Meta-analysis did not reveal any statistically significant
difference between the tears of the capsule from FSL groups and these from
manual CCC group (P=0.68). These
findings should be interpreted cautiously because Abell et al[19] was a multicenter study, where different
techniques and experience may introduce several variables. While other
studies were single surgeon completed the surgery in every study. Under
scanning electron microscope, compared with the smooth edges of the manual CCC
capsule disk, the FSL capsule disk edge has a wave-like structures or
postage-stamp perforations[19,25,37].This
can lead to an increased rate of anterior capsule tears.
Potential
limitations of this study should be considered. First because of retraction of
the capsular bag, the diameter of the excised capsulorhexis was slightly
smaller than the in situ diameter of the capsule cut. Second limitation is
predefined study population of each study. All studies excluded eyes with
ocular diseases, some studies even excluded patients with systemic diseases (e.g. rheumatic disease). As a result,
the findings in this Meta-analysis are only valid for patients meeting these
criteria and initially having good prognostic factors for visual outcome and
complications. Another limitation is the high heterogeneity in terms of
circularity. When we analyzed RCTs and Case control respectively, the heterogeneity
was still high. As we did not restrict laser platform, each company used
different measurement techniquesfor capsulotomy shape. As a result a
comparison is not easily assessed[8], and unknown sources of clinical variation of
the impact of circularity by unmeasured confounders and methodological issues.
Further, future studies, especially multicenter prospective randomized
controlled studies should be matched for FSL platform, FSL energy setting, lens
grades, surgeon’s experience, and study designs to make valid comparisons
between studies.
In
conclusion, the data from the Meta-analysis do not indicate an advantage of FSL
over manual CCC. Overall, the use of the femtosecond laser in cataract surgery resulted in a better
capsulorhexis geometry and circularity than manual CCC.
ACKNOWLEDGEMENTS
Conflicts of Interest: Qian DW, None; Guo
HK, None; Jin SL, None; Zhang HY, None; Li YC, None.
REFERENCES
1 Uy HS,
Edwards K, Curtis N. Femtosecond phacoemulsification: the business and the
medicine. <ii>Curr Opin Ophthalmol</ii> 2012;23(1):33-39. [CrossRef] [PubMed]
2 Mohammadpour M, Erfanian R, Karimi N. Capsulorhexis:
Pearls and pitfalls. <ii>Saudi J Ophthalmol </ii>2012;26(1):33-40.
[CrossRef] [PubMed] [PMC free article]
3 Sanders DR, Higginbotham RW, Opatowsky IE, Confino
J. Hyperopic shift in refraction associated with implantation of the
single-piece Collamer intraocular lens. <ii>J Cataract Refract
Surg</ii> 2006;32(12):2110-2112. [CrossRef] [PubMed]
4 Friedman NJ, Palanker DV, Schuele G, Andersen D,
Marcellino G, Seibel BS, Batlle J, Feliz R, Talamo JH, Blumenkranz MS,
Culbertson WW. Femtosecond laser capsulotomy. <ii>J Cataract Refract
Surg</ii> 2011; 37(7):1189-1198. [CrossRef] [PubMed]
5 Walkow T, Anders N, Pham DT, Wollensak J. Causes of
severe decentration and subluxation of intraocular lenses. <ii>Graefes
Arch Clin Exp Ophthalmol</ii> 1998;236(1):9-12. [CrossRef]
6 Ravalico G, Tognetto D, Palomba M, Busatto P,
Baccara F. Capsulorhexis size and posterior capsule opacification. <ii>J
Cataract Refract Surg</ii> 1996;22(1):98-103. [CrossRef]
7 Sugar A. Ultrafast (femtosecond) laser refractive
surgery. <ii>Curr Opin Ophthalmol</ii> 2002;13(4):246-249. [CrossRef]
8 He L, Sheehy K, Culbertson W. Femtosecond
laser-assisted cataract surgery. <ii>Curr Opin Ophthalmol </ii>
2011;22(1):43-52. [PubMed]
9 Kranitz K, Mihaltz K, Sandor GL, Takacs A, Knorz MC,
Nagy ZZ. Intraocular lens tilt and decentration measured by Scheimpflug camera
following manual or femtosecond laser-created continuous circular capsulotomy.
<ii>J Refract Surg </ii>2012;28(4):259-263. [CrossRef] [PubMed]
10 Mihaltz K, Knorz MC, Alio JL, Takacs AI, Kranitz K,
Kovacs I, Nagy ZZ. Internal aberrations and optical quality after femtosecond
laser anterior capsulotomy in cataract surgery. <ii>J Refract
Surg</ii> 2011;27(10):711-716. [CrossRef] [PubMed]
11 Kranitz K, Takacs A, Mihaltz K, Kovacs I, Knorz MC,
Nagy ZZ. Femtosecond laser capsulotomy and manual continuous curvilinear
capsulorrhexis parameters and their effects on intraocular lens centration.
<ii>J Refract Surg </ii>2011;27(8):558-563. [CrossRef] [PubMed]
12 Palanker DV, Blumenkranz MS, Andersen D, Wiltberger
M, Marcellino G, Gooding P, Angeley D, Schuele G, Woodley B, Simoneau M,
Friedman NJ, Seibel B, Batlle J, Feliz R, Talamo J, Culbertson W. Femtosecond
laser-assisted cataract surgery with integrated optical coherence tomography.
<ii>Sci Transl Med </ii>2010;2(58):58ra85. [CrossRef] [PubMed]
13 Downs SH, Black N. The feasibility of creating a
checklist for the assessment of the methodological quality both of randomised
and non-randomised studies of health care interventions. <ii>J Epidemiol
Community Health</ii> 1998;52(6):377-384. [CrossRef] [PubMed] [PMC free article]
14 Altman DG, Burton MJ. The cochrane collaboration.
<ii>Langenbecks Arch Surg</ii> 1999; 384(5):432-436. [CrossRef] [PubMed]
15 Saunders LD, Soomro GM, Buckingham J, Jamtvedt G,
Raina P. Assessing the methodological quality of nonrandomized intervention
studies. <ii>West J Nurs Res</ii> 2003;25(2):223-237. [CrossRef]
16 Liang GL, Wu J, Shi JT, Liu J, He FY, Xu W.
Implantable collamer lens versus iris-fixed phakic intraocular lens
implantation to correct myopia: a meta-analysis. <ii>PLoS One</ii>
2014;9(8):e104649. [CrossRef] [PubMed] [PMC free article]
17 Higgins JP, Thompson SG, Deeks JJ, Altman DG.
Measuring inconsistency in meta-analyses. <ii>BMJ</ii>
2003;327(7414):557-560. [CrossRef] [PubMed] [PMC free article]
18 R. Core Team, R: A language and environment for
statistical computing. R Foundation for Statistical Computing. Vienna, Austria.
https://www.R-project.org/.2014
19 Abell RG, Davies PE, Phelan D, Goemann K, McPherson
ZE, Vote BJ. Anterior capsulotomy integrity after femtosecond laser-assisted
cataract surgery. <ii>Ophthalmology </ii> 2014;121(1):17-24. [CrossRef] [PubMed]
20 Reddy KP, Kandulla J, Auffarth GU. Effectiveness
and safety of femtosecond laser-assisted lens fragmentation and anterior
capsulotomy versus the manual technique in cataract surgery. <ii>J
Cataract Refract Surg </ii>2013;39(9):1297-1306. [CrossRef] [PubMed]
21 Tackman RN, Kuri JV, Nichamin LD, Edwards K.
Anterior capsulotomy with an ultrashort-pulse laser. <ii>J Cataract
Refract Surg</ii> 2011;37(5):819-824. [CrossRef] [PubMed]
22 Nagy ZZ, Kranitz K, Takacs A, Mihaltz K, Kovacs I,
Knorz MC. Comparison of intraocular lens decentration parameters after
femtosecond and manual capsulotomies. <ii>J Refract Surg</ii> 2011;
27(8):564-569. [CrossRef] [PubMed]
23 Abell RG, Davies PEL, Bylsma G, Phelan D, Goemann
K, Vote BJ. Does the femtosecond laser cut the anterior capsule in a safe and
accurate way? <ii>Clinical and Experimental Ophthalmology </ii>
2013; 41:64-65.
24 Abell R, Kerr N, Vote B. Catalys femtosecond laser
pretreatment in cataract surgery compared to conventional phacoemulsification
cataract surgery. <ii>Clinical and Experimental Ophthalmology</ii>
2012; 40:52-53.
25 Schultz T, Joachim SC, Tischoff I, Dick HB.
Histologic evaluation of in vivo femtosecond laser-generated capsulotomies
reveals a potential cause for radial capsular tears. <ii>Eur J
Ophthalmol</ii> 2014;25(2):112-118 [CrossRef] [PubMed]
26 Conrad-Hengerer I, Al JM, Schultz T, Hengerer FH,
Dick HB. Corneal endothelial cell loss and corneal thickness in conventional
compared with femtosecond laser-assisted cataract surgery: three-month
follow-up. <ii>J Cataract Refract Surg</ii> 2013;39(9):1307-1313. [CrossRef] [PubMed]
27 Abell RG, Kerr NM, Vote BJ. Toward zero effective
phacoemulsification time using femtosecond laser pretreatment. <ii>Ophthalmology</ii>
2013;120(5):942-948. [CrossRef] [PubMed]
28 Trikha S, Turnbull AM, Morris RJ, Anderson DF,
Hossain P. The journey to femtosecond laser-assisted cataract surgery: new
beginnings or a false dawn? <ii>Eye (Lond) </ii>2013;27(4):461-473.
[CrossRef] [PubMed] [PMC free article]
29 Nagy Z, Takacs A, Filkorn T, Sarayba M. Initial
clinical evaluation of an intraocular femtosecond laser in cataract surgery.
<ii>J Refract Surg </ii> 2009;25(12):1053-1060. [CrossRef] [PubMed]
30 Roberts TV, Lawless M, Bali SJ, Hodge C, Sutton G.
Surgical outcomes and safety of femtosecond laser cataract surgery: a
prospective study of 1500 consecutive cases. <ii>Ophthalmology
</ii>2013;120(2):227-233. [CrossRef] [PubMed]
31 Ostovic M, Klaproth OK, Hengerer FH, Mayer WJ,
Kohnen T. Light microscopy and scanning electron microscopy analysis of rigid
curved interface femtosecond laser-assisted and manual anterior capsulotomy.
<ii>J Cataract Refract Surg</ii> 2013;39(10):1587-1592. [CrossRef] [PubMed]
32 Cekic O, Batman C. The relationship between
capsulorhexis size and anterior chamber depth relation. <ii>Ophthalmic
Surg Lasers </ii> 1999;30(3):185-190. [PubMed]
33 Artzen D, Lundstrom M, Behndig A, Stenevi U, Lydahl
E, Montan P. Capsule complication during cataract surgery: case-control study
of preoperative and intraoperative risk factors: Swedish Capsule Rupture Study
Group report 2. <ii>J Cataract Refract Surg</ii>
2009;35(10):1688-1693. [CrossRef] [PubMed]
34 Moshirfar M, Churgin DS, Hsu M. Femtosecond
laser-assisted cataract surgery: A current review. <ii>Middle East Afr J
Ophthalmol </ii> 2011;18(4):285-291. [CrossRef] [PubMed] [PMC free article]
35 Lundstrom M, Barry P, Henry Y, Rosen P, Stenevi U.
Evidence-based guidelines for cataract surgery: guidelines based on data in the
European Registry of Quality Outcomes for Cataract and Refractive Surgery
database. <ii>J Cataract Refract Surg</ii> 2012;38(6):1086-1093. [CrossRef] [PubMed]
36 Bali SJ, Hodge C, Lawless M, Roberts TV, Sutton G.
Early experience with the femtosecond laser for cataract surgery.
<ii>Ophthalmology</ii> 2012;119(5):891-899. [CrossRef] [PubMed]
37 Schultz T, Tischoff I, Ezeanosike E, Dick HB.
Histological sections of corneal incisions in OCT-guided femtosecond laser
cataract surgery. <ii>J Refract Surg</ii> 2013;29(12):863-864. [CrossRef] [PubMed]
[Top]