INTRODUCTION
Visual impairment is the source of numerous serious medical, psychological, social, and economic problems.According to the World Health Organization (WHO), the number of visually impaired people worldwide, in 2010, was estimated at 285 million, of whom 39 million were blind[1].Because more than 90% of visually impaired people reside in developing countries, WHO approved an action for “Vision 2020” over the next decade. One of its main recommendations was that all countries worldwide provide regularly updated data regarding the prevalence and causes of blindness and visual impairment, for the use in evidence-based advocacy, planning,and monitoring of eye care programmes[2]. Consequently,population-based studies in different countries are required to estimate the burden of visual impairment.
In China, the majority of blindness data has come from rural or suburban areas[3-8]. The report of the Nine-Province Survey estimated the prevalence of blindness among rural people ≥60 years of age to be 2.29%[6]. Estimates of blindness among persons living in urban areas have been based primarily on two population-based studies conducted in the Beixinjing Block[9] and Dachang Block[10], two areas located near the Shanghai Medium Ring Road. As a result of the urbanization of China over the past 10y, Shanghai city become larger because more people begin living and working in the central areas and the inhabitants of that zone have been transformed from a rural to urban population[9-10]. Hence, the previously mentioned data might underestimate the magnitude of visual impairment in an economically developed area. To address this inconsistency, we conducted a population-based survey of an urban population of persons >60 years of age, living in the Xietu Block of Shanghai. In 2012, the Xietu Block had an estimated population of 66300 persons, 18653 (28.1%) of whom were ≥60 years of age, a far greater proportion than that in the national population of elderly people (13.3%) (based on the 2010 national population census)[11]. This study was designed to determine the prevalence, causes, and risk factors of blindness and visual impairment among elderly Chinese populations in metropolitan Shanghai. The blindness and visual impairment within our dataset were defined on both presenting visual acuity (PVA) and best-corrected visual acuity(BCVA).
MATERIALS AND METHODS
Sampling and Enumeration This study adhered to the tenets of the Declaration of Helsinki and was approved by the Ethics Committee of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital. Written informed consents were obtained from all of the participants.
The Xietu Block, a 2.792 kilometer area located in the Xuhui District of downtown metropolitan Shanghai, comprises 19 administrative communities. The Shanghai municipal government has developed this district as a commercial zone since the 1990s. The average annual income of an urban resident is 16683 yuan, the highest in China. One strategy to improve the availability and accessibility would be to set up public health facilities such as community health centers, district hospitals,and comprehensive hospitals. Meanwhile, the improved capital expenditure makes the quality of services affordable in this region.
The sample size was estimated according to the prevalence of blindness (3.22%) from the China Nine-Province Survey(2009)[6]. Assuming an error bound (25%) with 95%confidence, a response rate (90%), and a design effect (1.5),the sample of 3182 persons was required.
We conducted the random cluster sampling to identify participants. The sampling frame was constructed using geographically defined clusters based on community registry data. Cluster boundaries were defined such that each cluster had a population of approximately 1000 individuals (all ages). Depending on sample size and proportion of the elderly population, we randomly selected 18 clusters to reach the target sample size.
Field work was from March 2012 to May 2012. Lists of participants’ information were obtained from residence committees. Using door-to-door visits, information regarding name, age, gender, and educational level was obtained by Community Health Service physicians. Those unregistered adults living in the community for ≥6mo were enumerated and included in this study. Those registered adults being out of the community for ≥6mo were excluded from the study.
Data Collection Study participants were examined on a pre- scheduled date established at the time of enumeration.Participants’ identities were verified by identity cards (ID).A standard questionnaire was used to obtain demographic characteristics, personal and family medical history, and lifestyle risk factors[12]. The interview included questions related to the diagnosis and treatment of chronic diseases, including diabetes, hypertension, dyslipidemia, and cardiovascular events. Participants were also questioned about cigarette smoking, i.e. if they had ever smoked at least one cigarette a day for >6mo. Participants were defined as follows: “neversmokers” for those who answered “no”; “smokers” for those who answered “yes”; “occasional smokers” for those who smoked <20 pack-years (i.e. the number of packs of cigarettes per day multiplied by the number of years of smoking); and“heavy smokers” for those who smoked ≥20 pack-years.Alcohol intake was defined as the consumption of at least 30 g of alcohol per week 1y. Body weight and height were measured by standard methods, and body-mass index (BMI)was evaluated[12].
1y. Body weight and height were measured by standard methods, and body-mass index (BMI)was evaluated[12].
Early Treatment Diabetic Retinopathy Study (ETDRS) E-chart(Precision Vision, Villa Park, IL, USA) was used to measure distant visual acuity (VA). VA measurement was initiated at a distance of 4 m and VA was recorded on the lowest line read successfully. Counting fingers, hand movement, and light perception tests were performed for those unable to identify any of the chart’s symbols at a distance of 1 m. The initial PVA was measured without refractive correction or with the use of distance glasses, if worn. Any eyes with the PVA ≤20/40 had their vision retested with a pinhole to obtain the BCVA.
Detailed examinations of the eyelid, globe, lens and fundus were carried out by experienced ophthalmologists using a slit-lamp and direct ophthalmoscope (66 Vision Tech Co.,Ltd., Suzhou, China). Fundus photos were recorded by digital fundus photography (CR-2, Canon Co., Ltd., Tokyo, Japan).Optical coherence tomography (OCT) (OSE-2000, Moptim Co., Ltd., Shenzhen, China) was performed if any fundus abnormality was found. Goldmann applanation tonometry(66vision Tech Co., Ltd., Suzhou, China) was performed when the participant was suspected of having glaucoma.Some participants failed to walk, and we went to their home to examine eyes using a portable handheld slit lamp (KJ5S1,Kangjie Co., Ltd., Suzhou, China), direct ophthalmoscope and Goldmann applanation tonometry.
The pupils were dilated to examine for the participants whose lens and fundus status could not be examined suitably or with a BCVA ≤20/40. Those eyes with shallow anterior chambers were not dilated. The same experienced ophthalmologist diagnosed one principal cause for the eyes with the PVA≤20/40. Refractive errors were considered to be responsible for visual impairments when the VA was ≤20/40 and when it was improvable to >20/40 after correction. When corneal opacity, pterygium, and other eye diseases were considered to be the primary causes of blindness, diagnoses of these diseases followed standard clinical criteria.
A standard protocol was used to rapidly assess the main causes of blindness for each eye. In the absence of evidence of retinal abnormalities, cataract was the main cause of visual impairment in an eye with a significant vision-obscuring opaque lens. Myopic maculopathy was diagnosed for eyes with at least 6.0 diopters refractive error, and at least one of the findings: tessellated fundus with diffuse yellowishwhite areas, white patchy chorioretinal atrophy, posterior staphyloma, or macular haemorrhage[4]. According to agerelated macular degeneration (AMD) stage classifications of the Age-Related Eye Disease Study Research (AREDS),AMD was characterized by multiple large drusen, geographic atrophy, choroidal neovascularisation (CNV), and disciform scars[13]. Glaucoma was diagnosed based on the International Society for Geographical and Epidemiological Ophthalmology Classification[14]. Diabetic retinopathy (DR) was characterized by microaneurysms, hard exudates, intraretinal haemorrhages,and macular cystoid macular edema[15]. Other causes for visual impairment were based on routine clinical diagnoses.If there were two or more reasons responsible for the visual impairment in one eye, the experienced ophthalmologist evaluated all available information and choose the cause more available to treatment or prevention[16].
Quality Control Training Program All study investigators and staff members successfully completed a training program that familiarised them with the aims, specific tools, and methods of the study. At the training sessions, the inter-observer repeatability of measurements between the two groups of observers was determined by the κ value. Repeatability of VA reached a κ value of 0.8 between the two groups. For assignment of the principal causes of blindness, the κ value was 0.9. In addition to repeatability, reliability was also measured by comparing the diagnoses of the cataract and survey records of chronic diseases history, the results of this comparison also showed acceptable agreement (κ=0.8).
Definition The WHO criteria was conducted to categorize VA(which are similar to those used in the National Nine-Province Survey Survey) [6] as follows: normal vision, VA ≥20/63 in the better-seeing eye; visual impairment, VA of <20/63 to≥20/400 in the better-seeing eye; and blindness, VA of <20/400 in the better-seeing eye. Prevalences of blindness and visual impairment were based on both PVA and BCVA[4].
Statistical Analysis An electronic database was maintained using Version3.0 EpiData software (Epidata Association,Odense, Denmark). Data were double-checked and validated by inspection. Prevalences of blindness and visual impairment were stratified by age, gender, educational levels, and smoking status. The association of blindness and visual impairment with age, gender, and educational level were mesured using logistic regression. A multivariate logistic regression analysis was used to evaluate the association of demographics, lifestyle, and metabolic factors, with the odds ratio (OR) of blindness and visual impairment. All data were processed using Version7.0 STATA software (STATA Corp, College Station, TX, USA).P<0.05 was considered statistically significant.
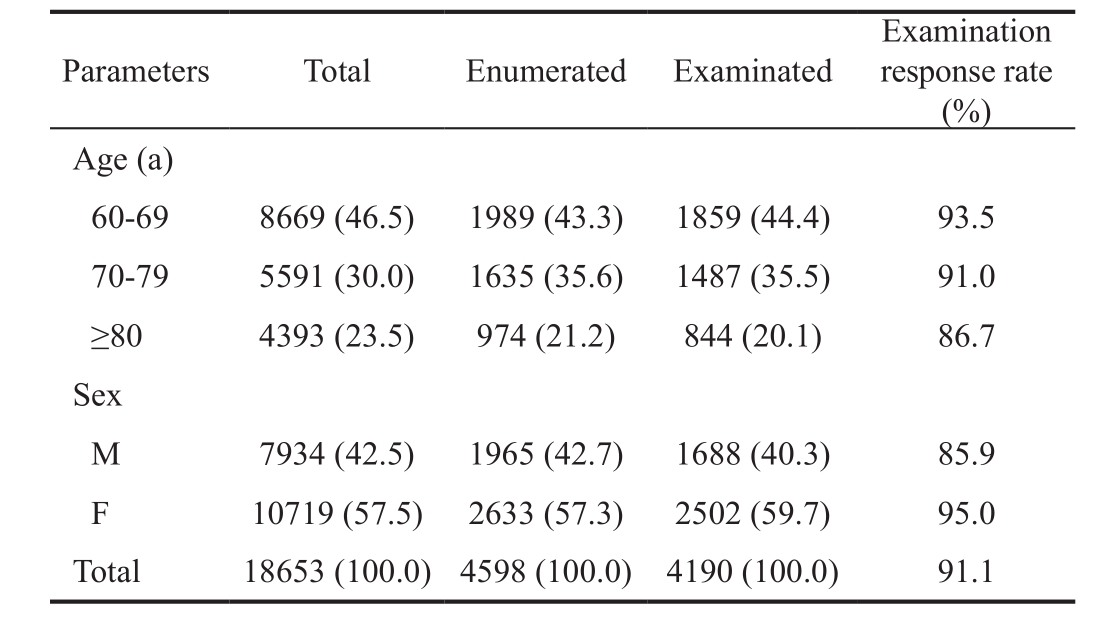
Table 1 Comparison of age and gender profiles of population vs examined sample n (%)
RESULTS
Among 18653 persons ≥60 years of age in the Xietu Block,4598 persons were enumerated, and 4190 participants were successfully examined, corresponding to an overall response rate of 91.1%. The main reasons for the 408 non-participants were 1) too busy (52.7%); 2) good VA (18.4%); 3) distrust of tests (16.9%); and 4) lack of comprehension of tests(4.4%), with the latter reason being indicated by incomplete questionnaires. The compared proportions of age and gender profiles in study population and examined sample were listed in Table 1.
Prevalences of blindness and visual impairment for the study population were stratified by age, gender, educational level and smoking status (Table 2). Based on PVA datum, the prevalences of blindness and visual impairment were 1.1% and 7.6%, respectively. Within our sample set, the prevalences of blindness and visual impairment increased rapidly with age,and this trend becomes more dramatic in residents >80 years of age (OR=2.8 for blindness, P=0.019; OR=3.8 for visual impairment, P =0.000). The prevalence of visual impairment was generally higher among women than men (OR=2.0,P=0.000; Table 2); however, the prevalence of blindness was not significantly different between women and men (OR=1.1,P=0.971; Table 2). Lower levels of education (not greater than high-school level) tended to be associated with visual impairment (P=0.000). The prevalence of visual impairment was also significantly higher among smokers than among never-smokers (OR=1.8, P=0.008; Table 3). Based on BCVA datum, the prevalences of blindness and visual impairment dropped to 0.9% and 3.9%, respectively (Table 2). The prevalence of visual impairment increased with older age,female gender, lower educational level, and smoking habits,with the differences showing statistical significance (P<0.05).Multivariate logistic regression models indicated that older age, female gender, less than high-school education, being overweight, and cigarette smoking were all significantly associated with increased odds for blindness and visual impairment, based on both PVA and BCVA simultaneously(P<0.01; Table 3). To explore the difference of occasional smoking and heavy smoking, we analyzed the prevalence of visual impairment stratified by age, gender, educational levels. As indicated in Table 4, based on both PVA-defined and BCVA-defined data, participants ≥80 years of age, femalegender and low educational level combined with a heavy smoking habit, exhibited a greater risk of visual impairment/blindness.
Table 2 The prevalence of blindness and visual impairment along with subgroup data in the study population

1Odds ratio was adjusted for age, sex and educational level. aP<0.05, bP<0.01.
Table 3 Epidemiological determinants of visual impairment and blindness in the study population

1Overweight was defined as a body-mass index (BMI) between 25.0 and 29.9; 2Cigarette smoking was defined as having smoked at least one cigarette every day for half a year or more; 3Alcohol drinking was defined as the consumption of at least 30 g of alcohol per week for one year or more; 4Odds ratio were adjusted for age, sex, educational level, presence of hypertension, family history of eye diseases, overweight,cigarette smoking and alcohol drinking.
Table 4 Association of smoking status and visual impairment stratified by age, sex, and education levels
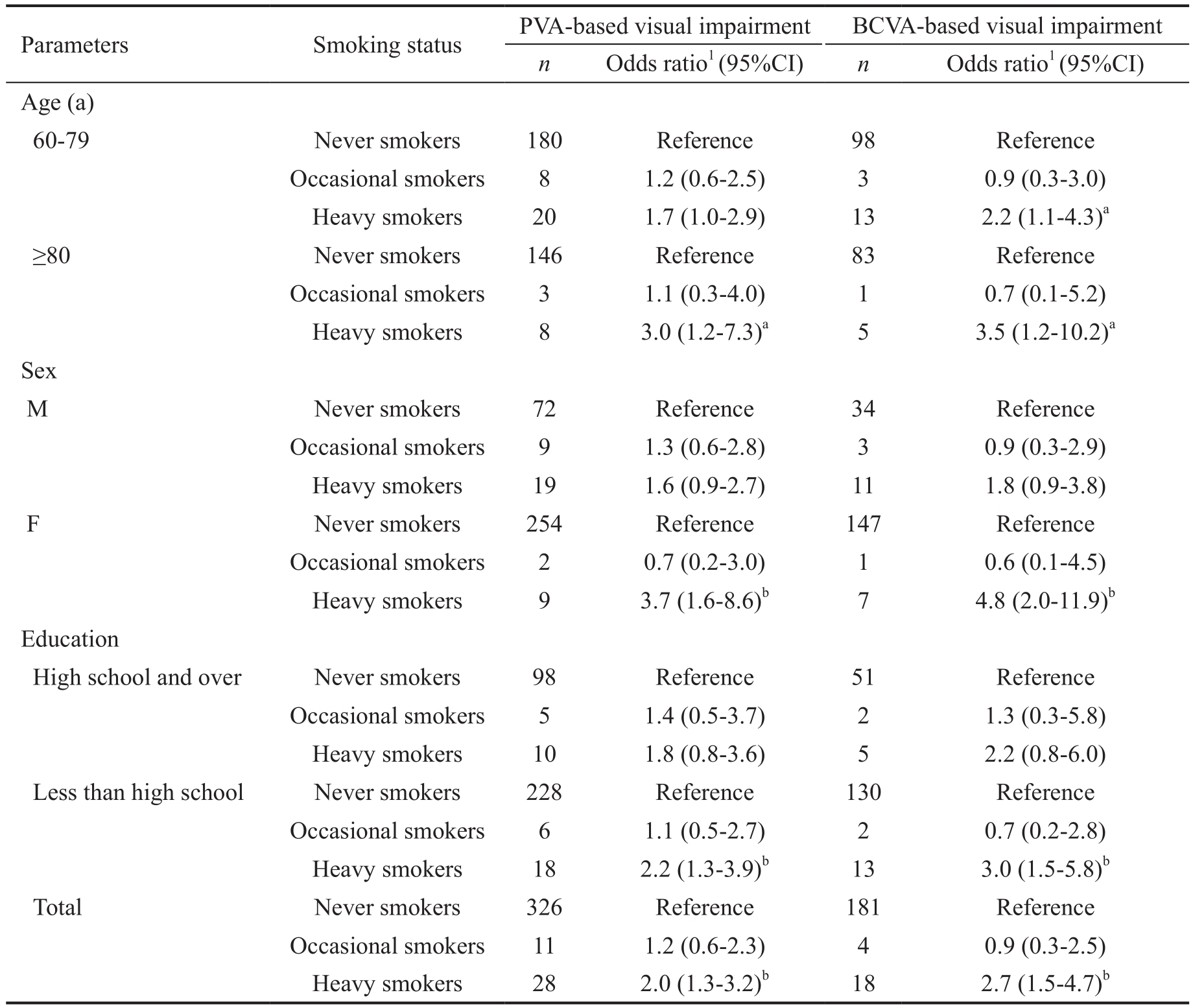
1Odds ratio were adjusted for age, sex, and educational level. aP<0.05, bP<0.01.
Table 5 Principle causes of visual impairment and blindness in the study population

AMD: Age-related macular degeneration; PVA: Presenting visual acuity; BCVA: Best-corrected visual acuity.
Cataract was the major cause of visual impairment across all levels of severity (Table 5), accounting for 37.6% of PVA-defined blindness and 64.0% of PVA-defined visual impairment. Even after refractive correction, cataract remained the leading cause of blindness (37.1%) and visual impairment (58.7%). For PVA blindness, myopic maculopathy (28.1%) was the second most common cause, followed by AMD (7.3%). However, for PVA visual impairment, the main causes were cataract (64.0%),myopic maculopathy (13.8%), refractive error (6.9%), and AMD (5.3%). Based on BCVA criteria, myopic maculopathy,AMD, and phthisical/enucleated eye accounted for 26.4%,7.1%, and 5.0% of blindness, respectively. However, for BCVA visual impairment, the main causes were cataract (58.7%),myopic maculopathy (19.2%), AMD (5.3%), and DR (4.5%),respectively.
DISCUSSION
China is a rapidly developing country undergoing significant economic expansion. Meanwhile, the population of China has increased rapidly, especially the elderly population ≥60 years of age. According to the traditional standards of the United Nations (elderly ≥60 years of age over 10% of the total population), China has become an aging society since 2000.This issue becomes dramatic in Shanghai City. As referred in the Introduction, our target population has 28.1% of elder people ≥60 years of age, far greater than that in our country[11],it is crucial to learn the situation of blindness and visual impairment in our target population. In this study, we evaluated the prevalence, causes, and risk factors of blindness and visual impairment in a metropolitan Shanghai elderly population ≥60 years of age. Despite risk factors such as old age[4,17], female gender[6], low educational level[4-5,18], and obesity[19], we are,to our knowledge, thefirst to identify an association between cigarette smoking and visual impairment in the populationbased survey. Many studies have explored the association between smoking and age-related eye diseases (ARED), such as nuclear cataract, AMD, DR, and glaucoma[20]. However, the relationship between smoking and visual impairment has not been extensively evaluated and is not clearly understood. Using a multivariate logistic regression model, we found that the estimated prevalence of visual impairment was higher among smokers than that of never-smokers. After stratification by age,gender, and educational levels, smoking was still established as a risk factor. However, further studies were recommended to confirm this association. This finding is similar as that of Surgeon General's report in the United States, which showed that smoking increases the risk of the blind-causing eye disease[21]. Thisfinding not only has important implications for the vision protection policy, but also towards characterizing the populations needing to be targeted for intervention.
The results of this study provide valuable population-based data on the prevalence and causes of blindness and visual impairment in one specific metropolitan area of China.Previous surveys[3-8] in China have reported prevalences of visual impairment (in urban and rural adult populations with heterogeneous age distribution) that differ from ours. The results may possibly come from the reason that these studies used dissimilar definitions of visual impairment. Thus, two sets of of results should only be compared when the age range and definitions of visual impairment are similar. The prevalence(1.1%) of PVA-based blindness in this study was lower than that reported in Beixinjing (1.6%) and higher than that of Dachang Blocks (0.9%), two surveys in Shanghai[9-10]. The prevalence was also lower than that reported in Hong Kong elderly ≥60 years of age (1.8%)[22]. We found the prevalence of PVA-based visual impairment to be lower than either of the aforementioned surveys. Although the prevalence of BCVA-defined blindness dropped to 0.9%, and that of visual impairment declined to 3.9%, both were higher than those reported in either the Shanghai Beixinjing or Dachang[9-10].However, this study reported lower prevalences compared with those of other urban Chinese population (Beijing and Guangdong)[6]. We also reported higher prevalences compared with those of an urban Malay population in Singapore and a Latino population in Los Angeles, CA, USA[23-24]. Although improvement of the accessibility and relative affordability of eye healthcare services in metropolitan Shanghai occurred faster than that in other urban and rural areas, there is still a need to develop suitable, effective eye care programs in urban China.
In agreement with other population-based surveys on the Chinese Han population, cataract was found to be the leading cause of blindness and visual impairment[4,6,25]. This study indicated that about 60% of visual impairment cases and 35% of blindness cases were due to cataracts. The Shanghai Beixinjing survey showed retinal degenerative diseases to be the leading cause of blindness, followed by cataract, refractive error, and corneal disease. Taking into account that cataract operations are similarly affordable for the two communities,the difference in results must have emanated from a disparity in the acceptance of cataract surgery among the residents of the two communities. It is indicated that as a result of the process of urbanization and rapid aging of society, visual impairment caused by cataract remains to be one of vital public health problems. We still need to strengthen the education about cataract operation among communities. Myopic maculopathy was the second principal cause of blindness and visual impairment. This result is in agreement of other reports from East Asia including China[8,26]. As such, myopic maculopathy may become an urgent challenge for the prevention of global blindness, once avoidable or treatable causes of blindness such as cataract are under control. AMD, a difficult disease to treat, is also likely to account for a greater proportion of future blindness in developing countries[27]. However, it is rather surprising that glaucoma was not a major cause. Because it was recently reported that glaucoma account for 17% of visual impairment in northern China[28], the absence of glaucoma as a major cause in the present study may be attributed partly to the relatively low prevalence of glaucoma in the Eastern Chinese population. Lack of visual field and gonioscopy tests would also underestimate the prevalence of glaucoma.
The strengths of our study include: 1) a large sample size;2) high response rate (91.1%); and 3) use of standardized protocols, based on those from the Nine-Province Survey[6].There are also several limitations to the present study. First,there may have been selection bias due to the exclusion of residents who worked outside of the block during the survey period, because most of these individuals were young, healthy participants who likely had normal vision. Meanwhile, the current study has more women and men, 2502 to 1688 (1.4 to 1), selection bias could not be avoided, even though we conducted gender adjustment. These might have led to a slight overestimation of the prevalence of visual impairment in the group 60 to 69 years of age. Second, we used only central VA data but did not use the results of visualfield tests to assess PVA. Because we used only pinhole VA data and not the results of refractometry tests to assess BCVA, this may overestimate the prevalence of visual impairment. Third,Table 2 showed that the prevalence of visual impairment and blindness was similar between smokes and non-smokers and for PVA-based and BCVA-based visual impairment, it was actually higher in nonsmokers. It seemed to contradict otherfindings that smoking is associated with visual impairment[29].It was because the overall prevalence of smoking in our target population (11.2%) is much lower than that was reported among Chinese adults (31.8%)[30]. Fourth, because cataracts accounted for 58.65% of visual impairment even after refractive correction, it is possible that a significant retinal disease was masked by the presence of a dense cataract, resulting in the underreporting of age-related retinopathy and maculopathy.Finally, the sample size calculated based on 25% error bound would minimize the sample size and generate bias in the outcomes.
In conclusion, we report preliminary results of a comprehensive, population-based study of older (≥60 years of age)urban adults in China. Our data on the prevalence, causes, and risk factors of blindness and visual impairment indicate the ocular status of the population sample from the eastern part of metropolitan China to be worse than expected. This study may help the eye-care project in developing strategies for highquality services.
REFERENCES
1 World Health Organization. Gobal data on visual impairment 2010.Available at: http://www.who.int/blindness/publications/globaldata/en.Accessed on August 18, 2015.
2 World Health Organization. Action plan for the prevention of avoidable blindness and visual impairment 2009-2013. Geneva: WHO, 2010
3 Li X, Zhou Q, Sun L,Wang Z, Han S, Wu S, Wang N. Prevalence of blindness and low vision in a rural population in northern China: preliminary results from a population-based survey. Ophthalmic Epidemiol 2012;19(5):272-277.
4 Li J, Zhong H, Cai N, Luo T, Li J, Su X, Li X, Qiu X, Yang Y, Yuan Y, Yu M. The prevalence and causes of visual impairment in an elderly Chinese Bai ethnic rural population: the Yunnan minority eye study. Invest Ophthalmol Vis Sci 2012;53(8):4498-4504.
5 Zhang Y, Wang H, Liu J, Wang T, Cao S, Zhou D, Du L, Li Z, Liu P.Prevalence of blindness and low vision: a study in the rural Heilongjiang Province of China. Clin Exp Ophthalmol 2012;40(5):484-489.
6 Zhao J, Ellwein LB, Cui H, Ge J, Guan H, Lv J, Ma X, Yin J, Yin ZQ,Yuan Y, Liu H. Prevalence of vision impairment in older adults in rural China: the China Nine-Province Survey. Ophthalmology 2010;117(3):409-416.416.e1.
7 Li T, Du L, Du L. Prevalence and causes of visual impairment and blindness in Shanxi province, China. Ophthalmic Epidemiol 2015;22(4):239-245.
8 Tang Y, Wang X, Wang J, Huang W, Gao Y, Luo Y, Lu Y. Prevalence and causes of visual impairment in a Chinese adult population: the Taizhou Eye Study. Ophthalmology 2015;122(7):1480-1488.
9 Huang XB, Zou HD, Wang N, Wang WW, Fu J, Shen BJ, Xie TH,Chen YH, Xu X, Zhang X. A prevalence survey of blindness and visual impairment in adults aged equal or more than 60 years in Beixinjing blocks of Shanghai, China. Zhonghua Yan Ke Za Zhi 2009;45(9):786-792.
10 Tong XW, Zhao R, Zou HD, Zhu JF, Wang J, Yu J, Wang W, He XG,Lu HH, Zhao HJ, Wang WB. A prevalence investigation of blindness and vision impairment in 2009 in older adults of Dachang Blocks of Baoshan District, Shanghai, China. Zhonghua Yan Ke Za Zhi 2011;47(9):785-790.
11 National Bureau of Statistics People’s Republic of China. Majorfigures of the 2010 population census. Available at: http://www.stats.gov.cn/tjsj/pcsj/rkpc/6rp/indexch.htm. Accessed on August 18, 2015.
12 Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, Shan Z, Liu J, Tian H, Ji Q,Zhu D, Ge J, Lin L, Chen L, Guo X, Zhao Z, Li Q, Zhou Z, Shan G, He J. Prevalence of diabetes among men and women in China. N Engl J Med 2010;362(12):1090-1101.
13 The Age-Related Eye Disease Study (AREDS): design implications.AREDS report no.1. Control Clin Trials 1999;20(6):573-600.
14 Foster PJ, Buhrmann R, Quigley HA, Johnson GJ. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol 2002;86(2):238-242.
15 Akhter A, Fatema K, Ahmed SF, Afroz A, Ali L, Hussain A.Prevalence and associated risk indicators of retinopathy in a rural Bangladeshi population with and without diabetes. Ophthalmic Epidemiol 2013;20(4):220-227.
16 World Health Organization. Programme for the prevention of blindness and deafness. coding instructions for the WHO/PBL eye examination record (version III). Geneva: WHO, 1988:1-17.
17 Yonekawa Y, Varma R, Choudhury F, Torres M, Azen SP. Risk factors for four-year incident visual impairment and blindness: the Los Angeles Latino Eye Study. Ophthalmology 2011;118(9):1790-1797.
18 Jones GC, Crews JE, Danielson ML. Health risk profile for older adults with blindness: an application of the international classification of functioning, disability, and health framework. Ophthalmic Epidemiol 2010;17(6):400-410.
19 Kyari F, Tafida A, Sivasubramaniam S, Murthy GV, Peto T, Gilbert CE; Nigeria National Blindness and Visual Impairment Study Group.Prevalence and risk factors for diabetes and diabetic retinopathy: results from the Nigeria national blindness and visual impairment survey. BMC Public Health 2014;14:1299.
20 Zhang X, Kahende J, Fan AZ, Barker L, Thompson TJ, Mokdad AH,Li Y, Saaddine JB. Smoking and visual impairment among older adults with age-related eye diseases. Prev Chronic Dis 2011;8(4):A84.
21 Asfar T, Asfar T, Lam BL, Lee DJ. Smoking causes blindness: time for eye care professionals to join thefight against tobacco. Invest Ophthalmol Vis Sci 2015;56(2):1120-1121.
22 Michon JJ, Lau J, Chan WS, Ellwein LB. Prevalence of visual impairment, blindness, and cataract surgery in the Hong Kong elderly. Br J Ophthalmol 2002;86(2):133-139.
23 Wong TY, Chong EW, Wong WL, Rosman M, Aung T, Loo JL, Shen S,Loon SC, Tan DT, Tai ES, Saw SM. Prevalence and causes of low vision and blindness in an urban malay population: the Singapore Malay Eye Study. Arch Ophthalmol 2008;126(8):1091-1099.
24 Varma R, Ying-Lai M, Klein R, Azen SP. Prevalence and risk indicators of visual impairment and blindness in Latinos: the Los Angeles Latino Eye Study. Ophthalmology 2004;111(6):1132-1140.
25 Rabiu MM, Jenf M, Fituri S, Choudhury A, Agbabiaka I, Mousa A. Prevalence and causes of visual impairment and blindness, cataract surgical coverage and outcomes of cataract surgery in Libya. Ophthalmic Epidemiol 2013;20(1):26-32.
26 Yamada M, Hiratsuka Y, Roberts CB, Pezzullo ML, Yates K, Takano S, Miyake K, Taylor HR. Prevalence of visual impairment in the adult Japanese population by cause and severity and future projections.Ophthalmic Epidemiol 2010;17(1):50-57.
27 Rasoulinejad SA, Zarghami A, Hosseini SR, Rajaee N, Rasoulinejad SE, Mikaniki E. Prevalence of age-related macular degeneration among the elderly. Caspian J Intern Med 2015;6(3):141-147.
28 Song W, Sun X, Shao Z, Zhou X, Kang Y, Sui H, Yuan H. Prevalence and causes of visual impairment in a rural North-east China adult population: a population-based survey in Bin County, Harbin. Acta Ophthalmol 2010;88(6):669-674.
29 Klein R, Lee KE, Gangnon RE, Klein BE. Relation of smoking,drinking, and physical activity to changes in vision over a 20-year period:the Beaver Dam Eye Study. Ophthalmology 2014;121(6):1220-1228.
30 Li Z, Yao Y, Han W, Yu Y, Liu Y, Tao Y, Kou C, Jiang L, Sun Q, Yin Y, Zhang H, Li B. Smoking prevalence and associated factors as well as attitudes and perceptions towards tobacco control in Northeast China. Int J Environ Res Public Health 2015;12(7):8606-8618.