·Clinical Research··Current Issue· ·Achieve· ·Search Articles· ·Online Submission· ·About IJO·
Comparison of two different methods of preoperative
marking for toric intraocular lens implantation: bubble marker versus pendulum
marker
Javed Hussain Farooqui, Archana Koul, Ranjan Dutta, Noshir Minoo Shroff
Cataract
and IOL Services, Shroff Eye Center, New Delhi 110048, India
Correspondence to: Javed Hussain Farooqui. C-44
Panchsheel Enclave, New Delhi 110017, India. jhfarooqui@gmail.com
Received:
2015-03-03
Accepted: 2015-07-21
Abstract
AIM: To compare the accuracy of two different methods of preoperative marking for toric intraocular lens (IOL) implantation, bubble marker versus pendulum marker, as a means of establishing the reference point for the final alignment of the toric IOL to achieve an outcome as close as possible to emmetropia.
METHODS: Toric IOLs were implanted in 180 eyes of 110 patients. One group (55 patients) had preoperative marking of both eyes done with bubble marker (ASICO AE-2791TBL) and the other group (55 patients) with pendulum marker (RumexÒ3-193). Reference marks were placed at 3-, 6-, and 9-o'clock positions on the limbus. Slit-lamp photographs were analyzed using Adobe Photoshop (version 7.0). Amount of alignment error (in degrees) induced in each group was measured.
RESULTS: Mean absolute rotation error in the preoperative marking in the
horizontal axis was 2.42±1.71 in the bubble
marker group and 2.83±2.31in the pendulum marker group (P=0.501). Sixty percent of the pendulum group and 70% of the bubble group had rotation error ≤3 (P=0.589),
and 90% eyes of the pendulum group and 96.7% of the bubble group had rotation
error ≤5 (P=0.612).
CONCLUSION: Both preoperative marking techniques result in approximately 3 of alignment error. Both marking techniques are simple, predictable, reproducible and easy to perform.
KEYWORDS: toric intraocular lens; pendulum marker; bubble marker
DOI:10.18240/ijo.2016.05.11
Citation: Farooqui JH, Koul A, Dutta R,
Shroff NM. Comparison of two different methods of preoperative marking for
toric intraocular lens implantation: bubble marker versus pendulum marker. Int J Ophthalmol 2016;9(5):703-706
INTRODUCTION
Toric intraocular
lenses (IOLs) have become an integral part of cataract and
refractive surgery. Toric IOLs were developed to
neutralize preexisting corneal astigmatism in cataract patients[1]. They provide the opportunity to correct
preexisting astigmatism, offering patients optimum distance vision without the
use of spectacles or contact lenses[2].
Alignment of the toric IOLs at the
calculated alignment axis is necessary to achieve effective astigmatism
correction. Misalignment of the IOL can be caused by inaccurate placement of
the IOL, rotation of the IOL, or both[3]. Accurate placement of the IOL is the most
important step in avoiding misalignment as the design and fixation techniques
of most of the IOLs today give them good rotational stability.
In addition to
careful keratometry and biometry for a toric IOL, accurate preoperative
marking, intraoperative marking and correct alignment of the IOL in the bag are
of utmost importance.
Various preoperative
marking techniques have been described, ranging from simple methods like single
free hand mark and simple toric reference markers, to slit-lamp based methods which include alignment by
a narrow slit beam and marking by gentian violet pen, Nd: YAG laser[4] and devgan axis marker[5].
New
techniques to improve the accuracy of toric IOL alignment have become
available. Osher[6] described an iris fingerprinting technique, in which a
preoperative detailed image of the eye is obtained and the alignment axis is
drawn. A printout of this image is used during surgery to align the toric IOL
based on iris characteristics. A second technique to align toric IOLs is by intraoperative wavefront aberrometry[7] (Orange, Wavetec Vision Systems). This device is
connected to the operating microscope and enables intraoperative measurement of
residual refraction. A third device, the Surgery Guidance SG3000 system
(Sensomotoric Instruments GmbH), uses real time eye tracking based on iris and
blood vessel characteristics.
In
our series, we have
compared two different methods of preoperative marking for toric IOL
implantation- bubble marker and pendulum marker. The purpose of this study was
to compare the accuracy of the two methods as a means of establishing the
reference point for the final alignment of the toric IOL. This was done to
achieve an outcome as close as possible to emetropia.
SUBJECTS AND METHODS
Study Design and Patient Population This prospective study comprised recruitment of 180 eyes of 110
patients presenting to the Outpatient Department of Shroff
Eye Centre, New Delhi from January 2012 to January 2013. The study was carried out in
accordance with the Declaration of Helsinki and was registered with the
institutional review board and an approval was obtained from the ethics
committee. All patients enrolled in the study were explained the procedure and
were made to sign an informed consent.
The patients were divided in two groups. Patients were assigned alternately to both groups. In group 1, which comprised of 90 eyes of 55 patients, preoperative marking was done using a bubble marker (ASICO AE-2791TBL) (Figure 1A). In group 2, which also comprised of 90 eyes of 55 patients, preoperative marking was done using pendulum marker (RumexÒ3-193) (Figure 1B). Prior to the marking, the eye was anesthetized with 0.5% proparacaine drops. The patient was seated in the upright position and made to fixate at a distant target. Bubble marker (ASICO AE-2791TBL) was used for marking the reference marks for identifying the 3-, 6- and 9-o'clock positions on the limbus. When the bubble was in between the two vertical lines, it indicated that the 3- and 9- wedges of the marker were truly horizontal (Figure 2A). A special gentian violet pen was used to ink the wedges. The marker was gradually advanced towards the eye while the examiner ensured the bubble was in the central position when the wedges make contact with the limbus. Similarly, for the pendulum marker, the patient was asked to fixate on a distant target. The 0, 90 and 180 degrees contact wedges on a hemicircle of this device are rotatably coupled via a shaft within a hollow handle to a gravity pendulum which ensures that these wedges remain perfectly horizontal even if the handle is rotated to either side (Figure 2B). All marking procedures were performed by the same observer (Koul A).
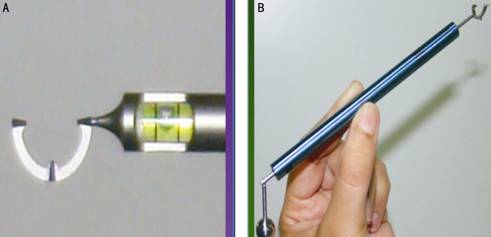
Figure 1 The use of two preoperative markers
A: Bubble marker
(ASICO AE-2791TBL);
B: Pendulum marker (Rumex®3-193).
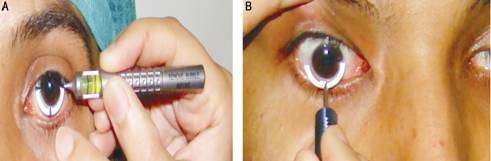
Figure 2 Preoperative
marking being done A: Bubble marker; B: Pendulum marker.
Image Analysis Slit-lamp photographs were analysed using tools in Adobe Photoshop
(version 7.0) and were taken by a single masked observer (Dutta R). Amount of alignment error in each group, as well as inter eye
difference within the same group was calculated. A preoperative photograph with
the reference marks was imported in the Adobe Photoshop (version 7). Using the
“single row marquee tool” a straight line was placed on the image adjacent to
the limbal reference marks using the “transform tool” straight line was
rotated in such a manner so as to align through the reference marks on the
limbus. The amount of rotation (clockwise or anti-clockwise) was noted from the
“set rotation” dialogue box, which is a feature of the Adobe Photoshop (version
7).
RESULTS
The study enrolled 180 eyes of 110 patients. The
mean age was 65y (range from 45 to 80y). The mean absolute rotation of
reference marks in the horizontal axis in group 1 was 2.42±1.71 and in group 2
was 2.83±2.31 (P=0.501) (Figure 3).

Figure 3 Comparison of rotational misalignment.
We
also analysed the percentage of eyes showing absolute rotation of reference
marks <3 degrees and <5 degrees. In group 1 70% (63 eyes) and in
group 2 60% (54 eyes) showed absolute rotation of reference marks <3 degrees (P=0.589). Also, an absolute
rotation of reference marks <5
degrees was seen in 96.7% (87 eyes) of group 1 patients and 90% (81 eyes) of
group 2 patients (P=0.612) (Figure 4).
Figure 4 Comparison of misalignment of ≤3°
and ≤5° in both groups.
DISCUSSION
We performed all our preoperative markings in
sitting position to avoid cyclotorsion. Cyclotorsion of the eye from the
upright to supine position is approximately 2 to 4 degrees on average, but can
be up to 15 degrees in individual patients[8-10].
During our study, there was no statistical
difference between the two marking techniques and both of them induced almost
similar amount of error.
Also, there were few observations that we made. In
the bubble marker group, we found it difficult to concentrate simultaneously on
patient’s eye as well as the position of the bubble. Marking of right eyes with
the investigator’s left hand (non-dominant hand) was difficult compared with
marking of left eye with the right hand (dominant hand). Similarly, with the
pendulum marker, right eyes as well as left eyes could be marked with equal
ease using the dominant hand. However, attention had to be paid to ensure that
all the three wedges of the hemi-circle
touch the limbus simultaneously. Premature contact with any one wedge would
induce a rotation leading to improper marking. Having said that, we still
consider both the bubble marker and the pendulum marker to be superior to the
slit-lamp technique and the free hand technique,
which were used earlier, as both the bubble marker and the pendulum markers are
more precise and reproducible techniques. Also, the advantage of both the
bubble marker and pendulum marker is that it can be done in the operating
theater. However, if the earlier slit-lamp
technique is to be used, then the patient has to be transferred to the
Outpatient Department where the slit-lamp is available, and this causes
unnecessary movement of the patient before the surgery and may be specifically
difficult for older patients or patients with gait abnormalities.
In
a comparative study done by Popp et al[11]
and colleagues in Vienna, the pendulum-marking device
showed the least rotational deviation to the reference meridian (mean 1.8
degrees). There was no statistically significant difference between slit-lamp
marking and pendular marking (P=0.05); however, there was a significant
difference between the pendulum marker and
the bubble marker.
To the best
of our knowledge, we could not find any other study done on Indian eyes where a
comparison was made between various preoperative marking techniques.
In
our study, both preoperative marking techniques resulted in approximately 3
degrees of alignment error. It is seen that with
10 degrees of axis deviation, 1/3 of the desired effect is lost. With 20
degrees of axis deviation, 2/3 of the effect is lost. Lens misalignment greater
than 30 degrees will actually increase the net astigmatic error[12]. Our
results were better than results shown by another study done comparing the
toric reference marker, slit beam marking and mapping method[13] and also by newer marking techniques like
iris fingerprinting[6]. The next step would be to study newer marking techniques which are
now available in the market, like electronic preoperative two steps toric
IOL reference marker[14].
Accuracy of corneal marking before surgery is critical to achieving good surgical-astigmatism correction outcomes, and both our marking methods gave good results. Errors in intraoperative marking and final alignment of the IOL in the bag could possibly add on to this error. We believe that slit-lamp based methods are cumbersome to perform and require greater patient cooperation; the YAG laser method requires additional instrumentation. Also, sophisticated methods such as iris fingerprinting and intraoperative wavefront aberrometry, although highly accurate, cannot be routinely incorporated in the average ophthalmologist’s practice. However, both the bubble marker and the pendulum marker for preoperative marking were simple, predictable, reproducible and easy to perform.
ACKNOWLEDGEMENTS
Presented at Delhi Ophthalmic Society
Annual Conference, Delhi, April 2013.
Conflicts of Interest: Farooqui
JH, None; Koul A, None; Dutta R, None; Shroff NM,
None.
REFERENCES
1
Shimizu K, Misawa A, Suzuki Y. Toric intraocular lenses: correcting astigmatism
while controlling axis shift. J Cataract Refract Surg 1994;20(5):523-526. [CrossRef]
2
Visser N, Berendschot TT, Bauer NJ, Jurich J, Kersting O, Nuijts RM. Accuracy
of toric intraocular lens implantation in cataract and refractive surgery. J
Cataract Refract Surg 2011;37(8):1394-1402. [CrossRef] [PubMed]
3 Lane SS. The Acrysof toric IOL’s FDA trial results.
Cataract & Refractive Surgery Today 2006;5:66-68.
4 Crespo Bordonaba M, Alvarez-Rementería Fernandez L.
Marking the axis for toric IOL implantation. Cataract & Refractive Surgery
Today 2009;7:27-28.
5
Graether JM. Simplified system of marking the cornea for a toric intraocular
lens. J Cataract Refract Surg 2009;35(9):1498-1500. [CrossRef] [PubMed]
6
Osher RH. Iris fingerprinting: new method for improving accuracy in toric lens
orientation. J Cataract Refract Surg 2010;36(2):351-352. [CrossRef] [PubMed]
7
Packer M. Effect ofintraoperativeaberrometryon the rate of postoperative enhancement:
retrospective study. J Cataract Refract Surg 2010;36(5):747-755. [CrossRef] [PubMed]
8
Arba-Mosquera S, Merayo-Lloves J, de Ortueta D. Clinical effects of pure
cyclotorsional errors during refractive surgery. Invest Ophthalmol Vis Sci
2008;49(11):4828-4836. [CrossRef]
[PubMed]
9
Chernyak DA. Cyclotorsional eye motion occurring between wavefront measurement
and refractive surgery. J Cataract Refract Surg 2004;30(3):633-638. [CrossRef] [PubMed]
10
Swami AU, Steinert RF, Osborne WE, White AA. Rotationalmalposition during laser
in situ keratomileusis. Am J Ophthalmol 2002;133(4):561-562. [CrossRef]
11
Popp N, Hirnschall N, Maedel S, Findl O. Evaluation of 4 corneal astigmatic
marking methods. J Cataract Refract Surg 2012;38(12):2094-2099. [CrossRef] [PubMed]
12 Chang DF. Pearls on implanting the Staar toric IOL. Br
J Ophthalmol 2001;85:1-126.
13
Cha D, Kang SY, Kim SH, Song JS, Kim HM. New axis- marking method for a toric
intraocular lens: mapping method. J Refreact Surg 2011;27(5):375-379. [CrossRef] [PubMed]
14
Farooqui JH, Sharma M, Koul A, Dutta R, Shroff NM. Evaluation of a new
electronic pre-operative reference marker for toric IOL implantation by two
different methods of analysis: Adobe photoshop versus iTrace. Adv Ophthalmol
Vis Syst 2015;2(5):00057. [CrossRef]
[Top]