·Opinion· ·Current
Issue· ·Achieve· ·Search Articles· ·Online Submission· ·About IJO·
New
two-point scleral-fixation technique for foldable intraocular lenses with four
hollow haptics
He-Ting Liu, Zheng-Xuan Jiang, Li-Ming Tao
Department of
Ophthalmology, the Second Hospital Affiliated to Anhui Medical University,
Hefei 230601, Anhui Province, China
Correspondence to: Li-Ming Tao. Department of Ophthalmology, the Second Hospital Affiliated
to Anhui Medical University, Hefei 230601, Anhui Province, China.
taolimingchina@163.com
Received:
2014-11-06
Accepted: 2015-08-08
Abstract
The study was to report a
new two-point scleral-fixation technique for foldable intraocular lenses with
four haptics. Lenses were slid into the anterior chamber from a
2.8 mm corneal incision and fixed under two sclera flaps at two opposite
points. The postoperative best-corrected visual acuities (BCVAs) of all patients were
significantly better than their preoperative BCVA. The results demonstrate that
two-point, scleral fixations of foldable, intraocular lenses might be
practicable and effective.
KEYWORDS: cataract; intraocular lens; aphakia; scleral fixation
DOI:10.18240/ijo.2016.03.26
Citation: Liu HT,
Jiang ZX, Tao LM. New two-point
scleral-fixation technique for foldable intraocular lenses with four hollow
haptics. Int J Ophthalmol 2015;9(3):469-471
INTRODUCTION
More and more patients in China
received cataract surgery in recent years. For various reasons, without
sufficient capsular support aphakia might appear in some of these patients.
Additional studies have demonstrated a technique for fixing intraocular lens
(IOL) in aphakic patients with insufficient capsular support[1-2]. However, implantation of traditional polymethyl-methacrylate IOL requires a
larger incision which can cause iatrogenic
astigmatism, intraoperative hypotony, and detachment of the choroid. That said,
with the further development of ocular
science and technology, a greater range of foldable IOL types have become
available; indeed, recent studies have
reported the success of techniques that use small-incision injector
implantations of foldable IOLs[3-4].
The presented technique entails the
placement of an acrylic, posterior-chamber IOL. The one-piece lens used has
four haptics and is inserted through a small incision, using a sutured,
two-point fixation. The four-haptic IOL not only obviates large incisions, it
also reduces the chance of displacement.
SUBJECTS AND METHODS
Patient Assessments Single eyes of 16 patients (mean age: 37.9y; range:
9-72y; 12 males and 4 females) comprised the sample for this study. The eyes
included in this study evinced a complete lack of or, at the very least,
inadequate posterior capsular support. Patients with serious corneal scars,
glaucoma, proliferative diabetic retinopathies, or age-related macular
degeneration were excluded. All patients were recruited from the Department of
Ophthalmology, the Second Affiliated Hospital of Anhui Medical University in
Hefei, Anhui Province, China, from February, 2011 to February, 2012. All
patients provided informed consent. The study was approved by the local
institutional-ethics committee of the Second Affiliated Hospital of Anhui
Medical University. All procedures followed the tenets of the Declaration of
Helsinki.
Materials A complete preoperative assessment including slit-lamp, fundus, visual
acuity, best-corrected
visual acuity (BCVA), spherical equivalents (SE), and corneal
endothelial cell count (ECC) evaluations, which were performed on all patients. A logMAR visual chart was used to test visual acuity. The
IOL’s power was calculated using IOL Master (Carl Zeiss Meditec AG, YZB/GEM
4270-2008). A one-piece, acrylic-posterior chamber lens (Bausch & Lomb;
Akreos Adapt; 5.5 mm optics; 11.0 mm, 10.7 mm, or 10.5 mm haptic diameter) was
implanted into the eye using the accompanying injector system. Statistical analysis was performed using SPSS software
(version 13.0; SPSS, Inc., Armonk, NY, USA). A P<0.05 was considered statistically significant.
Surgical Technique Figure 1 was showing the operation pattern, while Figure
2 was a photo of the operation itself. After retro-bulbar anesthesia was
administered, two triangular, limbus-based sclera flaps
approximately half the thickness of the sclera were created in each eye at the
4 and 10 o’clock locations. Forceps were used to gently grasp the outer edges
of the sclera flaps at their 10 o’clock locations. A 2.8 mm side-port blade was
then used to make a full-thickness, self-sealing incision under each sclera
flap, and the resulting anterior chambers were entered. A 10-0, double-armed
polypropylene suture [AUM-5&SC-5; 0.2 METRIC; 30 cm (10-0); Alcon,
Dallas-Ft. Worth, TX, USA] was used, one end of which suture was a
curved needle and the other end of which was a straight needle. Then, the
straight needle was inserted at the 10 o’clock location through the bed of each
sclera flap, 1-1.5 mm posterior to the limbus,
and threaded into a 27-gauge needle, which had been inserted into the anterior
chamber from the same location on the opposite side (Figures 1A-1B, 2A-2B). The
sutures were cut after they had been pulled out through the corneal incisions
using a hook (Figures 1C, 2C). The two ends of each suture were settled for
fixing each IOL’s haptics. In each operation, an IOL (Akreos, Basuch&Lomb)
was placed into its accompanying injector with the aid
of its viscoelasticity. A lenticular hook was used to keep one haptic
(the first haptic) outside each eye (Figures 1D, 2D). Each suture at
the 4 o’clock location was tied, leaving the annular haptic outside the eye;
then, each haptic was slid back into the anterior chamber (Figures 1E-1F, 2E-2F).
Next, each anterior-chamber lens was carefully rotated clockwise 180° with a
hook (Figures 1G-1H, 2G-2H). The opposite haptic (the second haptic), which was
180° discrete from the first haptic, was hooked from each corneal incision and
was then tied with each suture at the 10 o’clock location (Figures 1I-1J,
2I-2J). Afterward, the second haptic was slid back into each anterior chamber.
Finally, the tightness of each suture at the 4 and 10 o’clock locations was
adjusted, to ensure each IOL remained at the center of the eye (Figures 1K,
2K).
The
curved needle attached to each 10-0 polypropylene suture and exiting from the
sclera bed was used to secure the superior haptic with a knot after the IOL’s
position was checked. Each knot was trimmed and buried under the sclera flap,
which was closed with a 10-0 monofilament suture (Figures 1, 2).
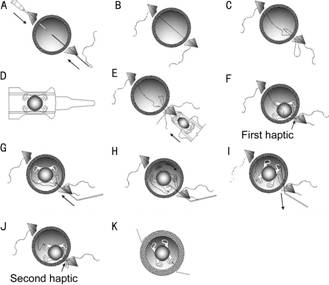
Figure 1 Photo showing the operation
pattern.
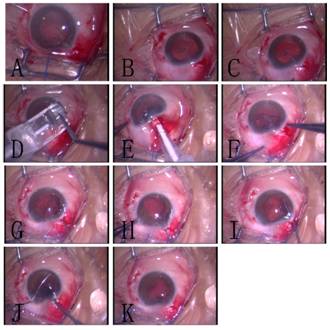
Figure 2 Photo of the operation.
RESULTS
The
patients were examined postoperatively 3d, 1wk, 1, 6, 24mo after their
respective operations. These follow-up examinations consisted of BCVA, SE,
slit-lamp, keratometry, ECC, and fundus evaluations, as well as the use of an
ultrasound biological microscope. All eyes maintained or improved their BCVAs
postoperatively; preoperatively, the patients’ mean BCVAs were 0.98±0.37,
whereas, after 24mo, their results for the same had improved to a mean of
0.52±0.07 (P=0.005, paired sample t-test). The mean preoperative SE was
1.45±1.00, and the mean postoperative SE was 1.42±1.00, thus evidencing no
significant improvement to SE between the pre- and postoperative states (P=0.388, paired sample t-test). The mean preoperative ECC was
2726±713, and the mean postoperative ECC was 2700±708 (three months after
surgery), thus evidencing no significant improvement to ECC between the pre-
and postoperative states as well (P=0.114,
paired sample t-test). No IOL
displacement, suture exposure, pigment dispersion, endophthalmitis, or retinal
detachment occurred. The most common complication was cystoid macular edema,
which occurred in two eyes (12.5%) and from which the subject patients
recovered within 6mo. Intraoperative hypotony and vitreous hemorrhage each
occurred in one eye (6.25%), and both subject patients recovered without
further treatment for these conditions within 1mo of surgery.
DISCUSSION
When the
IOL cannot be implanted into the eye because of insufficient capsular support,
scleral fixation might be considered as one of the most practicable alternative
treatments. Most reports suggest that a foldable-acrylic IOL with two haptics
is the most suitable for scleral fixation because it can be inserted through a
small corneal incision with or without the use of an injector[3]. Fass and Herman[4] have
reported their use of a foldable-acrylic IOL in eyes without sufficient capsule
support. According to their report, limbus-based scleral tunnels and dual
paracenteses were created in the sulcus. Then the IOLs were fixed to the
sclerals through said tunnels for four points. Thus, although the Akreos IOL
has been in use for many years ago, the IOLs used in the present study were
rotated clockwise for both scleral and two-point intra-scleral fixation.
Because
smaller incisions have highly advantageous to vision improvement, surgeons
typically prefer to let them as small as possible. Indeed, traditional
large-incision techniques often cause intraoperative hypotony, postoperative
hypotony, and subsequent vitreous hemorrhaging. The technique presented herein
therefore incorporated the use of a sutureless, 2.8 mm incision and a one
piece-lens injection. A closed, anterior-chamber system utilizing the 2.8 mm
incision maintained constant intraocular pressure. This surgical technique
could reduce complications associated with intraoperative hypotony, especially
in eyes with little to no vitreous support[4];
moreover, it could promote better visual rehabilitation of the postoperative
eye, while the use of a sutureless, 2.8 mm incision can reduce the likelihood
of postoperative astigmatism.
IOL
dislocation is one of the most serious complications of transscleral and
scleral fixation, which can lead to clinically significant, uncorrectable
irregular astigmatism and diminish the efficacy of the implant. When a
traditional, two-haptic IOL is implanted in the eye without capsular support,
the IOL might roll and cause retinal damage. Reducing the occurrence of this
complication has become one of the most important of ophthalmological goals.
The four-haptics system featuring transscleral scleral fixation, as presented
herein, is one promising realization of this goal; it not only ensures the IOL
remain fixed at the center of the eye due to haptic short-arm force, but also
due to said short-arm force, it provides uniform tension on both symmetrical
haptics over a large surface area as well.
Finally,
it is worth noting that suture exposure did not occur in any of the 16 cases
after 2y. Although many other practitioners have begun using newer kinds of
sutures[5-6], such as the
9-0 suture, and have even gone so far as to use sutureless techniques[7], the 10-0 suture used in
present study proved safe and caused comparatively fewer eye lesions. Thus,
long-term follow-ups to the present study should be conducted to determine
whether the sutures used degrade.
In conclusion, the presented technique, which introduces
injector implantation of transscleral IOLs and is a novel modification of the
two-point transscleral-fixation technique that instead uses a four-haptic,
foldable IOL, offers a simpler, lower-risk alternative to previously proposed
operations, as well as a shorter recovery time and faster restoration of the
visual function.
ACKNOWLEDGEMENTS
Conflicts of Interest: Liu HT, None; Jiang ZX, None; Tao LM, None.
REFERENCES
1 Por YM, Lavin MJ. Techniques of
intraocular lens suspension in the absence of capsular/zonular support.
<ii>Surv Ophthalmol</ii> 2005;50(5):429-446. [CrossRef] [PubMed]
2 Kjeka O, Bohnstedt J, Meberg K, Seland JH. Implantation
of scleral-fixated posterior chamber intraocular lenses in adults.
<ii>Act Ophthalmol</ii> 2008;86(5):537-542. [CrossRef] [PubMed]
3 Kim DH, Heo JW, Hwang SW, Lee JH, Chung H. Modified
transscleral fixation using combined temporary haptic externalization and
injector intraocular lens implantation. <ii>J Cataract Refract
Surg</ii> 2010;36(5):707-711. [CrossRef] [PubMed]
4 Fass ON, Herman WK. Sutured intraocular lens placement
in aphakic post-vitrectomy eyes via small-incision surgery. <ii>J
Cataract Refract Surg </ii> 2009;35(9):1492-1497. [CrossRef] [PubMed]
5 LeBoyer RM, Werner L, Snyder ME, Mamalis N, Riemann CD,
Augsberger JJ. Acute haptic-induced ciliary sulcus irritation associated with
single-piece AcrySof intraocular lenses. <ii>J Cataract Refract
Surg</ii> 2005;31(7):1421-1427. [CrossRef] [PubMed]
6 Snyder ME, Perez MA. Tiltless and centration adjustable
scleral-sutured posterior chamber intraocular lens. <ii>J</ii>
<ii>Cataract Refract Surg</ii> 2014;40(10):1579-1583. [CrossRef] [PubMed]
7 Ohta T, Toshida H, Murakami A. Simplified and safe
method of sutureless intrascleral posterior chamber intraocular lens fixation:
Y-fixation technique. <ii>J Cataract Refract Surg
</ii>2014;40(1):2-7. [CrossRef] [PubMed]
[Top]