·Opinion··Current Issue· ·Achieve· ·Search Articles· ·Online Submission· ·About IJO·
Intraocular
lens exchange- removing the optic intact
Matthew
Hao Lee1, Diane Lesley Webster2
1Department of Ophthalmology, Alfred Hospital, Melbourne, VIC 3004,
Australia
2Royal Victorian Eye and Ear Hospital, East
Melbourne, VIC 3002, Australia
Correspondence
to: Matthew Hao Lee. Alfred Hospital, 55 Commercial Road,
Melbourne, VIC 3004, Australia. matthew.leehao@icloud.com
Received: 2015-01-31
Accepted: 2015-07-09
Abstract
Current practice for intraocular lens (IOL)
exchange is to cut the optic of the posterior chamber intraocular lens (PCIOL)
prior to removing it. Great care must be taken during this maneuver to avoid a
posterior capsular tear. Removing the haptics from the fibrosed capsule can
also be hazardous, as it may result in zonular stress and dehiscence. A technique is described for performing
foldable (one-piece acrylic) IOL removal without cutting the optic. Careful
visco-dissection of the haptics with a low viscosity ophthalmic viscosurgical
device (OVD) in the fibrosed peripheral capsular tunnel avoids
zonular or capsular stress. Internal wound enlargement permits foldable IOL
removal in one piece, whilst preserving a self-sealing sutureless corneal
wound. This technique may
enhance the safety and efficacy of foldable IOL exchange.
KEYWORDS: intraocular lens exchange; viscodissection; posterior capsular tear
DOI:10.18240/ijo.2016.06.23
Citation: Lee MH, Webster DL. Intraocular
lens exchange- removing the optic intact. Int
J Ophthalmol 2016;9(6):925-928
INTRODUCTION
Intraocular lens (IOL) implantation, an
essential part of modern phacoemulsification surgery, is a commonly performed
and extremely successful procedure. However, complications relating to the IOL
occasionally arise and necessitate the need for an IOL exchange.
Incorrect IOL power is the most common
indication for IOL exchange[1-2] and is a common cause of malpractice
claims[3]. This is partly related to increasing
patient expectations and a demand for refractive results near emmetropia and
independence from spectacles[1,4-5]. Another rising indication is intolerance
of multifocal IOLs especially due to dysphotopsia or photic phenomena[4-6].
Similarly, the “glistenings” of the
commonly used Acrysof® IOLs results
in patient dissatisfaction[7]. Other well-known indications also include
lens decentration/dislocation[2,8-10] and optic opacification [2,9,11-12].
Many effective techniques for IOL exchange
exist[13-17], but the majority involve cutting the
optic to remove the IOL which risks damaging the posterior capsule with the
intraocular scissors. Lee et al[18], Theoulakis et al[19],
Kubaloglu et al[20]
and Dagres et al[21]
reported a posterior capsule rupture rate of 8.6%, 3.6%, 12% and 9%
respectively. Zonular dehiscence is also a common complication due to the fact that
separating the haptics from the fibrosed capsule is technically challenging[21-22]. When it occurs, additional procedures
are required such as removal of the prolapsed vitreous, trans-scleral fixation
of the IOL or unplanned anterior chamber IOL implantation[18].
We describe a technique that can lower the
risk of both zonular dehiscence and posterior capsule rupture. We employ
careful viscodissection of the haptics in the fibrosed peripheral capsular
tunnel which effectively frees it up and can subsequently be rotated out. We
also avoid the potentially dangerous maneuver of cutting the optic based on the
principle that “if the IOL can fold in, it will fold out”, facilitated by
internal wound enlargement which enables IOL removal in one piece. This simultaneously
preserves the benefits of a self-sealing sutureless corneal wound. This technique also preserves the
integrity of the capsular bag so that a foldable IOL can be replaced into the
capsule bag.
SURGICAL
TECHNIQUE
A temporal clear corneal two step sealing
incision is made at the limbus with a 2.75 mm keratome. A cohesive low-viscosity ophthalmic viscosurgical device (OVD) such as Provisc® is injected into the anterior chamber. A
1.2
mm corneal side port is made
45 degrees from the main incision. A sinskey hook is used to create a passage
between the anterior capsular flap and IOL (Figure 1A). The low-viscosity OVD
is inserted on a Rycroft cannula through the passage and the optic of the IOL
is visco-dissected from the anterior capsule. The OVD is used to viscodissect
the haptics free in their fibrosed peripheral capsular tunnel. The IOL is
rotated carefully out of the capsular bag and into the anterior chamber (Figure
1B, 1C). The 2.75 mm incision is
internally enlarged 0.5 mm
approximately each side so that the internal diameter is approximately 3.75 mm and the external diameter remains at
2.75
mm to maintain self-sealing
wound integrity (Figure 1D). The haptics are checked to make sure they are not
trapped under the corneal shelves of the main incision. Two Kelman McPhearson
forceps are needed to remove the IOL in one piece under OVD protection of the
corneal endothelium using Arshninof’s soft-shell technique (Figure 1E). The
optic is grasped with the Kelman forcep in the right hand. The IOL is then gently
and firmly brought to the corneal wound. The centre of the optic is regrasped
with the left hand Kelman forcep; the right hand Kelman then regrasps the optic
and the IOL is gently removed from the eye (Figure 1F). It is important not to
grasp the haptic alone as it may then break off. Following IOL removal, the capsular bag is refilled
with OVD. The replacement IOL is injected through the main incision and into
the intact capsular bag (Figure 1G). The replacement IOL is centred and the OVD
is subsequently removed. The corneal wounds are sealed with balanced salt
solution (BSS) for stromal hydration (Figure 1H). A corneal suture is placed if
there is demonstrated wound leak if there has been any stretching of the
corneal wound by the manouvers. Cefazolin 1 mg in 0.1 mL is then injected
through the side port into the anterior chamber for endophthalmitis
prophylaxis.
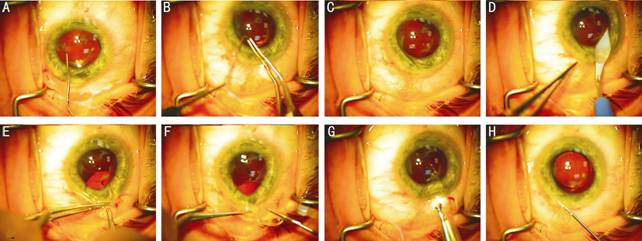
Figure
1 Steps involved in the foldable (one-piece acrylic) IOL exchange
technique without cutting the optic A: Sinskey hook creates a passage between anterior
capsular flap and the IOL; B:
Circumferential rotation of IOL under cohesive OVD; C: Circumferential rotation of IOL with resultant
freeing of haptics; D: Internal
enlargement of corneal wound to approximately 3.75 mm but keeping the external diameter of 2.75 mm so it is likely to self seal without
sutures; E: Foldable IOL
removed from the eye under soft-shell technique; F: Hand over hand
technique with Kelman forceps so one hand is always holding the optic (as
opposed to the haptic) with forceps; G: Injection of alternative foldable IOL into capsular bag; H: Hydration
of self-sealing wound with BSS.
DISCUSSION
Cataract surgery and IOL implantation has
seen a rapid evolution over the past few years. While surgical improvement of
cataract surgery has greatly reduced the incidence of IOL exchange in the past
decade[1-2,9],
complications such as IOL dislocation[23-25], incorrect IOL power[4-6] and IOL opacification[12,26-29] remain common indications for the exchange
procedure. As more patients with higher visual expectations receive refractive
lenses such as multifocal or toric lenses, the request for IOL exchange due to
patient dissatisfaction is on the rise; the reasons are predominantly due to
intrinsic weaknesses associated with these lenses such as unsatisfactory visual
acuity at specific working distances, increased dysphotopsia compared to
monofocal IOLs, decreased contrast sensitivity, and increased intraocular
straylight[8,30-33]. In uncommon situations where a reason for
refractive surprise cannot be identified, a mislabeled IOL ought to be
considered as a potential cause[34].
There are numerous IOL exchange techniques
which involve cutting the optic or optic/haptic junction. These include optic bisection and
partial optic bisection[13], trisection[15], crisscross lensotomy[16], optic-only removal[18], piggybacking technique[35], and the IOL scaffold technique[17,36-37].
Whilst effective, the risk of posterior capsular rupture is still present-Lee et al[18] optic-only removal technique was reported
to have an 8.7% posterior capsule rupture rate when the optic was being divided
with Vannas scissors. He also acknowledged that attention is required when
cutting the haptic-optic junction to avoid damaging intraocular structures.
Kubaloglu et al[20] technique, also involving division of the optic, had a
12% posterior capsule rupture rate. Another reason disfavoring the cutting of
the optic is that one must either purchase special and often expensive
micro-instruments or enlarge the incision to permit entry of the scissors[38]. For these reasons, we prefer avoiding the
need to cut the optic altogether and feel that folding the IOL is a safer
option.
Based on the principle “if the IOL folds
in, it will fold out”, the foldable IOL will fold out with minimal trauma to
the corneal endothelium if it is protected by the OVD and if the internal
opening of the wound is enlarged to 3.75 mm. Henderson and Yang[38], who used a similar technique of “sandwiching” the IOL between the dispersive OVD, found that there
was no additional loss of endothelial cells or corneal edema after two months
in their first patient and after one year in their second patient. Our use of
internal wound enlargement further improves on Henderson’s technique; he states
that if the original cataract surgery incision is <2.75 mm, the wound needs to be widened. However,
we found that internal wound enlargement to approximately 3.75 mm (but keeping the external diameter of
2.75
mm) permits extraction of the
IOL yet negates the need for external wound enlargement, hence preserving the
benefits of a small self-sealing sutureless wound. These include a lower risk
of surgically induced astigmatism, postoperative inflammation and
endophthalmitis[39]. There was no significant surgically induced
astigmatism in our cases and corneas remained clear attesting to a healthy
endothelial cell count with no significant losses due to the technique.
Another prominent feature of our technique
is careful hydrodissection of the haptics out of its fibrosed tunnel with a
cohesive OVD (Provisc®) rather than
a dispersive OVD (Viscoat®). If this
is gently injected within the fibrosed tunnel, the haptics are easily freed up
and can be rotated out. This step greatly decreases the risk of zonular
dehiscence. Many surgeons have found separating the haptics from the fibrosed
capsule technically challenging[21-22]; Izak et
al[40] described a case in which a second attempt
at explantation of an SA20AL IOL (Alcon) in the presence of a fibrosed and
contracted capsular bag resulted in explantation of the IOL together with the
capsular bag. Lee et al[18] proposed a workaround by suggesting an
optic-only removal to avoid zonular dehiscence. However, complications that can
occur as a result of remnant haptics include dislocation of the haptic to the
optic zone or into the vitreous cavity, interference with the positioning of
the newly implanted IOL, and iritis due to chafing of the iris when the haptics
of the new IOL are located in the ciliary sulcus.
In conclusion, this technique provides a
safe and efficient technique for foldable (one-piece acrylic) IOL removal
without cutting the optic. By removing the IOL intact and enlarging the wound
internally, we eliminate the need for using intraocular scissors yet permit
safe explantation of the IOL with minimal trauma to the corneal endothelium by
employing the soft-shell technique. The use of cohesive OVD to hydrodissect the
haptics out of the fibrosed capsule also greatly reduces the risk of zonular
dehiscence. The description of
this procedure provides the surgeon with an alternative technique for foldable
IOL removal and exchange.
ACKNOWLEDGEMENTS
Conflicts
of Interest:
Lee MH, None; Webster
DL, None.
REFERENCES
1 Jin GJ,
Crandall AS, Jones JJ. Changing indications for and improving outcomes of
intraocular lens exchange. Am J
ophthalmol 2005;140(4):688-694.
[PubMed]
2 Mamalis
N, Brubaker J, Davis D, Espandar L, Werner L. Complications of foldable
intraocular lenses requiring explantation or secondary intervention-2007 survey
update. J Cataract Refract Surg 2008;34(9):1584-1591. [CrossRef] [PubMed]
3
Mavroforou A, Michalodimitrakis E. Physicians' liability in ophthalmology
practice. Acta Ophthalmologica
Scandinavica
2003;81(4):321-325. [CrossRef]
[PubMed]
4 Galor A,
Gonzalez M, Goldman D, O'Brien TP. Intraocular lens exchange surgery in
dissatisfied patients with refractive intraocular lenses. J Cataract Refract Surg 2009;35(10):1706-1710. [CrossRef] [PubMed]
5 Woodward
MA, Randleman JB, Stulting RD. Dissatisfaction after multifocal intraocular
lens implantation. J Cataract Refract
Surg 2009;35(6):992-997. [CrossRef] [PubMed]
6 de Vries
NE, Webers CA, Touwslager WR, Bauer NJ, de Brabander J, Berendschot TT, Nuijts
RM. Dissatisfaction after implantation of multifocal intraocular lenses. J Cataract Refract Surg 2011;37(5):859-865.
[CrossRef] [PubMed]
7 Lane SS.
Foldable intraocular lens removal/exchange: can it be prevented? Ophthalmology 2004;111(11):1965-1966. [CrossRef] [PubMed]
8 Jones JJ,
Jones YJ, Jin GJ. Indications and outcomes of intraocular lens exchange during
a recent 5-year period. Am J Ophthalmol 2014;157(1):154-162.e1.
[CrossRef] [PubMed]
9 Leysen I,
Bartholomeeusen E, Coeckelbergh T, Tassignon MJ. Surgical outcomes of intraocular
lens exchange: five-year study. J
Cataract Refract Surg 2009;35(6):1013-1018. [CrossRef] [PubMed]
10
Fernández-Buenaga R, Alió JL, Pérez-Ardoy AL, Larrosa-Quesada A, Pinilla-Cortés
L, Barraquer R, Alio JL 2nd, Muñoz-Negrete FJ. Late in-the-bag intraocular lens
dislocation requiring explantation: risk factors and outcomes. Eye (Lond) 2013;27(7):795-801;quiz 802. [CrossRef] [PubMed] [PMC free article]
11
Fernández-Buenaga R, Alió JL, Pinilla-Cortés L, Barraquer RI. Perioperative
complications and clinical outcomes of intraocular lens exchange in patients
with opacified lenses. Graefe's Arch Clin
Exp Ophthalmol 2013;251(9):2141-2146. [CrossRef] [PubMed]
12 Werner
L. Causes of intraocular lens opacification or discoloration. J Cataract Refract Surg 2007;33(4):713-726. [CrossRef] [PubMed]
13
Karamaounas N, Kourkoutas D, Prekates C. Surgical technique for small-incision
intraocular lens exchange. J Cataract
Refract Surg 2009;35(7):1146-1149. [CrossRef] [PubMed]
14 Mehta
JS, Wilkins MR, Gartry DS. Explantation of an acrylic Acrysoft intraocular lens
without wound enlargement. Acta
Ophthalmol Scand 2005;83(2):262-263. [CrossRef]
[PubMed]
15 Por YM,
Chee SP. Trisection technique: a 2-snip approach to intraocular lens
explantation. J Cataract Refract Surg 2007;33(7):1151-1154. [CrossRef] [PubMed]
16 Osher
RH. Crisscross lensotomy: New explantation technique. J Cataract Refract Surg 2006;32(3):386-388. [CrossRef] [PubMed]
17 Narang
P, Steinert R, Little B, Agarwal A. Intraocular lens scaffold to facilitate
intraocular lens exchange. J Cataract
Refract Surg 2014;40(9):1403-1407. [CrossRef] [PubMed]
18 Lee SJ,
Sun HJ, Choi KS, Park SH. Intraocular lens exchange with removal of the optic
only. J Cataract Refract Surg 2009;35(3):514-518. [CrossRef] [PubMed]
19
Theoulakis PE, Brinkmann CK, Petropoulos IK, Gatzogias MI, Katsimpris JM.
Hydrogel intraocular lens exchange: five-year experience. Klin Monbl Augenheilkd 2009;226(4):254-257. [CrossRef] [PubMed]
20
Kubaloglu A, Sari ES, Koytak A, Cinar Y, Erol K, Ozerturk Y. Intraocular lens
exchange through a 3.2-mm corneal incision for opacified intraocular lenses. Indian J Ophthalmol 2011;59(1):17-21. [CrossRef] [PubMed] [PMC free article]
21 Dagres
E, Khan MA, Kyle GM, Clark D. Perioperative complications of intraocular lens
exchange in patients with opacified Aqua-Sense lenses. J Cataract Refract Surg 2004;30(12):2569-2573. [CrossRef] [PubMed]
22 Gashau
AG, Anand A, Chawdhary S. Hydrophilic acrylic intraocular lens exchange:
five-year experience. J Cataract Refract
Surg 2006;32(8):1340-1344. [CrossRef] [PubMed]
23 Davis D,
Brubaker J, Espandar L, Stringham J, Crandall A, Werner L, Mamalis N. Late
in-the-bag spontaneous intraocular lens dislocation. Ophthalmology 2009;116(4):664-670. [CrossRef] [PubMed]
24 Kim SS,
Smiddy WE, Feuer W, Shi W. Management of dislocated intraocular lenses. Ophthalmology 2008;115(10):1699-1704. [CrossRef] [PubMed]
25 Hayashi
K, Hirata A, Hayashi H. Possible predisposing factors for in-the-bag and
out-of-the-bag intraocular lens dislocation and outcomes of intraocular lens
exchange surgery. Ophthalmology
2007;114(5):969-975. [CrossRef]
[PubMed]
26 Werner
L, Kollarits CR, Mamalis N, Olson RJ. Surface calcification of a 3-piece
silicone intraocular lens in a patient with asteroid hyalosis:a
clinicopathologic case report. Ophthalmology
2005;112(3):447-452. [CrossRef]
[PubMed]
27
Stringham J, Werner L, Monson B, Theodosis R, Mamalis N. Calcification of
different designs of silicone intraocular lenses in eyes with asteroid
hyalosis. Ophthalmology
2010;117(8):1486-1492. [CrossRef]
[PubMed]
28 Haymore
J, Zaidman G, Werner L, Mamalis N, Hamilton S, Cook J, Gillette T. Misdiagnosis
of hydrophilic acrylic intraocular lens optic opacification. Ophthalmology 2007;114(9):1689-1695. [CrossRef] [PubMed]
29 Voros
GM, Strong NP. Exchange technique for opacified hydrophilic acrylic intraocular
lenses. Eur J Ophthalmol 2005;15(4):465-467. [PubMed]
30 Pepose
JS, Qazi MA, Davies J, Doane JF, Loden JC, Sivalingham V, Mahmoud AM. Visual
performance of patients with bilateral vs combination Crystalens, ReZoom, and
ReSTOR intraocular lens implants. Am J
Ophthalmol 2007;144(3):347-357. [CrossRef] [PubMed]
31 Zhao G,
Zhang J, Zhou Y, Hu L, Che C, Jiang N. Visual function after monocular
implantation of apodized diffractive multifocal or single-piece monofocal
intraocular lens Randomized prospective comparison. J Cataract Refract Surg 2010;36(2):282-285. [CrossRef] [PubMed]
32 Hofmann
T, Zuberbuhler B, Cervino A, Montés-Micó R, Haefliger E. Retinal straylight and
complaint scores 18 months after implantation of the AcrySof monofocal and
ReSTOR diffractive intraocular lenses. J
Refract Surg 2009;25(6):485-492. [PubMed]
33 de Vries
NE, Franssen L, Webers CA, Tahzib NG, Cheng YY, Hendrikse F, Tjia KF, van den
Berg TJ, Nuijts RM. Intraocular straylight after implantation of the multifocal
AcrySof ReSTOR SA60D3 diffractive intraocular lens. J Cataract Refract Surg 2008;34(6):957-962. [CrossRef] [PubMed]
34 Solebo
LA, Eades Walker RJ, Dabbagh A. Intraocular lens exchange for pseudophakic
refractive surprise due to incorrectly labeled intraocular lens. J Cataract Refract Surg 2012;38(12):2197-2198. [CrossRef] [PubMed]
35
Parikakis EA, Chalkiadakis SE, Mitropoulos PG. Piggybacking technique for
vitreous protection during opacified intraocular lens exchange in eyes with an
open posterior capsule. J Cataract
Refract Surg 2012;38(7):1130-1133. [CrossRef] [PubMed]
36 Narang
P, Agarwal A, Kumar DA, Jacob S, Agarwal A, Agarwal A. Clinical outcomes of
intraocular lens scaffold surgery. Ophthalmology
2013;120(12):2442-2448. [CrossRef] [PubMed]
37 Kumar
DA, Agarwal A, Prakash G, Jacob S, Agarwal A, Sivagnanam S. IOL scaffold
technique for posterior capsule rupture. J
Refract Surg 2012;28(5):314-315. [CrossRef] [PubMed]
38
Henderson BA, Yang EB. Intraocular lens explantation technique for one-piece
acrylic lenses. J Refract Surg 2012;28(7):499-502. [CrossRef] [PubMed]
39
Lundström M. Endophthalmitis and incision construction. Curr Opin Ophthalmol 2006;17(1):68-71. [CrossRef]
[PubMed]
40 Izak AM, Werner L, Pandey SK, Apple DJ, Vargas LG, Davison JA.
Single-piece hydrophobic acrylic intraocular lens explanted within the capsular
bag: case report with clinicopathological correlation. J Cataract Refract Surg 2004;30(6):1356-1361. [CrossRef] [PubMed]
[Top]