INTRODUCTION
Although monofocal intraocular lenses (IOLs) are typically implanted after cataract surgery, monofocal IOLs require the use of glasses for far or near distance vision, as these lenses per definition have only one focus. Recently, the number of patients who prefer multifocal IOLs, which contain both near and far foci, has increased, due to the improved quality of life offered by such lenses. Although multifocal IOLs and multifocal contact lenses (CLs) maintain clear vision for both near and distance vision, their contrast sensitivity is lower than that of monofocal IOLs and CLs[1-15]. This is also noted in the visual field test[16-20].
When the dome-shaped visual field test is performed for presbyopic patients and those with implanted monofocal IOLs,it requires near refractive correction, as stimuli are presented in a spherical plane of radius 30 cm[21]. On the other hand,distance refractive correction can generally be applied if the dome-shaped visual field test is performed in an eye with a multifocal IOL or CL, as these are theoretically optically designed with a focal point for both far and near distance[16-20].
However, we have found some difficulty in refractive correction for such cases in the clinical visual field test[22]. In particular,optimal refractive correction is important in patients with glaucoma, as it is thought that the decreased sensitivity induced by inadequate refractive correction influences the estimate of visual field progression[23].
In a previous study of the effect of multifocal IOLs and CLs on visual field sensitivity, the mean deviation value was decreased by approximately 1-2 dB in standard automated perimetry(SAP) as compared with the effect of monofocal IOLs and CLs[16,18]. On the other hand, the visual field sensitivity was not significantly decreased in SAP[7] or frequency doubling technology[24]. However, SAP has previously been performed with distance correction, without near correction[16,18]. It is possible that the decreasing sensitivity in the visual field test caused by multifocal IOLs or CLs can be prevented with near refractive correction, because some refractive and diffractive multifocal IOLs have been designed to be slightly distancedominant[25-26].
The aim of this study was to evaluate the refractive correction required for SAP in eyes harboring multifocal IOLs. To this end, we mimicked this situation in healthy young participants by using an accommodation-paralyzing agent and refractive multifocal CLs.
SUBJECTS AND METHODS
Clinical Trial Registration: UMIN Clinical Trials Registry(http://www.umin.ac.jp/) under unique trial number UMIN 000018390 (date of registration: 07/23/2015).
This study followed the tenets of the Declaration of Helsinki.Each participant provided written informed consent after the Ethics Committee of the Kitasato University School of Allied Health Science approved the study (No.2015-10).
In this cross-sectional study, we evaluated 30 student volunteers studying the Orthoptic and Visual Science course at Kitasato University who had undergone SAP at least three times within the last 3mo. All the participants underwent comprehensive ophthalmic examinations, including noncycloplegic refraction testing, visual acuity testing at a 5-m distance using a Landolt ring chart, intraocular pressure measurement, ocular axial length measurement, and slit-lamp and fundus examination by a glaucoma specialist (Shoji N).Participants were included in the study if they had a corrected visual acuity of 20/20 or better, intraocular pressure of 21 mm Hg or less, cylindrical power of -1.50 diopter or less, a normal optic disc appearance, open angle, and no ophthalmic diseases that could affect the results of the visual field test. For each participant, the eye with the lower amount of astigmatism was selected as the study eye. If the amount of astigmatism was the same in both eyes, the eye with the lower level of myopia was chosen as the study eye.
SAP was performed using the Humphrey field analyzer(HFA, Carl Zeiss Meditec AG, Dublin, CA, USA) and the Swedish Interactive Threshold Algorithm Standard strategy.Both the 24-2 and 10-2 test point protocols were used for SAP measurement. The measurement conditions for SAP were calibrated to a background luminance of 10 cd/m2 (31.4 asb), stimulus size was set at Goldmann size III, stimulus presentation time at 0.2 second, and foveal threshold measurement as “on”. Pupil diameter was recorded during SAP using HFA.
Multifocal CLs (ROHTO i.Q 14 Bifocal D-type; ROHTO Pharmaceutical Co., Ltd., Osaka, Japan) were used in the current study. This refractive multifocal CL has a far distance zone in the central area of the lens, with a progressive transition zone in the middle area of the lens, and a near distance zone in the peripheral area of the lens (Figure 1). This refractive multifocal CL also has additional power for near distance (+2.50 diopter).
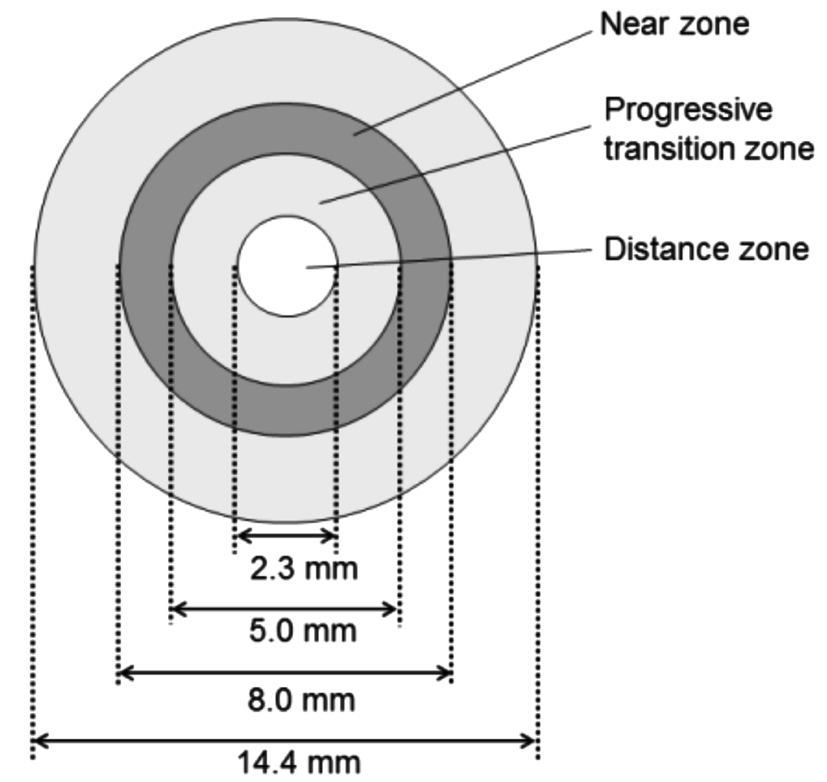
Figure 1 Optical design of the refractive multifocal contact lens(ROHTO i.Q 14 Bifocal D-type) The refractive multifocal CL used in the current study consists of three zones, with distance, progressive transition, and near zones in order from the central to the peripheral zones, respectively. Additional power for near vision is+2.50 diopter.
To paralyze accommodation, 1% cyclopentolate hydrochloride(Cyplegin®, Santen Pharmaceutical Co., Ltd, Osaka, Japan)was used. This eyedrop was instilled three times with 5-min intervals, one drop per-time. CL power was defined by refraction testing using an auto-refractometer at 1h after the initial instillation. Refraction power was measured with the assumption of a 12-mm vertex distance. The vertex distance of the auto-refractometer was converted to 0-mm vertex distance on the corneal surface using the following formula:
For example, when corrections were performed for participants who had -4.00 diopter as measured by the auto-refractometer after instillation of cyclopentolate hydrochloride, the CL power was calculated using the following formula:
as -3.82 diopter. The CLs used in the current study are made with 0.25-diopter intervals. Thus, this participant would receive a correction with a -3.75 diopter CL as the closest approximation of the required CL power.
All participants underwent SAP using the 10-2 and 24-2 test point protocol under the following conditions: monofocal CL corrected for near vision (baseline); multifocal CL corrected for distance vision, without additional near correction with a spectacle lens (mCL-D); and mCL-D with additional near correction with a spectacle lens of +3 diopter (mCL-N). The 1-Day ACUVUE (Johnson & Johnson Vision Care, Inc.,New Brunswick, NJ) was used as monofocal CL. Although multifocal CLs used in the current study have an optical design of additional power of +2.50 diopter for near vision, correction for all participants was performed with spectacle lenses of+0.50 diopter for the mCL-D condition.
Primary outcome measures were mean deviation (MD), pattern standard deviation (PSD), and the foveal threshold with each refractive correction. Secondary outcome measures were fixation loss rate, false-positive rate, false-negative rate, test duration, and pupil size after instillation with three refractive corrections.
Participants were excluded from the study if the fixation loss was more than 20% and the FP rate was more than 15%; and if intracranial disorder was suspected based on the visual field test result.
Statistical Analysis All data were analyzed using MedCalc version 16.1 (MedCalc Software, Ostend, Belgium) and G*Power3 version 3.1.7 (Franz Faul, Universität Kiel, Kiel,Germany). Bonferroni tests were used for data comparisons.The Bonferroni-corrected probability values of <0.05 were considered statistically significant. The effect size, α error,power (1−β error), and nonsphericity correction were as follows: 0.25 (middle), 0.05, 0.80, and 0.50, respectively, and the required sample size was 29 participants for three repeated measurements.
RESULTS
One participant was given a false-positive rate >20%. Eventually,29 eyes of 29 participants were finally analyzed. Table 1 shows the demographic characteristics of the participants included in the current study.
Table 2 shows the parameters for the three refractive corrections.With mCL-N, the foveal threshold decreased significantly by 1.0-2.5 dB in the 24-2 test point protocol (P<0.0001) and by 2.2 dB in the 10-2 test point protocol (P<0.0003), as compared to the baseline and mCL-D values. Although the foveal threshold with mCL-D decreased significantly, by 1.5 dB(P=0.0427), from that of the baseline value with the 24-2 test point protocol, there was no significant difference in the foveal threshold between the baseline and mCL-D with the 10-2 test point protocol. From CL-N, the MD decreased significantly by-1.01 to -1.12 dB with the 24-2 test point protocol (P<0.0038)and by-1.23 to -1.32 dB with the 10-2 test point protocol(P<0.0001), as compared to that for baseline and mCL-D.With both the 24-2 and 10-2 test point protocols, there were no significant differences in the MD between the baseline and mCL-D. The PSD was also not significantly different among the three refractive conditions, for either the 24-2 or the 10-2 test point protocol.
Fixation loss, false-positive, and false-negative values were not significantly different among the three refractive conditions with either the 24-2 or the 10-2 test point protocol. Although the test duration of the mCL-N was significantly longer,by 20.8-24.8s, in the 10-2 test point protocol (P<0.0034),this duration was not significantly different among the three refractive conditions for the 24-2 test point protocol.Furthermore, although the pupil size for mCL-D was significantly larger (by 0.6-0.9 mm) for both the 24-2 and 10-2 test point protocol than that at baseline and mCL-N,there was no significant difference between baseline and mCL-D values.
Table 1 Participants’ demographic and ocular characteristics

Visual acuity is given as best corrected visual acuity.
In two-way repeated measure analysis of variance for the three refractive corrections between the test point protocols,an interaction was found for the foveal threshold (P=0.003)between the 24-2 and 10-2 test protocol, but there were no interactions for the other parameters.
Figures 2 and 3 show representative results with three refractive corrections in the 24-2 and 10-2 test protocol, respectively.
DISCUSSION
In the current study, the MD as determined using both the 24-2 and 10-2 protocols was comparable between the baseline and mCL-D, while the MD of the mCL-N was significantly decreased compared to the baseline and mCL-D values. In previous reports[16-19] that compared patients with diffractive multifocal IOLs or refractive multifocal CLs, and monofocal IOLs or CLs, the MD with diffractive multifocal IOLs or refractive multifocal CLs corrected for distance vision was decreased by approximately -1 to -2 dB as compared to that of the monofocal IOLs or CLs corrected for near vision using the 24-2[16,18] and 10-2 protocols[17], as well as a custom protocol[19]. The difference was thought to be due to pupil dilation induced by the accommodative paralyzing agent and the difference in the refractive optical design, which is dependent on pupil diameter. In the present study, the average pupil diameter after instillation of accommodative paralyzing agent was approximately 8-9 mm. The refractive multifocal CLs used in the present study would be distance-dominant with a small to medium pupil diameter (Figure 1). In such a case, it would theoretically be more appropriate to correct distance vision to near vision using near correction when a domed-shaped perimeter is used. However, with increasing pupil diameter, visual performance tends to be near-dominant,despite the distance correction. Thus, the MD of mCL-N decreased significantly as compared with that of the baseline and mCL-D.
Table 2 Comparison of visual field results among the three refractive correction methods
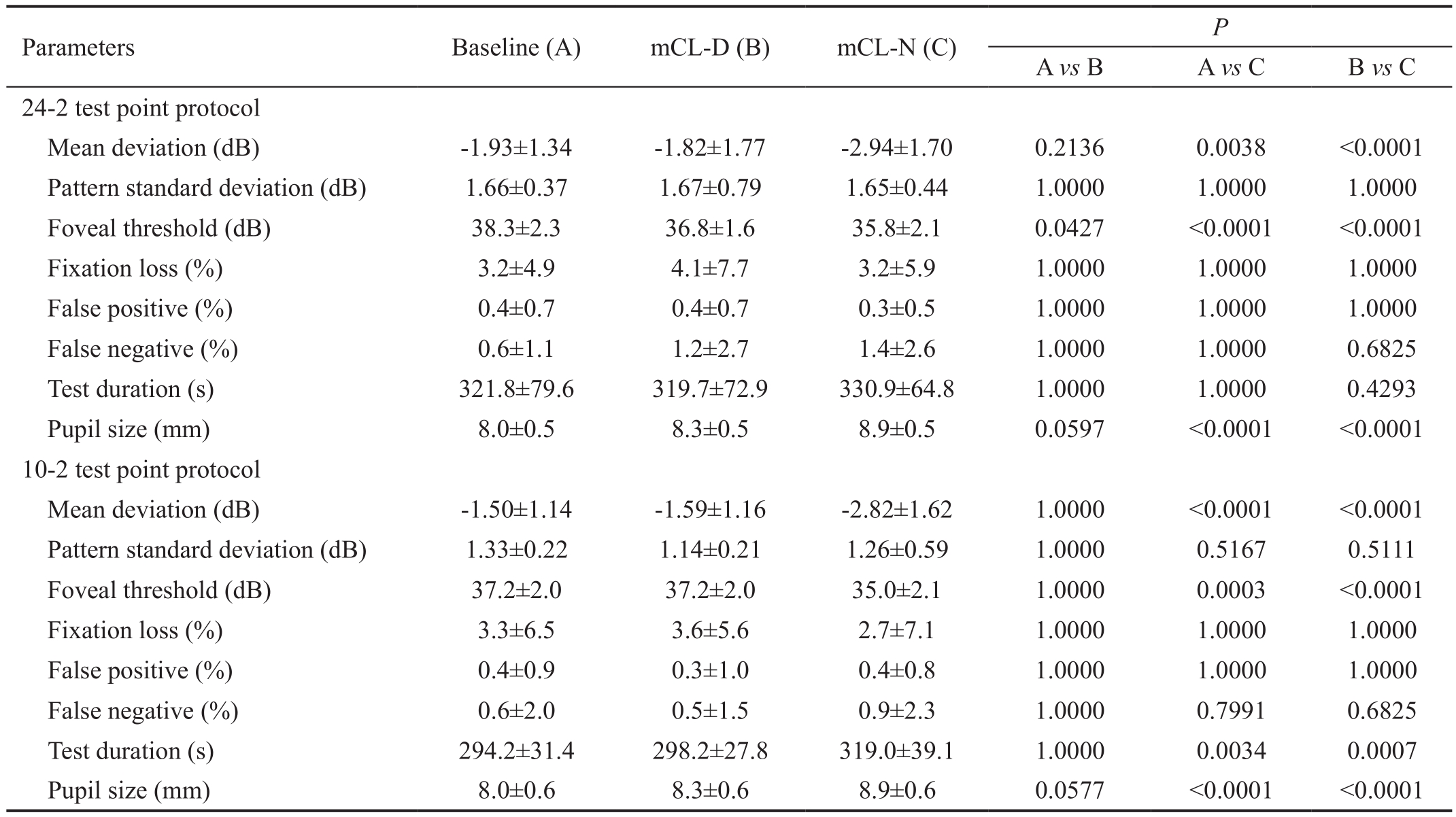
P values adjusted with Bonferroni correction are given. Baseline: Monofocal contact lens (CL) corrected with near distance. mCL-D: Multifocal CL without near correction (distance correction). mCL-N: Multifocal CL and near correction with spectacle lens.
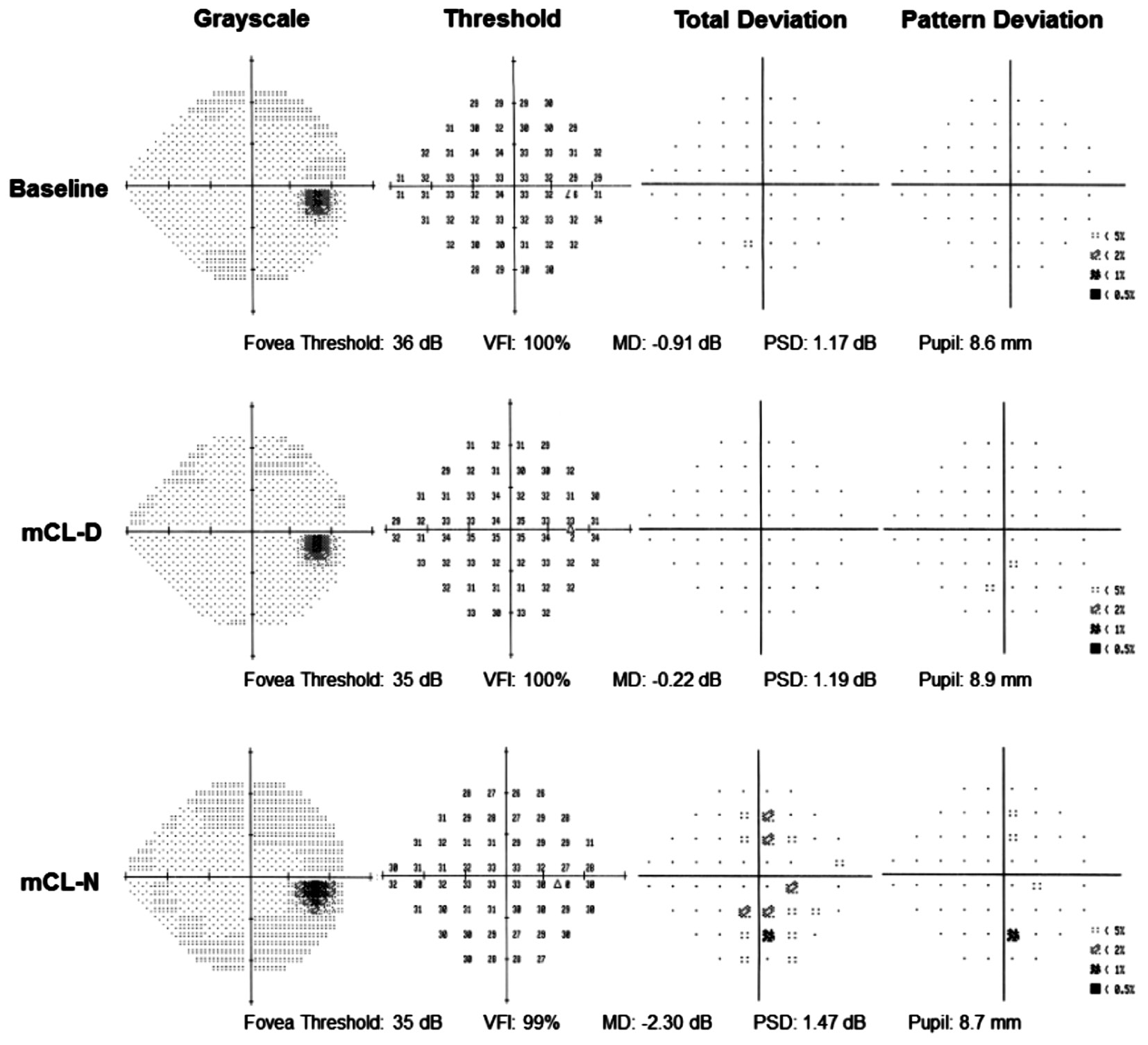
Figure 2 Representative results with three refractive corrections in the 24-2 test protocol Top: The result of monofocal contact lens (CL)corrected for near vision (Baseline). Middle: The result of multifocal CL corrected for distance vision (mCL-D). Bottom: The result of mCL-D and near additional correction by spectacle lens (mCL-N).

Figure 3 Representative results with three refractive corrections in the 10-2 test protocol Top: The results of monofocal contact lens (CL)corrected for near vision (Baseline). Middle: The result of multifocal CL corrected for distance vision (mCL-D). Bottom: The result of mCL-D and near additional correction by spectacle lens (mCL-N).
The foveal threshold with mCL-N also decreased by approximately 1.0 to 2.5 dB as compared with the baseline and mCL-D, similar to the MD findings. A previous study has reported that the foveal threshold was not significantly different between refractive multifocal CLs corrected for distance and monofocal CL corrected for near vision[19]. As with MD, the decreased foveal threshold of mCL-N may imply that visual performance tended to be near-dominant, even though distance correction is in fl uenced by the optical design of the multifocal CL used in the present study. However, the foveal threshold of mCL-D was significantly decreased with the 24-2 test protocol as compared with that of the baseline. It is highly unlikely that a learning effect occurred, given that the test order was randomized and that only perimetric experienced participants were recruited. In addition, the principle used for measuring the foveal threshold with both the 24-2 and 10-2 test protocols was the same. It is therefore highly unlikely that the foveal threshold of mCL-D decreased as compared with Baseline only with the 24-2 protocol, but we were unable to clarify the reason for this finding.
The pupil diameter for mCL-N was slightly larger than that for both the mCL-D and baseline. Although all participants underwent perimetric measurement using a random order of each refractive condition at 1h after instillation of a cyclopentolate hydrochloride agent, it is highly unlikely that the effect of the cyclopentolate hydrochloride and measurement order could be attributed to pupil diameter. It is more likely to be due to the effect of the shape of the spectacle lens of +3.00 diopter used for the mCL-N.
The test duration of the mCL-N was significantly longer,by 20.8-24.8s, in the 10-2 test point protocol. Although MD with mCL-N was almost the same in both the 24-2 and 10-2 test protocol, MDs with Baseline and mCL-D in the 10-2 test protocol tended to slightly better than those in the 24-2 protocol. Clinically, test time increases as visual field sensitivity decreases; hence, it is likely that the difference in visual field sensitivity affected test duration.
With the refractive multifocal CLs used in the current study,as pupil diameter increased, light directed to the near zone increased and visual performance tended to be near-dominant.In contrast, for refractive or diffractive multifocal IOLs[2,12]and refractive multifocal CLs[18], more light was directed at the distance zone, so that visual performance tended to be distance-dominant. Although a previous study comparing refractive multifocal IOLs (Array, AMO, Santa Ana, CA,USA) and monofocal IOLs (SI40NB, AMO) reported that contrast sensitivity in the near photopic and mesopic conditions was reduced with refractive multifocal IOLs, the contrast sensitivity of multifocal IOLs with near correction yielded better results than multifocal IOLs with distance correction.Although some diffractive multifocal IOLs (Tecnis Multifocal,AMO, Abbott Medical Optics, Santa Ana, CA, USA) are less affected by changes in the pupil size, because theoretically,the light directed at the distance and near zones are equal in both miosis and mydriasis, other types of diffractive multifocal IOL (SI40N, AMO or SA60D3, Alcon) tend to be distancedominant in mydriasis[2]. Therefore, refractive correction should be performed with care; the combination of the optical design of the lens and pupil size should be considered when administering the dome-shaped visual field test with refractive multifocal IOLs and CLs. However, the present study did not investigate these issues in detail and further studies should determine whether retinal sensitivity changes with near correction in eyes with diffractive multifocal IOLs.
This study has some limitations. First, the accommodative paralyzing agent that was used to replicate the multifocal IOL induced mydriasis of approximately 8-9 mm and thus the present study was not performed in the context of a natural or small pupil size. Second, the multifocal CL used in the present study had a refractive, rather than a diffractive design, which is commonly used in a clinical setting. Moreover, this study was performed with eyes with multifocal CLs, rather than multifocal IOLs. Third, neuroadaptation of approximately 6mo[27] are needed to obtain better SAP results with multifocal CLs.
In summary, despite the mydriasis induced by cyclopentolate hydrochloride and the optical design of the multifocal lens used in this study, our results indicate that, when the dome-shaped visual field test is performed with eyes with large pupils and wearing refractive multifocal CLs, distance correction without additional near correction is recommended.
ACKNOWLEDGEMENTS
Foundation: Supported by School of Allied Health Sciences,Kitasato University, Kanagawa, Japan.
Conflicts of Interest: Hirasawa K, None; Ito H, None; Ohori Y, None; Takano Y, None; Shoji N, None.
REFERENCES
1 Gundersen KG, Potvin R. Comparative visual performance with monofocal and multifocal intraocular lenses. Clin Ophthalmol 2013;7:1979-1985.
2 Bellucci R. Multifocal intraocular lenses. Curr Opin Ophthalmol 2005;16(1):33-37.
3 Martinez Palmer A, Gomez Faina P, Espana Albelda A, Comas Serrano M, Nahra Saad D, Castilla Cespedes M. Visual function with bilateral implantation of monofocal and multifocal intraocular lenses:a prospective, randomized, controlled clinical trial. J Refract Surg 2008;24(3):257-264.
4 Pepose JS, Qazi MA, Davies J, Doane JF, Loden JC, Sivalingham V, Mahmoud AM. Visual performance of patients with bilateral vs combination Crystalens, ReZoom, and ReSTOR intraocular lens implants.Am J Ophthalmol 2007;144(3):347-357.
5 Mester U, Hunold W, Wesendahl T, Kaymak H. Functional outcomes after implantation of Tecnis ZM900 and Array SA40 multifocal intraocular lenses. J Cataract Refract Surg 2007;33(6):1033-1040.
6 Williamson W, Poirier L, Coulon P, Verin P. Compared optical performances of multifocal and monofocal intraocular lenses (contrast sensitivity and dynamic visual acuity). Br J Ophthalmol 1994;78(4):249-251.
7 Boesten IE, Beekhuis WH, Hassmann E, Pameyer JH, Baarsma GS.Comparison of the Storz bifocal zonal and the 3M diffractive multifocal intraocular lenses. J Cataract Refract Surg 1995;21(4):437-441.
8 Gimbel HV, Sanders DR, Raanan MG. Visual and refractive results of multifocal intraocular lenses. Ophthalmology 1991;98(6):881-887.
9 Kamlesh, Dadeya S, Kaushik S. Contrast sensitivity and depth of focus with aspheric multifocal versus conventional monofocal intraocular lens.Can J Ophthalmol 2001;36(4):197-201.
10 Montés-Micó R, Alió JL. Distance and near contrast sensitivity function after multifocal intraocular lens implantation. J Cataract Refract Surg 2003;29(4):703-711.
11 Winther-Nielsen A, Gyldenkerne G, Corydon L. Contrast sensitivity,glare, and visual function: Diffractive multifocal versus bilateral monofocal intraocular lenses. J Cataract Refract Surg 1995;21(2):202-207.
12 Montés-Micó R, España E, Bueno I, Charman WN, Menezo JL.Visual performance with multifocal intraocular lenses: mesopic contrast sensitivity under distance and near conditions. Ophthalmology 2004;111(1):85-96.
13 Gifford P, Cannon T, Lee C, Lee D, Lee HF, Swarbrick HA. Ocular aberrations and visual function with multifocal versus single vision soft contact lenses. Cont Lens Anterior Eye 2013;36(2):66-73; quiz 103-104.
14 Llorente-Guillemot A, García-Lazaro S, Ferrer-Blasco T, Perez-Cambrodi RJ, Cerviño A. Visual performance with simultaneous vision multifocal contact lenses. Clin Exp Optom 2012;95(1):54-59.
15 García-Lázaro S, Ferrer-Blasco T, Madrid-Costa D, Albarrán-Diego C, Montés-Micó R. Visual performance of four simultaneous-image multifocal contact lenses under dim and glare conditions. Eye Contact Lens 2015;41(1):19-24.
16 Aychoua N, Junoy Montolio FG, Jansonius NM. Influence of multifocal intraocular lenses on standard automated perimetry test results.JAMA Ophthalmol 2013;131(4):481-485.
17 Farid M, Chak G, Garg S, Steinert RF. Reduction in mean deviation values in automated perimetry in eyes with multifocal compared to monofocal intraocular lens implants. Am J Ophthalmol 2014;158(2):227-231.e1.
18 Madrid-Costa D, Ruiz-Alcocer J, García-Lázaro S, Albarrán-Diego C,Ferrer-Blasco T. Effect of multizone refractive multifocal contact lenses on standard automated perimetry. Eye Contact Lens 2012;38(5):278-281.
19 Alongi S, Rolando M, Corallo G, Siniscalchi C, Monaco M, Saccà S,Verrastro G, Menoni S, Ravera GB, Calabria G. Quality of vision with presbyopic contact lens correction: subjective and light sensitivity rating.Graefes Arch Clin Exp Ophthalmol 2001;239(9):656-663.
20 Bi H, Cui Y, Ma X, Cai W, Wang G, Ji P, Xie X. Early clinical evaluation of AcrySof ReSTOR multifocal intraocular lens for treatment of cataract. Ophthalmologica 2008;222(1):11-16.
21 Anderson DR, Patella VM. Automated Static Perimetry. 2nd ed. St.Louis: Mosby; 1999.
22 Vanderschueren I, Zeyen T, D'Heer B. Multifocal IOL implantation: 16 cases. Br J Ophthalmol 1991;75(2):88-91.
23 Ichhpujani P, Bhartiya S, Sharma A. Premium IOLs in Glaucoma. J Curr Glaucoma Pract 2013;7(2):54-57.
24 Bojikian KD, Vita JB, Dal Forno CP, Tranjan Neto A, Moura CR. Does the apodized diffractive intraocular lens Acrysof ReSTOR Natural interfere with FDT Matrix perimetry results? Arq Bras Oftalmol 2009;72(6):755-759.
25 Pieh S, Marvan P, Lackner B, Hanselmayer G, Schmidinger G, Leitgeb R, Sticker M, Hitzenberger CK, Fercher AF, Skorpik C. Quantitative performance of bifocal and multifocal intraocular lenses in a model eye:point spread function in multifocal intraocular lenses. Arch Ophthalmol 2002;120(1):23-28.
26 Ravalico G, Parentin F, Sirotti P, Baccara F. Analysis of light energy distribution by multifocal intraocular lenses through an experimental optical model. J Cataract Refract Surg 1998;24(5):647-652.
27 Lubinski W, Podboraczynska-Jodko K, Gronkowska-Serafin J,Karczewicz D. Visual outcomes three and six months after implantation of diffractive and refractive multifocal IOL combinations. Klin Oczna 2011;113(7-9):209-215.