·Letter to the Editor··Current Issue· ·Achieve· ·Search Articles· ·Online Submission· ·About IJO· PMC
A
surprising visual improvement following a prolonged 5-month retained subfoveal
perfluorocarbon liquid
Daniel
SW Ting, Vicky Hsin-Ju
Lu, Gavin SW Tan, Edmund YM Wong
Singapore
National Eye Center, 11 Third Hospital Avenue, 168751, Singapore
Correspondence to: Daniel SW Ting. Singapore
National Eye Center, 11
Third Hospital Avenue,
168751, Singapore.
daniel.ting45@gmail.com
Received: 2015-01-17
Accepted: 2015-10-28
DOI:10.18240/ijo.2016.07.24
Citation: Ting DS, Lu V, Tan G, Wong E. A
surprising visual improvement following a prolonged 5-month retained subfoveal
perfluorocarbon liquid. Int J Ophthalmol
2016;9(7):1079-1081
Dear
Sir,
I am Dr. Daniel Ting, from the Department of
Ophthalmology, Singapore National Eye Centre, Singapore. I write to present a
case of a surprising significant visual improvement following a prolonged
5-month retained subfoveal perfluorocarbon liquid.
Retained
perfluorocarbon liquid (PFCL) has been shown to cause decreased visual acuity,
retinal pigment epithelial (RPE) toxicity, retinal degeneration and gravity
deformation[1],
secondary glaucoma[2] and
loss of endothelial cells in aphakic eyes[3].
Retained subretinal PFCL was found to cause droplet phagocytosis in rabbit RPE
as early as 1h. Nevertheless, case reports describe visual prognosis following
prompt PFCL removal within 2wk to be reasonable[4-5], and
less so with increased duration of retention up to one month[6]. The
purpose of this study was to report a case of good visual recovery following a
retained subfoveal PFCL for 5mo in a patient with an initial shallow macula-off
rhegmatogenous retinal detachment.
Madam X, a
65-year-old Chinese female, presented to Singapore National Eye Center with
right macula-off rhegmatogenous retinal detachment, preceded by one week
history of right eye floaters and inferior visual field deficit. Past ocular
history include myopia (-3.0 dioptre). On presentation, her best-corrected
visual acuity (BCVA) was 6/24 OD and 6/18 OS with no evidence of afferent
pupillary defect. Confrontational visual field showed a right inferior
hemifield defect. She had mild nuclear sclerotic cataracts in both eyes and
intraocular pressure (IOP) was 10 mm Hg and 14 mm Hg in the right and left eye respectively.
Posterior segment examination showed a right macula-off retinal detachment
extending from ten to three o’clock with an U-shaped tear (measuring
approximately 1 clock hour) at one o’clock meridian at the equator. There was
no vitreous haemorrhage or signs of proliferative vitreoretinopathy (PVR) in
her right eye and both eyes had complete posterior vitreous detachment.
The patient
underwent a right combined pars plana 20-gauge (G) vitrectomy, 240 encircling
band and lensectomy with the aid of PFCL (Arcotane, C8F18,
ARCAD, France) to flatten the retina followed by insertion of intraocular
gas-15% hexafluroethane (C2F6) at the end of the
operation. She was left aphakic with an intact posterior capsule.
Post-operative day one, her retina was flat with 90% gas fill. A small
subretinal PFCL was noted inferiorly. At four weeks post-operatively, BCVA OD
was CF at 1 metre despite complete resorption of 15% C2F6.
Fundal examination revealed presence of a several subretinal PFCL bubbles at
the macula (Figure 1),
confirmed on spectral domain optical coherence tomography (SD-OCT, Spectralis,
Heidelberg, Deutschland, Germany) (Figure 1).
On the same visit, she was offered surgical removal of PFCL but she was
reluctant to undergo a repeat vitrectomy despite being counseled regarding the
risk of retina toxicity secondary to retained PFCL.
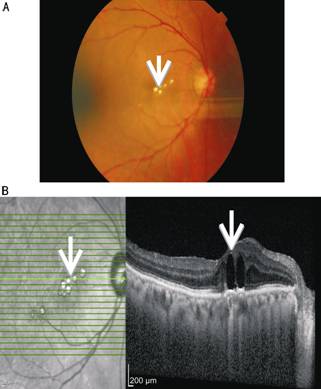
Figure 1
Presence of subfoveal perfluorocarbon liquid in fundus photo (A, white arrow) and in spectral domain optical coherence
tomography (B, white arrow).
Due to the
persistent poor vision for 5mo, she finally agreed to undergo surgical removal
of the retained PFCL bubbles, followed by insertion of secondary sulcus
intraocular lens. Intra-operatively, the internal limiting membrane (ILM) was
peeled with Eckhardt forceps (John Weiss and Son Ltd.,
Italy) for 2 to 3 disc diameter around the fovea. A localized subretinal bleb
of balanced salt solution (BSS) was created temporally from the fovea with 41 G cannula (Bausch and Lomb, Rochester,
NY, USA) but de-roofing with BSS was not successful. A small hole was then
created using 41 G cannula one
disc diameter superior to the fovea to drain the PFCL bubbles. Subsequently, air fluid exchange was
performed and 15% perfluoropropane (C3F8) gas was
utilized as endotamponade. Postoperatively, her BCVA OD had improved to 6/12
with residual extrafoveal subretinal PFCL bubbles (Figure
2).
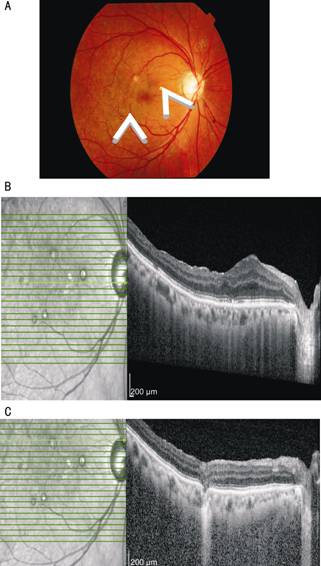
Figure
2 A clear subfoveal region with a few residual extrafoveal perfluorocarbon
liquid bubbles (white arrow) post surgical removal using 41 G cannula (A), and SD-OCT
shows a flat subfoveal region with absence of perfluorocarbon liquid bubbles (B) and the area where the 41 G cannula was inserted intraoperatively (C).
PFCLs are
fluorinated, synthetic compounds containing carbon fluorine bonds. They have
been utilized in various vitreoretinal surgical scenarios including rhegmatogenous
retinal detachments, PVR, giant retinal tears, tractional retinal detachment
from diabetes and dislocated crystalline lens or intraocular lens. PFCLs are
colorless, odorless and have high affinity for oxygen. Different types of PFCLs
such as perfluorooctane, perfluorodecalin, perfluoroperhydrophenanthrene and
perfluorotributylamine have been used intraoperatively in posterior segment
surgeries with subsequent removal and vitreous substitute replacement at the
end of operation. Due to its higher specific gravity than water, it is utilized
to flatten the detached retina against the underlying retinal pigment
epithelium and displaces subretinal fluid anteriorly.
Some of the postoperative
complications associated with PFCLs were retained PCFL (3.8%)[7],
recurrent retinal detachment with or without PVR (19%), transient hypotony (6%)
and increased IOP (4%). Even though PFCL has been shown to be toxic in animal
experiments[8], it
has been found to be inert to the intraocular environment[9]. Our
case with retained subfoveal PFCL removal after 5mo demonstrated that there is
still a possibility for marked visual improvement following surgical removal.
Nevertheless, the visual recovery of the patients with retinal detachment often
depends on the types of presentation-macula on or off; duration and also the
pre-existing state of the retina (status of ellipsoid zone, formerly known as
the inner segment/outer segment line) [10].
In our case, we
utilized perfluorooctane (Arcotane, C8F18, ARCAD, France)
as the choice of heavy liquid which has specific gravity of 1.76 and boiling
point of 110℃. It not only has viscosity of 0.8 cSt
which allows easy removal but also high vapour pressure (56 mm Hg)
that theoretically allows small droplets to vaporize quickly into the air or
gas bubble at the end of surgery, reducing the chance of retained droplets.
However, it will remain in-situ when it is trapped at the subretinal plane.
Depending on the location of the perfluorooctane, it generally requires removal
if it is close to the fovea as it will affect visual acuity and function.
According to Garcia-Valenzuela et al[11]
perfluorooctane and perflurodecalin showed no significant difference in
subretinal retention rates. The size of peripheral retinotomy, absence of
saline rinse after fluid-air exchange, use of silicone oil and removal of the
intraocular lens were found to be associated with increased risk of subretinal
PFCL retention[11].
Our case report
demonstrated a remarkable visual recovery following an extended period of
subfoveal perfluorooctane retention (up to 5mo). This may suggest that
perfluorooctane may be less toxic to the retinal pigment epithelial cells as
compared to other types of PFCLs. Further in
vitro studies may aid in the evaluation of changes in the setting of
retained subretinal perfluorooctane.
ACKNOWLEDGEMENTS
Conflicts of Interest: Ting DS, None;
Lu V, None; Tan G, None; Wong E, None.
REFERENCES
1 Chang S,
Lincoff H, Zimmerman NJ, Fuchs W. Giant retinal tears. Surgical techniques and
results using perfluorocarbon liquids. Arch
Ophthalmol 1989;107(5):761-766. [CrossRef] [PubMed]
2 Foster RE,
Smiddy WS, Alfonso EC, Parrish RK 2nd. Secondary glaucoma associated with
retained perfluorophenanthrene. Am J
Ophthalmol 1994;118(2):253-255. [CrossRef]
3 Moreira H, de
Queiroz JM Jr, Liggett PE, McDonnell PJ. Corneal toxicity study of two
perfluorocarbon liquids in rabbit eyes. Cornea
1992;11(5):376-379. [CrossRef]
4 Escalada Gutiérrez F, Mateo García C. Extraction of subfoveal liquid
perfluorocarbon. Arch Soc Esp Ophthalmol 2002;77(9):519-521.
5 Wong TY, Ho
T. Retained perfluorodecalin after retinal detachment surgery. Int Ophthalmol 1996;20(6):293-294. [PubMed]
6 Lesnoni G,
Rossi T, Gelso A. Subfoveal liquid perfluorocarbon. Retina 2004;24(1):172-176. [CrossRef]
7 Verma LK,
Peyman GA, Wafapoor H, Greve MD, Millsap CM, Adile SL. An analysis of posterior
segment complications after vitrectomy using the perfluorocarbon
perfluoroperhydrophenanthrene (Vitreon). Vitreon Collaborative Study. Ophthalmic Surg 1995;26(1):29-33. [PubMed]
8 Chang S,
Ozmert E, Zimmerman NJ. Intraoperative perfluorocarbon liquids in the
management of proliferative vitreoretinopathy. Am J Ophthalmol 1988;106(6):668-674. [CrossRef]
9 Chang S,
Sparrow JR, Iwamoto T, Gershbein A, Ross R, Ortiz R. Experimental studies of
tolerance to intravitreal perfluoro-n-octane liquid. Retina 1991;11(4):367-374. [CrossRef]
10 Baba T,
Yamamoto S, Arai M, Sugawara T, Mitamura Y, Mizunoya S. Correlation of visual
recovery and presence of photoreceptor inner/outer segment junction in optical
coherence images after successful macular hole repair. Retina 2008;28(3):453-458. [CrossRef]
[PubMed]
11
Garcia-Valenzuela E, Ito Y, Abrams GW. Risk factors for retention of subretinal
perfluorocarbon liquid in vitreoretinal surgery. Retina 2004;24(5):746-752. [CrossRef] [PubMed]
[Top]