INTRODUCTION
Glaucoma management in the 21st century is a complex interplay of several factors not only guided by the Scientific rigour of evidence-based medicine, but also personal and anecdotal experiences gathered during years of practice. At the behest of several national, international and notional bodies in glaucoma, guidelines have been issued for management of various aetiologies of glaucoma, and though not irrevocable, a glaucomatologist is expected to work within that framework of standard precept.
India is a large country with approximately 11.2 million persons aged 40y and older with glaucoma. Moreover,majority of those with disease are undetected and there exists major challenges in detecting and treating these[1]. While the data regarding practice patterns of glaucoma are available from surveys performed in the developed world (USA[2-9], UK[10-14],
Australia and New Zealand[15], and Canada[16]) there is paucity of information originating in developing countries, including India.
Furthermore, previously conducted surveys on practice patterns of glaucoma were either comprehensive covering broad principles of diagnosis and management of glaucoma[15-16]or were focused only on specific areas of glaucoma care[2-14].
Moreover, while some previous surveys were of glaucoma specialists[2-11], others included general ophthalmologists as well[12-16]. The information on the prevailing practice patterns of the specialists in the diagnosis and management of glaucoma in India is discussed in this comprehensive survey, with reference to how these compare with the practice patterns in other parts of the world and the current evidence base.
SUBJECTS AND METHODS
This survey was conducted under the aegis of the Glaucoma Society of India (GSI); this body holds a meeting every year and the registered ophthalmologists at the annual conference in Indore, India in 2013 participated in this survey of glaucoma practice patterns.
Development of the Questionnaire At the outset, we developed a pilot questionnaire similar to several previously conducted surveys on glaucoma practice patterns, but keeping regional differences in mind [2,3,5-17]. This questionnaire was administered and the responses were analysed using an interactive audience response system (ARS), with keypads, to a mixed sample of ophthalmologists attending another national meeting[18]. This exercise was done a priori to ensure that the format covered all the relevant questions, was simple to answer, and that the response could be accurately interpreted and analysed.Feedback was obtained and it assisted us in modifying the pilot questionnaire, so that we could set it up for the current study.
Questionnaire Design The questionnaire consisted of thirty-five questions in multiple choice format. The first four questions were general in nature to determine nature of training received in ophthalmology, years of experience, type of practice (institutional, private, etc.), and the proportion of glaucoma patients managed in that practice. The subsequent questions concentrated on management issues-these included practice patterns related to clinical diagnosis, use of investigative procedures such as visual fields and optic nerve head or retinal nerve fibre layer (RNFL) imaging, and preferences with respect to medical and surgical interventions.
Administration of the Questionnaire The questionnaire was administered to the ophthalmologists attending the Annual Conference of GSI held in 2013. An ARS identical to the one used in the pilot exercise was used for this survey. Participation in the survey was entirely voluntary and there was no financial compensation for participating in it. No personal details were asked and confidentiality of response was maintained throughout.
Statistical Analysis The results were cross-tabulated by subdividing respondents with respect to experience and subspeciality training in glaucoma. Differences in categorical data were analysed using Chi-square test or Fisher’s exact test as appropriate, and the alpha error was set at P<0.05. A logistic regression model was used to study whether speciality training in glaucoma had any influence on the preferred practices in the diagnosis or management of glaucoma. The information collated is primarily descriptive. Statistical analysis was done using commercial software (Stataver. 11.2; StataCorp, College Station, TX, USA).
RESULTS

Figure 1 The subdivision of glaucoma specialists based on their years of experience in managing patients with glaucoma.
Demography There were 647 ophthalmology professionals who registered for the meeting, out of which 441 (68.1%)participated in the survey. Information obtained from 146(33.1%) participants was analysed, as these were glaucoma specialists.
Approximately half of the specialists (n=74, 50.6%) were in ophthalmic institution based practice whilst a quarter of the specialists (n=37, 25.3%) were in private practice. More than half of the specialists (n=83, 56.8%) had ≥10y of experience and about a third (n=49, 33.5%) had >15y of experience in managing glaucoma (Figure 1). Glaucoma patients made up more than half the outpatient volume for n=57 (41.3%)specialists. Patients with angle closure disease made up more than a quarter of the outpatient volume for n=79 (57.2%)specialists.
Practice Pattern Related to Glaucoma Diagnosis Goldmann applanation tonometry (GAT) was preferred by n=103 (72%)specialists whilst n=25 (17.4%) used non-contact tonometer.Additionally, six (4.2%) specialists reported regular use of Schiotz tonometer, whilst eight (5.5%) glaucoma specialists reported not checking intra ocular pressure (IOP) in all patients.
One hundred and fourteen (82.6%) reported doing gonioscopy in all patients with glaucoma or those that were suspects, whilst n=20 of the remaining (14.4%) preferred to do so only when peripheral anterior chamber depth was shallow and/or IOP was raised, or did not perform it at all. Indentation gonioscopy was favoured by two-thirds (n=90, 66%) and about a third (n=43,31.3%) reported use of either a two- or a three-mirror goniolens, when choice of gonio-prism was enquired. Slit-lamp biomicroscopy was the preferred modality for assessment of the optic disc by majority of the specialists (n=115, 85.8%),and a third (n=42, 32.3%) also routinely obtained optic disc photographs in patients with glaucoma.
Table 1 The choice of first line anti-glaucoma medication and combination anti-glaucoma medications by glaucomatologists in primary open angle glaucoma

Practice Pattern Related to Investigations in Glaucoma The majority of specialists surveyed (n=114; 83.2%) reported use of Humphrey Visual Field Analyser (Carl Zeiss Meditec,Dublin, CA, USA) for perimetry; a significant minority (n=12,8.7%) were using the Octopus perimeter. An overwhelming majority had access to optic disc or RNFL imaging, except for 5 (3.7%). A third of the specialists (n=46, 34%) advised optic disc or RNFL imaging in <25% glaucoma patients while another third (n=58, 42.9%) reported obtaining optic disc or RNFL imaging in >50% patients with glaucoma in their practice. Suspicious optic discs with normal visual fields was the most common indication for obtaining optic disc or RNFL imaging (n=101, 76.5%). The majority of specialists (n=96;72.1%) preferred optical coherence tomography (OCT). Eleven(8.3%) specialists indicated that they initiated anti-glaucoma therapy in patients with abnormal optic disc or RNFL imaging despite IOP and visual fields being normal.
Practice Pattern Related to Glaucoma Management efficacy of anti-glaucoma medication was an important factor considered while prescribing an anti-glaucoma medication by about two-thirds, (n=94; 70.6%) whilst one-fifths laid stress on patient affordability (n=26, 19.5%). Preferred choice of the anti-glaucoma medication by the glaucoma specialists in primary open angle glaucoma is shown in Table 1. Majority of the glaucoma specialists surveyed (n=103; 84.4%) steppedup anti-glaucoma treatment when optic disc or visual field progression was seen whilst 10.6% (n=3) specialists did so on the basis of absolute IOP value and another 4.1% (n=5)specialists did so on the basis of inter-visit IOP fl uctuation.
The response of the specialists on unilateral drug trial in normal tension glaucoma (NTG) was diverse. Twenty two(17.1%) specialists did it routinely, 31.2% (n=40) considered it only when the damage was asymmetric, 24.2% (n=31)specialists did not think unilateral drug trial was required in NTG whilst 27.3% (n=35) did not comment.
An overwhelming majority (n=117, 92.8%) reported laser iridotomy as their primary choice of treatment for angle closure disease whilst a third (n=38; 35.1%) were in favour of performing it in all angle closure suspects as well. Three(2.3%) specialists preferred lens extraction and 1.5% (n=2)reported filtering surgery as primary procedure in angle closure disease. Post-iridotomy gonioscopy was routinely performedby 70.5% (n=96), a quarter (n= 33, 24.2%) considered it only when peripheral anterior chamber depth was suspicious or IOP was raised and 5.1% (n=7) did not do it at all. Pilocarpine was the primary management approach to post-iridotomy occludable angles by 45.8% (n=60) specialists (Table 2).
Table 2 The primary approach of glaucoma specialists to occludable drainage angle despite a functional iridotomy

Trabeculectomy with (n=94, 69.6%) or without anti- fibrotics(n=33, 24.4%) to control primary adult glaucoma was the preferred surgical modality of two-thirds and one-fourths specialists respectively. An overwhelming majority (n=122,91%) preferentially used mitomycin C (MMC) as their firstchoice anti-fibrotic agent. The majority (n=97; 73.4%) also preferred making a fornix-based conjunctival flap when performing trabeculectomy and approximately half of the specialists (n=67; 51.1%) reported placing releasable sutures.Approximately only a third of the specialists surveyed (n=37;28%) were performing trabeculectomy as well as implantation of a glaucoma drainage device and about half (n=64; 47%)were not operating on congenital glaucoma at all. The more experienced glaucoma specialists (>10y of experience)differed from lesser experienced glaucoma specialists (<10y of experience) in their performance of surgery for congenital glaucoma (P=0.02).
With respect to combined cataract and filtering surgery, 48.1%(n=53) glaucoma specialists did so when IOP was uncontrolled on a single anti-glaucoma medication or at the most, a combination drug, whilst 25.4% (n=28) preferred to perform combined surgery either when IOP was uncontrolled or when there was threat to fixation on 24-2 perimetry.
Eighty (61.5%) specialists reported patient referral for low vision aids on the basis of activity limitation (Table 3; online supplementary material). Forty eight (38.1%) specialists reported using Scientific journals to upgrade knowledge (Table 4;online supplementary material).
Table 3 Basis of patient referral for low vision aids by the glaucoma specialists
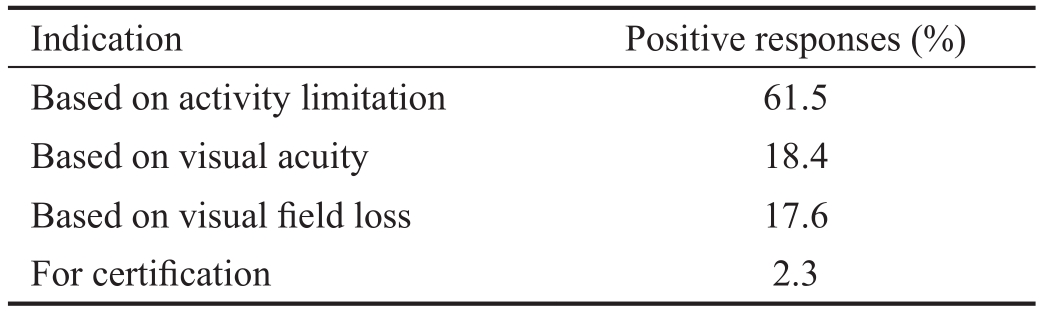
Table 4 Preferred mode of knowledge upgrading by the glaucoma specialists

DISCUSSION
We conducted this survey to discern the practice patterns of glaucoma amongst specialists, in the country. While on the one hand it demonstrated congruence with preferred practice patterns across the breadth of diagnosis and management of glaucoma, there were significant exceptions.
Our survey was conducted using a novel response system in the form of interactive electronic ARS with keypads; use of this guaranteed anonymity. All questions were administered in the form of multiple choice and participants registered their responses live, by using the voting keypad. All previous surveys on glaucoma specialists have been executed by administering paper questionnaire/s to the participants and obtaining reply by mail[2-16]. Participation rate of the identified participants is a major concern in such paper surveys. This is evident in the response rates of 22% in the survey of American Glaucoma Society[2] and 46% in a survey in UK[11] when compared with the response rate of 68% in our survey. Low response rates may induce participant bias. The perceived limitation on concealing the identity of the participants can influence the response rate related to such surveys. The key benefits for using the ARS includes improvement in participation rate, attention levels, and engagement, besides improvised data collection. These advantages are worth the challenges of ARS, viz time needed to learn and set up the ARS technology, creating effective ARS questions, and ability to appropriately handle the data[19]. A-priori administration of a pilot questionnaire in an identical format to a smaller sample of ophthalmologists helped us circumnavigate some of these challenges[18].
The survey reveals certain areas of non-uniform adherence to glaucoma society guidelines for diagnosis of glaucoma[20]. The existing quality of evidence is formidable in this segment and the recommendations are robust. The guidelines recommend Goldmann-style applanation tonometry and Tonopen if GAT is unavailable[20]. However, a considerable proportion of glaucoma specialists (28%) reported routinely using non Goldmann-style applanation tonometers with 17% using non-contact tonometry. Since IOP is the only modifiable risk factor for glaucoma and most of the clinical decisions in glaucoma are made based on IOP, the practice of using non Goldmann-style applanation tonometers may have significant implications on the management of such patients. The Asia Pacific Glaucoma (APG) guidelines recommend a gonioscope that allows indentation gonioscopy as one of the minimal acceptable resources for examination[20]. Nevertheless, only 66%glaucoma specialists reported doing indentation gonioscopy in this survey. The guidelines also recommend considering serial optic nerve head photographs, if not optic nerve imaging, as resources vary widely across the Asia-Pacific region[20]. Though most of the glaucoma specialists reported examining the optic disc stereoscopically, only a third glaucoma specialists managed to obtain optic disc photographs routinely in patients with glaucoma.
In contrast to recommendations in clinical diagnosis of glaucoma,guidelines related to imaging are less robust. Quantitative assessment of optic disc and RNFL with imaging is useful but has limited ability to diagnose early disease[21]. The consensus of the World Glaucoma Association (WGA) has described only a complementary role of glaucoma imaging in detecting progression[21]. The variability in the proportions of patients advised to undergo glaucoma imaging by the specialists participating in this survey may indirectly highlight the evolving role of imaging in glaucoma. The practice of initiating anti-glaucoma therapy in patients with abnormal optic disc or RNFL imaging alone, despite IOP being normal,should be discouraged, when, in fact, the decision of initiation or reinforcement of treatment should depend on the likelihood of developing significant functional impairment during a patient’s life time[21].
The rates of primary angle closure disease are higher among Asians than in other populations, despite substantially varied rates between studies[20]. Therefore, the prevalence of plateau iris syndrome (PIS), a subtype of primary angle closure disease, is expected to be higher in this region. Appropriate treatment of the blockade of trabecular mesh work at the level of the ciliary body, as seen in PIS is more complex than that at the level of iris typified by pupillary block[22]. The prevalence of PIS as assessed previously, in an exclusive Caucasian population in young patients with recurrent angle closure symptoms despite initial iridotomy or iridectomy, was reported to be as high as 54%[23]. Post iridotomy gonioscopy is thus essential to detect cases of PIS, especially since ultrasound biomicroscopy may not be available, due to its cost, or may not be practical to perform in every case of angle closure disease[24]. Only about 70% of glaucoma specialists who participated in this survey were reportedly performing post iridotomy gonioscopy. Efforts to improve this practice should be made, as this will increase detection rates for this aggressive subtype of angle closure disease.
Currently, no specific imaging modality can be regarded as the perfect reference standard for detection of glaucomatous structural progression[21]. Optical coherence tomography was the most preferred imaging modality in our survey. This is in contrast to a survey in UK where Heidelberg retinal tomography was the most preferred optic nerve imaging modality despite better availability of OCT[13]. The preference for OCT in our country may be linked to its greater versatility and availability owing to a wider clinical application across other sub-specialties.
With regard to the choice of anti-fibrotic agents during trabeculectomy, the majority of glaucoma specialists (91%)selected MMC in this survey, while only 5 (3.7%) glaucoma specialists denied usage of anti-metabolite in glaucoma surgery. The preference for MMC may be related to the advent of newer and more effective anti-glaucoma medications leading to a shift towards a higher risk in the pro file of patients undergoing trabeculectomy. Though the same agent is most preferred in America and Japan as well[2,17], 5-fluorouracil(5-FU) appears to be the most preferred anti-metabolite in UK[14]. This may be because the particular anti-metabolite survey was done more than a decade ago, in January 2000,with emphasis on prevalent risk factors for conjunctival scarring or it may simply be a result of popular practice in UK,with the emphasis being on relative safety of 5-FU compared to MMC[14].
The use of glaucoma drainage device (GDD) is on the rise and this was evident in the survey of the American Glaucoma Society[2]. Mean GDD usage increased from 17% in 1996 to 50% in 2008, and mean trabeculectomy usage decreased from 80% in 1996 to 45% in 2008. However, in our survey, only 28% glaucoma specialists reported doing GDD implantation.This may be alluding to the fact that most glaucoma in our country is perhaps actually being managed by self-proclaimed glaucoma specialists, rather than fellowship trained ones, of which there is a dearth vis-à-vis the population served. Several limitations of residency training have also been unearthed in our system, which makes delivery of specialist glaucoma services sketchy at best of times[25].
We acknowledge that several limitations may have crept in: selection bias due to non-participation of the other attendees and the very fact that it was conducted at a national level glaucoma conference, can induce a selection bias.Consequently, the stated practice of these glaucoma specialists may not be wholly representative of the average care delivered in glaucoma across all sectors of healthcare and society in India. The lack of a direct question enquiring about fellowship training was a limitation too. Furthermore the format of questioning (multiple choice) limits the number of responses to only those offered. Also, live voting via an ARS provides a limited time allowance to respond to the multiple choice format, leading to inadvertent errors. Exercises of this kind are also prone to recall bias.
In conclusion, this survey is the first of its kind in India and,in its usage of the interactive ARS, possibly the first of its kind in the world. It has found conformance with preferred practice patterns in several areas of diagnosis and management of glaucoma, but there was diversity in other aspects. The reported information should help practising glaucoma specialists to compare their own practices with those of their colleagues. This information is an important step towards improvement of glaucoma care in India, including planning for future strategies.
Note: Though 146 glaucomatologits participated in this survey,the number of respondents to each question was variable.The percentage of respondents is calculated on the basis of respondents to that particular question.
ACKNOWLEDGEMENTS
Presented as a poster at World Glaucoma Congress 2015, Hong Kong. Alcon supported procuring of the Audience Response System.
Conflicts of Interest: Choudhari NS, None; Pathak-Ray V,None; Kaushik S, None; Vyas P, None; George R, None.
REFERENCES
1 George R, Ve RS, Vijaya L. Glaucoma in India: estimated burden of disease. J Glaucoma 2010;19(6):391-397.
2 Desai MA, Gedde SJ, Feuer WJ, Shi W, Chen PP, Parrish RK 2nd.Practice preferences for glaucoma surgery: a survey of the American Glaucoma Society in 2008. Ophthalmic Surg Lasers Imaging 2011;42(3):202-208.
3 Joshi AB, Parrish RK 2nd, Feuer WF. 2002 survey of the American Glaucoma Society: practice preferences for glaucoma surgery and anti fibrotic use. J Glaucoma 2005;14(2):172-174.
4 Jampel HD, Parekh P, Johnson E, Robin AL, Miller RB. Preferences for eye drop characteristics among glaucoma specialists: a willingness-to-pay analysis. J Glaucoma 2005;14(2):151-156.
5 Reynolds AC, Skuta GL, Monlux R, Johnson J. Management of blebitis by members of the American Glaucoma Society: a survey. J Glaucoma 2001;10(4):340-347.
6 Salvo EC Jr, Luntz MH, Medow NB. Use of viscoelastics posttrabeculectomy: a survey of members of the American Glaucoma Society.Ophthalmic Surg Lasers 1999;30(4):271-275.
7 Davidorf JM, Baker ND, Derick R. Treatment of the fellow eye in acute angle-closure glaucoma: a case report and survey of members of the American Glaucoma Society. J Glaucoma 1996;5(4):228-232.
8 Wand M, Quintiliani R, Robinson A. Antibiotic prophylaxis in eyes with filtration blebs: survey of glaucoma specialists, microbiological study, and recommendations. J Glaucoma 1995;4(2):103-109.
9 Schwartz AL. Argon Laser Trabeculoplasty in Glaucoma: What’s Happening (Survey Results of American Glaucoma Society Members). J Glaucoma 1993;2(4):329-336.
10 Tailor R, Batra R, Mohamed S. A National Survey of Glaucoma Specialists on the Preoperative (Trabeculectomy) Management of the Ocular Surface. Semin Ophthalmol 2016;31(6):519-525.
11 Malik R, Baker H, Russell RA, Crabb DP. A survey of attitudes of glaucoma sub-specialists in England and Wales to visual field test intervals in relation to NICE guidelines. BMJ Open 2013;3(5).pii:e002067
12 Stead R, Azuara-Blanco A, King AJ. Attitudes of consultant ophthalmologists in the UK to initial management of glaucoma patients presenting with severe visual field loss: a national survey. Clin Experiment Ophthalmol 2011;39(9):858-864.
13 Gordon-Bennett PS, Ioannidis AS, Papageorgiou K, Andreou PS. A survey of investigations used for the management of glaucoma in hospital service in the United Kingdom. Eye (Lond) 2008;22(11):1410-1418.
14 Siriwardena D, Edmunds B, Wormald RP, Khaw PT. National survey of antimetabolite use in glaucoma surgery in the United Kingdom. Br J Ophthalmol 2004;88(7):873-876.
15 Gaskin BJ, Carroll SC, Gamble G, Goldberg I, Danesh-Meyer HV.Glaucoma management trends in Australia and New Zealand. Clin Experiment Ophthalmol 2006;34(3):208-212.
16 Schertzer RM, Orton T, Pratt D. Practice patterns of Canadian glaucoma specialists: planning for the next generation. Can J Ophthalmol 2007;42(4):580-584.
17 Chen PP, Yamamoto T, Sawada A, Parrish RK 2nd, Kitazawa Y. Use of anti fi brosis agents and glaucoma drainage devices in the American and Japanese Glaucoma Societies. J Glaucoma 1997;6(3):192-196.
18 Chandran P, Choudhari NS, Pathak-Ray V, Dave P. Glaucoma practice patterns. E Poster (Poster No.: EP-0514) presented at the Congress of the Asia-Pacific Academy of Ophthalmology held in conjunction with the 71st Annual Conference of the All India Ophthalmological Society at Hyderabad, India in January 2013. Abstract book available at: http://www.aios.org/aioc13abstractbook.pdf. Accessed April 29, 2015.
19 Kay RH, LeSage A. Examining the benefits and challenges of using audience response systems: A review of the literature. Computers and education 2009;53:819-827.
20 Asia Pacific Glaucoma Guidelines. South East Asia Glaucoma Interest Group. Available at:http://www.apglaucomasociety.org/toc/APGG2_fullversionNMview.pdf. Accessed March 27, 2015.
21 Garway-Heath T, Kotecha A, Lerner F, Dayanir V, Brandt J, Pepose J, et al. Measurement of intraocular pressure. In: Weinreb RN, Brandt JD, Garway-Heath DF, Leung C (eds). World Glaucoma Association:Intraocular pressure: Consensus series-4. Kugler publications:Amsterdam, 2007, pp 45-90.
22 Ritch R, Lowe RF. In: Ritch R, Shields MB, Krupin T, eds. The Glaucomas. St. Louis: Mosby; 1996:801.
23 Stieger R, Kniestedt C, Sutter F, Bachmann LM, Stuermer J.Prevalence of plateau iris syndrome in young patients with recurrent angle closure. Clin Experiment Ophthalmol 2007;35(5):409-413.
24 Kiuchi Y, Kanamoto T, Nakamura T. Double hump sign in indentation gonioscopy is correlated with presence of plateau iris configuration regardless of patent iridotomy. J Glaucoma 2009;18(2):161-164.
25 Thomas R, Dogra M. An evaluation of medical college departments of ophthalmology in India and change following provision of modern instrumentation and training. Indian J Ophthalmol 2008;56(1):9-16.