INTRODUCTION
Upper eyelid cicatricial entropion (UCE) presents a complex challenge for the eyelid surgeon in terms of management[1-2]. Although numerous surgical techniques with many modifications have been described to correct this condition, none of them offers the ultimate solution[1-4]. There is anatomic and physiologic balance between the anterior and the posterior upper eyelid lamellae keeping the eyelid margin in the normal position[5]. In cicatricial entropion, which has a very complex and dynamic mechanism, this normal balance is damaged[6-9]. Posterior lamellar shortening exerts a direct pull on the skin of the lid margin and redirects the anterior lamellar structures, so that the lashes are directed towards the globe[2,6,8-9]. This can be aggravated by other eyelid abnormalities and involutional changes that often coexist with UCE, especially in long standing cases and aged patients including dermatochalasis, blepharoptosis, lid retraction, and brow ptosis. UCE correction without addressing these issues may lead to a failure of the functional goal of surgery and significant patient dissatisfaction[7-11].
Anterior lamellar recession (ALR) is a well-known conventional surgical method for the correction of a mild to moderate upper lid entropion. It consists of splitting skin and orbicularis oculi muscle from tarsus and conjunctiva, recessing the anterior lamella and leaving the exposed tarsus bare[2-4,8-9]. Interlamellar separation can be performed through lid margin approach,eyelid crease approach, or both[8-17]. Few studies are available that present the effect of this procedure through upper lid crease incision in UCE[18].
In this study, the authors reviewed the surgical outcome of their approach for UCE correction based on addressing commonly associated lid problems including dermatochalasis,brow ptosis, blepharoptosis, and lid retraction and on the postsurgical aesthetic concerns in combination with ALR through an eyelid crease incision.
SUBJECTS AND METHODS

Figure 1 Intraoperative photographs showing steps of ALR combined with levator recession in a 48-year-old male with a history of bilateral upper eyelid entropion and retraction secondary to trachoma A: The anterior lamella (skin and orbicularis) has been dissected off the tarsal plate beyond the lash follicles; B: Upper lid retractors have been dissected from the superior border of the tarsus plate; C: The anterior lamellar flap with the aberrant lashes is recessed superiorly without tension.
This is a retrospective, non-comparative case series of consecutive patients with mild to moderate UCE who underwent correction with a minimum postoperative followup of 6mo from 2014 to 2016. The research adhered to the tenets of the Declaration of Helsinki and was conducted after the approval of the Ethical Review Committee of Fayoum University Faculty of Medicine. UCE surgery involved ALR through an upper lid crease incision with specific correction of the coexisting lid abnormalities including dermatochalasis,brow ptosis, blepharoptosis, and lid retraction through the same incision. Patients with severe UCE who needed posterior lamellar grafts were excluded. The charts of the included patients were reviewed for age, sex, possible underlying etiology, extent of involvement, accompanying eyelid abnormalities, and follow-up period. Outcomes were assessed based on the extent of eyelid margin eversion, the direction of the lashes, the palpebral fissure height (PFH), the corneal status, the wound healing of the split eyelid margin,the cosmesis, the postoperative complications, and the frequency of recurrence. Success was defined as the lack of any lash affecting the globe without additional treatment, and acceptable cosmesis at the final follow-up examination.
Surgical Technique General anesthesia was used for children.For adults, a local anesthetic (5 mL of 2% lidocaine with epinephrine 1:100 000) was injected into the subcutaneous plane of the lid to be operated upon. Different operative plans were determined according to the concurrent eyelid abnormalities.
Preoperative skin marking The inferior incision was placed 2-3 mm below the intended eyelid-crease across the entire lid and shaped slightly upwards and outwards into the lateral canthus. The second incision was made at a variable distance away from the second line, according to the amount of redundant skin to be excised.
Operative procedure 1) The skin incision was made along the markings with a #15 scalpel blade. A myocutaneous flap was developed and dissected off the orbital septum; 2) Transeyelid browpexy was selectively performed through the upper incision for simultaneous correction of brow ptosis. Dissection continued on the surface of the orbital septum beneath the brow fat to the superior orbital rim then in a preperiosteal plane. A 4-0 prolene suture was then placed through the periosteum at 10 mm above the orbital rim. The suture was then placed through the brow fat; 3) The orbital septum was selectively opened to expose the levator aponeurosis: the levator and Müller’s muscle were dissected free from the conjunctiva, the levator was then recessed to make a correction for a preexisting lid retraction, or the underlying aponeurosis was repaired to address a concurrent ptosis; 4) Dissection continued between the tarsus and the pretarsal anterior lamella using Westcott scissors to expose the anterior tarsal surface peeling the whole anterior lid margin with aberrant lashes and keratinizaton away from the tarsus, the anterior lamella was completely dissociated from the tarsus with creation of a bipedicle flap;5) The bipedicle flap was then repositioned superiorly to leave 3 mm of bare tarsus at the eyelid margin and sutured to the anterior tarsal surface using 3 to 4 interrupted mattress sutures;6) The skin edge was closed using sutures to incorporate the levator aponeurosis to reform the eyelid crease; 7) The anterior tarsal surface was left bare to epithelialize secondarily (Figure 1).
Statistical Analysis Statistical analysis was performed using SPSS 16.0 statistical software package. Results were presented as the frequencies, percent for qualitative data, mean and standard deviation for quantitative variables. Statistical analysis of pre- and postoperative outcome changes was performed using paired t-test. The results were considered statistically significant if P was less than 0.05.
RESULTS
Fifty (73.5%) patients were female and 18 (26.5%) patients were male. The mean patient age was 46y (range, 18-56y).The mean follow up period was 17.8mo (range, 6.0-24.0mo).Trachoma was the most common underlying diagnosis with 94 eyelids involved (96.6%). One patient (2 eyelids)had a diagnosis of ocular cicatricial pemphigoid and one patient (1 eyelid) had a diagnosis of Kindler syndrome.Concurrent dermatochalasis was found in 64 eyelids (66.0%),blepharoptosis in 19 eyelids (19.6%), upper lid retraction in 18 eyelids (18.6%), and brow ptosis in 31 eyelids (32.0%).
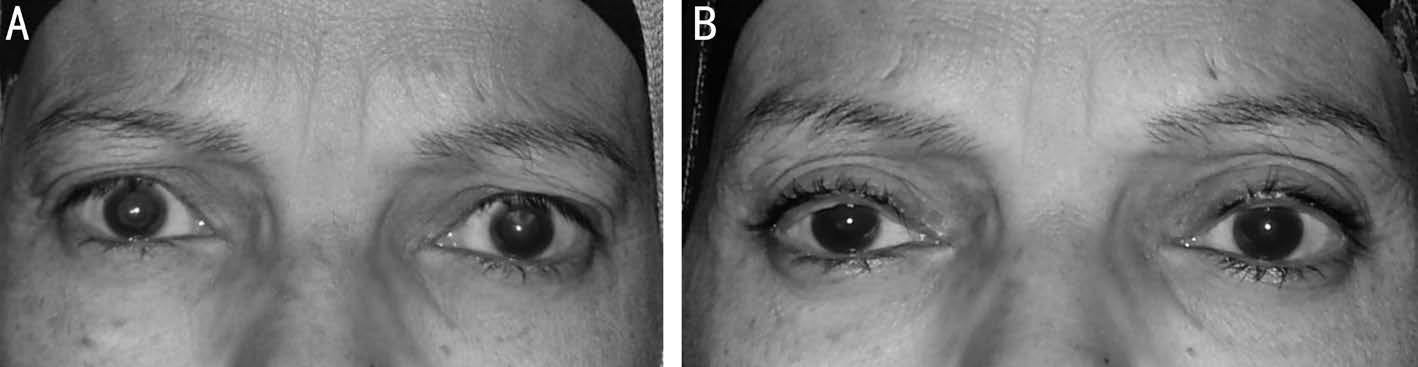
Figure 2 A 46-year-old female patient with bilateral UCE and concurrent moderate lid retraction who underwent bilateral ALR combined with upper lid retractor recession A: Pre-operative appearance; B: Six months post-operative appearance.
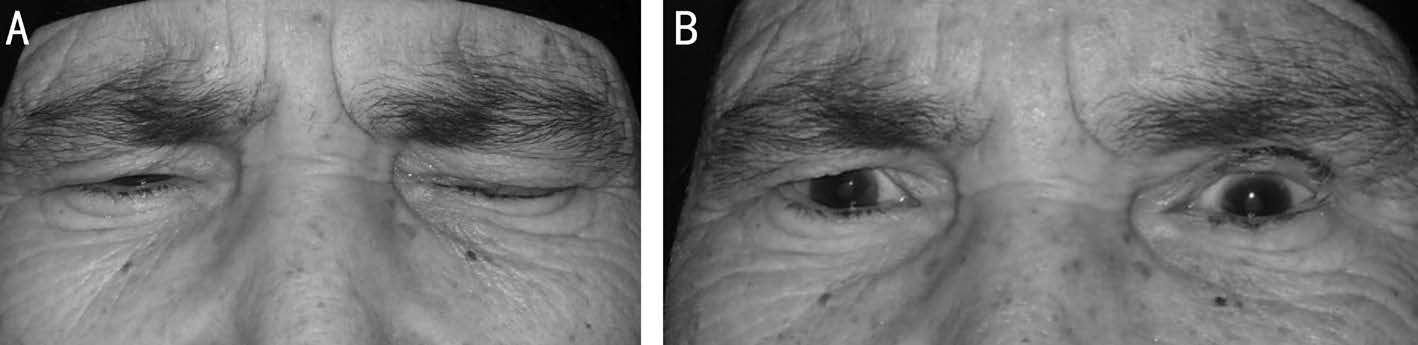
Figure 3 A 55-year-old female patient, with left UCE with secondary blepharospam and brow ptosis who underwent combined ALR and internal browpexy on the left A: Pre-operative appearance; B: Three months post-operative appearance. The patient has residual upper eyelid retraction; however, her symptoms of ocular irritation have resolved.

Figure 4 A 70-year-old male patient with bilateral UCE and concurrent bilateral brow ptosis and ptosis A: Pre-operative appearance; B:Postoperative appearance 6mo after undergoing bilateral ALR combined with blepharoplasty, internal browpexy, and levator tucking; C: When up-gazed, no eyelashes touched the globe, and the exposed tarsus was smoothly covered by the re-epithelised epidermis.
Apart from concurrent blepharoplasty, 54 combined procedures were performed to correct UCE and other associated lid problems. Upper lid retractor recession was performed for 18 eyelids (18.6%) (Figure 2), internal browpexy for 31 eyelids(32.0%) (Figure 3), and levator tucking for 19 eyelids (19.6%)(Figure 4). There was significant improvement of subjective discomfort in all patients and punctate epithelial erosions disappeared in 63 eyes (98.4% of 64 eyes with preoperative lesions). All separated eyelid margins had epithelialized within 2 to 3wk. Younger patients were anecdotally noted to epithelialize more quickly than older patients (Figure 5). All lids showed marginal thickening after surgery that softened over time and disappeared by the 3rd month. Complete success with no lashes touching the globe was achieved in 86 lids(90.5%). Six lids (6.2%) had recurrence of ≤5 trichiatic lashes.Electrolysis was successful in five of them that were considered partial success as no further surgeries were performed for them. The procedure was repeated in 4 eyelids (4.2%). Two of whom had postoperative flap overlap, one had recurrent trichiasis with failed electrolysis, and one had overcorrection and lid retraction. There was no significant effect of age(P=0.69), gender (P=0.7), involved side (P=0.488) or extent of entropion (P=0.720) on the success rate. The degree of entropion correction (the amount of anterior lamella uplift)appeared to be the only factor affecting the success rate.
At 6mo after surgery, patients were asked whether the results of the procedure were cosmetically acceptable to them. If not, they were asked to state their reasons for dissatisfaction.Ninety-two patients (96.8%) were satisfied, 1 was neither satisfied nor dissatisfied, and 2 were dissatisfied. Central lid notch and overcorrection with lateral flare were the reasons for the 2 patients with dissatisfaction. Postoperative complications included 5 cases of flap necrosis (5.2%), 2 cases of flap overlap(2.1%), 6 cases of trichiasis recurrence (6.3%), 2 cases of madarosis (2.1%), and 2 cases of overcorrection (2.1%). Flap necrosis ranged from epidermolysis to full-thickness necrosis,and was managed conservatively and healed completely with residual madarosis in 2 lids and central notch in one lid.However, this did not alter the lid margin position or cause recurrent trichiasis. There were no cases of postoperative ectropion, lagophthalmos, pyogenic granuloma, infections, and eyelash ptosis.
DISCUSSION

Figure 5 A close up photograph of the left eyelid of a 13-year-old female child demonstrating that the bare tarsus color “normalized”rapidly and the lid margin appears in a good position with lashes directed upwards 4wk after ALR compared to the preoperative photo.
Despite of the diversity of the techniques available for correction of UCE, a significant recurrence rate (21%-71%) was reported in most surgical series[1-3]. ALR is an established procedure for treating cicatricial entropion with reported superior success rate (72%-89%)[2,4,12-17]. The procedure for ALR adopted in this study was similar to the technique described by Bi et al[8] and Ross et al[3] with a few modifications. Instead of dissection at two sites, i.e. the grey line and superior lid crease as described by others, the dissection was performed only through the upper lid crease incision and down to the lid margin as the lid margin is usually distorted in UCE with no identifiable grey line[3-4,7-9,13-17]. This approach allows for more accurate and meticulous dissection especially at the lid margin without losing the tissue plane or inadvertently cutting through the tarsal plate. Dissection may continue beyond the lash follicles,peeling the entire anterior lid margin from the tarsus in cases of metaplastic lashes and keratinization. In addition, the upper lid crease incision allows the surgeon to address the associated lid problems with no need for extra incision[11-12].
Other eyelid abnormalities often coexist with UCE including dermatochalasis, blepharoptosis, lid retraction, and brow ptosis[3,7-8,10-12]. These lid problems may necessitate additional surgical procedures. Advancing dermatochalasis mechanically may affect the position of the lashes resulting in worsening of the entropion[13-14]. With the ALR procedure alone, the redundancy of the upper eyelid skin and the underlying orbicularis muscle may be aggravated. Hence, excess skin and muscle removal through blepharoplasty has been recommended to prevent downward migration of the anterior lamella and provide a less bulky eyelid[8-9,11,13,17,19-20].
There were 18 eyelids with upper lid retraction which appeared to be due to the shortening of the posterior lamella and fornix. Other causes of upper eyelid retraction were excluded.Combining the procedure with lid retractors recession successfully prevented any postoperative lagophthalmos and achieved symmetric and good PFH. Other authors advised dissecting the upper lid retractors off the tarsus in UCE surgery to advance the posterior lamella inferiorly and compensate for the degree of the lid retraction[3,9,19,21]. Barr et al[16] assumed the high recurrence rate observed (21%) in their study following ALR was due to not performing concurrent levator recession.Blepharoptosis was found in 19 eyelids (19.6%) which appeared to be aponeurotic. Levator tucking was performed concomitantly with ALR in 19 eyelids to correct ptosis and improve lid margin eversion. A good PFH was achieved in all cases. The coexistent ptosis in UCE may be due to Müller muscle dysfunction secondary to structural changes of the tarsal conjunctiva in UCE, involutional changes, chronic eyelid rubbing, or long standing blepharospasm[22-24]. Combining ptosis correction with ALR will not only enhance the cosmetic appearance, but also maintain an upward vector of traction on the anterior lamella to aid in lid margin eversion[8].
The eyebrow skin and fat were found to descend over the upper lid in 30 eyelids for which an internal browpexy was combined with ALR. The blepharospasm from ocular irritation in long standing entropion is assumed to detach the frontoorbicularis fibers and displace the brow inferiorly[10]. Marked brow ptosis can impair lid dynamics leading to upper lid entropion and can aggravate existing conditions[25]. Nasr[10]commented that the surgical repair of the entropion does not usually reverse the brow ptosis and invariably these patients require suspension of the brow. In the Bi et al’s[8] study, 20 eyelids had brow ptosis, but in only 8 lids, brow surgery was undertaken simultaneously. However the technique of brow elevation was not stated in their study.
Anterior lamellar necrosis was the most frequent complication encountered in this study. Five eyelids had varying degrees of anterior lamellar necrosis ranging from epidermolysis to full thickness necrosis. All cases healed conservatively with consequent localized madarosis in two lids and a central notch in one eyelid. However, this did not alter the lid margin position or cause recurrent entropion. Although patients with anterior lamellar necrosis had multiple risk factors, scarifying both the marginal and the peripheral arcades during the combined procedure may be the cause[26].
The retrospective design, limited numbers, and lack of a comparison or control group are limitations to the current study. In addition, the vast majority of patients in this study had entropion secondary to trachoma. A prospective, randomized study comparing the method described in this manuscript to other conventional methods would be valuable.
In conclusion, simultaneous correction of associated lid problems may maximize the efficacy of ALR and enhance the postoperative cosmesis. We believe satisfactory functional and cosmetic correction of UCE can only be achieved by individualized surgical approach, which is tailored for every patient according to understanding the salient underlying pathophysiology, and determining the associated lid problems and post-surgical aesthetic desires.
ACKNOWLEDGEMENTS
We acknowledge Richard C. Allen, MD PhD FACS for critical discussions, editing, and review of the manuscript.
Conflicts of Interest: Gawdat TI, None; Kamal MA, None;Saif AS, None; Diab MM, None.
REFERENCES
1 Rajak SN, Collin RO, Burton MJ. Trachomatoustrichiasis and its management in endemic countries. Surv Ophthalmol 2012;57(2):105-135.
2 Kemp EG, Collin JR. Surgical management of upper lid entropion. Br J Ophthalmol 1986;70(8):575-579.
3 Ross AH, Cannon PS, Selva D, Malhotra R. Management of upper eyelid cicatricial entropion. Clin Exp Ophthalmol 2011;39(6):526-536.
4 Elder MJ, Collin R. Anterior lamellar repositioning and grey line split for upper lid entropion in ocular cicatricial pemphigoid. Eye (Lond)1996;10(1):439-442.
5 Hart WM. The eyelids. Hart WM, ed. Adler’s Physiology of The Eye;Clinical Application. 9th ed. US:Mosby Year Book Inc; 1992.
6 Guzey M, Ozardali I, Basar E, Aslan G, Satici A, Karadede S. A survey of trachoma: the histopathology and the mechanism of progressive cicatrization of eyelid tissues. Ophthalmologica 2000;214(4):277-284.
7 Sadiq MN, Pai A. Management of trachomatous cicatricial entropion of the upper eye eyelid: our modified technique. J Ayub Med Coll Abbottabad 2005;17(1):1-4.
8 Bi YL, Xu W, Rong A. Anterior lamellar repositioning with complete lid split: a modified method for treating upper eyelids trichiasis in Asian patients. J Plast ReconstrAesthet Surg 2009;62(11):1395-1402.
9 Aghai GH, Gordiz A, Falavarjani K, Kashkouli MB. Anterior lamellar recession, blepharoplasty, and supratarsal fixation for cicatricial upper eyelid entropion without lagophthalmos. Eye (Lond) 2016;30(4):627-631.10 Nasr AM. Eyelid complications in trachoma: diagnosis and management. Acta ophthalmol (Copenh) 1991;69(2):200-204.
11 Cruz AA, Akaishi PM, Al-Dufaileej M, Galindo-Ferreiro A. Upper lid crease approach for margin rotation in trachomatous cicatricial entropion without external sutures. Arq Bras Oftalmol 2015;78(6):367-370.
12 Cruz AA, Akaishi PM, Al-Dufaileej M, Galindo-Ferreiro A. The versatile lid crease approach to upper eyelid margin rotation. Middle East Afr J Ophthalmol 2015;22(4):407-409.
13 Sodhi PK, Yadava U, Pandey RM, Mehta DK. Modified grey line split with anterior lamellar repositioning for treatment of cicatricial lid entropion. Ophthalmic Surg Lasers 2002;33(2):169-174.
14 Rhatigan MC, Ashworth JL, Goodall K, Leatherbarrow B. Correction of blepharoconjunctivitis-related upper eyelid entropion using the anterior lamellar reposition technique. Eye (Lond) 1997;11(1):118-120.
15 Koreen IV, Taich A, Elner VM. Anterior lamellar recession with buccal mucous membrane grafting for cicatricial entropion. Ophthal Plast Reconstr Surg 2009;25(3):180-184.
16 Barr K, Essex RW, Liu S, Henderson T. Comparison of trichiasis recurrence after primary bilamellar tarsal rotation or anterior lamellar repositioning surgery performed for trachoma. Clin Exp Ophthalmol 2014;42(4):311-316.
17 Ahmed RA, Abdelbaky SH. Short term outcome of anterior lamellar reposition in treating trachomatous trichiasis. J Ophthalmol 2015;2015:568363.
18 Owji N, Tehrani J. Anterior lamellar recession in the management of the trachomatous cicatricial entropion of the upper eyelids: Outcomes and indications. Asian J Ophthalmol 2013;13(2):42-47.
19 Collin JRO. Manual of Systematic Eyelid Surgery. 3rd ed. Philadelphia:Elsevier Health sciences: 2006:29-56.
20 Dong L, Jianning L. Correction of recurrent entropion in Chinese patients. Eur J Plast Surg 2002;25(6):301-304.
21 Leatherbarrow B. Oculoplastic Surgery. 2nd ed. UK:Informa Healthcare; 2011;94-109.
22 Flowers RS. The art of eyelid and orbital aesthetics: multiracial surgical considerations. Clin Plast Surg 1987;14(4):703-721.
23 Fujiwara T, Matsuo K, Kondoh S, Yuzuriha S. Etiology and pathogenesis of aponeurotic blepharoptosis. Ann Plast Surg 2001;46(1):29-35.
24 Griffin RY, Sarc A, Unal M. Acquired ptosis secondary to vernal conjunctivitis in young adults. Ophthal Plast Reconstr Surg 2006;22(6):438-440.
25 Georgescu D, Anderson RL, McCann JD. Brow ptosis correction: a comparison of five techniques. Facial Plast Surg 2010;26(3):186-192.
26 Chi M, Kim HJ, Vagefi R, Kersten RC. Modified tarsotomy for the treatment of severe cicatricial entropion. Eye (Lond) 2016;30(7):992-997.