Dear Editor,
M ansonella ozzardi, one of many filarial nematodes exclusively found in parts of Latin America, is one of two Mansonella sp which cause mansonelliasis, an infestation first described by Sir Patrick Manson, the founder of the field of tropical medicine[1-2]. The third-stage larvae of this vector-borne human parasite is transmitted into its primary host, a human, by small blood-sucking arthropods namely,midges or black fl ies[3]. The first vector, a small biting midge(Culicoidesfurens) breeds on sandy beaches near the sea[4].
The second vector, the black fl y is a larger blood-sucking insect and there are two species of black fl ies (Simuliumamazonicum and Simuliumneavei) which can transmit the disease[4]. Both S.amazonicum and S. Neavei breed in fast- fl owing streams and rivers[4]. We report a case of mansonelliasis presenting with fl uctuating upper eyelid swelling. To our knowledge there are no previous reports of orbital invasion by Mansonella ozzardi in humans.
Case Report
A 33-year-old male presented with an intermittent left upper eyelid swelling. Of note he travelled to Tulum in Mexico close to a nature reserve where only biodegradable insect repellents could be used and also fresh water pools which both him and his partner swam in. The initial presentation had resembled asymmetrical blepharitis and he received a 6-week course of doxycycline for this. He also underwent an incision and curettage procedure for a left upper eyelid swelling which was thought to be due to a chalazion one month prior to his referral to us. Although the eyelid swelling improved initially it recurred upon cessation of doxycycline (Figure 1A). He was prescribed a 10d course of oral cipro fl oxacin with which the eye lid swelling reduced. He was still on oral ciprofloxacin when he was referred to us for further investigation/treatment.A computed tomography (CT) scan of his orbits showed a soft tissue swelling in the supero-temporal orbit with some possible lacrimal gland involvement (Figure 1B). Apart from a slightly raised absolute eosinophil count of 0.49×109/L (normal range,0.04-0.40) and mild lymphopenia of 0.75×109/L (normal range,1.50-4.00) the full blood count was normal. The C-reactive protein (CRP) was 7 mg/L (normal range, 0.30-5.00). The erythrocyte sedimentation rate (ESR), thyroid function tests,thyroid autoantibodies, antinuclear antibodies (ANA), antineutrophil cytoplasmic antibodies (ANCA), immunoglobulin G (IgG), immunoglobulin A (IgA), immunoglobulin M (IgM),serum electrophoresis and liver pro file were all normal.
A magnetic resonance imaging (MRI) scan showed abnormal soft tissue in the superior aspect of the left orbit intimately related to the superior orbital margin (Figure 1C). This abnormal tissue was seen above the levator palpebrae superioris.There was also a small focal soft tissue lesion measuring approximately 8 mm in diameter which abutted the bone.There was no bony erosion. There was involvement of the adjacent fat extending to the lacrimal gland with enhancement of soft tissue adjacent to the tensor inter-muscularis muscle.
He underwent an exploration and biopsy of his left superior orbital abnormal tissue. During this procedure a white hairlike structure, possibly a part of a parasitic worm, was also revealed and it was sent for histology with the other biopsy samples taken. The histological analysis showed no evidence of neoplasia but there was marked eosinophilia and granulomatous inflammation. Filarial serology test was positive(level 3) and filarial blood films (with haemo-concentration)were positive for Mansonella ozzaardi micro filariae. Treatment with two doses of ivermectin 200 μg/kg was administered.A repeat filarial blood film test confirmed clearance of microfilariae parasites. There was no recurrence of the left orbital infection after the anti-parasitic treatment during the subsequent 2y follow up. A repeat MRI scan was performed four months after ivermectin treatment (5mo after surgical exploration) and this showed resolution of the left superotemporal mass (Figure 1D, 1E).
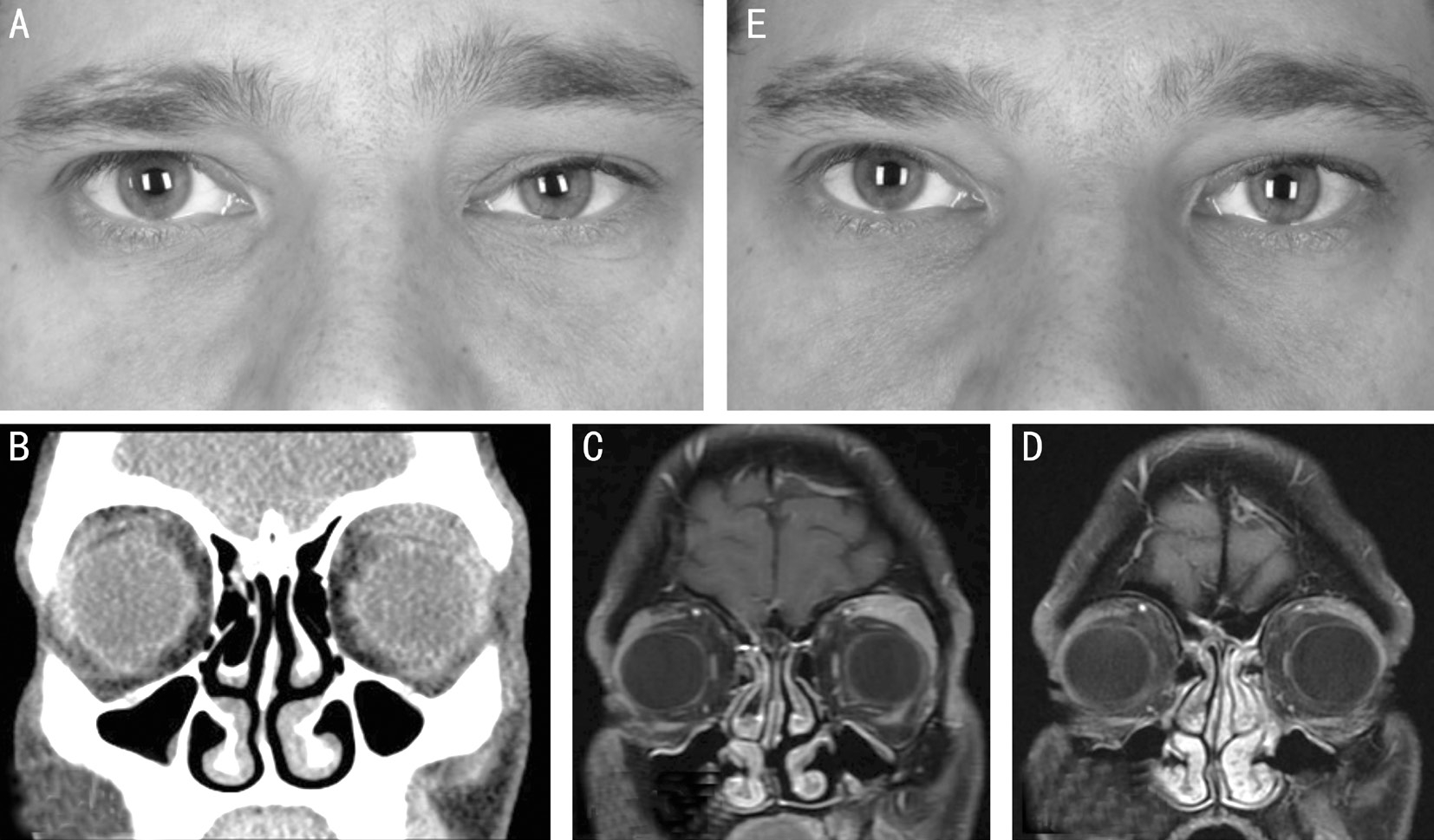
Figure 1 Pre and post-operative clinical photographs, CT and MRI scans A: Clinical photograph at presentation showing left upper eyelid swelling; B: Pre-treatment CT scan showing abnormal soft tissue material in the left supero-temporal orbit; C: MRI (T1 with fat suppression)scan showing the same abnormal soft tissue material in the superior aspect of the left orbit intimately related to the superior orbital margin, this lies above the levator muscle which appears normal, there is also a small focal soft tissue lesion measuring approximately 8 mm in diameter which abuts the bone and the bone is normal. There is involvement of the adjacent fat extending to the lacrimal gland with enhancement of soft tissue adjacent to the tensor inter muscularis; D: Post-treatment MRI (T1 with fat suppression) scan showing improved soft tissue abnormality; E:Post-treatment clinical photograph.
DISCUSSION
Humans are the only known vertebrate host for Mansonella ozzaardi[5]. Females of both vectors of Mansonella ozzaardi require a blood meal for the maturation of their eggs. During a blood meal, an infected female midge or black fl y introduce third-stage filarial larvae onto a human via the bite wound on the skin[5-7]. These larvae develop into adult male and female nematodes in humans and may grow up to several centimetres in length[7]. These adult female worms produce non-periodic unsheathed microfilariae that circulate in peripheral blood throughout the day and night[5-7]. During a blood meal from an infected host these microfilariae enter the gastrointestinal system of the arthropod[5-7]. After ingestion, microfilariae penetrate the insect's gut and go through several maturation stages in the thoracic muscles over 6 to 12d to become a thirdstage larvae before migrating to the head and proboscis, where they can be transferred to another human through an insect bite[5-7].
Presentation The clinical features of mansonelliasis are nonspecific and the infected individuals are often asymptomatic.Some individuals may develop headache, fever, arthralgia,pulmonary symptoms, lymphadenopathy and hepatomegaly[8].Micro filariae of Mansonella ozzardi can also invade the skin and cause pruritus[8]. A significant proportion of the affected individuals may suffer from microfilarial invasion of the corneal tissues resulting in parasitic keratitis[8-10]. The history of the skin rash in our patient and his partner may be related to skin involvement by Mansonella ozzardi during the early stage of the disease.
Orbital Involvement The orbital invasion by Mansonella sp has not been reported previously in the medical literature to our knowledge and this is the first reported case of orbital manifestations of Mansonella ozzardi infestation.Many filarial nematodes and their products have found to trigger an inflammatory response[8]. This may explain the redness, swelling and the eosinophilia in his blood film. Both macroscopically and microscopically the abnormal tissue removed during orbital biopsy was thought to be parasitic and strongly suggestive of the presence of adult Mansonella ozzardi in the orbit.
Investigations In the infected individuals the microfilariae of Mansonella ozzardi can be identified by simple light microscopy examination of Giemsa-stained thin or thick smears of peripheral blood[11]. Although they require a minimal amount of reagents and equipment, the sensitivity of this method may be hampered by the sparseness of organisms on the slide. Therefore, concentration techniques such as density gradient centrifugation, haemolysis and filtration of the blood through a polycarbonate membrane, which retains the parasite,are preferred[12-14]. Knott’s technique, one of the simplest known, uses 2% formalin in distilled water to concentrate the parasite[11]. In addition antigen detection assays and polymerace chain reaction (PCR) can also be useful in the identification of the disease[15-19]. The newer techniques such as DNA sequence comparisons can be used for characterizing proposed new strains.
In addition, in several epidemiological studies, high grade eosinophilia has been observed to be associated with Mansonella ozzardi infestation[20].
Treatment Therapy for mansonelliasis is challenging because there is no standard drug recommended for its treatment[21]. The introduction of ivermectin (Mectizan®) in 1987 has changed the face of tropical medicine perhaps more than any other drug in the past century[22]. Ivermectin possesses an unusually broad spectrum of potent activity against Mansonella ozzardi and several investigators have shown the safety and efficacy of this drug in patients with mansonelliasis[21,23-24].
Adverse Effects of Ivermectin Krolewiecki et al[25] reported two cases of serious anaphylactic reactions after treatment with oral ivermectin in two patients with Mansonella ozzardi infestations[25]. Both these patients had suffered systemic and respiratory symptoms and recovered without sequelae. In spite of the anaphylactic reaction in both has shown clearance of micro filaremia in both cases.
Due to its scarcity except in Latin America and in the absence of specific signs/symptoms Mansonella ozzardi infestation may pose a diagnostic dilemma when patients present to the eye units elsewhere. It is vital to take a detailed travel history and to exclude possible endemic infections/infestations to the geographical areas visited when an unusual pathophysiology is suspected in an individual concerned.
ACKNOWLEDGEMENTS
Conflicts of Interest: Lee P, None; Dharmasena A, None;Ajdukiewicz KMB, None; Ataullah S, None.
REFERENCES
1 Martins M, Pessoa FA, de Medeiros MB, de Andrade EV, Medeiros JF. Mansonellaozzardi in Amazonas, Brazil: prevalence and distribution in the municipality of Coari, in the middle Solimões River. Mem Inst Oswaldo Cruz 2010;105(3):246-253.
2 Jay V. Sir Patrick Manson. Father of tropical medicine. Arch Pathol Lab Med 2000;124(11):1594-1595.
3 Shelley AJ, Coscarón S. Simuliid Blackflies (Diptera: Simuliidae)and Ceratopogonid Midges (Diptera: Ceratopogonidae) as vectors of Mansonellaozzardi (Nematode: Onchocercidae) in Northern Argentina.Mem Inst Oswaldo 2001;96:451-458.
4 Shelley AJ, Luna Dias AP, Moraes MA. Simulium species of the amazonicum group as vectors of Mansonella ozzardi in the Brazilian Amazon. Trans R Soc Trop Med Hyg 1980;74(6):784-788.
5 Garcia L. Diagnostic Medical Parasitology. 5th ed. Washington, DC:American Society for Microbiology; 2007.
6 Marquardt W. Biology of Disease Vectors. 2nd ed. London, UK:Elsevier Academic Press; 2004. Afr J Infect Dis 2010;4(1):7-14.
7 Downes BL, Jacobsen KH. A Systematic review of the epidemiology of mansonelliasis. Afr J Infect Dis 2010;4(1):7-14.
8 Vianna LM, Martins M, Cohen MJ, Cohen JM, Belfort R Jr.Mansonellaozzardi corneal lesions in the Amazon: a cross-sectional study.BMJ Open 2012;2(6):e001266.
9 Ewert A, Smith JH, Corredor A. Micro filariae of Mansonella ozzardi in human skin biopsies. Am J Trop Med Hyg 1981;30(5):988-991.
10 Garrido C, Campos M. First report of presumed parasitic keratitis in Indians from the Brazilian Amazon. Cornea 2000;19(6):817-819.
11 Kerketta LS, Rao VB, Ghosh K. Standard karyotyping concentrates micro filaria and can be a valid concentrating technique for their detection.Trop Med Int Health 2012;17(10):1222-1226.
12 Denham DA. The diagnosis of filariasis. Ann Soc Belg Med Trop 1975;55(5):517-524.
13 Jones TC, Mott K, Pedrosa LC. A technique for isolating and concentrating micro filariae from peripheral blood by gradient centrifugation.Trans R Soc Trop Med Hyg 1975;69(2):243-246.
14 Feldmeier H, Bienzle U, Schuh D. Combination of techniques for concentration and identification of microfilariae from peripheral blood.Trans R Soc Trop Med Hyg 1981;75(2):251-253.
15 Raccurt CP, Brasseur P, Cicéron M, Boncy J. Epidemiologic survey of Mansonella ozzardi in Corail, Haiti. Am J Trop Med Hyg 2014;90(6):1167-1169.
16 Morales-Hojas R, Post RJ, Shelley AJ, Maia-Herzog M, Coscarón S,Cheke RA. Characterisation of nuclear ribosomal DNA sequences from Onchocerca volvulus and Mansonella ozzardi (Nematoda: Filarioidea)and development of a PCR-based method for their detection in skin biopsies. Int J Parasitol 2001;31(2):169-177.
17 Vera LJ, Basano Sde A, Camargo Jde S, França AK, Ferreira Rde G,Casseb AA, Medeiros JF, Fontes G, Camargo LM. Improvement of a PCR test to diagnose infection by Mansonella ozzardi. Rev Soc Bras Med Trop 2011;44(3):380-382.
18 Tang TH, López-Vélez R, Lanza M, Shelley AJ, Rubio JM, Luz SL. Nested PCR to detect and distinguish the sympatric filarial species Onchocerca volvulus, Mansonella ozzardi and Mansonella perstans in the Amazon Region. Mem Inst Oswaldo Cruz 2010;105(6):823-828.
19 Marcos LA, Arrospide N, Recuenco S, Cabezas C, Weil GJ, Fischer PU. Genetic characterization of atypical Mansonella (Mansonella) ozzardi micro filariae in human blood samples from northeastern Peru. Am J Trop Med Hyg 2012;87(3):491-494.
20 Nutman TB, Nash TE, Ottesen EA. Ivermectin in the successful treatment of a patient with mansonella ozzardi infection. J Infect Dis 1987;156(4):662-665.
21 Basano S de A, Fontes G, Medeiros JF, Aranha Camargo JS, Souza Vera LJ, Parente Araújo MP, Pires Parente MS, Mattos Ferreira Rde G, Barreto Crispim Pd, Aranha Camargo LM. Sustained clearance of Mansonellaozzardi infection after treatment with ivermectin in the Brazilian Amazon. Am J Trop Med Hyg 2014;90(6):1170-1175.
22 Cupp EW, Mackenzie CD, Unnasch TR. Importance of ivermectin to human onchocerciasis: past, present, and the future. Research and Reports in Tropical Medicine 2011;2:81-92.
23 Gonzalez AA, Chadee DD, Rawlins SC. Single dose of ivermectin to control mansonellosis in Trinidad: a four-year follow-up study. Trans R Soc Trop Med Hyg 1998:92(5):570-571.
24 Ette EI, Thomas WO, Achumba JI. Ivermectin: a long-acting micro filaricidal agent. Ann Pharmacother 1990;24(4):426-433.
25 Krolewiecki AJ, Cajal SP, Villalpando C, Gil JF. Ivermectin-related adverse clinical events in patients treated for Mansonella ozzardi infections. Rev Argent Microbiol 2011;43(1):48-50.