·Meta-Analysis··Current
Issue· ·Achieve· ·Search
Articles· ·Online Submission· ·About IJO·
Radial
optic neurotomy in treating central retinal vein occlusion: a Meta-analysis
Zhen-Na Chen,
Yan Shao, Xiao-Rong Li
Eye Institute & School of Optometry and
Ophthalmology, Tianjin Medical University Eye Hospital, Tianjin 300384, China
Correspondence
to: Xiao-Rong Li.
Eye Institute & School of Optometry and Ophthalmology, Tianjin Medical
University Eye Hospital, No. 251, Fukang Road, Nankai District, Tianjin 300384,
China. xiaorli@163.com
Received: 2015-07-06 Accepted: 2016-02-13
Abstract
AIM: To
assess the feasibility of radial optic neurotomy (RON) in central retinal vein
occlusion (CRVO) treatment with a Meta-analysis.
METHODS:
Electronic databases were searched for
comprehensive articles that compared efficacy of RON with that of other
treatments in CRVO. Study quality was assessed and risk ratio (RR) and 95% confidence interval (CI) with
fix- or random-effects model were calculated according to the heterogeneity.
RESULTS: A
total of 200 eyes from 5 studies were included. The results indicated that no
significant differences were found between groups with and without RON in
improvement of visual acuity (VA) at 6mo follow-up (pooled RR 0.51,
95%CI 0.22 to 1.18, P=0.117) while
improvement of VA showed significantly favourable in patients receiving RON
treatment at 12mo follow-up (pooled RR 2.27, 95%CI 1.31 to 3.95, P=0.004). For complications, RON
treatment was more effective in reducing neovascular glaucoma (pooled RR 0.45,
95%CI 0.21 to 0.97, P=0.042) but was
comparable in retinal detachment (pooled RR 2.41,
95%CI 0.51 to 11.39, P=0.267) and vitreous
hemorrhage (pooled RR 0.91, 95%CI 0.33 to 2.46, P=0.847).
CONCLUSION:
Compared with some certain treatment modalities, RON might offer better VA at
12mo and decrease the rate of neovascular glaucoma without changing the rate of
retinal detachment and vitreous hemorrhage. Further studies are required
considering the limitation of the research.
KEYWORDS: radial
optic neurotomy; central retinal vein occlusion; Meta-analysis
DOI:10.18240/ijo.2016.06.19
Citation: Chen ZN, Shao Y, Li XR. Radial optic neurotomy in
treating central retinal vein occlusion: a Meta-analysis. Int J Ophthalmol 2016;9(6):898-903
INTRODUCTION
Retinal
vein occlusion (RVO) is an important cause of vision loss and indeed a common
retinal vascular disease secondary to diabetic retinopathy[1-2]. Central
retinal vein occlusion (CRVO), which can block all venous outflow and result in
severe complications, counts the most important in the realm of RVO. Treatment
modalities of CRVO include close observation and other active treatments such
as laser photocoagulation, intravitreal injection of anti-inflammatory agents
and surgical approaches[2-3]. While controversies concerning
the standard of care have remained for many years since no intervention had
been proved to be absolutely effective and safe. Radial optic neurotomy (RON),
which is based on the theory hypothesized by Opremcak
et al[4] that
a “compartment syndrome” occurs in CRVO with neurovascular compression within
the optic nerve at the level of lamina cribrosa, arises as an exciting
advancement in recent years. It is believed to exert its function by
decompressing central retinal artery and vein and alleviating the potential
syndrome finally. Given the outcomes of patients with CRVO who underwent RON as
a method of treatment, RON was considered as a possible treatment of CRVO[4-7].
However,
despite the previous favourable evidence, concerns were raised since part of
subsequent studies didn’t support the significance of RON in the treatment of
CRVO, making RON treatment equivocal[8-11].
Besides that, few Meta-analysis was found in this field. We therefore conducted
the Meta-analysis of the available evidence on efficacy of RON compared with
other treatments in treating CRVO.
MATERIALS
AND METHODS
Search
Strategy Medline, PubMed, Embase, Cochrane Library
and Chinese database-Wanfang Database, Vip Database, China National Knowledge Internet
were searched form inception until January 1, 2015. Language was restricted to
English. We used mesh terms as “central retinal vein occlusion”, “radial optic
neurotomy” and abbreviation of the
keywords “CRVO”, “RON”. Additionally, the references lists of the identified
articles were examined for extra eligible studies.
Inclusion Criteria The goal of our study was to
determine the efficacy in treating CRVO. Therefore, articles were considered
eligible if they fulfilled the following criteria: 1) type of study:
comparative studies including randomized controlled trials (RCTs), prospective
and retrospective studies; 2) participates: patients diagnosed with CRVO with
VA ≥0.3 logMAR (0.5 Snellen or less);3) interventions and comparison:
RON compared with other treatment; 4) outcomes: at least the outcome of visual
acuity (VA) were included; 5) duration: the history of CRVO was not longer than
12mo. Exclusion criteria included animal studies, trial protocols, secondary
studies and duplicate publications.
Data Extraction Data extraction
was performed by two independent reviewers (Chen ZN and Shao Y). Any disagreement
was resolved by discussion and consensus during the extraction. Data extraction
included: 1) general characteristics: first author, year and site of
publication and number of eyes included in the study; 2) subjects: patient age,
sex, disease duration and follow-up; 3) methodology: type and quality of study;
4) intervention (RON) and control group; 5) outcomes: outcome measurements
include VA, proportion of eyes with a significant improvement. Complications
such as retinal detachment, neovascular glaucoma, and vitreous hemorrhage were
also included.
Assessment
of Study Quality The Downs and Black quality assessment
method[12] and the
Newcastle-Ottawa scale (NOS)[13]
were used to assess the study quality also by two reviewers (Chen ZN and Shao Y)
independently. The Downs and Black score was employed to evaluate RCTs and
non-RCTs, while NOS only for non-RCT. The Downs and Black score
system consisted of 27 questions, making total achievable scores from 0 to 32.
These questions evaluated reporting, external validity, internal validity (bias
and confounding) and power. NOS, which was only used to evaluate non-RCTs,
included selection, comparability and exposure. Nine scores were the maximum
score and studies ≥6 scores were considered to be with relatively higher
quality.
Statistical
Analysis All statistical analyses were performed
with State version 12.0. The primary outcome was proportion of eyes with a
significant improvement defined as ≥3 lines of logMAR scale or any other
methods corresponding to it. Improvement from light perception (LP) to hand
movement (HM) or from HM to finger count (FC) were also included. The secondary
outcomes were incidence of adverse event, such as retinal detachment,
neovascular glaucoma and vitreous hemorrhage.
In
the Meta-analysis, pooled risk ratio (RR) and 95% confidence intervals (CI)
were measured. Statistically heterogeneity among studies was evaluated with an I2 test. A fixed-effect (Mantel-Haeszel)
statistical model was employed when no heterogeneity was reported (P>0.10, I2<70%), otherwise the DerSimonian-Lairel random
effects model was undertaken after exploring the cause of heterogeneity. We
considered P<0.05 as statistically
significant.
RESULTS
To
explore the source of heterogeneity, we had also adopted a subgroup analysis.
Potential publication bias was estimated with a funnel plot by examining
visually the asymmetry and Egger’s linear regression method.
Literature
Search The number of studies identified through
database search was 202. After checking the titles and abstracts of the
articles, we reviewed 20 full texts and finally 5 were included in the Meta-analysis.
Five articles were met by 2 RCTs[14-15], 2 prospective trials[16-17]
and 1 retrospective ones[18] (Figure 1).
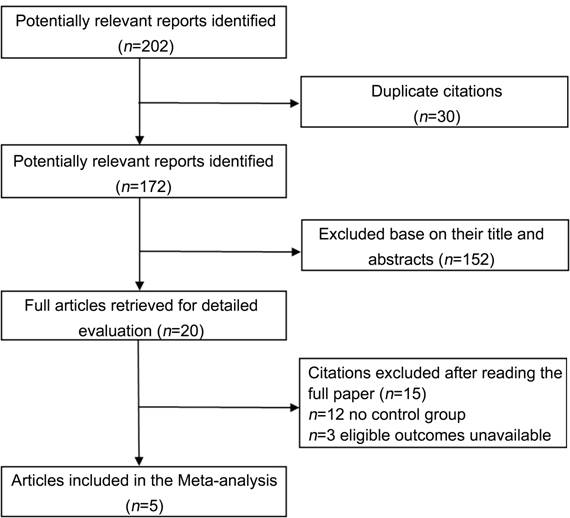
Figure 1 Flow diagram of trial selection.
Study
Characteristics Characteristics
of articles included in Meta-analysis are presented in Tables 1 and 2. Geographic
distributions were sporadic: 2 in Asia and 3 in Europe. Of the 5 eligible
studies, intervention was RON surgery and controls were other available
treatments. Three studies compared RON with intravenous injection of tissue
plasminogen activator (tPA), retinal endovascular surgery (REVS) and panretinal
photocoagulation (PRP) respectively[15-16,18]. One study focused on the
comparison with natural history[17]. Intravitreal triamcinolone (IVT)
and natural history as controls were investigated in one study alone[14].
Table 1 Characteristics of articles included in the Meta-analysis n=5
|
First author, year |
Country |
No.of eyes (RON: control) |
Mean age |
Sex (male:female) |
Disease duration |
Control group |
Follow-up (mo) |
|||
|
RON |
Control |
|
Control |
RON |
control |
|||||
|
Austria |
63 (38:25) |
NA |
NA |
NA |
NA |
<12mo |
<12mo |
IVT |
12 |
|
|
Aggermann T, 2012[14]b |
Austria |
58 (38:20) |
NA |
NA |
NA |
NA |
<12mo |
<12mo |
Placobo |
12 |
|
Crama N, 2010[16] |
France |
6 (3:3) |
79 (58-85) |
45 (41-58) |
2:1 |
3:0 |
14 (4-18)wk |
24 (13-36)wk |
REVS |
6 |
|
Yamamoto T, 2009[15] |
Japan |
21 (11:10) |
67.0±6.5 |
63.3±7.2 |
6:5 |
7:3 |
14.7±8.7wk |
10.6±6.4wk |
tPA |
6 and 12 |
|
Callizo J, 2009[17] |
Germany |
63 (28:35) |
67.4±9.1 |
65.5±14.5 |
16:12 |
19:16 |
≤3mo |
≤3mo |
Natural
history |
12 |
|
Kim TW, 2005[18] |
Korea |
27 (11:16) |
52 (23-69) |
55 (23-77) |
5:6 |
5:11 |
2.13 (0.5-5)mo |
2.25 (0.5-6)mo |
PRP |
6 and 12 |
NA:
Not available; RON: Radial optic neurotomy; REVS: Retinal endovascular surgery;
tPA: tissue plasminogen activato; PRP: Panretinal photocoagulation. IVT:
Intravitreal triamcinolone. aA control group as a single dose of 4
mg IVT; bA control group who received a sham injection (placebo).
Table 2 Characteristics of articles
included in the Meta-analysis
n=5
|
First author,
year |
VA |
|
Complications (RON/control) |
||||
|
Preoperative (RON/Control) |
Outcome (RON/Control) |
RON |
Control |
Retinal
detachment |
Neovascular
glaucoma |
Vitreous
hemorrhage |
|
|
Aggermann T, 2012[14]a |
1.46 (0.9-1.36)/1.02
(0.75-2) |
0.75 (0.46-1.22)/0.86
(0.51-1.78) |
18/38 |
2/25 |
1:38/0:25 |
2:38/3:25 |
1:38/0:25 |
|
Aggermann T, 2012[14]b |
1.46 (0.9-1.36)/1.02
(0.9-1.36) |
0.75 (0.46-1.22)/1.02
(0.85-3) |
18/38 |
5/20 |
1:38/0:20 |
2:38/3:20 |
1:38/2:20 |
|
Crama N, 2010[16] |
HM,14,14/17,50,35d |
CF,CF,5/62,70,78d |
1/3 |
3/3 |
NA |
1:3/0:3 |
NA |
|
Yamamoto T, 2009[15] |
(16/200±20/51)/(10/200±20/69) |
(20/182±20/43)/(20/154±20/65) (20/167±20/43)/(20/200±20/111) |
2/11 5/11 |
6/10 5/10 |
1:11/0:10 |
2:11/4:10 |
2:11/1:10 |
|
Callizo J, 2009[17] |
0.10±0.087/0.23±0.18 |
0.23±0.20/0.28±0.19 |
NA |
NA |
1:28/0:35 |
1:28/4:35 |
1:28/3:35 |
|
Kim TW, 2005[18] |
(1.365±0.78)/(1.104±0.77) |
NA |
1/11 1/11 |
0/16 0/16 |
NA |
0:11/2:16 |
1:11/0:16 |
NA: Not
available; HM: Hand movement; FC: Finger count. aA control group as
a single dose of 4 mg IVT; bA control group who received a sham
injection (placebo); cProportion of eyes with a significantly
improvement defined as an improvement of 3 lines of logMAR scale, a 3-line
change on the ETDRS chart, improvement from LP to HM or from HM to FC; dDescribed
in ETDRS.
Quality
Assessment For the Downs and Black score, all
studies were assessed from 5 different aspects and no study reached the limit
of the maximum of 24 points. The lowest score was 17 points with only 6
patients included. Scores were on average 19.6 points (SD=2.7). Only 2 studies[14-15] made attempts to blind the subjects and
assessor by means of a sealed-envelope system. Of 3 non-RCTs assessed by the
NOS, only one was with high quality of 6 scores (Table 3).
Table 3 Evaluation
of the articles included in the Meta-analysis
|
First author, year |
Study design |
Downs and
Black sore |
NOS |
|||
|
Selection |
Comparability |
Expose/outcome |
Total Score |
|||
|
RCT |
23 |
- |
- |
- |
- |
|
|
Crama
N, 2010[16] |
Prospective |
17 |
3 |
1 |
1 |
5 |
|
Yamamoto
T, 2009[15] |
RCT |
22 |
- |
- |
- |
- |
|
Callizo
J, 2009[17] |
Prospective |
18 |
4 |
0 |
1 |
5 |
|
Kim
TW, 2005[18] |
Retrospective |
18 |
3 |
1 |
2 |
6 |
-:
No data provided; RCT: Randomized-controlled trials; NOS: Newcastle-Ottawa
Scale. aThe Study quality is evaluated by Downs and NOS. Downs and
Black Score for both RCT and non-RCT while NOS for only non-RCT.
Postoperative
Visual Acuity Improvement
To evaluate the efficacy of RON, we used proportion of eyes with a
significant improvement in RON and control group at 6 and 12mo follow-up. We
included 3 articles[15-16,18] at 6mo follow-up (Figure 2).
Since no significant heterogeneity (P
=0.300, I 2=16.9%) was
detected, we combined the results using fixed-effect model. The result
demonstrated that dramatic postoperative VA was not significantly different at
6mo follow-up in two groups (pooled RR 0.51, 95%CI 0.22 to 1.18, P =0.117). While as is shown in Figure 3
which included 4 comparisons[14-15,18], the result demonstrated
that compared to those receiving other treatments, patients in RON group had
significant better postoperative VA improvement at 12mo follow-up
(pooled RR 2.27, 95%CI 1.31 to 3.95, P
=0.004). Fixed-effect model was employed for the Meta-analysis (P =0.101, I 2=51.8%).

Figure 2 Meta-analysis of postoperative
VA at 6mo follow-up.

Figure 3 Meta-analysis of postoperative
VA at 12mo follow-up.
Complications To evaluate the safety of RON, we
also made Meta-analysis for complications between compared groups in each
study. We focused our attention on retinal detachment, neovascular glaucoma and
vitreous hemorrhage.
Retinal
Detachment Retinal detachment was mentioned in
three articles[14-15,17]. There were 4 (3.5%)
events of 115 patients in RON group while no retinal detachment was observed in
control group. No signigicant heterogeneity (P =0.985, I 2=0)
was found in this analysis. Fixed-effect model was employed, showing that RON
treatment was not associated with retinal detachment (pooled RR 2.41, 95%CI
0.51 to 11.39, P =0.985) (Figure
4).

Figure 4 Meta-analysis of retinal
detachment.
Neovascular
Glaucoma Five articles[14-18] were
included in analysing the incidence of neovascular glaucoma. Eight (6.20%) of
129 CRVO patients in receiving RON experienced the complication compared with
16 (14.7%) of 109 patients in receiving control. Also no significant
heterogeneity (P =0.856, I 2=0.0%) was found and
fixed-effect model was used. We found that the incidence of neovascular
glaucoma in RON group was significantly less than that in control group
(pooled RR 0.45, 95%CI 0.21 to 0.97, P
=0.042) (Figure 5).
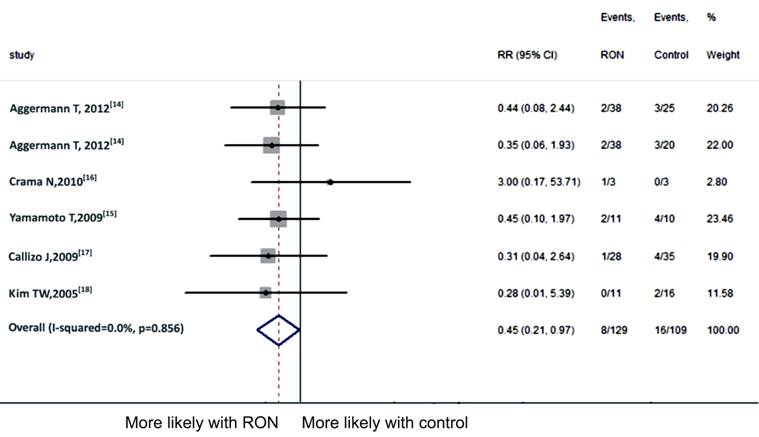
Figure 5 Meta-analysis of neovascular
glaucoma.
Vitreous Hemorrhage As to vitreous hemorrhage,
4 articles[14-15,17-18] were included in the Meta-analysis. The
complication ocurred in 6 (4.8%) of 126 patients in RON group as compared to 6 (5.7%)
of 106 patients in the control. Since no significant heterogeneity (P =0.540, I 2=0) was detected, we
employed the fixed-effect model and found that RON was not associated with
vitreous hemorrhage (pooled RR 0.91, 95%CI 0.33 to 2.46, P =0.847) (Figure 6).

Figure 6 Meta-analysis of vitreous
hemorrhage.
Publication
Bias Publication bias was not calculated
considering that just six studies were identified, making the calculation less
informative .
DISCUSSION
This Meta-analysis
compared RON with other treatment modalities in treating CRVO. Pooled data from
two RCTs, two prospective and one retrospective study demonstrated that RON
therapy was not associated with significant improvement on postoperative VA at
6mo follow-up and complications like retinal detachment and vitreous hemorrhage
as compared with control. While for VA at 12mo follow-up and reduction of
neovascular glaucoma, RON was shown to have better outcomes.
Since
natural course of CRVO is always disappointing and no treatment modalities have
been clarified to show certain effect, new therapy with high expectation is
needed. When Opremcak et al[4] first proposed
the use of RON in treating CRVO, RON has drawn more and more attention and also
been compared with other treatments in various means. However, we found that
conclusions from different studies were not consistent.
Although,
we tried to conduct a thorough and convinced Meta-analysis from the existing
literatures, there were still limitations that might reduce the reliability of
evaluation. Firstly, although we searched in multiple databases, only published
literatures were included in the Meta-analysis, which might cause publication
bias. Secondly, the overall quality of included studies was not high. Given the
numbers of articles comparing RON with other treatments were limited, criteria
of inclusion was set regardless of the type of articles, type of CRVO and the
number of patients. Considering that control group was consisted of different
treatment modalities including observation, IVT, REVS, tPA and PRP and only one
article was included in each comparison, we regarded the treatments as a whole
rather than that in subgroups, which made the conclusion quite conservative.
Thirdly, RON was always performed with pars plana vitrectomy (PPV) technically.
Whether unspecific effects of the vitrectomy itself, like reduced oxygen
consumption and removal of mediators achieved the beneficial effect of PPV was
obscure[14,18-20] and the mechanisms behind this effect
objectively cannot be identified.
Despite
these limitations listed above, our Meta-analysis showed that RON might serve
as a useful tool in treating CRVO when other treatment modalities are not
available. Further studies assessing efficacy and safety of RON are needed by
selecting studies with large scale and patients with more matching factors.
Furthermore, whether visual improvement is attributed to vitrectomy procedure
itself is still a question. There is therefore an urgent need
for further studies concerning prospective, randomized clinical trials to rest
the debate over the efficacy of RON and PPV itself in the treatment of CRVO.
ACKNOWLEDGEMENTS
Foundation:
Supported by National Science Foundation of Tianjin,
China (No. 15JCQNJ11400).
Conflicts
of Interest: Chen ZN, None; Shao Y,
None; Li XR, None.
REFERENCES
1 Natural history and clinical management of central retinal vein
occlusion. Arch Ophthalmol
1997;115(4):486-491. [CrossRef] [PubMed]
2 MacDonald D. The ABCs of RVO: a review of retinal venous
occlusion. Clin Exp Optom 2014;97(4):
311-323. [PubMed]
3 Berker N, Batman C. Surgical treatment of central retinal vein
occlusion. Acta Ophthalmol
2008;86(3):245-252. [CrossRef] [PubMed]
4 Opremcak EM, Bruce RA, Lomeo MD, Ridenour CD, Letson AD, Rehmar
AJ. Radial optic neurotomy for central retinal vein occlusion: a retrospective
pilot study of 11 consecutive cases. Retina
2001;21(5):408-415. [CrossRef]
5 Stoffelns BM, Kramann C, Hoffmann E. Radial optic neurotomy
(RON) for central retinal vein occlusion. Klin
Monbl Augenheilkd 2007;224(4):282-287. [CrossRef] [PubMed]
6 Hasselbach H, Thale A, Bunse A, Paulsen F, Roider J.
Ultrastructural analysis of the lamina cribrosa after radial optic neurotomy. Ann Anat 2009;191(3):267-272. [CrossRef] [PubMed]
7 Verdaguer Agusti P, Nadal Reus J. Long-term clinical outcome of
radial optic neurotomy. Arch Soc Esp
Oftalmol 2010;85(11):370-375. [CrossRef]
8 Beck AP, Ryan EA, Lou PL, Kroll AJ. Controversies regarding
radial optic neurotomy for central retinal vein occlusion. Int Ophthalmol Clin 2005;45(4):153-161. [CrossRef]
9 Ramezani AR. Radial optic neurotomy for central retinal vein
occlusion. J Ophthalmic Vis Res
2009;4(2): 115-121. [PMC free article]
[PubMed]
10 Arevalo JF, Garcia RA, Arevalo JF, Garcia RA, Wu L, Rodriguez
FJ, Dalma-Weiszhausz J, Quiroz-Mercado H, Morales-Canton V, Roca JA, Berrocal
MH, Graue-Wiechers F, Robledo V, Pan-American Collaborative Retina Study Group.
Radial optic neurotomy for central retinal vein occlusion: results of the
Pan-American Collaborative Retina Study Group (PACORES). Retina 2008;28(8):1044-1052. [CrossRef] [PubMed]
11 Hayreh SS, Zimmerman MB, Podhajsky PA. Retinal vein occlusion
and the optic disk. Retina
2012;32(10):2108-2118. [CrossRef]
[PubMed]
12 Downs SH, Black N. The feasibility of creating a checklist for
the assessment of the methodological quality both of randomised and
non-randomised studies of health care interventions. J Epidemiol Community Health 1998;52(6):377-384. [CrossRef] [PubMed] [PMC free article]
13 Stang A. Critical evaluation of the Newcastle-Ottawa scale for
the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25(9):603-605. [CrossRef] [PubMed]
14 Aggermann T, Brunner S, Krebs I, Haas P, Womastek I, Brannath
W, Binder S; Rovo Study Group. A prospective, randomised, multicenter trial for
surgical treatment of central retinal vein occlusion: results of the radial
optic neurotomy for central vein occlusion (ROVO) study group. Graefes Arch Clin Exp Ophthalmol
2013;251(4):1065-1072. [CrossRef]
[PubMed]
15 Yamamoto T, Kamei M, Sakaguchi H, Oshima Y, Ikuno Y, Gomi F,
Ohji M, Tano Y. Comparison of surgical treatments for central retinal vein
occlusion; RON vs cannulation of tissue plasminogen activator into the retinal
vein. Retina 2009;29(8):1167-1174. [CrossRef] [PubMed]
16 Crama N, Gualino V, Restori M, Charteris DG. Central retinal
vessel blood flow after surgical treatment for central retinal vein occlusion. Retina 2010;30(10):1692-1697. [CrossRef] [PubMed]
17 Callizo J, Kroll P, Mennel S, Schmidt JC, Meyer CH. Radial
optic neurotomy for central retinal vein occlusion: long-term retinal perfusion
outcome. Ophthalmologica
2009;223(5):313-319. [CrossRef]
[PubMed]
18 Kim TW, Lee SJ, Kim SD. Comparative evaluation of radial optic
neurotomy and panretinal photocoagulation in the management of central retinal
vein occlusion. Korean J Ophthalmol
2005;19(4): 269-274. [CrossRef]
[PubMed]
19 Skevas C, Wagenfeld L, Feucht M, Galambos P, Richard G, Zeitz
O. Radial optic neurotomy in central retinal vein occlusion does not influence
ocular hemodynamics. Ophthalmologica 2011;225(1):41-46. [CrossRef] [PubMed]
20 McAllister IL. Central retinal vein occlusion: a review. Clin Experiment Ophthalmol
2012;40(1):48-58. [CrossRef]
[PubMed]
[Top]