·Clinical Research··Current Issue· ·Achieve· ·Search
Articles· ·Online
Submission· ·About IJO·
The
refractive outcome of Toric Lentis
Mplus implant in cataract surgery
Patrick J Chiam1,
Say A Quah2
1Birmingham and Midland Eye Centre, City Hospital, Birmingham BH18 7QH,
United Kingdom
2Optegra Manchester Eye Hospital,
Manchester M20 2EY,
United Kingdom
Correspondence to: Patrick J Chiam.
Birmingham
and Midland Eye Centre, City Hospital, Dudley Road,
Birmingham
BH18 7QH, United Kingdom. pjtchiam@yahoo.com
Received:
2015-09-20
Accepted: 2015-11-17
Abstract
AIM: To evaluate the refractive outcome of Toric
Lentis Mplus
intraocular lens (IOL) implant.
METHODS: This
is a retrospective case series. Consecutive patients with corneal astigmatism
of at least 1.5 D had Toric Lentis Mplus IOL implant during cataract surgery. The
exclusion criteria included irregular astigmatism on corneal topography, large
scotopic pupil diameter (>6
mm), poor visual potential and
significant ocular comorbidity. Postoperative manifest refraction, uncorrected distance visual acuity (UDVA), best-corrected distance visual acuity (BCVA), uncorrected intermediate visual acuity (UIVA)
at 3/4 m and uncorrected near visual acuity (UNVA) were obtained.
RESULTS: There
were 70 eyes from 49 patients in this study. Patients were refracted at a
median of 8.9wk (range 4.0 to 15.5) from the operation date. Sixty-five percent
of eyes had 6/7.5 (0.10 logMAR) or better, and 99% 6/12 (0.30 logMAR) or better
postoperative UDVA. Eighty-nine percent could read Jaeger (J) 3 (0.28 logMAR)
and 95% J5 (0.37 logMAR) at 40
cm. The median magnitude of
astigmatism decreased from 1.91 D to 0.49 D (Wilcoxon, P<0.001) after the operation. The range of the cylindrical error
was reduced from 1.5-3.95 D (keratometric) preoperatively to 0.00-1.46 D
(subjective refraction transposed to corneal plane) postoperatively.
CONCLUSION: Toric Lentis Mplus IOL
has good predictability in reducing preexisting corneal astigmatism.
KEYWORDS: Toric Lentis Mplus; multi-focal intraocular
lens implant; refractive outcome
Citation: Chiam PJ, Quah SA. The refractive outcome of Toric
Lentis Mplus implant in cataract surgery. Int J Ophthalmol 2016;9(5): 699-702
INTRODUCTION
Multifocal intraocular lenses (IOLs) were first introduced in
the 1980s[1-2]. Meta-analyses of randomised control trials showed these IOLs improve
uncorrected near visual acuity without compromising distance visual acuity and
reduce spectacle dependence[3-5]. However, the presence of more than 1 diopter (D) astigmatism has been
shown to have an adverse effect on the performance of these IOLs[6-8]. This is a significant
issue especially corneal astigmatism of 1.25 D or more is prevalent in
up to 30% of eyes that have cataract surgery[9-12]. Toric IOL has been
reported to provide better predictability in reducing moderate corneal
astigmatism compared to opposite clear corneal incision or arcuate keratotomy[13-14].
Today’s patients are more demanding, and they seek total
visual rehabilitation and spectacle independence. These requirements have
spurred the development of toric multifocal IOLs. These IOLs simultaneously
correct corneal astigmatism and the loss of accommodative ability after
crystalline lens extraction. The implantation of toric monofocal IOLs during
phacoemulsification has been shown to be effective in correcting preexisting
corneal astigmatism[15-17].
The Lentis Mplus is refractive rotational asymmetry IOL
designed to overcome the drawbacks of multifocal IOLs by providing high
contrast sensitivity and minimizing halos and glare[16]. The Lentis Mplus IOL consists
of 2 radial sectors-one for distance and the other for near vision.
Currently there are three strengths of addition (add) for near ±3.00
D (LS-312
MF30), +2.00 D (LS-312 MF20) and +1.50 D (LS-312 MF15).
Eighty-four percent of patients with bilateral Lentis Mplus +3.00
D add
implants have been shown to be spectacle independent for distant, intermediate
and near vision[16]. A toric version of this IOL (LU-313
MF30T ) is available however there is no data published to date. The purpose of
this study is to evaluate the refractive outcome of the Toric Lentis Mplus
IOL.
SUBJECTS AND METHODS
Subjects This is a retrospective case series
with 70 consecutive eyes implanted with Toric Lentis Mplus IOL during
phacoemulsification. The patients were operated between January 2011 and
December 2012 by a single surgeon (Quah SA) at Optegra Manchester Eye Hospital,
UK. The tenets of the Declaration of Helsinki were followed for all study procedures.
Because this is a retrospective study informed consent was not obtained from the subjects.
The inclusion criteria for the toric IOL implant were regular
corneal astigmatism of at least 1.5 D. The exclusion criteria included
irregular astigmatism on corneal topography, large scotopic pupil diameter
(>6 mm), poor visual potential and significant ocular comorbidity e.g. macular disease and glaucoma.
Intraocular Lens Toric Lentis Mplus (model LU-313
MF30T) is a biconvex 1-piece multifocal acrylic IOL made with an aspheric
posterior surface design. The IOL has an 11.0 mm overall length, a 6.0 mm
optic, and a square haptic design with 0-degree angulation. The non-rotational
symmetric multifocal IOL with a refractive design combines an aspheric
asymmetric distance vision zone with a sector-shaped near vision zone with a
+3.00 D add. All Toric Lentis Mplus lenses are custom made and
ordered using an online toric intraocular lens calculator
(www.lentistoric.com).
Surgical Technique All operations were performed without
any complications. Marks were made on the cornea under topical anaesthetic on
the slit-lamp preoperatively. A narrow slit beam was directed at the centre of
the pupil across the cornea horizontally. Peri-limbal scratches at 30° and the steepest axis of
alignment were made with a sterile needle. A surgical marker pen was then used
to stain these scratches.
At the start of the operation 5.5 mm diameter was marked on
the cornea to facilitate the desired diameter of capsulorrhexis.
Phacoemulsification was performed through a 2.75 mm clear corneal incision
placed 30° temporally in all cases. The IOLs were implanted
using a disposable injector (viscoject BIO 2.2 injector). The reference marks
on the optic of IOL were then aligned with the premarked steepest axis and the
near sector of the IOL optic placed inferiorly.
The targeted spherical equivalent was zero or the first
negative (myopic) figure. Postoperative patients were advised to use topical
steroid for a month and antibiotic for a fortnight. The fellow eye was operated
within 1mo later.
Patient Examination Preoperatively, all
patients underwent a complete ophthalmic evaluation including subjective
refraction, biometry with IOL Master 500 (Carl Zeiss), corneal topography and
pupillometry with Schwind Sirius and Combi Wavefront Analyzer, slit lamp
examination, fundoscopy and applanation tonometry. Uncorrected distance visual
acuity (UDVA),
best-corrected distance visual acuity (BCVA), uncorrected intermediate visual acuity (UIVA) at 3/4
m and uncorrected near visual acuity (UNVA) were obtained.
Data and Statistical Analysis The data were collected in Microsoft®
Office Excel® 2007 spreadsheet and analyzed with IBM® SPSS® Statistics version
20. Snellen acuities were converted into logMAR for statistical calculations.
The magnitude of refractive change induced by the clear
corneal main incision at the beginning of the surgery was taken as 0.50
D and
factored into the toric IOL calculation. The postoperative astigmatism is the
manifest refractive cylindrical error obtained postoperatively. The latter was
vertexed on the cornea plane for comparison with preoperative
keratometric
astigmatism.
Shapiro-Wilk test was used to ascertain the data distribution
for normality. Paired Student’s t-test
and Wilcoxon signed rank test were used to analyse parametric and
non-parametric data respectively. The post-operative astigmatism was determined
whether it was different from zero using dioptric power matrix transformation.
Where appropriate the results were reported as mean±standard deviation.
The difference vector (DV) is the vector that allows the
induced surgical astigmatism effect to intended surgical astigmatism effect.
This is an absolute measure of success and ideally should be zero. The
magnitude of error (ME) is the arithmetic difference between the magnitudes of
the induced surgical astigmatism effect and intended surgical astigmatism
effect. The ME is positive if there is an overcorrection and negative for
undercorrection. The angle of error (AE) is the angle between the induced
surgical astigmatism effect and intended surgical astigmatism effect vectors.
If AE is positive, this means the achieved correction is counterclockwise to
the intended axis; if negative it is clockwise to the intended axis. The
absolute angle of error (AAE) is the sum of the absolute difference between the
intended and induced angle of correction. The correction index (CI) was
calculated as the ratio of the absolute values of Induced surgical astigmatism
effect to the Intended surgical astigmatism effect. An ideal correction index
is 1.0. If this is greater than 1.0, it means the operation has caused an
overcorrection, and if less than 1.0 refers to undercorrection.
RESULTS
There were 70 eyes from 49 patients in this study. There were
34 female (47 eyes) patients. The mean age was 60.2±7.7 year-old (range 47 to
81). Thirty-seven right and 33 left eyes were operated. There were no
intraoperative complications. Seven eyes with amblyopia and documented visual
potential of at least 0.30 logMAR were included.
The set of data distributed in a Gaussian fashion were pre
and postoperative spherical equivalent only (Shapiro-Wilk, P=0.21 and P=0.18). The rest was
non-Gaussian.
Visual Outcome Patients were refracted at a median
of 8.9wk (range 4.0 to 15.5) from the operation date. Table 1 shows the
preoperative and postoperative various distance visual acuities. Sixty-five
percent of eyes had 6/7.5 (0.10 logMAR) or better, and 99% 6/12 (0.30 logMAR)
or better postoperative UDVA.
Eighty-nine percent could read Jaeger (J) 3 (0.28 logMAR) and 95% J5
(0.37 logMAR) at 40 cm.
Table 1 Preoperative and postoperative visual acuity and refractive
error
|
Visual acuity |
Preoperative (logMAR) |
Postoperative (logMAR) |
P |
|
Median
UDVA |
0.90 |
0.10 |
<0.001a |
|
Range |
-0.10 to 1.70 |
-0.1 to 0.5 |
|
|
Mean UDVA |
0.76 |
0.10 |
|
|
Median BCVA |
0.10 |
0.00 |
0.001a |
|
Range |
-0.10 to 0.60 |
-0.10 to 0.30 |
|
|
Mean BCVA |
0.10 |
0.03 |
|
|
Median UIVA |
0.35 |
0.10 |
0.002a |
|
Range |
0.00 to 0.40 |
-0.10 to 0.30 |
|
|
Mean UIVA |
0.28 |
0.06 |
|
|
Median UNVA |
0.63 |
0.13 |
<0.001a |
|
Range |
0.10 to 0.90 |
0.00 to 0.60 |
|
|
Mean UNVA |
0.55 |
0.18 |
aWilcoxon signed rank test.
Fifty-six eyes (80%) had a manifest astigmatic error of 0.75
D or less. In these eyes, the median UDVA was 0.10 logMAR (range -0.10 to
0.30), UIVA 0.05 (range -0.10 to 0.20) and UNVA 0.13 (range 0.00 to 0.60). The
remaining fourteen eyes had astigmatic error of more than 0.75 D (maximum was
1.5 D). In this group, the median UDVA was 0.23 logMAR (range 0.10 to 0.50),
UIVA 0.10 (range 0.10 to 0.30) and UNVA 0.20 (range 0.10 to 0.53). The Wilcoxon
P values for each distant was 0.0001,
0.003 and 0.008.
Refractive Outcome Table 2 shows the preoperative and
postoperative refractive changes. The spherical equivalent (SE) before and
after the Toric Lentis Mplus implant was not statistically significant (paired
Student’s t-test, P=0.71). The median magnitude
of astigmatism decreased from 1.91 D to 0.49 D (Wilcoxon, P<0.001) after the operation. The
mean spherical equivalent postoperative was 0.00±0.36 D
and the range
was -1.00 to +1.00 D.
Table 2
Preoperative and postoperative refractive changes
|
Refractive error |
Preoperative (D) |
Postoperative (D) |
P |
|
Spherical equivalent |
|
|
|
|
Mean±SD |
-0.27±5.05 |
0.00±0.36 |
0.71a |
|
Range |
-10.00 to +9.13 |
-1.00 to +1.00 |
|
|
Astigmatism |
(Keratometric) |
(Subjective refraction at corneal
plane) |
|
|
Vector |
1.41 at 89.5° |
0.18 at 28.7° |
|
|
Median magnitude |
1.91 |
0.49 |
<0.001b |
|
Range |
1.5 to 3.95 |
0.00 to 1.46 |
|
aPaired student’s t-test; bWilcoxon signed rank test.
Table 3 reveals the vectorial
analysis of the astigmatic change. The DV was not significantly different from
zero (P=0.48). There was a slight overcorrection, as indicated by a
CI of 1.07.
Table 3
Preoperative
and postoperative astigmatism analysis
![]()
|
Parameters |
Astigmatism |
|
Intended surgical astigmatism effect |
1.41 D at 179.5° |
|
Induced surgical astigmatism effect |
1.51 D at 2.4° |
|
Difference vector |
0.18 D at 28.7°a |
|
Magnitude of error (D) |
0.10±0.36 |
|
Angle of error |
2.8°±4.5° |
|
Absolute angle of error |
3.7°±5.2° |
|
Correction index |
1.07 |
aNot significantly different from zero; P=0.48 (dioptric
power matrix transformation).
Forty-eight eyes (69%) had a postoperative subjective
refractive cylinder (at spectacle plane) of up to 0.50 D, and 56 eyes (80%) up
to 0.75 D. Two eyes from different patients had a residual cylinder of 1.25 D
and 1.50 D. These were the only ones higher than 1.00 D. The range of the
cylindrical error was reduced from 1.5-3.95 D (keratometric) preoperatively to
0.00-1.46 D (subjective refraction transposed to corneal plane)
postoperatively. Figure 1 shows the individual change in preoperative
keratometric astigmatism compared to postoperative subjective refraction. The
double angle vector diagram showed a reduced range of astigmatic spread after
the IOL implant (Figure 2).
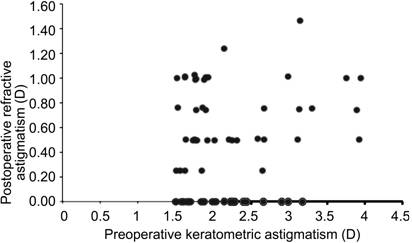
Figure 1 Change in
preoperative keratometric astigmatism versus postoperative subjective refractive
astigmatism.
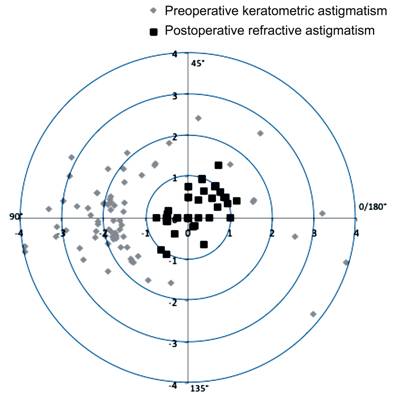
Figure 2 Double-angle
vectorial diagram for positive cylinder (D) pre and postoperation.
Patient Satisfaction All patients were satisfied with the
IOL implant and would recommend the procedure to a friend. These included the
two patients with residual postoperative astigmatism of 1.25
D and more.
Their preoperative astigmatisms were 2 and 3 D respectively. Despite
the photopic phenomenon was not formally evaluated, no patients complained of
severe symptoms requiring explantation.
DISCUSSION
Our results show that Toric Lentis Mplus IOL has good
predictability in reducing the amount of preexisting corneal astigmatism which
is crucial in allowing the maximum multifocal utility. Preoperatively the
median keratometric astigmatism was 1.91 D, and this was reduced to a median of
0.49 D in the postoperative subjective refractive astigmatism.
Currently, the published literature on the visual outcome of
Toric Lentis Mplus is limited. In our study, 69% of eyes had a subjective
manifest astigmatism of 0.50 D or less; and 80.0% had 0.75 D or less after the
operation. This is comparable to the only published data on Toric Lentis Mplus
by Venter and Pelouskova[18] where 65% of eyes had a refractive
astigmatism of 0.50 D or less despite their range of preoperative astigmatism
was slightly wider. The mean preoperative keratometric astigmatism in our study
was only 2.2 D, while the study aforementioned was 3.0 D. In other types of
toric multifocal IOL studies with comparable preoperative astigmatism, the
mean
postoperative refractive cylinders were found to be 0.40±0.25 D and 0.71±0.42 D[19-20]. Another series with higher
preoperative astigmatism of 3.4±1.17 D revealed a 3-month postoperative result
of 0.80±0.42 D[21].
Vector analysis of the overall astigmatic change shows that
the Toric Lentis Mplus has excellent predictability in correcting astigmatism
as shown by the small indices of ME, AE, AAE and CI. Our study could no
demonstrate a clear relationship between the amount of preoperative astigmatism
with the residual postoperative astigmatism as shown by Figure 1. A larger
study is required for this.
The UDVA in our study was 0.10 logMAR which was slightly
worse but within one Snellen line of Venter and
Pelouskova’s[18] result of 0.03. One of the reasons
might be due to the inclusion of 7 amblyopic eyes albeit their best recorded
visual potential was at least 0.3 logMAR or better. Excluding these eyes, our
UDVA improved to 0.09 logMAR. Our findings on UNVA was 0.18 logMAR which was
almost the same as Venter and Pelouskova’s[18] finding of 0.17. In a large series
non-Toric Lentis Mplus data, the mean UDVA was 0.05 logMAR and UNVA 0.21[22].
Patients found with residual objective astigmatism of more
than 0.75 D are more likely to be dissatisfied with their vision[23-24]. Our results showed
acuities at all distances were statistically significantly worse when the
astigmatism was more than 0.75 D. This shows the importance of residual
astigmatism to be corrected below this level. It’s not in the remit of this
study to discuss the options available to enhance the refractive error in these
cases.
The mean postoperative spherical equivalent in our study was
excellent at 0.00±0.36 D. A large study of non-Toric Lentis Mplus, with a
follow-up of more than 5000 eyes at 3-month found a SE of -0.02±0.60 D which is
comparable our findings[22]. This shows the
predictability of Toric Lentis Mplus is comparable to the non-Toric Lentis
Mplus.
Our study found the Toric Lentis Mplus LU-313 MF30T has
similar visual acuities at distance and near compared to the non-toric version
of the same IOL. Eyes with no or a residual astigmatism of less than 0.75 D has
the best acuity outcome. The refractive outcomes confirm the correction of
astigmatism by this IOL has a good predictability in majority of cases.
ACKNOWLEDGEMENTS
Chiam PJ analysed and wrote the manuscript, Quah SA conceived
the study idea, collected the data and provided critical review.
The study was
performed at the Optegra Manchester Eye Hospital, United Kingdom.
Conflicts
of Interest: Chiam PJ, None; Quah SA, None.
REFERENCES [Top]
1 Hansen TE, Corydon L, Krag S, Thim K. New multifocal
intraocular lens design. J Cataract
Refract Surg 1990;16:(1)38-41.
[CrossRef]
2 Leyland M, Zinicola E. Multifocal versus monofocal
intraocular lenses in cataract surgery; a systematic review. Ophthalmology 2003;110(9):1789-1798. [CrossRef]
3 Leyland M, Pringle E. Multifocal
versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev 2006; (4):
CD003169.
4 Statham M, Apel A, Stephensen D. Comparison of the AcrySof
SA60 spherical intraocular lens and the AcrySof Toric SN60T3 intraocular lens
outcomes in patients with low amounts of corneal astigmatism. Clin Exp Ophthalmol 2009;37(8):775-779.
[CrossRef] [PubMed]
5 Alio JL, Agdeppa MC, Pongo VC, El Kady B. Microincision
cataract surgery with toric intraocular lens implantation for correcting
moderate and high astigmatism: pilot study. J
Cataract Refract Surg 2010;36(1):44-52. [CrossRef] [PubMed]
6 Hayashi K, Manabe S, Yoshida M, Hayashi H. Effect of
astigmatism on visual acuity in eyes with a diffractive multifocal intraocular
lens. J Cataract Refract Surg 2010;36(8):1323-1329.
[CrossRef] [PubMed]
7 Ravalico G, Parentin F, Baccara F. Effect of astigmatism on
multifocal intraocular lenses. J Cataract
Refract Surg 1999;25(6):804-807. [CrossRef]
8 Hayashi K, Hayashi H, Nakao F, Hayashi F. Influence of
astigmatism on multifocal and monofocal intraocular lenses. Am J Ophthalmol 2000;130(4):477-482. [CrossRef]
9 Ferrer-Blasco T, Montés-Micó R, Peixoto-de-Matos SC,
González-Méijome JM, Cerviño A. Prevalence of corneal astigmatism before
cataract surgery. J Cataract Refract Surg
2009;35(1):70-75. [CrossRef]
[PubMed]
10 Hoffer KJ. Biometry of 7,500 cataractous eyes. AmJ Ophthalmol 1980; 90(3):360-368. [CrossRef]
11 Hoffmann PC, Hütz WW. Analysis of biometry and prevalence
data for corneal astigmatism in 23,239 eyes. J Cataract Refract Surg 2010;36(9):1479-1485. [CrossRef] [PubMed]
12 Holland E, Lane S, Horn JD, Ernest P, Arleo R, Miller KM.
The AcrySof toric intraocular lens in subjects with cataracts and corneal
astigmatism; a randomized, subject-masked, parallelgroup, 1-year study. Ophthalmology 2010;117(11):2104-2111. [CrossRef] [PubMed]
13 Mendicute J, Irigoyen C, Ruiz M, Illarramendi I,
Ferrer-Blasco T, Montés-Micó R. Toric intraocular lens versus opposite clear
corneal incisions to correct astigmatism in eyes having cataract surgery. J
Cataract Refract Surg 2009;35(3):451-418. [CrossRef] [PubMed]
14 Titiyal JS, Khatik M, Sharma N, Sehra SV, Maharana PK,
Ghatak U, Agarwal T, Khokhar S, Chawla B. Toric intraocular lens implantation
versus astigmatic keratotomy to correct astigmatism during phacoemulsification.
J Cataract Refract Surg 2014;40(5):741-747. [CrossRef] [PubMed]
15 Ahmed II, Rocha G, Slomovic AR, Climenhaga H, Gohill J,
Grégoire A Ma J, Canadian Toric Study Group. Visual function and patient
experience after bilateral implantation of toric intraocular lenses. J Cataract Refract Surg
2010;36(4):609-616. [CrossRef]
[PubMed]
16 Mendicute J, Irigoyen C, Ruiz M, Illarramendi I, Ferrer-Blasco
T, Montés-Micó R. Toric intraocular lens versus opposite clear corneal
incisions to correct astigmatism in eyes having cataract surgery. J Cataract Refract Surg
2009;35(3):451-458. [CrossRef]
[PubMed]
17 Muñoz G, Albarrán-Diego C, Ferrer-Blasco T, Sakla HF,
García-Lázaro S. Visual function after bilateral implantation of a new zonal
refractive aspheric multifocal intraocular lens. J Cataract Refract Surg 2011;37(11):2043-2052. [CrossRef] [PubMed]
18 Venter J, Pelouskova M. Outcomes and complications of a
multifocal toric intraocular lens with a surface-embedded near section. J Cataract Refract Surg 2013;39(6):859-866. [CrossRef] [PubMed]
19 Mojzis P, Piñero DP, Ctvrteckova V, Rydlova I. Analysis of
internal astigmatism and higher order aberrations in eyes implanted with a new
diffractive multifocal toric intraocular lens. Graefes Arch Clin Exp Ophthalmol 2013; 251(1):341-348. [CrossRef] [PubMed]
20 Visser N, Nuijts RMMA, de Vries NE, Bauer NJC. Visual outcomes
and patient satisfaction after cataract surgery with toric multifocal
intraocular lens implantation. J Cataract
Refract Surg 2011; 37(11):2034-2042. [CrossRef] [PubMed]
21 Alió JL, Piñero DP, Tomás J, Plaza AB. Vector analysis of
astigmatic changes after cataract surgery with implantation of a new toric
multifocal intraocular lens. J Cataract
Refract Surg 2011;37(7):1217-1229. [CrossRef] [PubMed]
22 Venter JA, Pelouskova M, Collins BM, Schallhorn SC, Hannan
SJ. Visual outcomes and patient satisfaction in 9366 eyes using a refractive
segmented multifocal intraocular lens. J
Cataract Refract Surg 2013;39(10):1477-1484. [CrossRef] [PubMed]
23 de Vries NE, Webers CA, Touwslager WR, Bauer NJ, de
Brabander J, Berendschot TT, Nuijts RM Dissatisfaction after implantation of
multifocal intraocular lenses. J Cataract
Refract Surg 2011;37(5):859-865. [CrossRef] [PubMed]
24 Woodward
MA, Randleman JB, Stulting RD. Dissatisfaction after multifocal intraocular
lens implantation. J Cataract Refract Surg 2009;35(6):992-997.
[Top]