Dear Editor,
I am Dr. Xiu Wang, from Tianjin Medical University Eye Hospital, Tianjin, China. I write to present one case report of Posner-Schlossman syndrome (PSS) induced laser in situ keratomileusis (LASIK) keratectasia.PSS is a condition characterized by recurrent, acute attacks of mild, unilateral, non-granulomatous, anterior uveitis accompanied by markedly elevated intraocular pressure (IOP)[1].
We report a patient who underwent LASIK surgery for myopia and developed PSS a year after the LASIK surgery, causing transient LASIK keratectasia. Written informed consent was obtained from the patient for publication of this case report and any accompanying images. When appropriate the patient can share their perspective on the treatments they received.
A twenty-nine years old man underwent bilateral LASIK procedures for the treatment of myopia on December 13,2013. His preoperative manifest refraction were: OD, -5.25-0.50×95=1.2; OS, -6.00-0.25×30=1.2. Preoperative corneal tomography with the Pentacam (Oculus Optikgerate GmbH,Wetzlar, Germany) was normal in both eyes (Figure 1) and LASIK was performed with Intralase (USA) and VISX STAR S4 (USA). The uncorrected vision acuity (VA) in both eyes were 1.2 (20/16) at one year follow up. The patient reported blurring of vision in the right eye a year later. The unaided VA was 0.1 (20/200) in the right eye and 1.2 (20/16) in the left eye. IOP, measured by a Goldmann applanation tonometer(GAT; Haag-Streit AG, Bern, Switzerland), was 34 mm Hg in the right eye and 9 mm Hg in the left eye. Mild edema was observed in the right cornea, with inflammation in the anterior chamber characterized by a few keratic precipitates (KPs) and anterior chamber flare (++) (Figure 2). Gonioscopy showed open angles in both eyes. Fundal examination revealed cupto-disc ratio of approximately 0.3 in the right eye. Automated visual testing showed normal visual fields in both eyes. The above findings are consistent with the diagnosis of PSS.Pentacam revealed a steepening of the corneal curvature centrally (Figure 3). Manifest refraction of the right eye showed a significant increase in myopia and astigmatism(-3.25-2.87×1=1.0).
His condition resolved with the following eye drops and medication: brinzolamida (s.a. Alcon-Couvreurn.v. USA)t.i.d. 2% cartelol hydrochloride (Otsuka Pharmaceutical Co.,Ltd., China) b.i.d., prednisolone acetate (Allergan, Westport,Co., Mayo, Ireland) t.i.d. and 25 mg diamox b.i.d. (Baoling,Hangzhou, China). After a week, the VA of his right eye was 1.2 (20/16) and IOP was 9.2 mm Hg. Anterior chamber flare was negative and the right cornea was clear, though there was a single KP remaining on the corneal endothelium(Figure 4). Prednisolone acetate q.i.d. and pranpulin t.i.d.was continued to reduce the inflammatory reaction and was slowly tapered before complete cessation after three weeks.Corneal tomography of the right eye 2wk after treatment of PSS showed central flattening of the cornea and resolution of the keratectasia (Figure 5). The axial and front elevation maps showed a central flattening of the right cornea consistent with myopic LASIK treatment with complete resolution of the keratectasia. Corneal tomography of the right eye 5mo after treatment of PSS showed central flattening of the cornea and resolution of the keratectasia (Figure 6). The cornea remained fl at centrally with no evidence of keratectasia.
LASIK is a safe procedure with good visual outcomes[2].However, there are some complications that have been reported[3]. Corneal keratectasia, which can occur up to several months after surgery[4], is one of the long-term complications of LASIK. The potential risk factors include high attempted correction, thin residual corneal thickness, flap creation,irregular corneal topography and undiagnosed subclinical keratoconus[5]. In a recent report on a long-term follow-up of a large number of cases, it was found that the incidence of corneal keratectasia after myopic LASIK was 0.57%[3].Although corneal keratectasia after refractive surgery is a rare event, it is visually disabling to the patient.

Figure 1 Preoperative corneal tomography showing a normal pattern.

Figure 2 Posner-Schlossman’s syndrome with keratic precipitates.
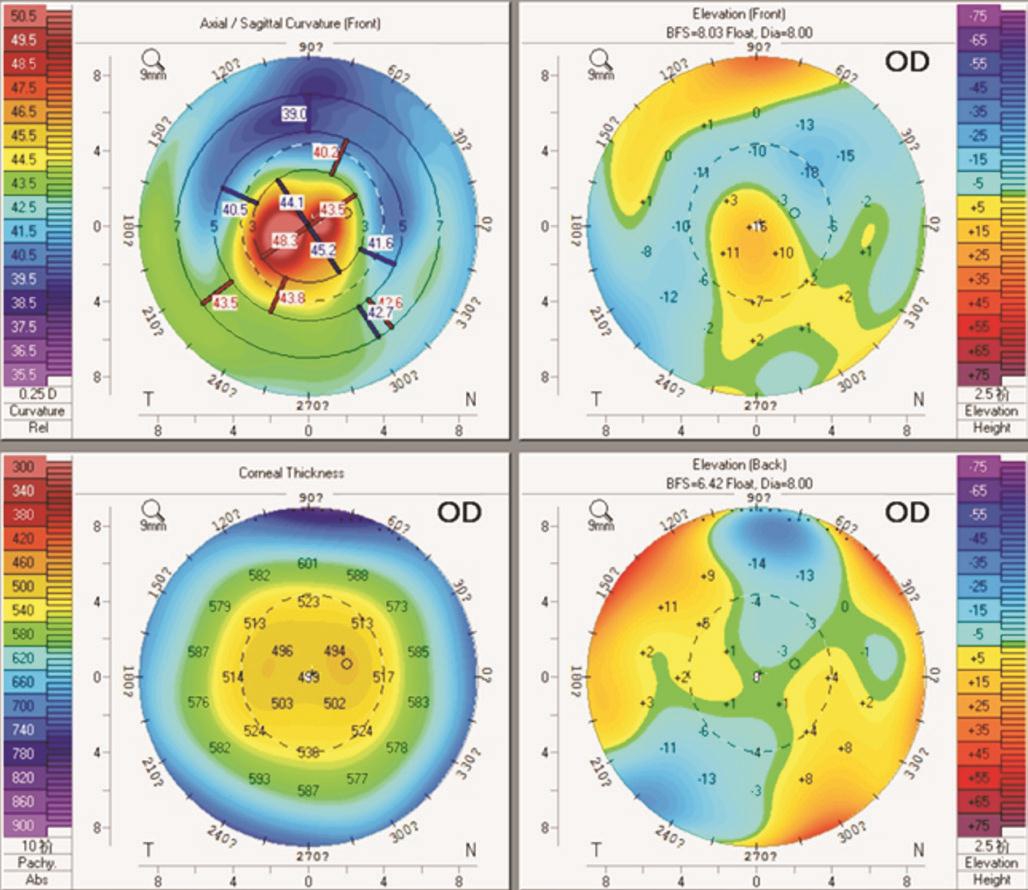
Figure 3 Corneal tomography of the right eye showing a central steep pattern suggestive of corneal keratectasia.
The patient described in this case report had a typical manifestation of PSS, characterized by recurrent episodes of elevated IOP, mild anterior chamber inflammation with a few KPs and anterior chamber fl are. The most important risk factor for corneal keratectasia in this patient is the elevated IOP. The relationship between VA, IOP, mean K and manifest spherical equivalent (MSE) over time was evaluated (Table 1).
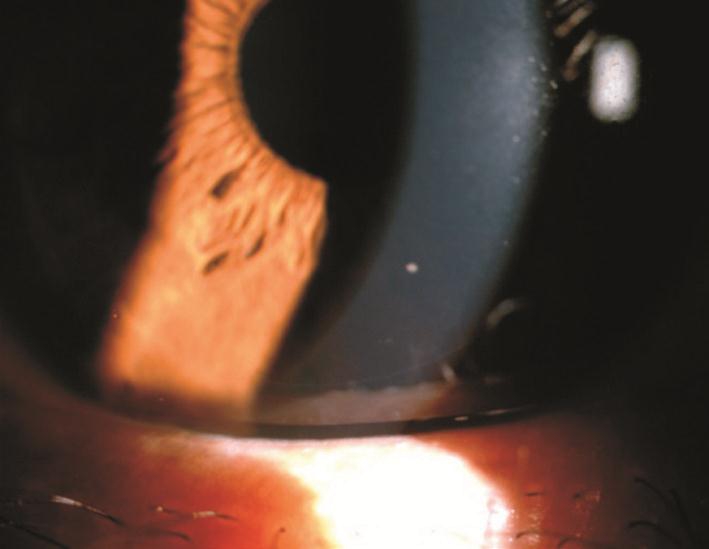
Figure 4 Resolution of Posner-Schlossman’s episode with a single KP remaining and anterior chamber fl are was negative.

Figure 5 Corneal tomography of the right eye 2wk after treatment of PSS showing central flattening of the cornea and resolution of the keratectasia.

Figure 6 Corneal tomography of the right eye 5mo after treatment of PSS showing central flattening of the cornea and resolution of the keratectasia.
Table 1 Relationship between VA, IOP, mean K and MSE over time
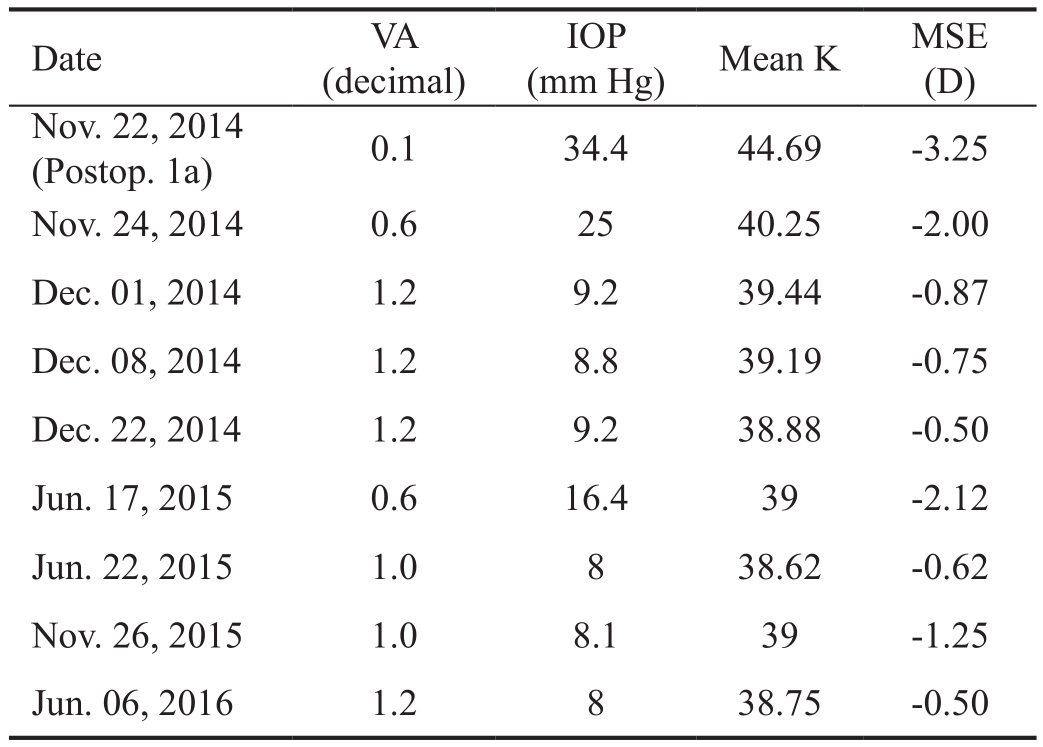
IOP: Intraocular pressure; MSE: Manifest spherical equivalent; Mean K: Mean keratometry; OD: Right eye.
There was positive correlation between MSE and mean keratometry (mean K) change for this patient (P=0.005,r=0.835). The increase in IOP had positive correlation with mean K (P=0.001, r=0.896) and negative correlation with VA(P=0.000, r=-0.943). High IOP pushes the post-LASIK thinned cornea forward resulting in an elevated mean K, causing a myopic shift in the MSE. The majority of current methods for measuring IOP make assumptions about corneal biomechanical parameters[6] which are altered after LASIK. The IOP reduction after LASIK is strongly correlated to the amount of myopia corrected, with 0.40 mm Hg (95% CI 0.39-0.41) reduction per diopter of myopic correction[7].
IOP may be one of risk factors for the development of post-LASIK keratectasia. Relative weakness in corneal shear leads to keratectasia[8]. Activities involving IOP spikes that are larger than those due to diurnal changes may be associated with larger corneal and refractive changes[9]. A high IOP acting on a cornea weakened by refractive surgery can provoke corneal steepening, inducing refractive changes even in the absence of keratectasia. The initial event that leads to PSS is an inflammation in the anterior chamber[10]and PSS is now recognised as an uncommon cause of chronic secondary glaucoma[11]. During an acute attack, also referred to as glaucomatocyclitic crisis, the IOP is usually high (40-60 mm Hg) and is the cause of the transient keratectasia seen in this patient. Hypotensive treatment of our patient led to resolution of the keratectasia. The clinical course of our patient differs from that reported by Razeghinejad et al[12], where a patient with post-LASIK keratectasia and primary open angle glaucoma had persistent keratectasia despite anti-glaucoma treatment and required rigid gas permeable contact lenses for vision correction, and possibly even requiring corneal transplantation and/or glaucoma filtration surgery in the future.In contrast, our patient had transient keratectasia with full resolution once IOP returned to normal.
We report a case of post LASIK PSS resulting in transient LASIK keratectasia. Resolution of the PSS with medication resulted in correction of the LASIK keratectasia. Monitoring IOP is important after LASIK surgery. Our case report illustrates the development of keratectasia following raised IOP. We suggest that screening for PSS as a possible risk factor will limit the incidence of keratectasia in these patients.
ACKNOWLEDGEMENTS
The authors thank the patient who generously agreed to participate in this report.
Authors’ contributions: Xiu Wang: Patient interaction,drafting manuscript; Elizabeth WL Lim and Li Lim: Editing the manuscript, including analysis and interpretation of data and drafting and revising the work for intellectual content.All authors read and approved the final manuscript. Rui-Hua Wei: Patient interaction, diagnosis, treatment, modification of manuscript.
Conflicts of Interest: Wang X, None; Lim EWL, None; Lim L, None; Wei RH, None.
REFERENCES
1 Posner A, Schlossman A. Syndrome of unilateral recurrent attacks of glaucoma with cyclitic symptoms. Arch Ophthal 1948;39(4):517-535.
2 Sugar A, Rapuano CJ, Culbertson WW, Huang D, Varley GA, Agapitos PJ, de Luise VP, Koch DD. Laser in situ keratomileusis for myopia and astigmatism: safety and efficacy: a report by the American Academy of Ophthalmology. Ophthalmology 2002;109(1):175-187.
3 Spadea L, Cantera E, Cortes M, Conocchia NE, Stewart CW. Corneal ectasia after myopic laser in situ keratomileusis: a long-term study. Clin Ophthalmol 2012;6:1801-1813.
4 Randleman JB. Post-laser in-situ keratomileusis ectasia: current understanding and future directions. Curr Opin Ophthalmol 2006;17(4):406-412.
5 Randleman JB, Russell B, Ward MA, Thompson KP, Stulting RD. Risk factors and prognosis for corneal ectasia after LASIK. Ophthalmology 2003;110(2):267-275.
6 Stamper RL. A history of intraocular pressure and its measurement.Optom Vis Sci 2011;88(1):E16-E28.
7 Schallhorn JM, Schallhorn SC, Ou Y. Factors that influence intraocular pressure changes after myopic and hyperopic LASIK and photorefractive keratectomy: a large population study. Ophthalmology 2015;122(3):471-479.
8 Dupps WJ Jr. Biomechanical modeling of corneal ectasia. J Refract Surg 2005;21(2):186-190.
9 McMonnies CW. Intraocular pressure spikes in keratectasia, axial myopia and glaucoma. Optom Vis Sci 2008;85(10):1018-1026.
10 Megaw R, Agarwal PK, Posner-Schlossman syndrome. Surv Ophthalmol 2017;62(3):277-285.
11 Jap A, Sivakumar M, Chee SP. Is Posner Schlossman syndrome benign? Ophthalmology 2001;108(5):913-918.
12 Razeghinejad MR, Nouri-Mahdavi K, Perera S. Primary open angle glaucoma and post-LASIK keratectasia. J Ophthalmic Vis Res 2010;5(3):196-201.