INTRODUCTION
Children are born with an immature visual system;therefore they need clear-focused images for normal visual development to occur. Refractive error is one of the most common causes of visual impairment in children[1-2]. The untreated and uncorrected refractive error (URE) may result in amblyopia, causing blindness[3]. In adults and children, there were an estimated 700 million cases of vision impairment caused by URE worldwide in 2007[4]. In general, in children,the common causes of blindness are vitamin A deficiency[5],measles, meningitis, and congenital rubella syndrome[6-8].
Hence, the burden of URE in children still becomes an important topic to be investigated. It is due to the impact of uncorrected vision impairment in the future, includes reduced employment, educational opportunities, increased morbidity,and poverty[4,9]. Gilbert and Foster[6] estimated the economic cost of vision impairment due to URE reached about 202.000 million USD each year. The increase of URE burden of disease might be underlined by, for instances: the lack of availability of eye care personnel, affordable equipment and spectacles.
Although accurate prevalence data are difficult to be obtained due to large samples required, population-based prevalence surveys are important to profile the pattern of refractive error in a particular area[10-11]. In South East Asia region, the prevalence of uncorrected myopia was 4.5% in Singapore Malay population[12] and in Cambodia, the prevalence of URE was 2.48%[13]. In addition, data from Timor-Leste showed that URE caused 81.3% low vision cases[14]. In Indonesia, the population-based refractive error data, especially in children,are less available. A study was conducted in 2003 found that URE was 12.9% in Sumatra, Indonesia population[15].
Furthermore, the present study aimed to overcome this lack of data in Indonesia, by directly comparing children’s residential area. From previous studies, there were differences between refractive error of school children from rural and urban areas in which the URE were 2.7% and 6.4%, respectively[16-17]. In this study, we compared more residential gradients such as: urban,suburban, exurban and rural, in order to profile the URE based on the characteristic of a socioeconomically heterogeneous population as comprised in Indonesia.
METHODS
Design and Sample Selection This study was a crosssectional study of school children from 3 districts (Yogyakarta City, Bantul and Gunungkidul) in the province of Yogyakarta and 1 district (Magelang) in the province of Central Java,Indonesia. The sample size was calculated using single population proportion formula by taking into consideration the prevalence rate of refractive error among school children.We calculated the sample size according to Lwanga and Lemeshow[18] formula, n=[Z2p(1-p)]/d2 (Z=1.96, d=0.05,p=12.9% or the proportion of URE according to Saw et al[15],n=176). The samples in were taken using consecutive sampling method from 7 elementary schools in Yogyakarta city, 14 elementary schools in Bantul (the area of Goa Cemara and Ganjuran), 5 elementary schools in Gunungkidul (the area of Tepus) and 10 elementary schools in Magelang (the area of Ngablak). Then, according to the population (see operational definition), we grouped Yogyakarta city into urban, Bantul into suburban, Magelang into exurban, and Gunungkidul into rural.
Field Examination Prior to the ophthalmic examination,school teachers were told to screen their students who have visual complaints (either by the children themselves, their parents or the teachers), and ask their students who did not pass the screening to come to the camp held by medical team from the Department of Ophthalmology, Dr. Sardjito General Hospital, Yogyakarta. The informed consent was made clear that children/parents were under no obligation to participate. The basic information of the school children,for instances: age, sex, school and grade, were recorded and were kept confidential. Complete ophthalmic examinations were done, including: initial unaided visual acuity (VA) using Snellen’s chart, inspection of anterior segment using slit lamp bio-microscope, evaluation of posterior segment using direct ophthalmoscope, evaluation of objective (using autorefractometer) and subjective refraction best corrected visual acuity (BCVA). The auto-refractometer results as guide for subjective refraction and did not included into analyses since non-cycloplegic refractometry may overestimate the prevalence of myopia in children with active accommodation[19]. The Snellen’s chart was used to measure the initial VA and to perform the subjective refraction. Necessary eye care services were provided free of charge and children requiring further diagnostic assessment or treatment was provided with an explanation and referred to the hospital/clinic nearest their home. The residential areas of the school children were then divided based on socioeconomic heterogeneous population into urban, suburban, exurban and rural. The study protocol,according to WHO protocol and manual[20] , has been reviewed and approved by local Ethic Committee.
Operational Definitions According to the WHO[20]recommendations on standards for characterization of vision loss and visual functioning, visual impairment and blindness is defined as best corrected vision in the better eye. Therefore,in the present study, only the eye with better VA (or the better eye) were included into the analyses[20]. The spherical equivalent (SE) was calculated as the spherical error plus half of the cylindrical error. Myopia is defined as SE ≤ -0.5 D, high myopia as ≤ -3.0 D, hyperopia as SE ≥ +0.5 D, high hyperopia as ≥ +3.0 D, and astigmatism as DC ≤ -0.5 D[21]. Anisometropia is defined as a difference in SE between the right and left eyes of ≥1.0 D. URE was defined as subjects who presented VA >0.15 logMAR but achieved ≤0.15 logMAR BCVA after refractive correction. VA ≥0.15 logMAR was considered to be normal; 0.15< VA ≤0.5 logMAR was considered as moderate vision impairment; 0.5< VA ≤1.3 logMAR was considered as severe visual impairment; and VA >1.3 logMAR was considered as blindness[22-23].
The Definition of Residential Areas The urban area is a city with population over a million people. Suburban areas consist of dense to semi-dense population, which can vary from 10 000 to over a 1 000 000. Exurban is a commuter town with approximately 1000 to 20 000 people. Rural areas are settled places outside towns and cities with populations under 10 000 people[24-25].
The inclusion criteria were school children with complete socio-demographic clinical examination data, whereas the exclusion criteria was the school children with incomplete data.
Statistical Analysis Data verification was done in the beginning of data management included assessment on measurement frequency distributions, and consistency among related measurements. Cleaned data sets were translated into system files for statistical analysis, conducted on computer using SPSS version 18.0 (USA).
VA, SE, and BCVA were analyzed according to residential areas (urban, exurban, suburban and rural) using one-way ANOVA then followed by Bonferroni adjusted post-hoc pairwise comparison to observe the difference between two variables.
We analyzed the nominal variables included amblyopia(including amblyopia suspect, etc.), and severe vision impairment and blindness using Chi-square (χ2) proportion test and followed by analyzing the relative risk (RR). P<0.05 was considered statistically significant.
RESULTS AND DISCUSSION
In total, we examined 410 school children (who passed the inclusion criteria) from 36 elementary schools taken from 4 residential areas, with the demographic data and characteristic shown in Table 1.
We then analyzed VA, SE and BCVA according to residential areas (urban, suburban, exurban and rural) (Table 2). Using one-way ANOVA, it showed that in VA, there were significant interactions between all residential areas, but not in SE. It was then followed by Bonferroni adjusted post-hoc pairwise comparison which showed that urban area had the lowest VA when compared with exurban (P<0.001) and rural areas(P<0.001), but not with suburban (P<0.309). In less strict posthoc analysis (using LSD-adjusted), urban vs suburban showed marginally significant (P=0.051). However, in BCVA the significant interactions were only between urban vs suburban(P=0.010) and urban vs exurban (P=0.003). It revealed that urban school children had the lowest VA and BCVA compared with other residential area. Using linear regression, it was found that school grader was associated with SE (P=0.019)regardless the area (adjusted P=0.034, area adjusted).
The proportion test using Chi-square (χ2) of severe vision impairment vs normal vision across 4 different residential areas revealed statistically significant result (P<0.001). It also showed that urban and suburban areas had higher risk for developing severe vision impairment and blindness as well as amblyopia (Table 3), but it was not shown in exurban and rural areas.
The proportion of URE (in total) among urban, suburban,exurban and rural area were 10.1%, 12.3%, 3.8%, and 1%,respectively, and it was significant when compared to the proportion of ametropia and corrected refractive error across residential densities (P=0.003). Furthermore, URE was associated with urban and suburban [2.218 (95%CI: 0.914-5.385) and 3.019 (95%CI: 1.266-7.197), respectively] but not with exurban, and rural area [0.502 (95%CI: 0.195-1.293), and 0.130 (95%CI: 0.017-0.972), respectively]. Table 4 shows the prevalence of URE according to residential areas based on the type of refractive error. It showed that the proportion of simple and high myopia proportion were significantly different all across residential areas (P<0.001 and P=0.017, respectively).It also showed that urban areas had higher risk for developing simple myopia (RR=1.913; 95%CI: 1.460-2.506) and high myopia (RR=2.476; 95%CI: 1.305-4.696), whereas in suburban areas the higher risk was only for simple myopia (RR=2.108;95%CI: 1.620-2.742). However, the exurban and rural areas had protective effects for developing simple and high myopia (Table 4).Additionally, we also analyzed the proportion of amblyopia and URE, as well as the proportion of referral to hospital vs eyeglasses prescription using Chi-square (χ2) test and it showed significant result (P=0.003 and P<0.001, respectively).
Table 1 Socio-demographic characteristics (n=410)

SD: Standard deviation.
There were limited studies regarding the prevalence of URE between urban, suburban, exurban and rural school children population. The present study was the first in investigating this issue in Indonesia. This research examined the patterns of visual impairment in children across several gradients of residential density which has different socio-cultural factors and accessibility of affordable eye care services[1,23].
Special attention has to be given to school age because it is the age at which refractive error begins. Failure of normal visual maturation cannot be corrected in adult life, therefore there is a level of urgency about treating childhood eye disease[26].From this study, it showed that severe visual impairment was 21.0% and blindness was 1.2%, in which the majority of students were never examined for the VA. This neglect is in line with the study done by Murthy et al[17] in India population.In our study, in urban areas, the prevalence increased into 31%and 8%, respectively, and increased the risk for developing blindness. It thus revealed the burden of visual problem in school age, and emphasizes the importance of obtaining current empirical data that could be reliably used to plan better eye-care services for children.
This study also revealed the large proportion of myopia and high myopia in urban school children population (myopia:32.68% and high myopia: 8.54%, Table 1) as well as increased risk for the development of URE. The similar socio-demographic characteristic in suburban and urban population made similar results of visual impairment and URE. More specifically, the exurban population showed increased risk for developing severe visual impairment, and simple myopia as similar with the urban population. The one difference was only that exurban population did not show increased risk in developing high myopia.
Table 2 Refractive error characteristics according to residential area
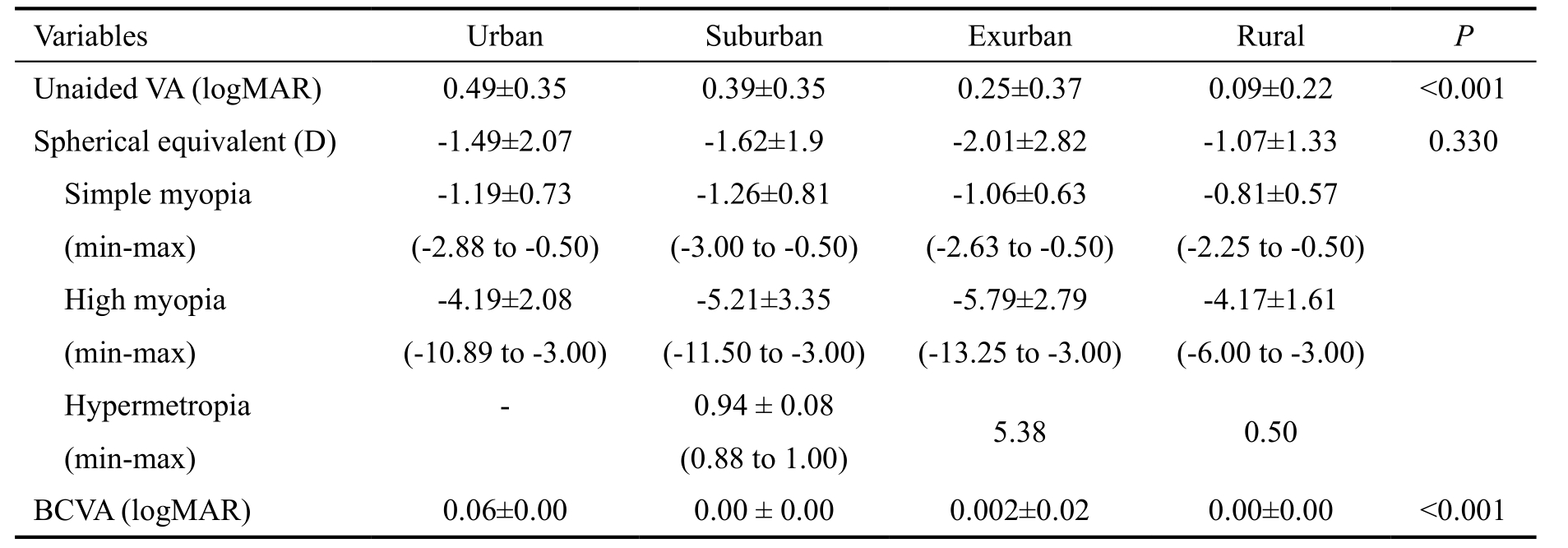
Data in mean±SD (standard deviation); D: Diopters; BCVA: Best corrected visual acuity; 4 groups were analyzed using oneway ANOVA. P<0.05 is considered as significant.
Table 3 Morbidity conditions and residential areas
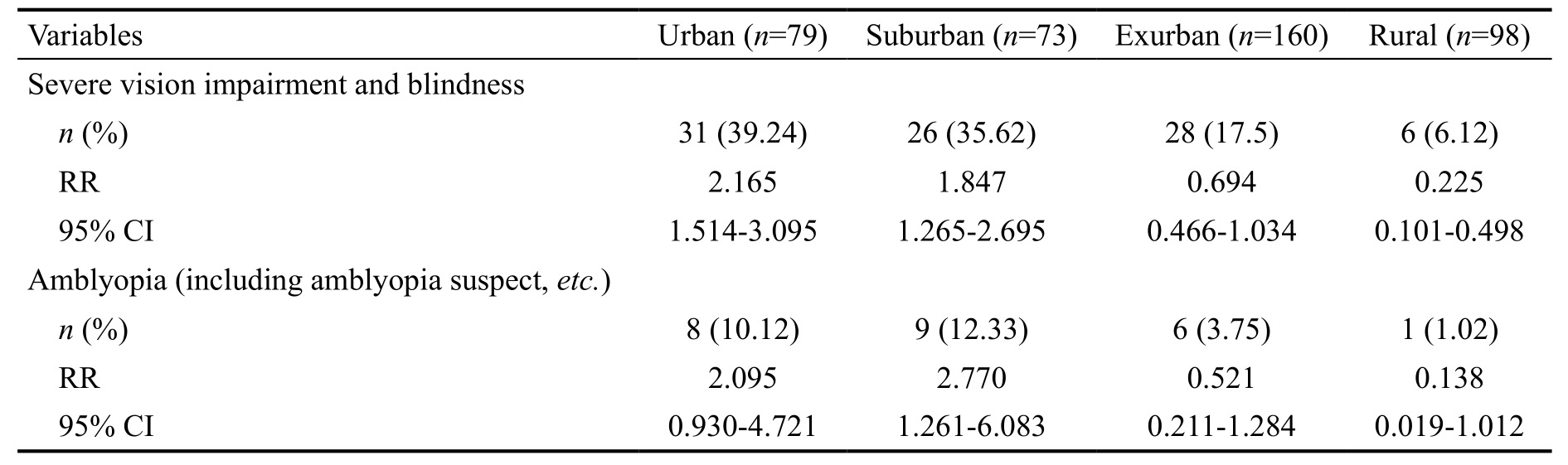
RR: Relative risk; CI: Confidence interval.
Table 4 The prevalence of URE
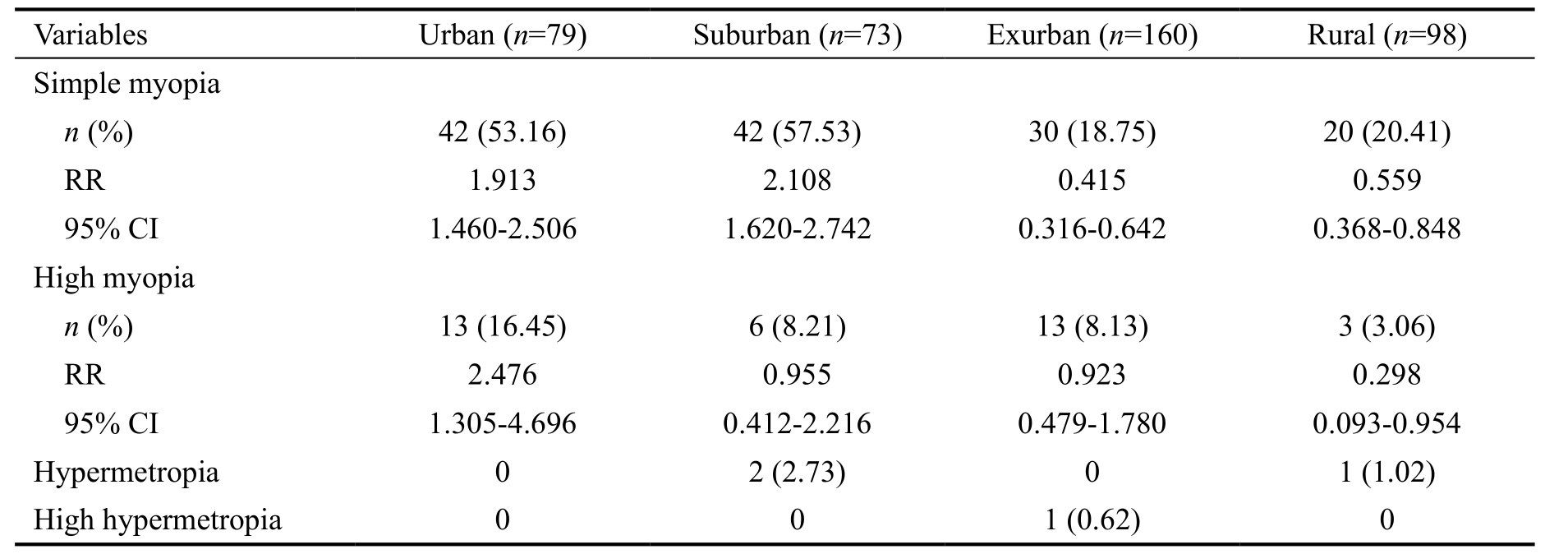
RR: Relative risk; CI: Confidence interval.
This obtained result in urban and exurban population might be underlined by the increased close work activity in urban population[17,27], for instances: reading and using electronic gadget which might be associated with the socioeconomic status. It might reflect other reasons such as the underdeveloped areas (for example: in rural population) are not faced with the same emphasis on schooling. The disparity with exurban and rural population may come from different socio-economic disparities, including infrastructure development or might be due to cultural differences[28].
Limitations of this study include limited sampling that was not representative of some parts of Indonesia population where a significant proportion of school-aged children do not attend school, also although we did direct fundus ophthalmoscopy,we did not take the fundus photograph to see in detail the underlying cause of visual impairment other than refractive error. Furthermore, we also were not asking detailed information about the children’s family.
However, in the future, simple vision-screening examination should be integrated into the school health program[29]. High proportion of blindness in children is due to preventable conditions acquired during childhood. One of the causes is URE, which could be treated easily using spectacles without need of complex management approach (such as surgery).This simple intervention may decrease the burden of visual impairment underlined by URE.
It was concluded that the refractive error is one of the most common causes of visual impairment in school children. In this study, we found that it has a strong relationship with urban and suburban populations. Here, urban school children showed the worst initial VA as well as BCVA. We could reveal that the school children in urban and suburban residential area had 2 times higher risk for developing URE (including: severe visual impairments, blindness and amblyopia). Further study is needed to overcome the limitations of this study. However,this study is expected to generate greater awareness, for development of effective interventions, and for requisite action in the form of better provision of services and methods of prevention.
ACKNOWLEDGEMENTS
We thank our colleagues from Department of Ophthalmology,Faculty of Medicine, Universitas Gadjah Mada, Yogyakarta,Indonesia who provided insight and expertise that greatly assisted the research.
Foundation: Supported by Department of Ophthalmology,Faculty of Medicine, Universitas Gadjah Mada, Yogyakarta,Indonesia.
Conflicts of Interest: Mahayana IT, None; Indrawati SG,None; Pawiroranu S, None.
REFERENCES
1 Pawar PV, Mumbare SS, Patil MS, Ramakrishnan S. Effectiveness of the addition of citicoline to patching in the treatment of amblyopia around visual maturity: a randomized controlled trial. Indian J Ophthalmol 2014;62(2):124-129.
2 Ramachandra K, Gilyaru S, Eregowda A, Yathiraja S. Prevalence of refractive error and the eye morbidity in school children in Bangalore,India. Int J Contemp Pediatr 2016;3(1):138-141.
3 Xiao O, Morgan IG, Ellwein LB, He M; Refractive Error Study in Children Study Group. Prevalence of amblyopia in school-aged children and variations by age, gender, and ethnicity in a multi-country refractive error study. Ophthalmology 2015;122(9): 1924-1931.
4 Fricke TR, Holden BA, Wilson DA, Schlenther G, Naidoo KS,Resnikoff S, Frick KD. Global cost of correcting vision impairment from uncorrected refractive error. Bull World Health Organ 2012;90(10):728-738.
5 Stevens GA, Bennett JE, Hennocq Q, et al. Trends and mortality effects of vitamin A deficiency in children in 138 low-income and middle-income countries between 1991 and 2013: a pooled analysis of population-based surveys. Lancet Glob Health 2015; 3(9):e528-e536.
6 Gilbert C, Foster A. Childhood blindness in the context of VISION 2020--the right to sight. Bull World Health Organ 2001;79(3):227-232.
7 Guo X, He M. Childhood blindness: more useful evidence from blind school survey. Asia Pac J Ophthalmol (Phila) 2015;4(6):319-320.
8 Kaur G, Koshy J, Thomas S, Kapoor H, Zachariah JG, Bedi S. Vision screening of school children by teachers as a community based strategy to address the challenges of childhood blindness. J Clin Diagn Res 2016;10(4):NC09-14.
9 Agrawal D, Singh JV, Garg SK, Chopra H, Roy R, Chaturvedi M.Current trends in eye diseases and its correlates in an urban population.Indian J Community Health 2015;27(1):41-45.
10 Rudnicka AR, Kapetanakis VV, Wathern AK, Logan NS, Gilmartin B,Whincup PH, Cook DG, Owen CG. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: implications for aetiology and early prevention. Br J Ophthalmol 2016;100(7):882-890.
11 Williams KM, Verhoeven VJ, Cumberland P, et al. Prevalence of refractive error in Europe: the European Eye Epidemiology (E(3))Consortium. Eur J Epidemiol 2015;30(4):305-315.
12 Lamoureux EL, Saw SM, Thumboo J, Wee HL, Aung T, Mitchell P,Wong TY. The impact of corrected and uncorrected refractive error on visual functioning: the Singapore Malay Eye Study. Invest Ophthalmol Vis Sci 2009;50(6):2614-2620.
13 Gao Z, Meng N, Muecke J, Chan WO, Piseth H, Kong A,Jnguyenphamhh T, Dehghan Y, Selva D, Casson R, Ang K. Refractive error in school children in an urban and rural setting in Cambodia.Ophthalmic Epidemiol 2012;19(1):16-22.
14 Ramke J, Palagyi A, Naduvilath T, du Toit R, Brian G. Prevalence and causes of blindness and low vision in Timor-Leste. Br J Ophthalmol 2007;91(9):1117-1121.
15 Saw SM, Husain R, Gazzard GM, Koh D, Widjaja D, Tan DT.Causes of low vision and blindness in rural Indonesia. Br J Ophthalmol 2003,87(9):1075-1078.
16 Dandona R, Dandona L, Srinivas M, Sahare P, Narsaiah S, Muñoz SR, Pokharel GP, Ellwein LB. Refractive error in children in a rural population in India. Invest Ophthalmol Vis Sci 2002;43(3):615-622.
17 Murthy GV, Gupta SK, Ellwein LB, Muñoz SR, Pokharel GP, Sanga L, Bachani D. Refractive error in children in an urban population in New Delhi. Invest Ophthalmol Vis Sci 2002;43(3):623-631.
18 Lwanga SK, Lemeshow S. Sample size determination in health studies:a practical manual. Sample size determination in health studies:World Health Organization; 1991.
19 Funarunart P, Tengtrisorn S, Sangsupawanich P, Siangyai P. Accuracy of noncycloplegic refraction in primary school children in southern Thailand. Chotmaihet Thangphaet 2009;92(6):806-811.
20 World Health Organization. Protocol and Manual of Procedures:Assessment of the Prevalence of Visual Impairment Attributable to Refractive Error or Other Causes in School Children. Geneva: World Health Organization; 2007.
21 Queirós A, González-Méijome J, Jorge J. Influence of fogging lenses and cycloplegia on open-field automaticrefraction. Ophthalmic Physiol Opt 2008;28(4):387-392.
22 Ferraz FH, Corrente JE, Opromolla P, Schellini SA. Influence of uncorrected refractive error and unmet refractive error on visual impairment in a Brazilian population. BMC Ophthalmol 2014;14:84.
23 Foster A, Gilbert C. Epidemiology of childhood blindness. Eye (Lond)1992;6(Pt 2):173-176.
24 Nelson AC. Characterizing exurbia. J Plan Lit 1992;6(4):350-368.
25 Ban H, Ahlqvist O. Representing and negotiating uncertain geospatial concepts-Where are the exurban areas? Comput Environ Urban Syst 2009;33(4):233-246.
26 Holden B, Davis S, Jong M, Resnikoff S. The evolution of uncorrected refractive error as a major public health issue. J proc R Soc New South Wales 2014;147(453):101.
27 Saxena R, Vashist P, Tandon R, Pandey RM, Bhardawaj A, Menon V, Mani K. Prevalence of myopia and its risk factors in urban school children in Delhi: The North India Myopia Study (NIM Study). PLoS One 2015;10(2):e0117349.
28 Sewunet SA, Aredo KK, Gedefew M. Uncorrected refractive error and associated factors among primary school children in Debre Markos District, Northwest Ethiopia. BMC Ophthalmol 2014;14:95.
29 Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, Wong TY, Naduvilath TJ, Resnikoff S. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050.Ophthalmology 2016;123(5):1036-1042.