Dear Editor,
P remacular hemorrhage is a common cause of sudden profound visual loss in otherwise healthy eye. One of the commonest causes of premacular hemorrhage in clinical practice is Valsalva retinopathy, which was first described by Thomas Duane in 1972[1]. In the setting of Valsalva retinopathy these hemorrhages are a result of ruptured perifoveal capillaries because of raised intravenous pressure of the eye.This happens when the raised intra-thoracic pressure due to Valsalva maneuver is transmitted to the ocular venous system because of valve-less nature of the later. While the exact location of these hemorrhages has been disputed, they can be present in the sub-hyaloid and/or the sub-internal limiting membrane (sub-ILM) space[2].
Various therapeutic options for premacular hemorrhage in Valsalva retinopathy include observation, laser membranotomy and vitrectomy. Since a large proportion of these hemorrhages resolve on their own, observation is usual initial recommendation especially for small hemorrhages. Large hemorrhages may however persist for long duration and may lead to toxic damage to the underlying retina by hemoglobin and its catabolites[3-4]. Laser membranotomy is a simple, outpatient procedure that releases the hemorrhage into the vitreous gel and expedites the process of visual recovery[5]. Laser membranotomy however is reserved for relatively fresh cases(less than one week old), as liquid state of blood is paramount for the success of this procedure.
With the advent of safe suture less micro-incision vitrectomy systems, surgeons worldwide have a lower threshold for surgical evacuation of such hemorrhages. It is the treatment of choice for patients presenting late (more than 4-6wk) and where haemorrhage fails to resolve spontaneously. Vitrectomy also prevents sequelae like persistent vitreous hemorrhage,epiretinal membrane and premacular cavity seen frequently following laser membranotomy[5-7]. Vitrectomy is also the preferred treatment modality where hemorrhage fails to resolve following observation or laser membranotomy.
This is a retrospective study of three eyes of three patients with long standing premacular hemorrhage due to Valsalva retinopathy that underwent 25-gauge pars plana vitrectomy(PPV). After vitrectomy, the patients were evaluated using spectral domain optical coherence tomography (SD-OCT)to assess morphological effects of long standing hemorrhage on retinal tissue. Systemic medical work-up was performed to rule out other predisposing factors such as hypertension,diabetes mellitus, and bleeding disorders. All three patients had old premacular hemorrhage (history of more than one month)along with evident whitish discoloration of blood due to dehemoglobinization. The patients were evaluated with respect to best-corrected visual acuity (BCVA, Snellen’s), colour fundus photographs and SD-OCT and underwent 25-gauge PPV. Informed consent was obtained from all the patients. The study was done according to the institutional guidelines and in accordance with the Declaration of Helsinki.
Case 1 A 32-year-old otherwise healthy female presented with sudden visual loss in her left eye that occurred eight weeks back following a bout of coughing. There were no systemic complaints. The right eye was unremarkable with BCVA of 20/20. BCVA in the left eye was hand movements.Anterior segment of the left eye was normal. Dilated fundus examination of left eye showed premacular altered hemorrhage of approximately 3-disc diameters area (Figure 1A). After informed consent, the patient underwent 25-gauge PPV.Following triamcinolone acetonide (TA) assisted posterior vitreous detachment (PVD), blood was found to be present in the sub-ILM space. The ILM was stained with Brilliant blue-G (BBG) dye and hemorrhage was aspirated passively after peeling the ILM (Figure 1B). Standard postoperative care along with topical steroids and cycloplegic were prescribed.At one month, BCVA improved to 20/30. Fundus examination showed resolution of hemorrhage and a whitish line corresponding to the outer margin of sub-ILM hemorrhage(Figure 1C). Horizontal SD-OCT scan through the fovea(Figure 1D) showed shallow foveal contour, thinning of temporal retina, localized disruption of interdigitation zone(IZ, white arrows) and irregular outer plexiform layer (OPL)showing hyper reflective processes extending into the outer nuclear layer (ONL). At six months BCVA was maintained at 20/30 and SD-OCT picture remained unchanged (Figure 1E).The patient was advised regular follow up.

Figure 1 Details of Case 1 Colour photograph of left eye of Case 1 showing altered premacular hemorrhage (A); Intraoperative photograph shows presence of hemorrhage below the stained ILM, which is being peeled (B); Postoperative fundus photograph shows resolution of hemorrhage and outer boundary of hemorrhage is visible as white line (C); At one month, SD-OCT (D) showed localized loss of interdigitation zone (white arrows), flattened foveal contour, temporal retinal thinning and abnormalities of Henle’s fiber layer that persisted at six months (E).
Case 2 A 19 years old male presented with severe decreased vision in his right eye since six weeks following a gym session of heavy weight lifting. There were no systemic complaints.The left eye was normal with BCVA of 20/20. The right eye BCVA was finger counting. Fundus showed an elongated premacular hemorrhage the central part of which showed white discoloration (Figure 2A). SD-OCT showed premacular hyper reflective lesion with shadowing underneath (Figure 2A). After informed consent the patient underwent 25-gauge PPV. After PVD induction, BBG dye assisted ILM peeling was done, as the hemorrhage was sub-ILM (Figure 2B). After evacuation of hemorrhage, appearance of macular hole was noted (Figure 2C). Fluid-air exchange was done and 20% SF6 was injected.The patient was advised standard postoperative care along face down position for 48h.
At one week, BCVA in the right eye was 20/30. Fundus examination still had appearance of macular hole (Figure 1D,blue arrow). SD-OCT revealed abnormally deep foveal contour and abnormalities in the Henle’s fiber layer (HFL, Figure 1E).
At one month, BCVA improved to 20/20. SD-OCT showed mild blunting of foveal contour and persisting Hflchanges(Figure 1F). The patient did not return for subsequent followups.
Case 3 A 50 years old male presented with sudden vision loss in his left eye over two months following a bout of coughing.There were no systemic complaints. The right eye was normal while left eye had BCVA of 20/100. The patient reported a large central scotoma. Dilated fundus examination showed an old premacular hemorrhage with total white discoloration of blood. The hemorrhage partially spared the fovea (Figure 3A). SD-OCT showed a dome shaped premacular bleed. After informed consent patient was undertaken for 25-gauge PPV.The hemorrhage was noted to be present in the subhyaloid space and could be aspirated along with TA crystals that were used for assisting PVD (Figure 3B). ILM peeling was therefore not attempted.
At one week, BCVA was 20/20. The patient reported resolution of scotoma and fundus showed clear media along with clearing of premacular hemorrhage (Figure 3C). SD-OCT showed normal scans (Figure 3D). The clinical picture remained unchanged at one and three months.
The premacular hemorrhages are presumed to be harmful to the underlying retina if longstanding. This could be due to the direct chemical effects of hemoglobin and its productsor mechanical effects of hemorrhage when contained in a “tight”sub-ILM compartment[3-4]. Since premacular hemorrhage results in sudden visual loss the patients tend to present early. Nd:YAG laser membranotomy being a simple, quick,inexpensive and effective procedure is often utilized for management of these hemorrhages. Laser membranotomy improves the visual acuity rapidly and may leave behind a premacular cavity without any disturbances in the retina(Figure 4)[7]. The exact pathological effects of long standing hemorrhage are thus unknown in the literature.

Figure 2 Details of Case 2 with sub-ILM haemorrhage following PPV Colour picture of Case 2 showing elongated premacular hemorrhage with discoloration in front of fovea (A); SD-OCT shows dome shaped hyper-reflectivity with shadowing underneath (inset); Intraoperative picture shows presence of hemorrhage after peeling the ILM (B); A macular hole is appreciated after clearing the hemorrhage (C); The postoperative photograph at one week shows resolution of hemorrhage and appearance of macular hole (D); SD-OCT at one week shows deepened foveal contour, temporal thinning and Henle’s fiber layer abnormalities (E). At one month, SD-OCT (F) shows normalization of foveal contour and with persistence of other features.

Figure 3 Details of Case 3 with subhyaloid haemorrhage Colour picture of left eye of Case 3 showing discolored premacular bleed (A);Intraoperative photograph shows premacular hemorrhage being aspirated along with triamcinolone crystals used for induction of PVD (B);Colour photograph at one-week (C) shows resolution of hemorrhage and normal SD-OCT scan (D).
All three patients in our series presented late after the initial episode and showed partial or complete alteration of hemorrhage. Nd:YAG laser membranotomy was therefore not attempted and patients were subjected to 25-gauge PPV for early restoration of vision as well as prevent effects of hemorrhage on the underlying macula.
In the first two cases, hemorrhage was in the sub-ILM space and could be removed only after ILM peeling. Interestingly both of these patients showed post-operative SD-OCT abnormalities. The first patient had flattening of foveal contour and focal loss of IZ. The second patient had steep foveal contour, which accounted for intra-operative appearance of macular hole. This appearance could have been due to centripetal forces exerted by stretched ILM (by the blood) on the underlying retina. These patients also showed thinning of temporal macula and abnormalities in the HFL. Though the thinning of temporal macula may possibly be ascribed to ILM peeling, changes seen in Hflhave not been described before[8].In the study by Treumer et al[8] changes in the retinal thickness due to ILM peeling were noted to occur late (mean of 46mo).However, retinal thickness changes evident in this study were seen in the early postoperative period and are unlikely to be due to ILM peeling alone. These effects in fact may be due to chemical and/or mechanical effects of premacular hemorrhage.In the third case hemorrhage was in the subhyaloid space and could be evacuated without peeling the ILM. Postoperative SD-OCT showed minimal changes despite of the fact that hemorrhage was of longest duration in this patient. There was early (at one week) recovery of good vision (20/20). This could point towards the barrier effect of ILM to the effects of premacular hemorrhage on the underlying retina.
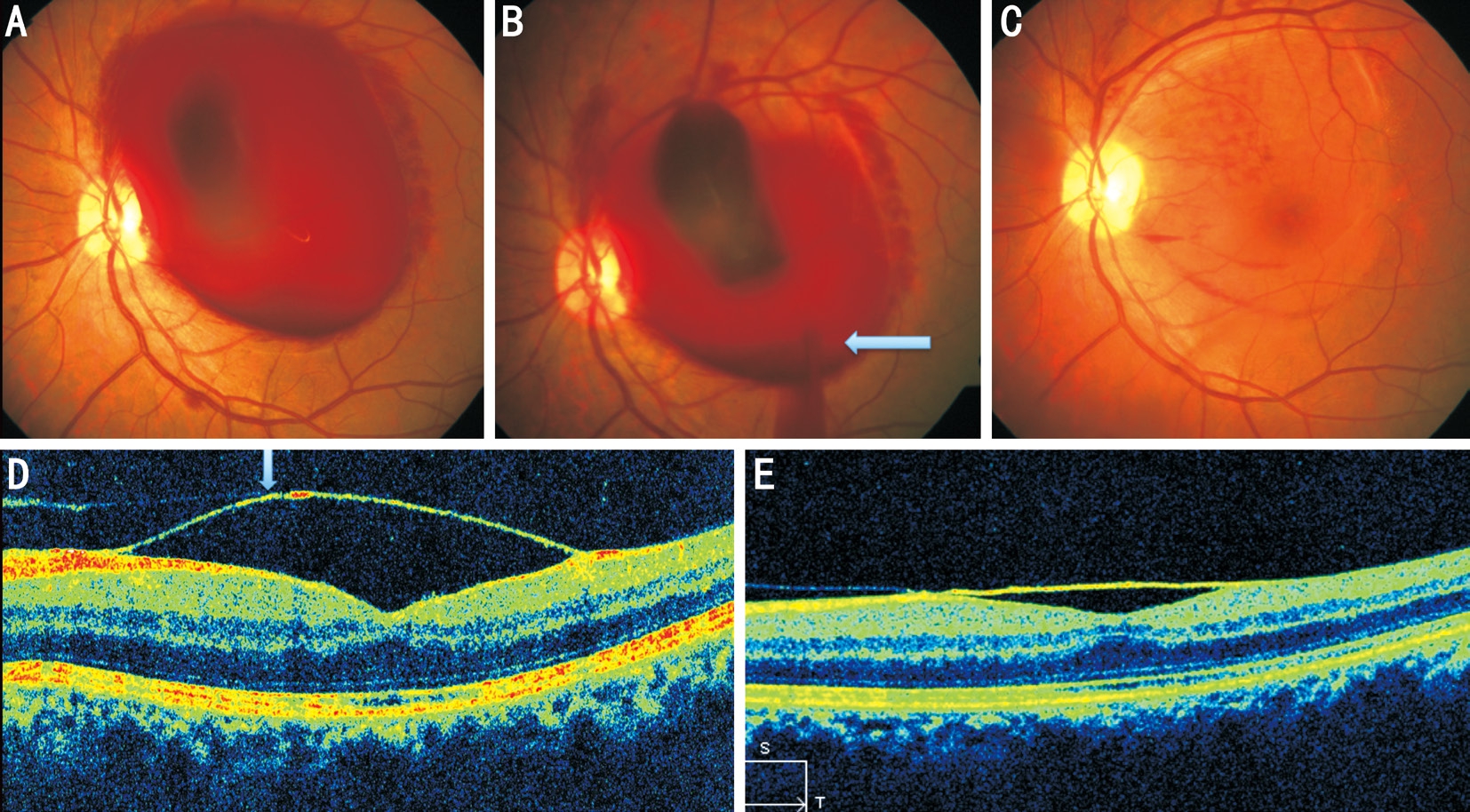
Figure 4 SD-OCT changes following hyaloidotom in premacular hemorrhage Colour picture of left eye (A) of a young male with premacular haemorrhage due to Valsalva retinopathy; Colour photograph of same eye immediately (B) and three weeks after laser membranotomy (C) showing draining blood (arrow) and clear macula respectively. SD-OCT at three weeks follow-up (D) shows premacular cavity bound by two separate layers (posterior hyaloid and ILM, arrow); At three months follow-up, retina is normal with shallow premacular cavity persisting (E).
Vitrectomy has been earlier reported in patients with sub-ILM hemorrhages of various causes and in Valsalva retinopathy;in none of the reported cases however preoperative colour alterations of haemorrhage were reported[9-10]. Apart from few complications like macular hole[11], good visual results have been reported in these studies. The literature however is silent on the postoperative OCT findings.
There are several drawbacks of this study. Apart from being retrospective, the sample size is small. However a clinical situation where patients present late with alteration of haemorrhage is quite rare. An objective test of macular function such as multi-focal electroretinogram could have given more information on its functional status.
To conclude, PPV may provide good visual outcomes in patients with long standing premacular hemorrhage in spite of structural changes in the retina. SD-OCT should be performed routinely in such eyes postoperatively to find the effects of such hemorrhages on the underlying retina.
ACKNOWLEDGEMENTS
Conflicts of Interest: Kumar V, None.
REFERENCES
1 Duane TD. Valsalva hemorrhagic retinopathy. Trans Am Ophthalmol Soc 1972;70:298-313.
2 Meyer CH, Mennel S, Rodrigues EB, Schmidt JC. Is the location of valsalva hemorrhages submembranous or subhyaloidal? Am J Ophthalmol 2006;141(1):231-232.
3 Kuhn F, Morris R, Witherspoon CD, Mester V. Terson syndrome. Results of vitrectomy and the significance of vitreous hemorrhage in patients with subarachnoid hemorrhage. Ophthalmology 1998;105(3):472-477.
4 Ulbig MW, Mangouritsas G, Rothbacher HH, Hamilton AM,McHugh JD. Long-term results after drainage of premacular subhyaloid hemorrhage into the vitreous with a pulsed Nd:YAG laser. Arch Ophthalmol 1998;116(11):1465-1469.
5 Durukan AH, Kerimoglu H, Erdurman C, Demirel A, Karagul S.Long-term results of Nd:YAG laser treatment for premacular subhyaloid haemorrhage owing to Valsalva retinopathy. Eye (Lond) 2008;22(2):214-218.
6 Kwok AK, Lai TY, Chan NR. Epiretinal membrane formation with internal limiting membrane wrinkling after Nd: YAG laser membranotomy in valsalva retinopathy. Am J Ophthalmol 2003;136(4):763-766.
7 Goel N, Kumar V, Seth A, Raina UK, Ghosh B. Spectral-domain optical coherence tomography following Nd:YAG laser membranotomy in valsalva retinopathy. Ophthalmic Surg Lasers Imaging 2011;42(3):222-228.
8 Treumer F, Wacker N, Junge O, Hedderich J, Roider J, Hillenkamp J.Foveal structure and thickness of retinal layers long-term after surgical peeling of idiopathic epiretinal membrane. Invest Ophthalmol Vis Sci 2011;52(2):744-750.
9 De Maeyer K, Van Ginderdeuren R, Postelmans L, Stalmans P, Van Calster J. Sub-inner limiting membrane haemorrhage: causes and treatment with vitrectomy. Br J Ophthalmol 2007;91(7):869-872.
10 García Fernández M, Navarro JC, Castaño CG. Long-term evolution of Valsalva retinopathy: a case series. J Med Case Rep 2012;6:346.
11 Kim KY, Yu SY, Kim M, Kwak HW. Macular hole formation after pars plana vitrectomy for the treatment of Valsalva retinopathy: a case report.Korean J Ophthalmol 2014;28(1):91-95.