Dear Editor,
The state of the vitreo-retinal interface affects various retinal diseases, and the presence or absence of a
posterior vitreous detachment (PVD) is one of the most important factors[1-5]. As such, various studies studying PVD in relation to retinal disease have been performed[1-5].
However, defining a PVD can be difficult, because the vitreous is not always well-visualized clinically due to its transparency and lacunae. Spectral-domain optical coherence tomography(SD-OCT), with its ability to visualize the vitreoretinal interface, has the potential to objectively determine if a PVD is present or not. Yet a clear definition of PVD on OCT imaging has not been established to date.
We suggest how to define a PVD by evaluating and describing the posterior vitreous structures of selected cases using enhanced high-density line spectral-domain optical coherence tomography (HD SD-OCT) images in vitreoretinal mode.This is a descriptive case series that includes SD-OCT (AvantiTM,Optovue Inc., CA, USA) images with enhanced HD line in vitreoretinal mode in 2014 and 2015.
We analyzed over 600 consecutive SD-OCT images with enhanced HD line mode from August, 2014 to March 2015. Four representative enhanced HD SD-OCT images that demonstrated either a PVD, or a partial PVD with large posterior precortical vitreous pocket (PPVP) masquerading as a PVD (false positive PVD), were included in the study (Table 1).
Enhanced HD line is a line scan designed to highlight the vitreous or choroid by choosing the vitreoretinal or chorioretinal modes respectively during live scanning[6]. After obtaining the OCT images in the enhanced HD line vitreoretinal mode, we manually adjusted the contrast settings in order to obtain better visualization of the vitreous gel.
Figure 1 shows two HD SD-OCT images with vitreous gel detached from the retina. Figure 1A is a 74-year old female’s HD SD-OCT image showing a PVD, in which the posterior hyaloid membrane (PHM; identified as a hyper reflective continuous line) is detached from the retinal surface and optic disc. Figure 1B is the HD SD-OCT image of a 13-year old male with juvenile retinoschisis, which demonstrates posterior cortical vitreous separated from the retina, though without a hyper reflective line in the vitreous gel, indicating the PHM has not detached from the retina.
Figure 2A is the HD SD-OCT image of a 46 year-old male with acquired immune deficiency syndrome (AIDS) while Figure 2B is that of a 54 year-old male with a history of central serous chorioretinopathy. Figure 2 shows that the vitreous gel is detached from the retina, but the PHM is discontinuous. The extrafoveal vitreous is detached with a visible PHM, while the detached vitreous overlying the fovea does not have a PHM.
After the advent of OCT, many researchers have tried to evaluate PVD, in isolation or corresponding to retinal changes,depending on the presence or absence of PVD[1-5]. Until recently,many studies used SD-OCT in standard retina-focused crossline mode. Two recently introduced OCT modules, HD SDOCT in vitreoretinal mode, and swept source (SS)-OCT,enable clear visualization of the posterior vitreous structures.However, there has been no consensus definition of PVD with criteria established using either SS-OCT or HD SD-OCT in vitreoretinal mode[2,5,7].
Clinicians may diagnose PVD intuitively via OCT when the images demonstrate a hypore fl ective space between the retina and vitreous gel. However, this space may be not the gap between the PMH and the retina, but rather a PPVP. This type of mistake is easily made when the OCT image is not a wideangle view, as these truncated images usually miss the PPVP margins[6]. However, in patients with a very large PPVP, even the wide-angle view may not show the PPVP margins (Figure 1B). Thus to differentiate the PPVP from a PVD, a hyper re fl ective PHM would be a more reliable clue than the PPVP margin. Both images in Figure 1 taken with the 40° angle show spaces between the vitreous gel and the retina without a PPVP margin, however Figure 1A is indeed a PVD, as it contains a hyper reflective PHM, while Figure 1B is a large liquefied PPVP as there is no hyper re fl ective line corresponding to the PHM.
Table 1 Characteristics of the cases

AIDS: Acquired immune deficiency syndrome. The cases do not have any ocular trauma and surgery history.
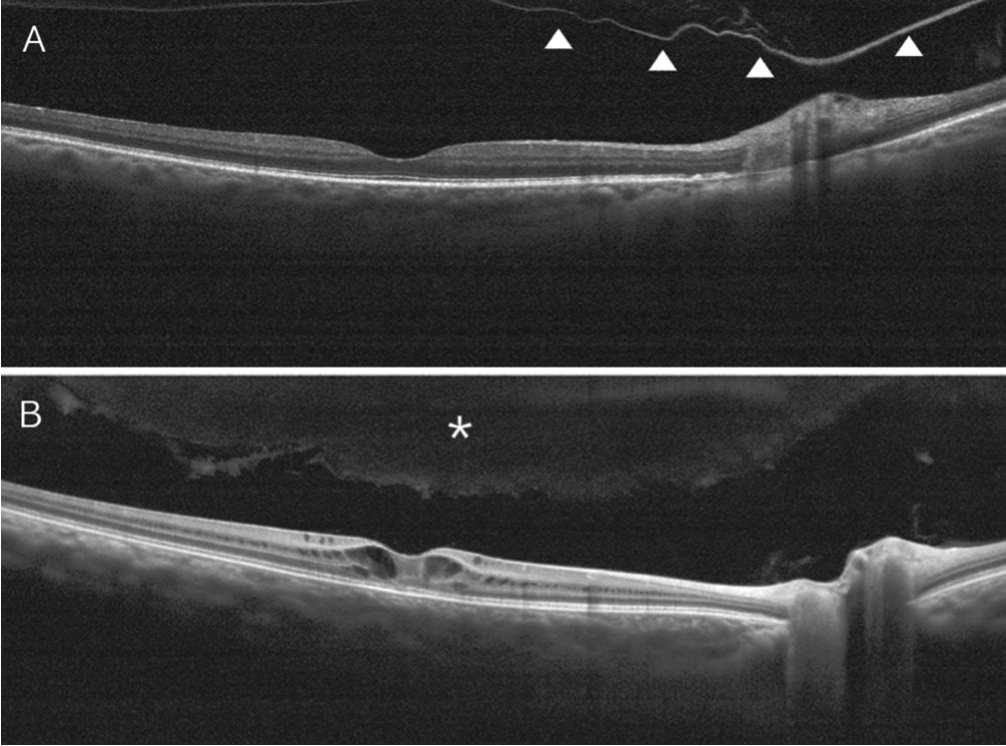
Figure 1 Optical coherence tomographic findings in PVD and false positive PVD PVD: A hyper refective posterior hyaloid membrane (PHM, arrow heads) is detached from the retina (A); False positive PVD: Vitreous gel (asterisk) is detached from the retina, but a PHM is not identified on its posterior border (B).

Figure 2 Posterior vitreous in the foveal and parafoveal area A:The posterior vitreous with the PHM (arrow heads) in the parafoveal area is detached from the retina; however vitreous anterior to the fovea does not show a hyper re fl ective PHM, as it is presumed to be a PPVP (arrows). A liquefied vitreous lacune (asterisk) is identified. B:The vitreous gel is detached, save for the vitreous anterior to the fovea(within arrows) which is not bound by the PHM (arrow heads).
Figure 2 reveals the reflectivity difference of the vitreous margin, depending on the presence or absence of the PHM.The vitreous gel anterior to the fovea does not show the hyper reflective PHM line, but the parafoveal vitreous is bound by the PHM. Because of this discontinuous PHM, we believe it is torn. Figure 2A suggests that the space posterior to the vitreous without a PHM is a PPVP. On the basis of thefinding,we can hypothesize that in some cases with an evolving PVD,the PHM around the PPVP is still attached on the fovea and the PHM beyond the PPVP is detached from the retina. The PHM attached to the fovea is easily seen after triamcinolonestaining during vitrectomy surgery, not only because the PHM is firmly attached on the fovea but also since it is separated from vitreous gel by PPVP. Tractional vitreous forces may not be transferred to the PHM on the fovea because of the PPVP,and the PHM on the peripheral PPVP is presumed to be torn by traction, as it has not detached from the retina.
Although this study has limitations due to its small size and case selection, we nonetheless suggest that a detached hyper reflective line corresponding to the PHM is an important sign in PVD diagnosis, and the PHM surrounding the PPVP may still be attached on the fovea during the process of PVD evolution. This has implications for preoperative planning in vitreoretinal surgery, as correctly identifying the status of the vitreoretinal interface can save time and avoid unnecessary,potentially dangerous surgical maneuvers when not indicated.Further study is warranted, to include a consecutive evaluation where PVD status as detected with enhanced HD SD-OCT in vitreoretinal mode is confirmed or rebutted during triamcinolone assisted pars planavitrecto my to prove these hypothesis and observations.
REFERENCES
1 Takezawa M, Toyoda F, Kambara C, Yamagami H, Kakehashi A.Clarifying the mechanism of idiopathic macular hole development in fellow eyes using spectral-domain optical coherence tomography. Clin Ophthalmol 2011;5:101-108.
2 Ophir A, Martinez MR. Epiretinal membranes and incomplete posterior vitreous detachment in diabetic macular edema, detected by spectral-domain optical coherence tomography. Invest Ophthalmol Vis Sci 2011;52(9):6414-6420.
3 Kakehashi A, Kado M, Akiba J, Hirokawa H. Variations of posterior vitreous detachment. Br J Ophthalmol 1997;81(7):527-532.
4 Ono R, Kakehashi A, Yamagami H, Sugi N, Kinoshita N, Saito T,Tamemoto H, Kuroki M, Lshikawa SE, Kawakami M. Prospective assessment of proliferative diabetic retinopathy with observations of posterior vitreous detachment. Int Ophthalmol 2005;26(1-2):15-19.
5 Kakehashi A, Takezawa M, Akiba J. Classification of posterior vitreous detachment. Clin Ophthalmol 2014;8:1-10.
6 Kim YC, Harasawa M, Salcedo-Villanueva G, Siringo FS, Paciuc-Beja M, Olson JL, Mandava N, Quiroz-Mercado H. enhanced high-density line spectral-domain optical coherence tomography imaging of the vitreoretinal interface: description of selected cases. Semin Ophthalmol 2016;31(6):559-566.
7 Stalmans P, Duker JS, Kaiser PK, Heier JS, Dugel PU, Gandorfer A,Sebag J, Haller JA. Oct-based interpretation of the vitreomacular interface and indications for pharmacologic vitreolysis. Retina 2013;33(10):2003-2011.