INTRODUCTION
Accurate calculation of intraocular lens (IOL) can help provide a satisfactory refractive outcome in phacoemulsification and IOL implantation surgery. To calculate IOL refractive power, corneal curvature measurement plays a key role, for the cornea is one of the main refractive materials, making up approximately 70% of the refractive power of the human eye[1-3]. In addition, previous studies have shown that cataract patients who did not receive a toric lens had different degrees of astigmatism and residual astigmatism after surgery will decrease visual function[4-8]. Also, it has been shown that toric lens implantation is an effective and safe method for astigmatism correction. These studies triggered the interests of correcting astigmatism simultaneously with toric lens implantation[9-11]. Both for toric and non-toric lens implantation,the most important factor is precise corneal measurement.
Clinically, corneal parameters used for IOL power calculation are mainly acquired from IOL-Master or Lenstar based on autokeratometer that calculate countable reflected points; also,tear film stability cannot be supervised during measurement,which can lead to further errors[12].
Here Ophtha Top topography, as a new IOL calculator based on a Placido-disk topographer, may provide more accurate results. Ophtha Top includes more detection points and it can also supervise tear film stability during measurements. There have been few studies on the repeatability of the Ophtha Top topography in cataract patients. In addition, for Ophtha Top topography to be integrated as a new method for IOL power calculation[13], it is necessary to clarify whether Ophtha Top can provide interchangeable corneal measurements in cataract patients compared with IOL-Master and Lenstar before it can be used for IOL power calculation.
The purpose of this study was to determine the repeatability of Ophtha Top topography in cataract patients and to assess the agreement of corneal refractive power and astigmatism segments with two clinically used devices, i.e. IOL-Master and Lenstar.
SUBJECTS AND METHODS
Subjects Senile cataract patients who were scheduled for cataract surgery at Tianjin Eye Hospital (during November 2013 to February 2015) were enrolled in this study. The exclusion criteria were a history of ocular pathology, eye trauma and subsequent surgery, recent use of contact lens or eye drops, and eyes with poor fixation ability. Before included into this study, informed consent was collected from each patient after the nature and risk of the study was explained.In addition, the study was approved by the Research Review Board of Tianjin Eye Hospital, and all measurements were performed strictly followed the tenets of the Declaration of Helsinki for the use of human participants in biomedical research.
Methods Eyes of patients who were scheduled for cataract surgery were enrolled and all received a comprehensive examination by an ophthalmologist including uncorrected distance visual acuity, slit-lamp bio-microscopy, non-contact tonometry, and the fundus examination after pupil dilation.Corneal power, corneal astigmatism, and axis location measurements were obtained using IOL-Master, Lenstar, and Ophtha Top topography. All devices were adjusted before measurement. Subjects were kept seated and positioned in a chin rest and forehead rest. Before each measurement, subjects were told to fixate on the fixation target and blink before a measurement began. Repeated measurements were performed at least 3 times with each device by experienced examiners.The final refractive parameters determined with IOL-Master and Lenstar were the mean values of 3 measurements. As for Ophtha Top topography, each of the three measurements was recorded to assess repeatability, and then measurement outcomes were chosen for comparison with the results of IOLMaster and Lenstar.
Devices The Ophtha Top (Version 2.4, Hummal, Germany) is a new IOL calculator that integrates a Placido-disk topographer and ray-tracing software. The corneal curvature is measured automatically with computer assisted topography, and the IOL power is calculated with thin lens theory based on a real ray tracing method. In Ophtha Top topography, 30 concentric rings are projected onto the diameter of a 9 mm anterior corneal surface, with 10 800 points that can be analyzed. The index of refraction 1.3375 is used to convert the radius of the curvature into corneal power diopters. The system calculates simulated K-readings (SimK) from the topography data by averaging two meridians that are perpendicular to each other in a radial area of 1.0 to 1.5 mm from the center.
The IOL-Master (Version3.02. Carl Zeiss Meditec AG, Germany)measures the corneal curvature with automated keratometry.A hexagonal array of six points is projected onto a diameter of approximately 2.3 mm of the anterior surface of the cornea.The refractive index of 1.3375 is adopted to convert the radius of curvature (mm) into the refractive power of the cornea in diopters.
The Lenstar LS 900 (Haag-Streit AG, Koeniz, Switzerland)uses automated keratometry to measure the corneal curvature.In total, 32 points are projected onto two concentric cycles with diameters of 1.65 and 2.30 mm and the corneal curvatures are converted with a refractive index of 1.3375.
Statistical Analysis All the data were recorded in Microsoft Office Excel and then transferred to SPSS for data analysis.P values less than 0.05 were considered significant. The distribution of all data was checked by a Kolmogorov-Smirnov test and was shown to have a normal distribution.
The parameters noted during each measurement included steep K, flat K, the mean value of flat K and steep K (Km), the axis of flat K and steep K and astigmatism. Cornea astigmatism results were valued by vector analysis developed by Thibos et al[14], according to the following equation with two new astigmatic vector components J0 (cylinder at 0-degree meridian) and J45 (cylinder at 45-degree meridian): J0=-(cylinder/2) cos (2axis); J45=-(cylinder/2) sin (2axis).
Repeatability of Ophtha Top Measurements To determine the repeatability of Ophtha Top topography, four parameters were used. First, intra-class correlation coefficients (ICCs) were obtained, which was first proposed by Bartko and Carpenter[15].We used these values to determine the consistency of the repeated data sets. ICCs ranged from 0 to 1. An ICC greater than 0.90 shows high repeatability and an ICC lower than 0.75 represents poor repeatability, and an ICC between 0.75 and 0.9 show moderate repeatability. Second, the coefficient of variance (COV) was determined by the ratio of the within subject standard deviation (Sw) to total mean values. A lower COV indicated higher repeatability. The advantage of COV values is that they can be used to compare data sets of different units or different means. The disadvantage is that when the mean value is close to zero, the COV is very sensitive to small changes in the mean values that limit its usefulness. Third,the Sw, which means the SD of repeatability, was included in the analysis[16]. Fourth, test-retest repeatability (2.77Sw) was considered, because 95% of the differences between repeated measurements are expected to lie in this range[16].
Comparison of Different Devices To assess the agreement of corneal K-readings and astigmatism values acquired from Ophtha Top topography, IOL-Master and Lenstar devices, the 95% limit of agreement (95%LOA) was calculated as the mean difference ±1.96 standard deviation. A narrower 95%LOA predicted better consistency between techniques. In addition,Pearson correlation coefficients were noted to determine the correlation between measurements. Bland-Altman plots were also adopted.
RESULTS
The study enrolled 125 eyes of 125 cataract patients, with an average age of 64.74±8.65y and including 55 males and 70 females. In total, 99 eyes with three measurements over 70% percent of the cornea were included to determine the repeatability of the new topography method. In total, 80 eyes were measured using IOL-Master and Lenstar, and these results were compared.
Repeatability of Ophtha Top Topography Table 1 shows the repeatability of flat K, steep K, Km, and astigmatism vectors J0 and J45 measured by Ophtha Top topography. The ICC of parameters analyzed was all above 0.9. The Sw was lower than 0.12 D, and the 2.77Sw was lower than 0.33. The COV of K-readings was lower than 0.25. All these parameters indicated there was good repeatability with Ophtha Top topography.
Agreement of Different Devices Table 2 describes the homogeneity of Ophtha Top topography and Lenstar. The Pearson R value was above 0.9, except for J45, which was 0.898. The difference in K-readings was within 0.41 D and the differences were 0.04 and 0.01 D for J0 and J45, respectively.The 95%LOA was from -0.10 D-0.95 D for K-readings,and the differences were -0.23 to 0.29 D for J0 and J45,respectively.
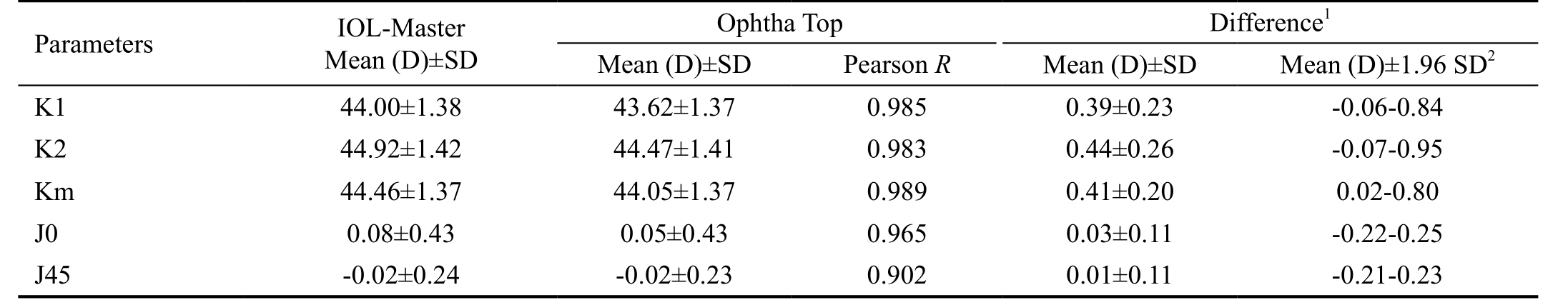
Table 3 describes the agreement between Ophtha Top topography and IOL-Master. The Pearson R value was above 0.9.The difference in K-readings was within 0.44 D, and the differences were 0.03 and 0.01 D for J0 and J45, respectively.The 95%LOA was from -0.07-0.95 D for K-readings, and the differences were -0.22 to 0.25 D for J0 and J45, respectively.Table 4 shows the differences for J0 and J45 using Ophtha Top topography, Lenstar and IOL-Master. The Pearson correlation coefficient was above 0.9. The 95%LOA for J0 and J45 comparisons among different devices was narrow.The correlation of the Ophtha Top topography vs Lenstar and Ophtha Top topography vs IOL-Master was described in the Figures. Figures 1, 2 (A1-C1) show the correlations for Ks,Kf, and Km were good in comparisons of autokeratometers using Lenstar, IOL-Master and Ophtha Top. For J0 and J45(Figure 3 A1-D1), the correlation was moderate. Figures 1, 2(A2-C2) shows moderate agreement for Ks, Kf, and Km, as the 95%LOA covered approximately 1.0 D. Figure 3 (A2-D2)shows the 95%LOA for J0 and J45 was within 0.5 D.
DISCUSSION
Both in clinical and research applications, it is crucial to maintain accurate and repeatable K-readings, because good repeatability can ensure high accuracy[17-20]. Our study showed excellent repeatability of corneal power and astigmatism vector measurements with Ophtha Top topography, with all ICCs above 0.93, 2.77Sw lower than 0.31, and the COV of the flattest meridian and steepest meridian lower than 0.25. The results are comparable with previous studies. For example, a study[11] of atlas corneal topography showed the ICC was above 0.96 for K-readings, and the ICCs were 0.92 and 0.90 for J0and J45, respectively. This was similar to our results. Read et al[21] analyzed Medmont E300 measurements and showed high repeatability with a repeatability coefficient (2.77Sw) of 0.12 for both J0 and J45, and the ICCs were 0.99 and 0.95,respectively. Studies analyzing EyeSys 2000 measurements showed high repeatability in tests with different curvature ranges[22-23].
Table 1 Repeatability of measurement outcomes with Ophtha Top topography n=99 (eye)
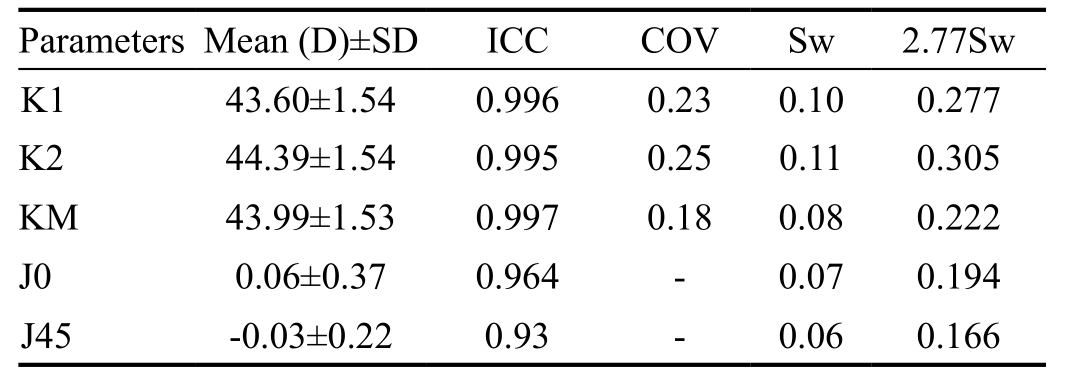
ICC: Intra-class correlation coefficient (for mean value); COV: With-in subject variation coefficient; Sw: With-in standard deviation; 2.77Sw:Coefficient of repeatability.
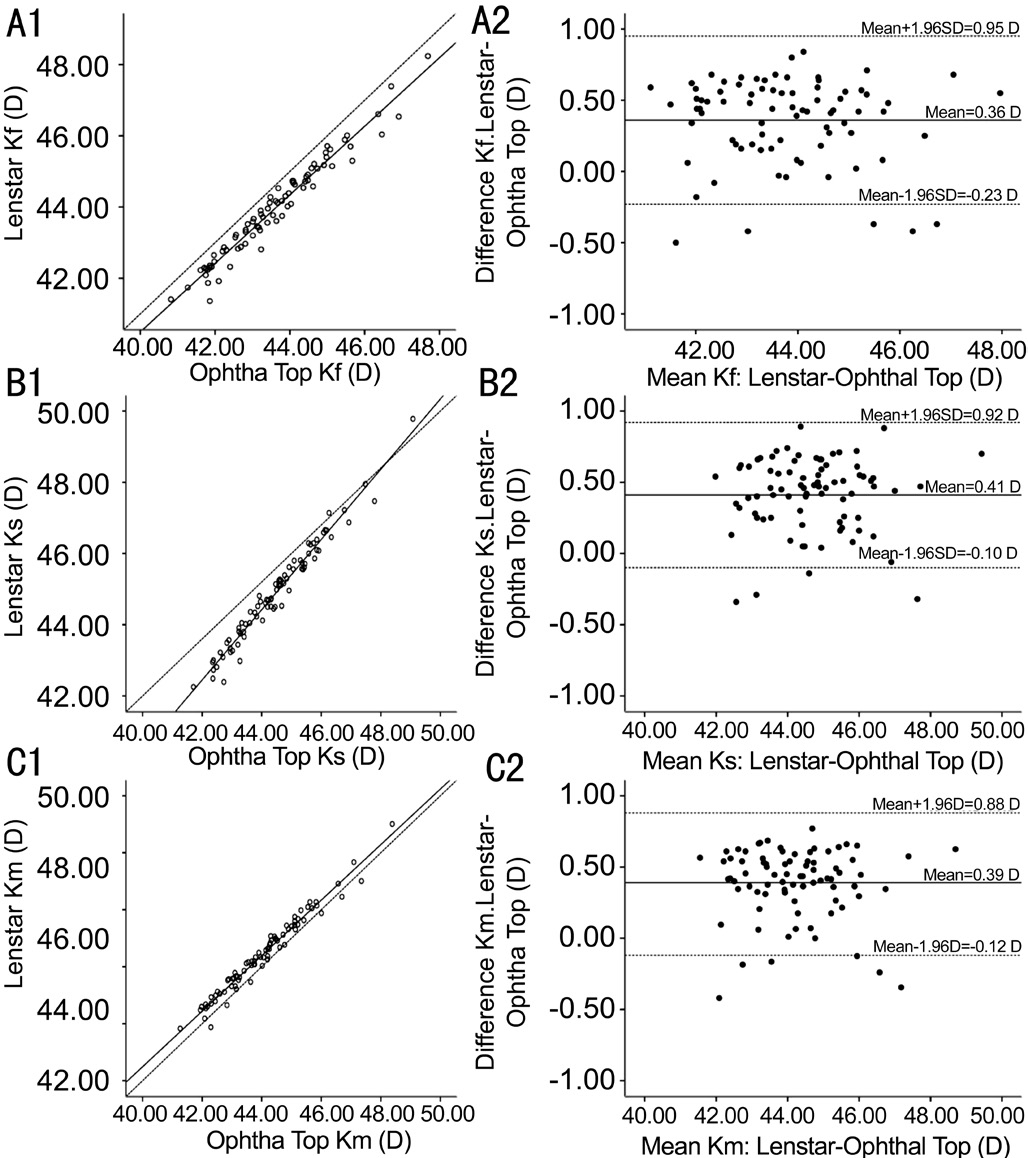
Figure 1 Linear correlation and Bland-Altman plots for Ks,Kf, Km between Lenstar and Ophthal Top A1-C1: The linear correlations between Lenstar and Ophtha Top measurements for Kf,Ks, and Km. The solid lines represent the real correlation lines for the two devices, while the dotted lines represent the quality lines; A2-C2:The Bland-Altman plots for Lenstar and Ophtha Top for Kf, Ks, and Km. The solid lines represent the mean values of differences, and the dotted lines represent the 95%LOA values.
Recently, Mao et al[24] studied a similar topographer (i.e.Keratopraph4) and reported an ICC over 0.98, 2.77Sw values from 0.26 to 0.30 for K-readings and 0.07 to 0.09 values for J0 and J45. The COV was between 0.21 and 0.27 for K-readings.Although all the above devices are based on Placido-disk,the Keratopraph4 and our new topographer showed higher repeatability. This may be because the Keratopraph4 includes 22 rings with 22 000 testing points. Our new topography method includes 30 rings with 10 800 testing points. The number of testing points was more than in other methods,
and both of these devices can supervise the tear film during measurements, which can provide more accurate results.
Table 2 Comparison between Lenstar and Ophtha Top topography mean±SD, n=80 (eye)
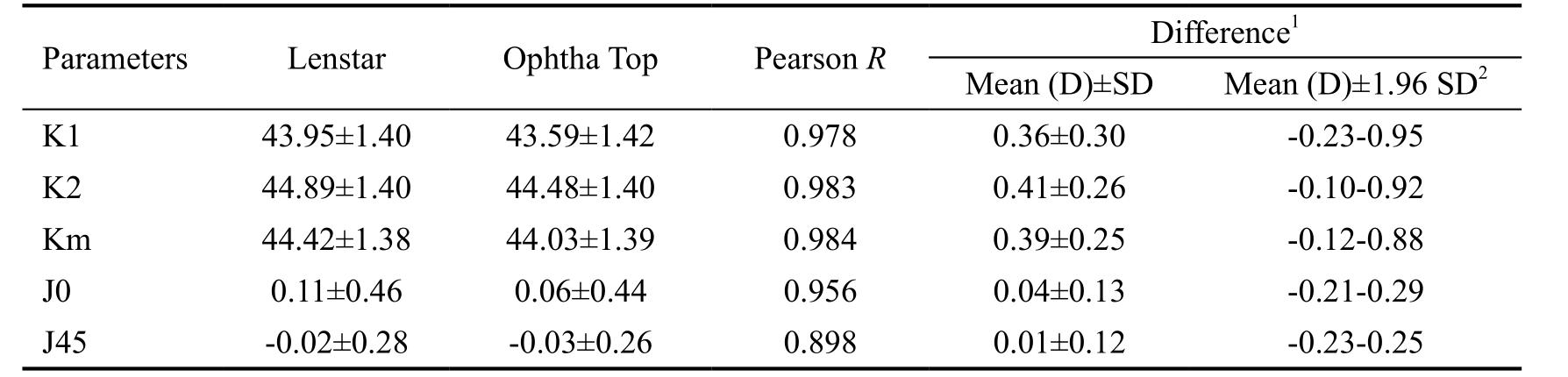
1Difference expressed as Lenstar-Ophtha Top topography; 295%LOA.
Table 3 Comparison between IOL-Master and Ophtha Top topography n=80 (eye)
1Difference expressed as IOL-Master-Ophtha Top Topography; 295%LOA.
Table 4 Comparison of J0 and J45 between devices

195%LOA.

Figure 2 Linear correlation and Bland-Altman plots for Ks, Kf, Km between IOL-Master and Ophthal Top A1-C1: The linear correlation between IOL-Master and Ophtha Top for Kf, Ks, and Km. The solid lines represent real correlation lines for the two devices, and the dotted lines represent the quality lines; A2-C2: The Bland-Altman plots for IOL-Master and Ophtha Top for Kf, Ks, and Km. The solid lines represent the mean values of differences, and the dotted lines represent the 95%LOA values.
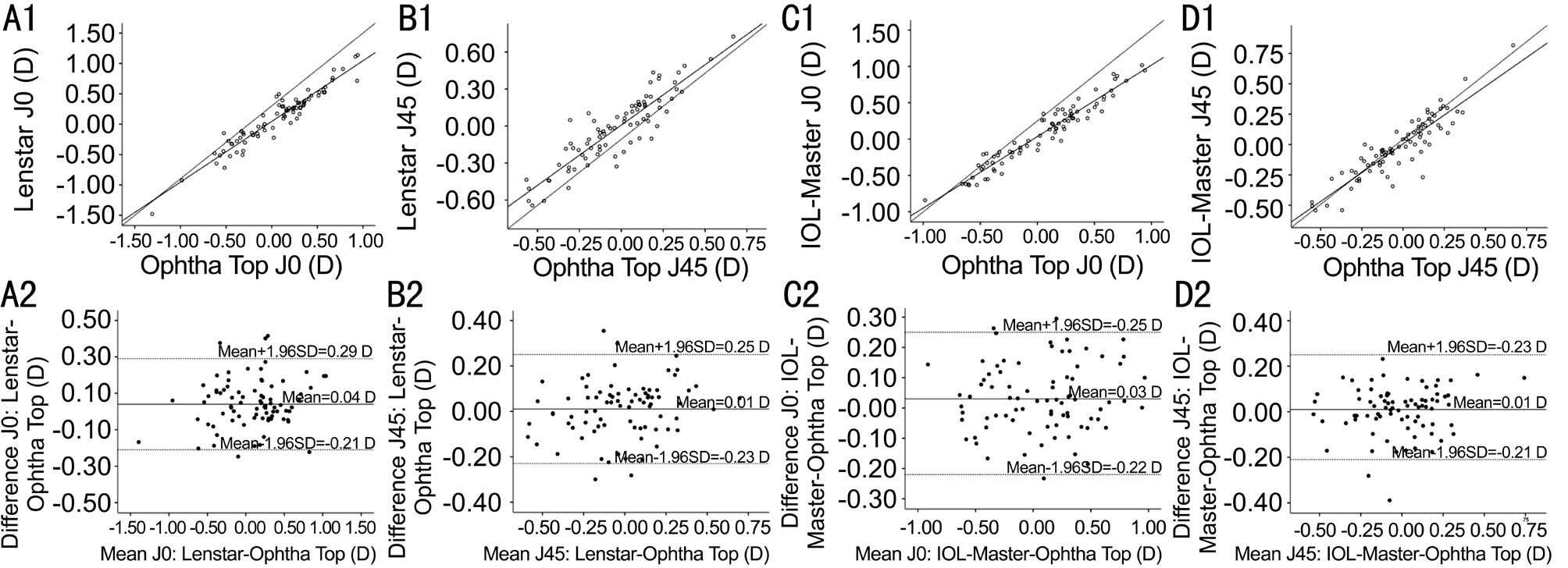
Figure 3 Linear correlation and Bland-Altman plots for J0, J45 between Lenstar and Ophthal Top, IOL-Master and Ophthal Top A1-B1: The linear correlations between Lenstar and Ophtha Top for J0 and J45; C1-D1: The IOL-Master and Ophtha Top. The solid lines represent real correlation lines for the two devices and the dotted lines represent the quality lines; A2-B2: The Bland-Altman plots for Lenstar and Ophtha Top for J0 and J45; C2-D2: The Bland-Altman plots for IOL-Master and Ophtha Top. The solid lines represent the mean values of differences,and the dotted lines represent the 95%LOA values.
Since Ophtha Top topography showed excellent repeatability,we further compared the results with IOL-Master and Lenstar,because different studies have compared Placido-based topography with autokeratometers[2,24]; however, there are few studies on comparisons with Ophtha Top topography.
In our study, the refractive curvatures of Ophtha Top topography were lower than the outcomes of Lenstar and IOLMaster; the differences in Kf, Ks, and Km were 0.36±0.30(95%LOA: -0.23-0.95), 0.41±0.26 (95%LOA: -0.10-0.92), and 0.39±0.25 (95%LOA: -0.12-0.88), respectively, compared with Lenstar. The differences in Kf, Ks, and Km were 0.39±0.23(95%LOA: -0.06-0.84), 0.44±0.26 (95%LOA: -0.07-0.95), and 0.41±0.20 (95%LOA: 0.02-0.80) compared with IOL-Master.According to a study by Eibschitz-Tsimhoni et al[25], the IOL refractive error was 0.8-1.3 D with 1 D keratometric error for both children and adults, here the differences may lead to 0.29-0.53 D IOL refractive error. Another study used corneal power formulas that multiplied the K-readings by approximately 0.9 to measure further errors in IOL power[26]. The resulting mean prediction refractive error here would have been 0.36-0.44 D,since the clinically used IOL had a 0.5 D gradation. The mean differences in corneal curvature readings within 0.5 D may have small influence on the IOL power chosen for most patients.
Huang et al[27] reported a comparison of Lenstar and Pentacam tomography with a 95%LOA for the flattest meridian and steepest meridian, and the mean values were -0.54-0.32 D,-0.63-0.43 D, and -0.53-0.33 D, respectively. Bullimore et al[28] found that the 95%LOA of IOL-Master and manual keratometry for Kf, Ks, and Km was -0.01-0.49 D, 0.02-0.84 D, and 0.08-0.58 D, respectively. Both showed good agreement. Lee et al[26] compared IOL-Master and Pentacam tomography showing good agreement for corneal power with a 95%LOA from -1.02 D to +1.13 D. Mao et al[24] showed that the 95%LOA was -0.27-0.15 D, -0.62-0.28 D, and -0.38-0.15 D for Kf, Ks, and Km, respectively, for IOL-Master and Keratopraph4, which is a Placido-disk topography. Kobashi et al[11] showed the 95%LOA of Kf, Ks, and Km was -0.51-0.48 D, -0.74-0.71 D and -0.56-0.53 D for an autokeratometer and topography. Although the 95%LOA in our study was comparable to the previous studies, we should still consider the predicted refractive errors.
We believed that clinical measurement of corneal parameters can be influenced by many factors. This may explain variations.In our study, the discrepancies in K-readings may be mainly attributed to different testing areas, measurement principles and patient related factors. Ophtha Top topography measures a radial area of 1.0 to 1.5 mm from the center, based on Placidodisk. Lenstar detects an area of 1.65 and 2.30 mm diameters,and IOL-Master detects an approximately 2.3 mm area based on autokeratometry. Pentacam tomography is based on a Placido-disk, integrated with two cameras detecting the cornea with 138 000 true elevation points. A larger testing area may result in flatter K-readings. Additionally, Gonzalez-Meijome[29]suggested that fixation instability, head reorientation and tearrelated events were strongly correlated with measurement variability. Park et al[30] also stressed the importance of maintaining a head up posture during measurement. Tear film stability can also affect the results, especially in the elderly[31].With Ophtha Top topography, the tear film can be supervised during measurements, while with IOL-Master and Lenstar,the influence of the tear film can only be influenced by timely blinking. In addition, we studied patients before cataract surgery who were, on average, 64.74±8.65 years old. Patient cooperativeness has not been considered to be comparable to younger subjects enrolled in most previous studies[24,26-27]. This may also account for the larger differences and wider 95%LOA ranges found in our study.
With both the astigmatism meridian and astigmatism magnitude being recognized as important J0 and J45 were also introduced in the evaluation of astigmatisms, which is believed to be more appropriate for astigmatism measurements[11,21,24]. To our knowledge, few studies have used J0 and J45 to measure the agreement of astigmatism segments between Ophtha Top topography and autokeratometry. According to Thibos’ theory,J0 and J45 represent astigmatism at 90 degrees/180 degrees and 45 degrees/135 degrees, respectively.
The results of astigmatism are shown in Table 4. The mean differences in J0 and J45 with Lenstar-Ophtha Top topography was 0.04±0.13 (95%LOA: -0.21-0.29 D) and 0.01±0.12(95%LOA: -0.23-0.25 D), respectively, and for IOL-Master-Ophtha Top topography, it was 0.03±0.11 (95%LOA: -0.22-0.25 D) and 0.01±0.11 (95%LOA: -0.21-0.23 D), respectively.The IOL-Master-Lenstar was 0.01±0.15 (95%LOA: -0.28-0.30 D)and 0.03±0.10 (95%LOA: -0.17-0.23 D), respectively. The Pearson correlation indexes were all over 0.9. All the 95%LOA values were comparable to previous studies.
Visser et al[10] used the vector analysis method of Holladay to measure corneal astigmatism with IOL-Master, Lenstar, and KR-1W, the difference in astigmatism was small and within 0.1 D. Kobashi et al[11] measured astigmatism with J0 and J45 of ARK-700 and atlas topography, and the 95%LOA ranges for J0 and J45 were from -0.32 to 0.30 D and -0.22 to 0.20 D,respectively. These values were comparable with our results.Mao et al[24] used J0 and J45 to assess differences between Keratopraph4 and IOL-Master and found that the differences between the two devices were small. The 95%LOA values were from -0.19 to 0.29 D and -0.13 to 0.18 D, respectively.This was narrower than our results as well as the results of Kobashi et al[11]. Regarding the differences in 95%LOA for J0 and J45 in our study, the same factors for K-readings may also have played a role. Another reason that should be stressed is the average astigmatism in our patients was within 1.0 D. It has been suggested that a lower astigmatism value was associated with bigger differences[32].
The limitations of our study on the repeatability of Ophtha Top topography include using the same operator for successive measurements at the same time. Further studies with different operators are needed in future studies. In addition, since the devices assessed were mostly used for senior cataract patients,age, measurement times, patient cooperation levels and other factors may affect the agreement between our study and other studies. Also, no complicated corneal surfaces were included,so further study of irregular ocular surfaces and the cornea after refractive surgery is still necessary.
In summary, Ophtha Top topography had excellent repeatability that was comparable to existing Placido-disk topography. Compared with the two other IOL power devices;that is, IOL-Master and Lenstar, although these three devices could provide comparable results for cataract patients, we should stress that the cornea curvature is flatter measured with Ophtha Top topography, also the astigmatism is lower. For clinical application, the differences should be noted.
ACKNOWLEDGEMENTS
The technic support from Department of Cataract and kindly help from Wen-Chen Xue and Huan Wang should be acknowledged.
Conflicts of Interest: Yu SS, None; Song H, None; Tang X,None.
REFERENCES
1 Lee AC, Qazi MA, Pepose JS. Biometry and intraocular lens power calculation. Curr Opin Ophthalmol 2008;19(1):13-17.
2 Wang Q, Savini G, Hoffer KJ, Xu Z, Feng Y, Wen D, Hua Y, Yang F, Pan C, Huang J. A comprehensive assessment of the precision and agreement of anterior corneal power measurements obtained using 8 different devices. PLoS One 2012;7(9):e45607.
3 Yuan X, Song H, Peng G, Hua X, Tang X. Prevalence of corneal astigmatism in patients before cataract surgery in northern china. J Ophthalmol 2014;2014:536412.
4 Yu JG, Zhong J, Mei ZM, Zhao F, Tao N, Xiang Y. Evaluation of biometry and corneal astigmatism in cataract surgery patients from Central China. BMC Ophthalmol 2017;17(1):56.
5 Prasher P, Sandhu JS. Prevalence of corneal astigmatism before cataract surgery in Indian population. Int Ophthalmol 2017;37(3):683-689.
6 Lin D, Chen J, Liu Z, Wu X, Long E, Luo L, Lin Z, Li X, Zhang L,Chen H, Liu J, Chen W, Lin H, Liu Y. Prevalence of corneal astigmatism and anterior segmental biometry characteristics before surgery in Chinese congenital cataract patients. Sci Rep 2016;6:22092.
7 Ale Magar JB, Cunningham F, Brian G. Comparison of automated and partial coherence keratometry and resulting choice of toric IOL. Optom Vis Sci 2013;90(4):385-391.
8 Chang M, Kang SY, Kim HM. Which keratometer is most reliable for correcting astigmatism with toric intraocular lenses? Korean J Ophthalmol 2012;26(1):10-14.
9 Gundersen KG, Potvin R. Prospective study of toric IOL outcomes based on the Lenstar LS 900(R) dual zone automated keratometer. BMC Ophthalmol 2012;12:21.
10 Visser N, Berendschot TT, Verbakel F, de Brabander J, Nuijts RM.Comparability and repeatability of corneal astigmatism measurements using different measurement technologies. J Cataract Refract Surg 2012;38(10):1764-1770.
11 Kobashi H, Kamiya K, Igarashi A, Ishii R, Sato N, Wang G, Shimizu K. Comparison of corneal power, corneal astigmatism, and axis location in normal eyes obtained from an autokeratometer and a corneal topographer.J Cataract Refract Surg 2012;38(4):648-654.
12 Erdelyi B, Csakany B, Nemeth J. Reproducibility of keratometric measurements decreases with time after blinking. Eur J Ophthalmol 2006;16(3):371-375.
13 Einighammer J, Oltrup T, Bende T, Jean B. Calculating intraocular lens geometry by real ray tracing. J Refract Surg 2007;23(4):393-404.
14 Thibos LN, Wheeler W, Horner D. Power vectors: an application of Fourier analysis to the description and statistical analysis of refractive error. Optom Vis Sci 1997;74(6):367-375.
15 Bartko JJ, Carpenter WT Jr. On the methods and theory of reliability. J Nerv Ment Dis 1976;163(5):307-317.
16 Bland JM, Altman DG. Measurement error. BMJ 1996;313(7059):744.
17 Baradaran-Rafii A, Fekri S, Rezaie M, Salehi-Rad S, Moradi A,Motevasseli T, Kalantarion M. Accuracy of different topographic instruments in calculating corneal power after myopic photorefractive keratectomy. J Ophthalmic Vis Res 2017;12(3):254-259.
18 Lin HY, Chen HY, Fam HB, Chuang YJ, Yeoh R, Lin PJ. Comparison of corneal power obtained from VERION image-guided surgery system and four other devices. Clin Ophthalmol 2017;11:1291-1299.
19 Nilforoushan MR, Speaker M, Marmor M, Abramson J, Tullo W,Morschauser D, Latkany R. Comparative evaluation of refractive surgery candidates with Placido topography, Orbscan II, Pentacam, and wavefront analysis. J Cataract Refract Surg 2008;34(4):623-631.
20 Elbaz U, Barkana Y, Gerber Y, Avni I, Zadok D. Comparison of different techniques of anterior chamber depth and keratometric measurements. Am J Ophthalmol 2007;143(1):48-53.
21 Read SA, Collins MJ, Iskander DR, Davis BA. Corneal topography with Scheimpflug imaging and videokeratography: comparative study of normal eyes. J Cataract Refract Surg 2009;35(6):1072-1081.
22 Gonzalez Perez J, Cervino A, Giraldez MJ, Parafita M, Yebra-Pimentel E. Accuracy and precision of EyeSys and Orbscan systems on calibrated spherical test surfaces. Eye Contact Lens 2004;30(2):74-78.
23 Jeandervin M, Barr J. Comparison of repeat videokeratography:repeatability and accuracy. Optom Vis Sci 1998;75(9):663-669.
24 Mao X, Savini G, Zhuo Z, Feng Y, Zhang J, Wang Q, Chen H,Huang J. Repeatability, reproducibility, and agreement of corneal power measurements obtained with a new corneal topographer. J Cataract Refract Surg 2013;39(10):1561-1569.
25 Eibschitz-Tsimhoni M, Tsimhoni O, Archer SM, Del Monte MA.Effect of axial length and keratometry measurement error on intraocular lens implant power prediction formulas in pediatric patients. J AAPOS 2008;12(2):173-176.
26 Lee BW, Galor A, Feuer WJ, Pouyeh B, Pelletier JS, Vaddavalli PK,Lemelman BT, See C, Yoo SH. Agreement between Pentacam and IOL master in patients undergoing toric IOL implantation. J Refract Surg 2013;29(2):114-120.
27 Huang J, Pesudovs K, Wen D, Chen S, Wright T, Wang X, Li Y,Wang Q. Comparison of anterior segment measurements with rotating Scheimpflug photography and partial coherence reflectometry. J Cataract Refract Surg 2011;37(2):341-348.
28 Bullimore MA, Buehren T, Bissmann W. Agreement between a partial coherence interferometer and 2 manual keratometers. J Cataract Refract Surg 2013;39(10):1550-1560.
29 Gonzalez-Meijome JM, Queiros A, Jorge J, Fernandes P, Cervino A,de Almeida JB. External factors affecting data acquisition during corneal topography examination. Eye Contact Lens 2007;33(2):91-97.
30 Park CY, Do JR, Kim SH, Lim CY, Chuck RS. The effect of head tilt on keratometric measurement using the IOLMaster. Eye (Lond) 2013;27(12):1411-1417.
31 Ottobelli L, Fogagnolo P, Guerini M, Rossetti L. Age-related changes of the ocular surface: a hospital setting-based retrospective study. J Ophthalmol 2014;2014:532378.
32 Karabatsas CH, Papaefthymiou I, Aslanides IM, Chatzoulis DZ.Comparison of keratometric and topographic cylinder and axis measurements on normal corneas with low astigmatism. Eur J Ophthalmol 2005;15(1):8-16.