INTRODUCTION
As age-related cataract is one of the major causes of blindness and visual impairment worldwide, and the contribution of cataracts to blindness worldwide is likely to increase due to an ageing population, it has become important to establish the most effective and safe surgical techniques for cataract surgery. Cataract blindness has significant impact on individuals, as well as on the socioeconomic development of individuals and societies[1-3].
Phacoemulsification was initiated in 1967 by Charles Kelman,and is the most commonly performed method of cataract surgery in the developed world[4]. Phacoemulsification remains the gold standard for cataract surgery in developed countries.A new phacoemulsification system, the Centurion®, was first reported in 2014[5].
The Infiniti® phacoemulsification system (IPS), introduced in 2003, has remained the mainstay for many surgeons carrying out cataract surgery for both low-density and high-density nuclear cataracts for many years. While scepticism is not uncommon in the utilisation of new technology, as this can be based on surgical “hype”, our group has not found this to be the case with the Centurion® phacoemulsification system(CPS). CPS has recently been shown to carry out satisfactory phacoemulsification surgery with less cumulated dissipated energy (CDE)[6-8].
This current study evaluated the surgical outcomes (SOs)and visual outcomes (VOs) for cataract surgery using the CPS compared with the IPS in real-world clinical practice.Prospective data collection included CDE, operative and postoperative complications, and corrected distance visual acuity (CDVA) at one month. Ultimately, VOs may be the most important arbiter of surgical and visual success in cataract surgery. Therefore, this study, which compares CDEs in CPS and IPS, is the first to document both VOs as well as SOs.
SUBJECTS AND METHODS
This was a prospective, consecutive, comparative study that investigated the SOs including CDE and complications, as well as VOs, in two cohorts of cataract procedures comparing CPS and IPS. All patients gave informed written consent prior to surgery. The University of New South Wales, Australia granted ethics approval (Approval HC13220), and the study was performed according to the tenets of the Declaration of Helsinki.
Patient clinical characteristics included age, gender, ocular comorbidity (e.g. glaucoma, macular degeneration, and amblyopia), and preoperative conditions potentially adversely affecting SOs and VOs (e.g. previous vitrectomy, corneal opacities, and pseudoexfoliation), preoperative CDVA,previous cataract surgery, and nuclear sclerosis (NS) grade. SOs included CDE, and complications of surgery. Complications were defined as intraoperative complications and postoperative complications, and were documented up to one month postoperatively. Similarly, VOs were assessed by means of CDVA at one month postoperatively.
CDE is the total energy dissipated at the wound site, which includes a combination of both torsional and longitudinal ultrasound energies. The calculation of CDE is based on the average ultrasound power multiplied by the total ultrasound time. The total ultrasound time is denoted by the duration of the foot pedal being kept in the third position. When using torsional phacoemulsification, the CDE is multiplied by a coefficient of 0.4 as there is an 80% reduction in frequency of the phacoemulsification tip and the stroke length is also reduced by half[6].
All procedures were performed by one surgeon (Francis IC)under either assisted topical anaesthesia or assisted local anaesthesia[9]. Prior to surgery, each cataract was graded in accordance with the Lens Opacities Classification System III(LOCS III)[10-11]. Regardless of equipment, all cases underwent the “Stop and Chop Phacoemulsification” technique by the single surgeon. There were no exclusion criteria. For the IPS cases, a 30-degree Kelman®, 0.9 mm, Turbosonics®, Mini-Flared ABS® Tip was used. For the CPS cases, a 30-degree Balanced® Tip, 0.9 mm, Intrepid® was used (Figure 1).
A standardised proforma was used to collect all data prospectively and consecutively. Upon completion of the IPS procedures, the CPS study was commenced. Data were documented by the Operating Room nursing staff during the procedure, and the surgeon at the conclusion of the procedure.Patients were reviewed at one day, one week, and one month postoperatively in 100% of cases.
CDVA was reported in Snellen and logarithm of theminimum angle of resolution (logMAR) format for means. Mean CDVA was determined by calculating the geometric mean with standard deviation stated in logMAR format[12].
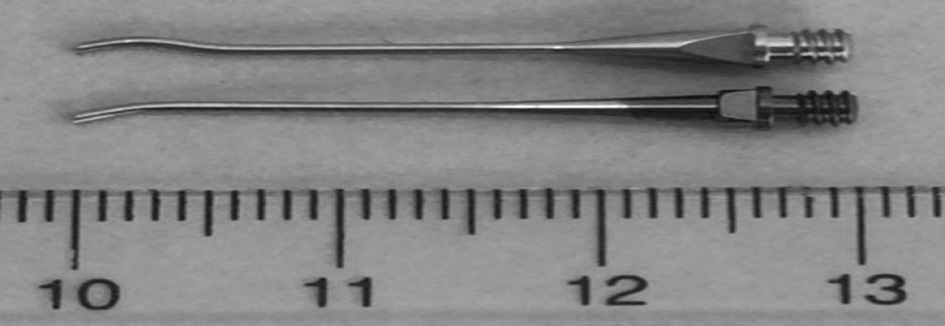
Figure 1 Intrepid® 30-degree Balanced® Tip (above), and Kelman®, Turbosonics®, Mini-Flared 30-degree ABS® Tip (below).
Statistical Analysis All statistical analyses were conducted with SPSS® software (version 22.0, SPSS, Inc., Chicago, IL,USA). Statistical analysis was performed using descriptive statistics, Chi-squared test, and t test. The decision was made to use simple t test for statistical analysis because the data showed a normal distribution pattern. Snellen visual acuity was analyzed using logMAR. The groups were calculated for a 0.05 level of significance, with P value less than 0.05 considered statistically significant. All P values reported were two-sided.The Chi-squared test was used for all categorical variables, and two sample t test used for all continuous variables.
RESULTS
The study comprised 207 eyes that underwent cataract surgery using the CPS, and 205 eyes that underwent cataract surgery using the IPS. Patient characteristics are shown in Table 1.There was, coincidentally, a statistically significant difference between CPS and IPS cases in terms of NS grading (P=0.002).The CPS subcohort had a higher proportion of patients with dense nuclear cataracts. Patient age, gender, ocular comorbidity, whether the patient’s cataract surgery was their first cataract procedure, and preoperative CDVA demonstrated no statistically significant difference[13].
Surgical Outcomes In terms of SOs, there was a statistically significant difference in the mean CDE between the whole CPS (15.70%) and IPS (18.15%) subcohorts, the IPS subcohort requiring a higher mean CDE (P=0.017). Pertinently, while the CPS cases required less CDE, the cataracts in this subcohort were significantly more dense (P=0.002) (Table 2).
In the NS grade III and greater cataracts, even less CDE was required by the CPS (18.45%) when compared with the IPS(25.94%) cases (P=0.010) (Table 3).
In terms of intraoperative complications, there was one case of a potentially sight-threatening complication, represented by a single vitreous loss in the CPS subcohort. This occurred due to a posterior capsular tear at the sub-incisional cortex site during automated irrigation/aspiration. Fortunately, this patient achieved CDVA of 6/4 at one month. Moreover, when the medical record of this case was reviewed, at 12mo the retina was flat and the CDVA had maintained at 6/4. In terms of nonsight-threatening complications, there was no statistically significant difference between CPS and IPS subcohorts up to one month following surgery (P=0.083). There were two intraoperative cases of iris prolapse in the CPS, but no reduction of mean CDVA at one month. There were no postoperative complications in either subcohort at up to one month post-surgery.
Table 1 Patient characteristics of the whole cohort, and Centurion® and Infiniti® subcohorts
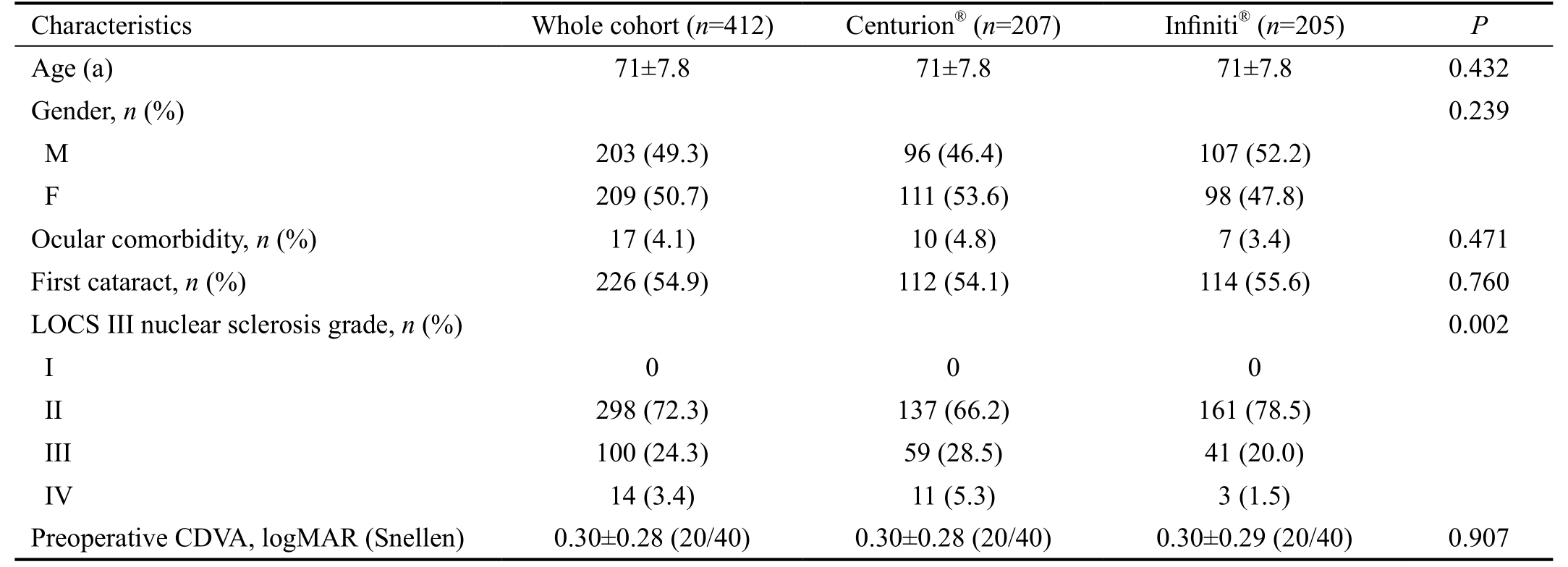
CDVA: Corrected distance visual acuity.
Table 2 Surgical outcomes and visual outcomes of the whole cohort, and Centurion® and Infiniti®subcohorts
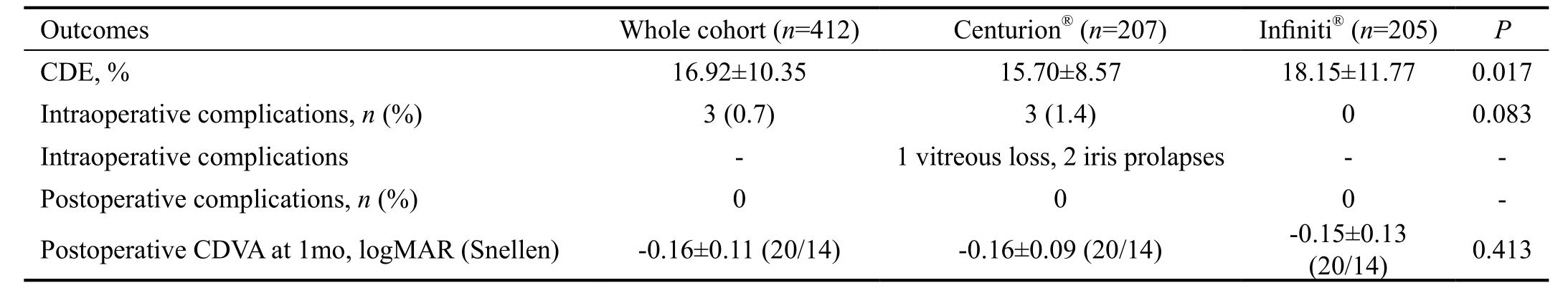
CDE: Cumulative dissipated energy; CDVA: Corrected distance visual acuity.
Table 3 Outcomes for nuclear sclerosis grade III and greater of whole cohort, and Centurion® and Infiniti®subcohorts
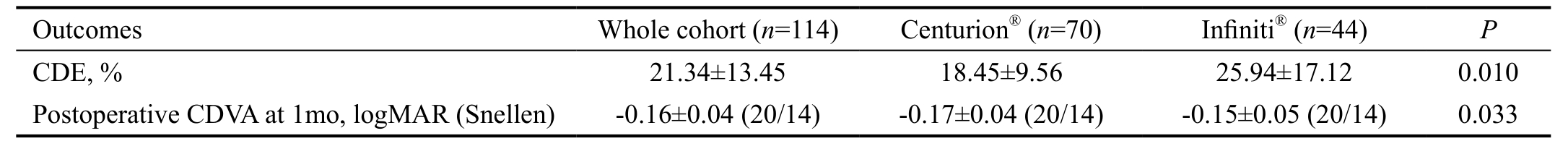
CDE: Cumulative dissipated energy; CDVA: Corrected distance visual acuity.
Visual Outcomes In terms of VOs, there was no statistically significant difference in postoperative mean CDVA at one month between the whole CPS and IPS subcohorts, with both achieving mean CDVAs of -0.16 logMAR (6/4.5) and-0.15 logMAR (6/4.5) respectively (P=0.413). When cases with ocular comorbidities that potentially adversely affected outcomes were excluded, again there was no significant difference in postoperative mean CDVA at one month between the whole CPS and IPS subcohorts.
However, as demonstrated in Table 3, for those patients with NS grades III and greater, postoperative mean CDVA was significantly better in the CPS subcohort. Specifically,the postoperative mean CDVA for the CPS cases was -0.17 logMAR (6/4.5) and IPS was -0.15 logMAR (6/4.5) (P=0.033).In other words, while the whole CPS subcohort and IPS subcohort had equal CDVA at one month, for NS grade III and greater cataracts, CPS VOs were significantly better than those of the IPS.
DISCUSSION
Cataract surgeons worldwide continue to pursue excellent VOs and SOs with minimisation of operative trauma, and maximisation of surgical safety. There are numerous phacoemulsification technologies available, using different phacoemulsification machine systems, which can render comparisons between machine modalities difficult[14].
To date, evaluations of the CPS and of Balanced® versus Kelman® tips have been documented in seven reports[5-8,15-17].Chen et al[6] demonstrated that CDE was less in CPS than IPS.This study was a retrospective chart review from five surgeons in Hawaii, commencing in 2014. The cohort of 2077 was impressive, but there may have been a lack of standardization of surgical technique, and there was no documentation of nucleus density, CDVA, or surgical complications[6]. Nicoli et al[16] in an experimental model also demonstrated the benefit of Active Fluidics® in an acrylic test chamber that modelled the anterior chamber of the eye.
Davison[17] and Demircan et al[8] emphasized the value of the Balanced® tip, employed in CPS. Our group entirely concurs with the benefit of the Balanced® tip. The IPS employs torsional ultrasound to establish a side-to-side oscillation of the partial Kelman tip, which has been found to be approximately half of the ultrasonic efficiency generated by the CPS’s Balanced® tip[17]. This efficiency was considered to translate to a substantially reduced CDE at the tip aperture. Sharif-Kashani et al[5] demonstrated the benefit of an improved occlusion break surge with the CPS relative to the IPS. This improved occlusion break surge may be attributed to the Active Fluidics® irrigation system, which reduced the anterior chamber collapse as well as facilitating the rapid evacuation of the nucleus. This feature of the CPS has been found by our group to be beneficial, and may potentially be so for the novice trainee surgeon. Indeed, surgical facility and comfort were subjectively better for the surgeon using CPS over the course of our study. Although it may have been beneficial from a research perspective to compare the CPS and IPS machines using the same Balanced® tip, this was not available during the period in which the surgeon performed his earlier cataract cases with the IPS.
Jensen et al[15], in a porcine study, showed that ‘chatter’was minimal at up to 60% of phacoemulsification power,and recommended that no greater power settings should be required. By contrast, our study (n=412) was prospective,consecutive, comparative, and in humans, demonstrating an improved CDE in CPS compared with IPS.
A recent prospective, randomized (to CPS or IPS) clinical case series by Solomon et al[7], compared CDE between 100 patients from three centres, two in the United States and one in Spain. The surgeries were done two weeks apart. Initially, 98 patients were operated. However, three further patients were then excluded from this study, presumably following their first surgery, because of death, corneal decompensation, and withdrawal of consent. Importantly, Solomon et al[7] found that CDE was significantly lower in their CPS cohort (P<0.001).This was similar to that in our cohort, where there was a 13.5%-28.87% CDE reduction (P=0.010) in our CPS cohort.Solomon et al[7] attributed this significant reduction to the Active Fluidics® technology of the CPS system. However,while the CPS definitely provided increased surgical facility and comfort, because of improved anterior chamber maintenance,our group considered that the more efficient Balanced® tip was the likely contributor to this finding[8,17]. Solomon et al[7] stated that there were no serious ocular adverse events. However, one patient had to be withdrawn from the study due to postoperative corneal decompensation. It was not clear from the Solomon et al[7] study how many patients actually contributed to the final outcomes. By contrast, our study comprised a larger cohort,being 210% greater than that of the Solomon et al[7] cohorts.Furthermore, in our studythere were no exclusion criteria, and follow-up was achieved in 100% of patients to one month.
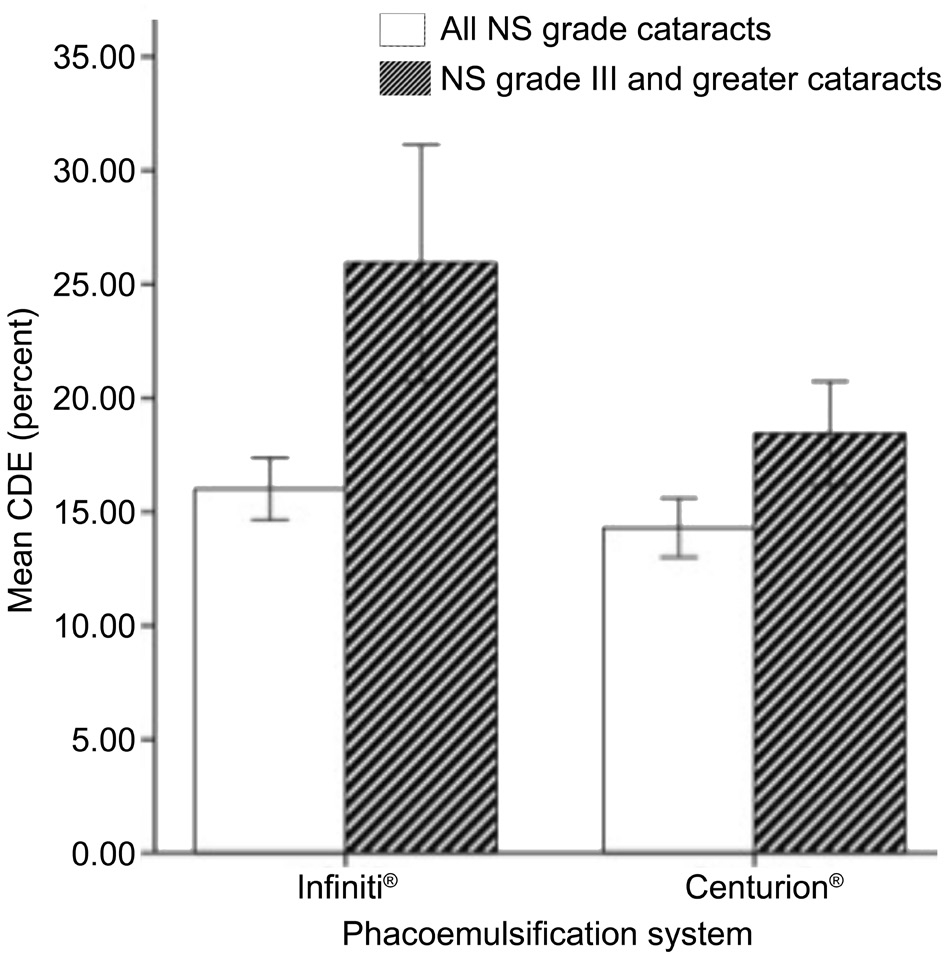
Figure 2 Cumulative dissipated energy for nuclear sclerosis grade III and greater, and all nuclear sclerosis grade cataracts in the Centurion® and Infiniti® subcohorts.
The improved CDE in CPS compared with IPS is already evident in the literature[6-8], with only two other studies reporting surgical complications and NS density[7-8]. Our study reviewed all of the aforementioned factors, but also compared VOs in terms of CDVA between the CPS and IPS for different NS grades.Interestingly, VOs within our study in the whole cohort,the CPS was comparable with the IPS. Indeed, there was no significant difference in the postoperative mean CDVA at one month between the CPS and IPS subcohorts, both achieving mean CDVAs of 6/4.5 (P=0.413). Even when cases with ocular comorbidities that potentially adversely affected outcomes were excluded, analysis of the outcomes did not yield any significant differences. However, the mean CDVA at one month for the NS grade III and above cataracts in the CPS subcohort (-0.17 logMAR) was significantly higher compared to the IPS subcohort (-0.15 logMAR) (P=0.033).
It has been shown that lower CDE is associated with less corneal endothelial cell damage, which may lead to improved SOs and VOs. While CDE is dependent on multiple factors,such as surgical setting, surgeon and phacoemulsification technique, the current study clearly showed that CDE was less in the CPS cohort[7-8]. In the multi-surgeon retrospective chart review study by Chen et al[6], the reduction in CDE in the CPS subcohort compared with the IPS subcohort was 38%.
In the current prospective, consecutive, no-exclusions, singlesurgeon study set in real-world clinical practice, the reduction in CDE for the CPS compared with the IPS for each whole subcohort was 13.50%. The numbers of cataracts NS grade III and above were 70 and 44 for the CPS and IPS respectively.The difference in CDE favoured the CPS in NS grade III or greater, demonstrating significantly (P=0.010) less CDE being required for CPS (18.45%) and IPS (25.94%) (Figure 2). This reduction of CDE, as well as the Active Fluidics®[7,17-18], may protect the corneal endothelium in cases with denser nuclei,and should therefore result in improved SOs and VOs.
There was one major complication in the CPS subcohort and no complications in the IPS. The CPS case was represented by a single vitreous loss. However, this case was dealt with appropriately and the VO at both one month and one year was 6/4.
The current study could arguably have been improved by randomizing the patients to CPS or IPS. However, this study involved a substantially new technique: Centurion. The facility of the technique, while not easily evaluated in an objective manner compared with traditional phacoemulsification, was felt to be substantially better in the surgeon’s hands. For our group therefore, to have gone back to the more traditional phaco with the Infiniti, randomising future cases, case by case,was simply not appropriate. This was because it would have been subjecting the group’s patients to what was considered to be an inferior technique and technology. Given the surgical facility and reduced CDE of CPS, it was felt by the authors to be difficult to justify ethically, because of the reduced energy expenditure in the anterior segment. Further, because of the different distribution of NS density, it may have been helpful to conduct a much larger study on CPS comparing IPS. However, having initially experienced both the surgeon facility of CPS, and the initial reduction of CDE, it was felt inappropriate to revert to IPS to do a randomized control study. The advantage of data from observational studies is that they provide an indication of what is occurring in routine clinical practice. Although clinical trials have the advantage of determining treatment efficacy in ideal and standardised conditions, observational studies such as this can assess treatment efficacy in an unaltered general population. The authors recommend that a randomized control trial assessing the comparative outcomes between the CPS and IPS using the same Balanced® tip be performed to confirm or disprove the results of this study.
In conclusion, there was a statistically significant difference between the CPS and the IPS subcohorts in terms of SOs and VOs. However, while VOs were comparable in the whole subcohorts, the VOs in NS grade III or greater were statistically superior. While CDEs were significantly reduced in the CPS subcohortin comparison with the IPS subcohort,this difference was even more significant in patients with denser NS cataracts. It is possible this related to the Balanced®tip in comparison with the Kelman, Mini-Flared ABS® tip.Surgical facility, while subjective for an individual surgeon,was reported to be improved in this study, possibly based on the Active Fluidics® of the CPS. The authors consider that the CPS represents an advance in surgical technique and SOs and VOs, and recommend the CPS for cases with denser nuclei.
ACKNOWLEDGEMENTS
Conflicts of Interest: Oh LJ, None; Nguyen CL, None;Wong E, None; Wang SY, None; Francis IC, None.
REFERENCES
1 de Silva SR, Riaz Y, Evans JR. Phacoemulsification with posterior chamber intraocular lens versus extracapsular cataract extraction (ECCE)with posterior chamber intraocular lens for age-related cataract. Cochrane Database Syst Rev 2014;(1):CD008812.
2 WHO. Global data on visual impairments 2010. World Health Organisation http://www.whoint/blindness/GLOBALDATAFINAL forwebpdf. 2012.
3 Riaz Y, Mehta JS, Wormald R, Evans JR, Foster A, Ravilla T, Snellingen T. Surgical interventions for age-related cataract. Cochrane Database Syst Rev 2006;(4):CD001323.
4 Kelman CD. Phaco-emulsification and aspiration. A new technique of cataract removal. A preliminary report. Am J Ophthalmol 1967;64(1):23-35.
5 Sharif-Kashani P, Fanney D, Injev V. Comparison of occlusion break responses and vacuum rise times of phacoemulsification systems. BMC Ophthalmol 2014;14:96.
6 Chen M, Anderson E, Hill G, Chen JJ, Patrianakos T. Comparison of cumulative dissipated energy between the Infiniti and Centurion phacoemulsification systems. Clin Ophthalmol 2015;9:1367-1372.
7 Solomon KD, Lorente R, Fanney D, Cionni RJ. Clinical study using a new phacoemulsification system with surgical intraocular pressure control. J Cataract Refract Surg 2016;42(4):542-549.
8 Demircan S, AtasM, Goktas E, Baskan B. Comparison of 45-degree Kelman and 45-degree balanced phaco tip designs in torsional microcoaxial phacoemulsification. Int J Ophthalmol 2015;8(6):1168-1172.
9 Figueira EC, Sharma NS, Ooi JL, Masselos K, Lee KJ, Rosenberg ML,Francis IC, Alexander SL, Ferch NI, Stapleton F. The Lanindar test: a method of evaluating patient suitability for cataract surgery using assisted topical anaesthesia. Eye (Lond) 2009;23(2):284-289.
10 Chylack LT Jr, Wolfe JK, Singer DM, Leske MC, Bullimore MA, Bailey IL, Friend J, McCarthy D, Wu SY. The Lens Opacities Classification System III. The Longitudinal Study of Cataract Study Group. Arch Ophthalmol 1993;111(6):831-836.
11 Davison JA, Chylack LT. Clinical application of the lens opacities classification system III in the performance of phacoemulsification. J Cataract Refract Surg 2003;29(1):138-145.
12 Holladay JT. Proper method for calculating average visual acuity. J Refract Surg 1997;13(4):388-391.
13 Ruan CW, Win SH, Francis KE, Francis IC. Optimizing the cataract order of the list in modern surgery. J Cataract Refract Surg 2014;40(5):842-843.
14 Mamalis N. Which phacoemulsification modalities are the best?Comparing apples to apples. J Cataract Refract Surg 2015;41(2):255-256.
15 Jensen JD, Shi DS, Robinson MS, Kramer GD, Zaugg B, Stagg BC, Pettey JH, Barlow WR Jr, Olson RJ. Torsional power study using CENTURION phacoemulsification technology. Clin Exp Ophthalmol 2016;44(8):710-713.
16 Nicoli CM, Dimalanta R, Miller KM. Experimental anterior chamber maintenance in active versus passive phacoemulsification fluidics systems.J Cataract Refract Surg 2016;42(1):157-162.
17 Davison JA. Two-speed phacoemulsification for soft cataracts using optimized parameters and procedure step toolbar with the CENTURION Vision System and Balanced Tip. Clin Ophthalmol 2015;9:1563-1572.
18 Chang JS, Ng JC, Chan VK, Law AK. Cataract surgery with a new fluidics control phacoemulsification system in Nanophthalmic eyes. Case Rep Ophthalmol 2016;7(3):218-226.