·Meta-Analysis· ·Current Issue· ·Achieve· ·Search Articles· ·Online Submission· ·About IJO·
Efficacy, safety, predictability,
aberrations and corneal biomechnical parameters after SMILE and FLEx:
Meta-analysis
Jing Ma, Nan-Jue Cao, Li-Kun Xia
Department of Ophthalmology, Shengjing Hospital of China Medical
University, Shenyang 110004, Liaoning Province, China
Correspondence to: Li-Kun Xia. Laser Treatment Center, Clinic Outpatient of Ophthalmology,
Department of Ophthalmology, Shengjing Hospital of China Medical University,
Shenyang 110004, Liaoning Province, China. xialk@sj-hospital.org
Received: 2015-10-31
Accepted: 2016-01-30
Abstract
AIM: To identify possible differences of efficacy, safety,
predictability, higher-order aberrations and corneal biomechnical parameters
after small-incision lenticule extraction (SMILE) and
femtosecond lenticule extraction (FLEx).
METHODS: A systematic literature retrieval was conducted in Medline,Embase and the Cochrane
Library, up to October, 2015. The included studies were subject to a Meta-analysis.
Comparison between SMILE and FLEx was measured as pooled odds
ratio (OR) or weighted mean differences (WMD). Of 95% confidence intervals (CI) were
used to analyze data.
RESULTS: A total of seven studies were included. Firstly, there were
no differences in uncorrected distance visual acuity (UDVA) 20/20 or better (OR, 1.37; 95%
CI, 0.69 to
2.69; P=0.37) and logMAR UDVA (WMD,
-0.02; 95% CI, -0.05 to 0.01; P=0.17)
after SMILE versus FLEx. We found no differences in corrected distance visual
acuity (CDVA) unchanged (OR, 0.98; 95% CI, 0.46 to 2.11; P=0.97) and logMAR CDVA (WMD, -0.00; 95% CI, -0.01 to 0.01; P=0.90) either. Secondly, we found no
differences in refraction within ±1.00 D (OR, 0.98; 95% CI, 0.13 to 7.28; P=0.99) and ±0.50
D (OR, 1.62; 95% CI, 0.62 to 4.28; P=0.33)
of target postoperatively. Thirdly, for higher-order aberrations, we found no
differences in the total higher-order aberrations (WMD, -0.04; 95% CI, -0.09 to
0.01; P=0.14), coma (WMD, -0.04; 95% CI,
-0.09 to 0.01; P=0.11), spherical
(WMD, 0.01; 95% CI, -0.02 to 0.03; P=0.60)
and trefoil (WMD, -0.00; 95% CI, -0.04 to 0.03; P=0.76). Furthermore, for corneal biomechanical parameters, we also
found no differences (WMD, 0.08; 95% CI, -0.17 to 0.33; P=0.54) after SMILE versus FLEx.
CONCLUSION: There are no statistically differences in efficacy, safety,
predictability, higher-order aberrations and corneal biomechnical parameters
postoperative between SMILE and FLEx.
KEYWORDS: visual quality; aberrations; corneal
biomechnical parameters; small-incision lenticule extraction; femtosecond
lenticule extraction
DOI:10.18240/ijo.2016.05.22
Citation: Ma J, Cao NJ, Xia LK. Efficacy,
safety, predictability, aberrations and corneal biomechnical parameters after SMILE
and FLEx: Meta-analysis. Int J Ophthalmol 2016;9(5):757-762
INTRODUCTION
Femtosecond laser has been introduced
into the refractive surgery market for laser in situ keratomileusis (LASIK) flaps for decades[1]. The
femtosecond laser has offered some advantages over manual microkeratomes,
including increased accuracy, fewer flap correlated complications, and the
ability to cut thinner flaps without the risk of forming a button hole[2-3]. In 2006, a
new breakthrough called refractive lenticule extraction (ReLEx) for correcting
myopia and myopic astigmatism was introduced[4]. In this procedure, neither a
microkeratome nor an excimer laser was required. It used only the femtosecond
laser system for flap creating and lenticule processing[5]. It was first conducted as femtosecond lenticule
extraction (FLEx). Clinical studies[6-8]
have evaluated FLEx as a potential alternative to femtosecond laser-assisted
LASIK. In other words, FLEx has been proved advanced[9-11]. Since then, the method developed and turned into
a flapless surgery named small-incision lenticule extraction (SMILE), which
allowed lenticule removal through a small incision[12]. Once it was first published in 2011,
SMILE has gained great interest among refractive surgeons for its flapless
feature and all-in-one femtosecond
laser procedure[13].
Clinical studies[14-15]
have shown that SMILE is a large success in the refractive surgery field.
Early refractive results have shown that ReLEx (SMILE and FLEx) is promising
and encouraging, but comparisons of the relative benefits between the two techniques are
still controversial. In the current study, a Meta-analysis was performed of
comparative studies of SMILE versus FLEx.
MATERIALS AND METHODS
Search Strategy We conducted a systematic
literature search (up to October, 2015) of Medline, Embase and the Cochrane
Library for studies describing the comparative outcomes of SMILE and FLEx. The
search terms were “small-incision lenticule extraction”, “femtosecond
lenticule extraction”, “SMILE” and “FLEx”. The search was limited to
English-published paper. The titles and abstracts were first selected according
to the objective of this study. The full-text articles were retrived to
determine whether they met our inclusion criteria.
Inclusion and Exclusion Criteria To start with, the studies had to be
randomized controlled trials (RCTs) or non-randomized comparative studies.
Second, the studies should compare the postoperative visual outcomes,
high-order aberrations or corneal biomechanical parameters postoperative. Third,
patients aged 18-60y with myopia and myopia astigmatism, no significant
co-pathology, no history of other ocular disease or previous ocular surgery, no
keratoconus or suspected keratoconus, no severe dry eyes, and no systemic
disease associated with impaired or abnormal wound healing. Patients were also
excluded with the calculated postoperative corneal residual bed thickness less
than 250 μm.
The search was not
restricted to RCTs, because of the paucity of the relevant studies. Controlled
clinical trials, including prospective and retrospective cohort studies, were
also included. Letters, review articles, animal or laboratory studies and conference
abstracts were not included. Studies irrelevent to our analysis were not
included.
Data Extraction Two independent
investigators (Ma J and Cao NJ) evaluated the quality of each study using the
Jadad Scale (5-point) or the Newcastle-Ottawa Scale (NOS). We used the Jadad
Scale for RCTs, the NOS for non-randomized cohort studies. The third
investigator (Xia LK) examined the results and a consensus was reached. Using
the Jadad Scale, high scores indicated high quality with questions regarding
randomization, double blinding and withdrawal and dropouts. Studies scoring
>3 points were considered to be of high quality. Using the NOS, we analyzed
the selection, comparability and outcomes. The maximum score was 9 points.
Studies scoring >6 points were considered to be of high quality.
Statistical Analysis All statistical analysis was
performed with Review Manager 5.3 (The Cochrane Collaboration, Oxford,
England). For continuous outcome data, we calculate the weighed mean
differences (WMD) in the Meta-analysis. For dichotomous outcome data, odds
ratios (ORs) were calculated. Of 95% confidence intervals (CIs) were calculated
for summary estimates. A P value less
than 0.05 was considered to be statistically significant different. A
fixed-effects model was used to pool the data. When substantial heterogerneity
was present, a random-effect model was used.
RESULTS
Literature Search
A
total of 23 studies were retrived and only 7 studies[16-22] were included in our analysis. The trial
selection process is shown in Figure 1
and Table 1. Four studies[17,19-20,22]
are RCTs, and the other 3 studies[16,18,21]
are non-randomized cohort studies (Tables 2, 3).
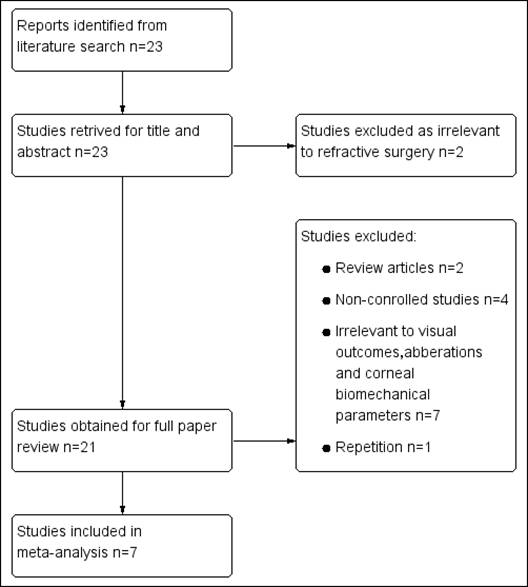
Figure 1 Study selection process of RCTs and non-randomizied
cohort studies.
Table 1 Characteristics of clinical studies
comparing SMILE and FLEx
|
Study |
Design |
Year |
Country |
SMILE group |
FLEx group |
Follow-up (mo) |
||
|
|
Preoperative |
Eyes (n) |
Preoperative |
|||||
|
Ang et
al[16] |
CT |
2014 |
Singapore |
17 |
-5.84±2.12 |
15 |
-5.90±2.01 |
12 |
|
Kamiya et
al[17] |
RCT |
2014 |
Japan |
26 |
-4.21±1.63 |
26 |
-4.18±1.72 |
6 |
|
Vestergaard
et al[18] |
CT |
2014 |
Denmark |
30 |
-7.56±1.11 |
31 |
-7.59±0.97 |
6 |
|
Agca
et al[19] |
RCT |
2014 |
Turkey |
20 |
-4.03±1.61 |
20 |
-4.46±1.61 |
12 |
|
Kamiya et
al[20] |
RCT |
2014 |
Japan |
24 |
-4.10±1.70 |
24 |
-4.10±1.70 |
3 |
|
Pedersen
et al[21] |
CT |
2014 |
Denmark |
29 |
-7.10±0.29 |
31 |
-7.43±0.20 |
- |
|
Vestergaard
et al[22] |
RCT |
2014 |
Denmark |
34 |
-7.56±1.11 |
34 |
-7.59±0.97 |
6 |
RCT: Randomized controlled trials;
CT: Comparetive trial; SE: Spherical equivalent; -: Not available.
Table 2 Jadad Scale (5-point) for
RCTs
|
Study |
Randomization |
Double blinding |
Withdrawals and dropouts |
Sum of score |
|
Kamiya et
al[17] 2014 |
2 |
2 |
1 |
5 |
|
Agca
et al[19] 2014 |
1 |
0 |
1 |
2 |
|
Kamiya et
al[20] 2014 |
1 |
0 |
1 |
2 |
|
Vestergaard
et al[22] 2014 |
1 |
0 |
1 |
2 |
Jadad Scale allocates 1 to 2 points
for the following items: Randomization, double blinding and withdrawal and
dropouts. The total score ranged from 0 to 5 (0-2 points means low quality and
3-5 points means high quality).
Table 3 Newcastle-Ottawa Scale for
non-randomized cohort studies
|
Study |
Selection |
Comparability |
Outcomes |
Sum of score |
|
Ang et
al[16] 2014 |
3 |
2 |
2 |
7 |
|
Vestergaard
et al[18] 2014 |
2 |
2 |
2 |
6 |
|
Pedersen
et al[21] 2014 |
3 |
2 |
2 |
7 |
NOS generates a quality score,
maximum of 9 points , based on assessment of three study characteristics:
selection (maximum of 4 points) , comparability (maximum of 2 points) and outcomes
(maximum of 3 points).
Quality Assessment
The
quality assessments of the included studies are shown in Tables 2, 3. In the 4 RCTs[17,19-20,22],
randomization, double blinding, withdrawal and dropouts were taken into
consideration. One study[17]
gained high score of 5 points, indicating high quality. Though the score of the
other 3 RCTs was not high, considering their clinical value and lacking in high
quality trials, we still included them in our analysis. In the NOS, we regarded
the selection, comparability and outcomes. All of the 3 studies gained high
score, indicating high quality.
Efficacy We calculated the
proportion of eyes with postoperative uncorrected distance visual acuity (UDVA)
of 20/20 or better. Four studies[16-19]
reported data for this outcome. Analysis of these data showed no
difference between the two groups (OR, 1.37; 95% CI, 0.69 to 2.69; P=0.37)
(Figure 2).

Figure 2 Proportion of eyes with UDVA 20/20 or better after
SMILE versus FLEx postoperatively.
We
also compared the mean logMAR UDVA between the two groups. Examination of the
forest plot showed no difference in the mean logMAR UDVA (WMD, -0.02; 95% CI, -0.05
to 0.01; P=0.17) (Figure 3).

Figure 3 LogMAR UDVA after SMILE versus FLEx postoperatively.
Safety We
counted the proportion of eyes with postoperative corrected distance visual
acuity (CDVA) unchanged postoperatively, 3 studies[17-19]
reported the results, showing no significant differences between the two groups
(OR, 0.98; 95% CI, 0.46 to 2.11; P=0.97)
(Figure 4).
Figure 4 Proportion of eyes with CDVA unchanged after SMILE versus
FLEx postoperatively.
Mean postoperative logMAR
CDVA were also analyzed. Three studies[17-19]
reported the mean logMAR CDVA and the results showed no significant differences
between the two groups (WMD, -0.00; 95% CI, -0.01 to 0.01; P= 0.90) (Figure 5).
Figure 5 LogMAR CDVA after SMILE versus FLEx postoperatively.
Predictability We analyzed the proportion
of eyes with postoperative refraction within ±1.00 D
and within ±0.50 D of target. Data were available for analysis in 4 studies[16-19]. There were no
statistically significant differences between the two groups within ±1.00 D of
target (OR, 0.98; 95% CI, 0.13 to 7.28; P=
0.99) (Figure 6) and within ±0.50 D of target (OR, 1.62; 95% CI,
0.62 to 4.28; P= 0.33) (Figure 7).
Figure 6 Proportion
of eyes with postoperative refraction within±1.00 D of target after SMILE
versus FLEx postoperatively.
Figure 7 Proportion of eyes with postoperative refraction within ±
0.50 D of target after SMILE versus FLEx postoperatively.
Corneal Higher-order Aberrations For higher-order aberrations (HOAs),
we analyzed total HOAs, coma, spherical and trefoil. Two studies[18-19] were
taken into account. The results showed no statistically significant differences
between the two groups in total HOAs (WMD, -0.04; 95% CI, -0.09 to 0.01; P=0.14), coma (WMD, -0.04; 95% CI, -0.09
to 0.01; P=0.11), spherical (WMD,
0.01; 95% CI, -0.02 to 0.03; P=0.60 )
and trefoil (WMD, -0.00; 95% CI, -0.04 to 0.03; P=0.76) (Figure 8).
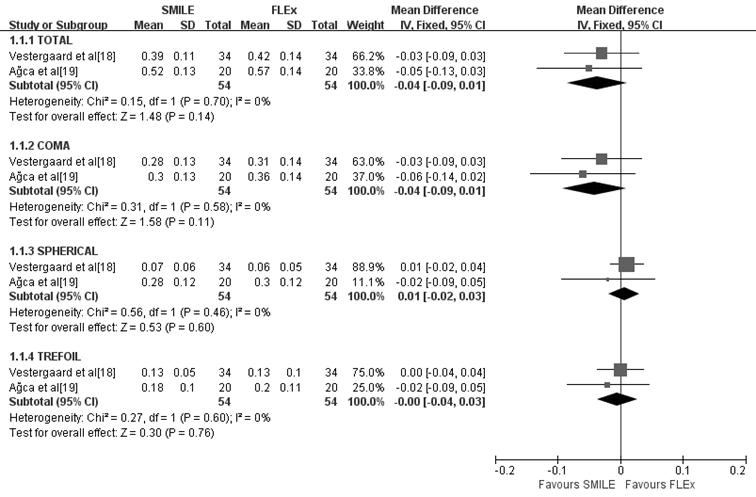
Figure 8 Higher-order aberrations of eyes after SMILE versus FLEx
postoperatively.
Corneal Biomechanical Parameters We analyzed corneal hysteresis (CH)
and corneal resistance factor (CRF) postoperative. Three studies[20-22] were included for
this objective. In terms of CH, there were no significant differences between
the 2 groups (WMD, 0.03; 95%CI, -0.29 to 0.35; P=0.87). For CRF, SMILE presented a better outcome (WMD, 0.15; 95% CI,
-0.24 to 0.54; P=0.45). For the total
result, SMILE presented a better result as well (WMD, 0.08; 95% CI, -0.17 to
0.33; P=0.54 ) (Figure 9).
Figure 9 Corneal biomechnical parameters of eyes after SMILE
versus FLEx postoperatively.
DISCUSSION
The results of efficacy,
safety, and predictability were identical between SMILE and FLEx in our study.
All of the relative data[16-19]
showed no statistical differences. That is to say, either SMILE or FLEx can
best correct myopia and myopic astigmatism. We are also looking forward to the
good consequence, because the techniques are similar during the 2 procedures
except for the difference in the cap (SMILE) and flap (FLEx). It is of clinical
value to compare SMILE with FLEx for the visual quality. SMILE is flapless, but
smaller incision, harder operation. The lenticule may be incomplete during the
extraction. On the contrary, a hinged-flap is created and lifted before
extracting the lenticule in FLEx, so the space is wide enough to operate.
Unfortunately, more corneal nerves are cut off and more patients are concerning
about dry eyes after FLEx. To sum up, considering the identical refraction
result postoperative, we can select either of the 2 methods under different
circumstances to correct myopia and myopic astigmatism.
In teams of HOAs, as is
known to all, corneal refractive surgeries will change HOAs of the cornea[23-25], and that is why
some patients always concern about the flare and the decreased quality of night
vision. Firstly, the pupil diameter will affect HOAs[26]. Under dim light, the pupil will widen and HOAs
will increase. In our study, we only included the data collected under the
pupil diameter equal to 5.0 mm or even larger[18-19] to make the result credible and homogeneous.
Secondly, the smaller optical zone, the higher HOAs[27] .We set the same diameter in the 2
procedures to avoid the diversity. Last but not least, the flap will induce
HOAs. Tran et al[28]
noted that the creation of the LASIK flap alone can induce aberrations. Unlike
LASIK, the femtosecond laser was used to create the flap in FLEx, and no flap
was created in SMILE. In the reported studies, the increase of HOAs was equal
to or less after SMILE or FLEx than other surgeries[23-25]. The common conclusion may be reached due to the
lenticule processing instead of corneal stroma ablating. But SMILE and FLEx are
similar in surgical techniques other than the cap (SMILE) and flap (FLEx). So
we are wondering if SMILE will have lower HOAs than SMILE postoperative. The results
in our study showed no statistically significant differences between the two
groups in total HOAs (P=0.14), coma (P=0.11), spherical (P=0.60) and trefoil (P=0.76)
(Figure 8). Therefore, we
infer that either a femtosecond flap or a subsequent surface incision
does increase HOAs, but the increase does not differ. Considering that only 2 studies[18-19] were taken into
consideration, the result may be limited, and further more data are still
required.
For corneal biomechnical
parameters, we analyzed CH and CRF postoperative. To our knowledge, removal of
corneal tissue can induce a biomechanical weakness of the cornea[21]. Therefore, it is
important to characterize such corneal biomechanical changes. On the one hand,
we can predict the outcomes preoperatively. On the other hand, we can avoid
adverse events postoperatively. In FLEx, a flap is created to access the
stromal lenticule, and the anterior stromal tissue is destroyed. In SMILE, a
subsequent surface incision allows the surgeon to dissect and remove the
lenticule, so less anterior stromal tissue is destroyed. We believe the
anterior stromal tissue is stronger than the posterior, and will have
benificial biomechanic effects[29].
So SMILE may have biomechanical advantages over FLEx in the early times. But we
found no differences since we searched the data for a long time postoperatively
(Figure 9). We have to admit that CH and CRF only reflect parts of corneal
biomechanical structure. Furthermore, although the visual outcomes may be the
same, ocular biomechanics may be different between the two methods. This may be
attributed to the lack of studies with long-term follow-ups. We would like to
accept the fact that the results are limited and more researches comparing
parameters other than CH and CRF should be explored.
A limitation of our review
was the diversity of follow-up time ranging from 3mo to 1y. We even cannot find
the exactly follow-up time of 1 study[21].
So the follow-up time shorter than 1y may be inadequate to determine the final
visual outcomes. Another limitation was the inclusion of RCTs and
non-randomized observational studies, resulting in potential bias. Furthermore,
only 7 studies[16-22] met
our analysis, more studies were required to verify our conclusion.
In conclusion, our present
study found no significant differences in efficacy, safety, predictability HOAs
and corneal biomechanical parameters after SMILE versus FLEx. Considering the
result was limited and inconclusive, further more randomized, prospective
studies with a large sample size, identical intervention parameters and
complete outcome measurements are needed to increase our understanding of the
benefits of SMILE and FLEx.
ACKNOWLEDGEMENTS
Conflicts of Interest: Ma J, None; Cao NJ, None; Xia LK,
None.
REFERENCES [Top]
1 Vestergaard
A, Ivarsen AR, Asp S, Hjortdal JØ. Small-incision lenticule
extraction for moderate to high myopia: predictability,
safety, and patient satisfaction. J Cataract Refract Surg 2012;38(11):2003-2010.
[CrossRef] [PubMed]
2 Holzer MP,
Rabsilber TM, Auffarth GU. Femtosecond laser-assisted corneal flap cuts:
morphology, accuracy, and histopathology. Invest Ophthalmol Vis Sci 2006;47(7):2828-2831.
[CrossRef] [PubMed]
3 Lee JK, Nkyekyer
EW, Chuck RS. Microkeratome complications. Curr Opin Ophthalmol 2009;20(4):260-263.
[CrossRef] [PubMed]
4 Sekundo W,
Gertnere J, Bertelmann T, Solomatin I. One-year refractive results, contrast
sensitivity, high-order aberrations and complications after myopic
small-incision lenticule extraction (ReLEx SMILE). Graefes Arch Clin Exp
Ophthalmol 2014;252(5):837-843. [CrossRef] [PubMed]
5 Kamiya K,Shimizu
K,Igarashi A,Kobashi H. Effect of femtosecond laser setting on visual
performance after small-incision lenticule extraction for myopia. Br J
Ophthalmol 2015;99(10):1381-1387. [CrossRef] [PubMed]
6 Gertnere J,
Solomatin I, Sekundo W. Refractive lenticule extraction (ReLEx flex) and
wavefront-optimized Femto-LASIK: comparison of contrast sensitivity and
high-order aberrations at 1 year. Graefes Arch Clin Exp Ophthalmol 2013;251(5):1437-1442.
[CrossRef] [PubMed]
7 Demirok A, Agca
A, Ozgurhan EB, Bozkurt E, Celik U, Demircan A, Guleryuz NB, Cankaya KI, Yilmaz
OF. Femtosecond lenticule extraction for correction of myopia: a 6 month
follow-up study. Clin Ophthalmol 2013;7:1041-1047. [PMC free article]
[PubMed]
8 Vestergaard A,
Ivarsen A, Asp S, Hjortdal JØ. Femtosecond (FS) laser vision correction
procedure for moderate to high myopia: a prospective study of ReLEx(®) flex and
comparison with a retrospective study of FS-laser in situ keratomileusis. Acta
Ophthalmol 2013;91(4):355-362. [CrossRef] [PubMed]
9 Ang M, Chaurasia
SS, Angunawela RI, Poh R, Riau A, Tan D, Mehta JS. Femtosecond lenticule
extraction (FLEx): clinical results, interface evaluation, and intraocular
pressure variation. Invest Ophthalmol Vis Sci 2012;53(3):1414-1421. [CrossRef] [PubMed]
10 Blum M, Flach
A, Kunert KS, Sekundo W. Five-year results of refractive
lenticule extrction. J Cataract Refract Surg 2014;40(9):1425-1429. [CrossRef] [PubMed]
11 Blum M, Kunert
K, Schröder M, Sekundo W. Femtosecond lenticule extraction for the correction
of myopia: preliminary 6-month results. Graefes Arch Clin Exp Ophthalmol 2010;248(7):1019-1027.
[CrossRef] [PubMed]
12 Xu Y, Yang
Y. Small-incision lenticule extraction for myopia: results
of a 12-month prospective study. Optom Vis Sci 2015;92(1):123-131. [CrossRef] [PubMed]
13 Zhang J, Wang
Y, Wu W, Xu L, Li X, Dou R.
Vector analysis of low to moderate astigmatism with
small incision lenticule extraction (SMILE): results of
a 1-year follow-up. BMC Ophthalmol 2015;15:8. [CrossRef]
14 Sekundo W,
Kunert KS, Blum M. Small incision corneal refractive surgery using the small
incision lenticule extraction (SMILE) procedure for the correction of myopia
andmyopic astigmatism: results of a 6 month prospective study. Br J Ophthalmol 2011;95(3):335-339.
[CrossRef] [PubMed]
15 Shah R, Shah S,
Sengupta S. Results of small incision lenticule extraction: all-in-one
femtosecond laser refractive surgery. J Cataract Refract Surg 2011;37(1):127-137.
[CrossRef] [PubMed]
16 Ang M, Mehta
JS, Chan C, Htoon HM, Koh JC, Tan DT. Refractive lenticule extraction:
transition and comparison of 3 surgical techniques. J Cataract Refract Surg 2014;40(9):1415-1424.
[CrossRef] [PubMed]
17 Kamiya K,
Shimizu K, Igarashi A, Kobashi H. Visual and refractive outcomes of femtosecond
lenticule extraction and small-incision lenticule extraction for myopia. Am J
Ophthalmol 2014;157(1):128-134. [CrossRef] [PubMed]
18 Vestergaard AH,
Grauslund J, Ivarsen AR, Hjortdal JØ. Efficacy, safety, predictability,
contrast sensitivity, and aberrations after femtosecond laser lenticule
extraction. J Cataract Refract Surg 2014;40(3):403-411. [CrossRef] [PubMed]
19 Agca A, Demirok
A, Cankaya Kİ, Yaşa D, Demircan A, Yildirim Y, Ozkaya A, Yilmaz OF. Comparison
of visual acuity and higher-order aberrations after femtosecond lenticule
extraction and small-incision lenticule extraction. Cont Lens Anterior Eye 2014;37(4):292-296.
[CrossRef] [PubMed]
20 Kamiya K,
Shimizu K, Igarashi A, Kobashi H, Sato N, Ishii R. Intraindividual comparison
of changes in corneal biomechanical parameters after femtosecond lenticule
extraction and small-incision lenticule extraction. J Cataract Refract Surg 2014;40(6):963-970.
[CrossRef] [PubMed]
21 Pedersen IB,
Bak-Nielsen S, Vestergaard AH, Ivarsen A, Hjortdal J. Corneal biomechanical
properties after LASIK, ReLEx flex, and ReLEx smile by Scheimpflug-based
dynamic tonometry. Graefes Arch Clin Exp Ophthalmol 2014;252(8):1329-1335. [CrossRef] [PubMed]
22 Vestergaard AH,
Grauslund J, Ivarsen AR, Hjortdal JØ. Central corneal sublayer pachymetry and
biomechanical properties after refractive femtosecond lenticule extraction. J
Refract Surg 2014;30(2):102-108. [CrossRef] [PubMed]
23 Gyldenkerne
A, Ivarsen A, Hjortdal JØ. Comparison of corneal shape changes
and aberrations induced By FS-LASIK and SMILE for myopia. J Refract
Surg 2015;31(4):223-229. [CrossRef]
24 Kamiya K,
Shimizu K, Igarashi A, Kobashi H, Komatsu M. Comparison of visual acuity,
higher-order aberrations and corneal asphericity after refractive lenticule
extraction and wavefront-guided laser-assisted in situ keratomileusis for
myopia. Br J Ophthalmol 2013;97(8):968-975. [CrossRef] [PubMed]
25 Gertnere J,
Solomatin I, Sekundo W. Refractive lenticule extraction (ReLEx flex) and
wavefront-optimized femto-LASIK: comparison of contrast sensitivity and
high-order aberrations at 1 year. Graefes Arch Clin Exp Ophthalmol 2013;251(5):1437-1442.
[CrossRef] [PubMed]
26 Oshika T,
Tokunaga T, Samejima T, Miyata K, Kawana K, Kaji Y. Influence of pupil diameter
on the relation between ocular higher-order aberration and contrast sensitivity
after laser in situ keratomileusis. Invest Ophthalmol Vis Sci 2006;47(4):1334-1338.
[CrossRef] [PubMed]
27 Cheng ZY, Chu
RY, Zhou XT. Influence of diameter of optical zone ablation on LASIK-induced
higher order optical aberrations in myopia. Zhonghua Yan Ke Za Zhi 2006;42(9):772-776.
[PubMed]
28 Tran DB,
Sarayba MA, Bor Z, Garufis C, Duh YJ, Soltes CR, Juhasz T, Kurtz RM. Randomized
prospective clinical study comparing induced aberrations with IntraLase and
Hansatome flap creation in fellow eyes. J Cataract Refract Surg 2005;31(1):97-105.
[CrossRef] [PubMed]
29 Agca A, Ozgurhan EB, Demirok
A, Bozkurt E, Celik U, Ozkaya A, Cankaya I, Yilmaz OF.
Comparison of corneal hysteresis and corneal resistance factor after small incision lenticule extraction andfemtosecond laser-assisted LASIK:a prospective fellow eye study.
Cont Lens Anterior Eye 2014;37(2):77-80. [CrossRef] [PubMed]
[Top]