INTRODUCTION
In the last few decades, cataract surgery and intraocular lenses (IOLs) have developed considerably to offer patients the best visual outcomes and better quality of life with fewer adverse effects. During this period, numerous designs of multifocal IOLs have been developed including refractive,diffractive, refractive-diffractive and apodized-diffractive multifocal IOLs, with the aim to provide optimal visual function and spectacle independence at various distances.
Previous multifocal IOLs are known to generate a decrease in contrast sensitivity as well as disabling photic phenomena like halos and glare[1]. Manufacturers have sought to improve IOL designs to overcome these limitations while maximizing visual outcomes. Changes in angulation, addition of aspheric and apodized surfaces are among these improvements that have resulted in better contrast sensitivity and less visual disturbances[2].
The most important benefit of multifocal IOLs is the ability to restore near vision function in cataract patients. Studies have reported that patients’ quality of life can be significantly reduced owing to the loss of reading ability[3-5]. Some multifocal IOLs have added powers ranging from 3.5 to 4.5 diopters (D) to provide excellent near visual acuity on the usual reading distance of 0.3 m. However, with the rise in computer use, there has been increased emphasis on intermediate vision. To achieve spectacle independence when performing intermediate tasks, multifocal IOLs with lower addition powers have been developed. Studies have shown that these IOLs with lower addition can provide satisfactory visual acuity at both near and intermediate distances[6-7].
Optiflex MO/HF D012 (Moss Vision Inc. Ltd, London, UK) is a new generation multifocal IOL, which has a diffractive step design and an aspheric optic to minimize photic phenomena and to provide optimal visual outcomes without impairing contrast sensitivity. The addition power is low (+3.00) to achieve patient satisfaction in both intermediate and near tasks.This current single-center retrospective study assessed the clinical outcomes of this new multifocal IOL.
SUBJECTS AND METHODS
This study included patients who underwent cataract surgery with bilateral implantation of Optiflex MO/HF D012 (Moss Vision Inc. Ltd, London, UK) multifocal IOL by a single surgeon (Toygar B) between January 2014 and October 2015 at Bahcesehir University Department of Ophthalmology.Ethical Committee approval was obtained for the study. All data collection was done in accordance with the principles of Declaration of Helsinki, International council of Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use Guidelines, and Good Clinical Practices, and International Organization for Standardization 14155:2011.
Electronic medical records of patients bilaterally implanted with the study IOL were retrospectively reviewed and data from preoperative and postoperative assessments were collected and analyzed. All included patients were followed for 6mo at regular intervals (1wk; 1, 3 and 6mo).
Data collected from preoperative assessments included:uncorrected distance visual acuity (UDVA) and corrected distance visual acuity (CDVA) tested with ETDRS charts at 4 m, refractive status as manifest spherical equivalent (MSE;value of the sphere plus one-half of the value of the cylinder)and optical biometry measurements. Biometry was performed with IOL Master (Carl Zeiss). Manual immersion biometry(Nidek, Japan) was utilized in eyes in which IOL master could not be performed because of the presence of a dense cataract. The IOL power was calculated with SRK-T formula(A-constant: 118.5) in eyes with an axial length (AL) of 22 to 24 mm. The Hoffer Q formula (pACD=5.61) was used in eyes with a shorter AL (<22 mm), and Holladay 2 formula (ACD constant=5.607) was used in eyes with a longer AL (>24 mm).Data collected from postoperative assessments included:UDVA and CDVA with ETDRS chart at 4 m, uncorrected near visual acuity (UNVA) and distance corrected near visual acuity (CNVA) with the Jaeger chart at 40 cm, uncorrected intermediate visual acuity (UIVA) and distance corrected intermediate visual acuity (CIVA) with ETDRS chart at 80 cm (converted to Jaeger) and refractive status as MSE.High contrast (100%) and low contrast (10%) visual acuities measured with ETDRS chart at 100 cm with distance correction under 85 cd/m2 luminance were also recorded.In addition, adverse events, subjective patient symptoms(halos, glare), spectacle independence and visual function questionnaire (VFQ-25; scale from 1 to 100, with 100 being the best score) scores at the end of 6mo were noted. Exclusion criteria were history of diabetes, preexisting retinal disease or ocular pathology and previous ocular surgery. Patients with incomplete data were also excluded from the study.

Figure 1 Optiflex MO/HF-DO12 multifocal IOL.
Intraocular Lens The Optiflex MO/HF-DO12 multifocal IOL(Figure 1) is a single piece, diffractive-refractive, 360-degree square edge IOL with an aspheric optic. The lens has a 6.0 mm optic and an overall size of 12.5 mm and is made from hydrophobic acrylic material containing a natural yellow chromophore.The IOL is designed to be implanted in the capsular bag and is available in a diopter range from +10.00 D to +30.00 D in steps of 0.5 D with +3.00 D addition power. IOL uses apodization,diffraction, and refraction. The apodized diffractive region is within the central 3.75 mm optic zone of the IOL. This area comprises 9 concentric steps of gradually decreasing height,creating multifocality from distance to near (2 foci). The refractive part of the optic surrounds the apodized diffractive region. This area directs light to a distant focal point with larger pupil diameters and is dedicated to vision at distance.
Statistical Analysis Statistical analysis was performed using Statistica (Version 12, Dell Systems, USA). Initially,summary descriptive statistics were produced for all the key variables of the study, including the mean, variance, standard deviation and standard error, median, mode and inter-quartile range. A Box-Whisker plot was also produced using the latter range. The sample data for all variables were examined for normality using a probability plot and a formal test of statistical significance was carried out using the Schapiro-Wilk test. Based on the assumption of normality, a 95% confidence/fiducial limit was computed.
For normal data, means were compared within the group using ANOVA repeated-measures. For non-normal data, a logarithmic transformation was used to meet the requirements of ANOVA. If this transformation was not successful, a nonparametric test was used to compare the medians of the variables. The preferred test was the Friedmann test.
RESULTS
Forty eyes of 20 patients who underwent cataract surgery with bilateral implantation of the study IOL were included.The study population had an equal distribution of gender (10 females, 10 males). The average age of the study population was 66.7±8.5y (range 53-82).
Visual Acuity Visual acuity results of the study group are summarized in Table 1.
Table 1 Visual acuity results (n=40) at all distances up to 6mo
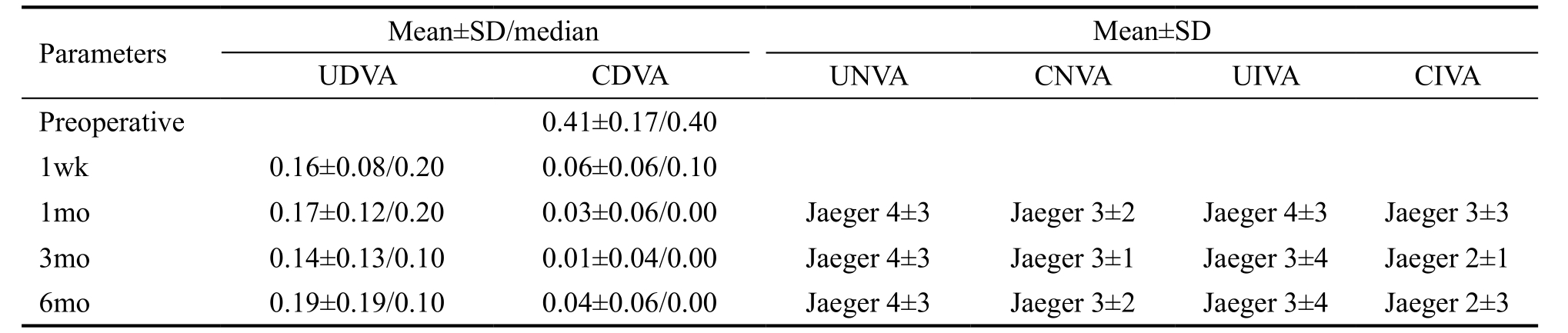
UDVA: Uncorrected distance visual acuity; CDVA: Corrected distance visual acuity; UNVA: Uncorrected near visual acuity; CNVA:Distance corrected near visual acuity; UIVA: Uncorrected intermediate visual acuity; CIVA: Distance corrected intermediate visual acuity.
Uncorrected Distance Visual Acuity UDVA remained stable through 6mo with no statistical difference through visits(P>0.05) (Figure 2A). At the 6-month visit, 59% of the patients had 20/25 or better UDVA.
Corrected Distance Visual Acuity Statistically significant improvement (P=0.0000) in preoperative CDVA was observed at every postoperative visit (Figure 2B). At the 6-month visit,mean CDVA was 0.04±0.06 logMAR (20/22 Snellen) and there was a significant improvement of 4 lines on average from the preoperative visit. At 6mo, 90% of the patients had 20/25 or better CDVA.
Uncorrected Near Visual Acuity and Distance Corrected Near Visual Acuity The mean UNVA at 6-month visit was J-4 with no significant differences through postoperative visits(P>0.05) (Figure 3A). Mean CNVA at 6mo was J-3 and it also remained stable with no statistically significant differences through follow up (Figure 3B).
Uncorrected Intermediate Visual Acuity and Distance Corrected Intermediate Visual Acuity Mean postoperative UIVA was J-3 and CIVA was J-2 at 6mo. No significant differences (P>0.05) were found in either UIVA (Figure 4A) or CIVA (Figure 4B) through postoperative visits.
Refraction There was significant reduction (P<0.05) in MSE in all postoperative visits when compared to the preoperative visit (Figure 5). At the end of 6mo mean MSE was -0.14±0.42.The mean target refraction was -0.004±0.10 (range: -0.28-0.16,median: 0.11). At 6mo, 92% of eyes were within 0.50 D of targeted refraction, 98% were within 1.00 D and all eyes were within 1.50 D.
Contrast Sensitivity Contrast sensitivity outcome is presented in Table 2. There was an improvement which did not reach significance (P=0.09) in high contrast (100%) visual acuity with an average improvement of 4 letters at 6mo visit compared to 1mo (Figure 6A). Low contrast (10%) visual acuity remained stable (P=0.54) through follow up with a mean of 0.35±0.17 logMAR at 6mo visit (Figure 6B).
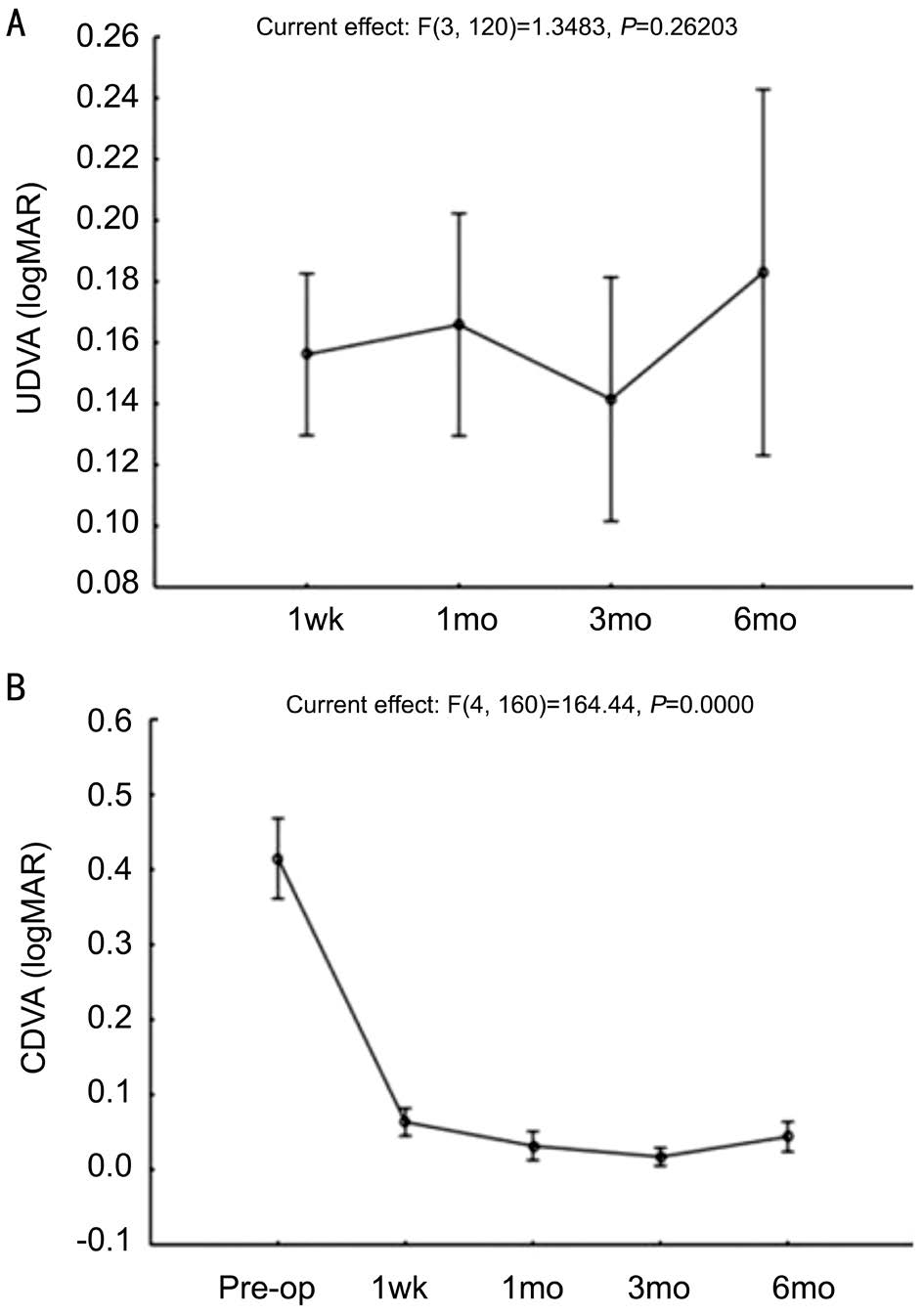
Figure 2 Distance visual acuity outcome of the study group A: Re-ANOVA graph for UDVA, within group analysis (n=40 eyes). B: Re-ANOVA graph for CDVA, within group analysis (n=40 eyes).
There were no reported adverse events during follow up. None of the patients reported halos or glare. The overall spectacle independence rate of the study population was 90% (18/20).None of the patients required spectacle correction for distance or intermediate vision. Two patients needed spectacles for near tasks. The overall patient satisfaction scores (VFQ-25) ranged between 76 and 100 (mean: 93.5±6.12, median: 93.15).
DISCUSSION
Optiflex MO/HF-DO12 IOL is one of the latest generation multifocal IOLs developed to restore distance, intermediate and near visual acuity and to address some of the clinically relevant limitations of previous multifocal IOLs such as disabling photic phenomena (halos, glare), poor intermediate vision and decrease in contrast sensitivity[8-12]. Contrast sensitivity tends to be impaired and glare disability is frequently cited with older versions of both diffractive and refractive multifocal IOLs[9-12].
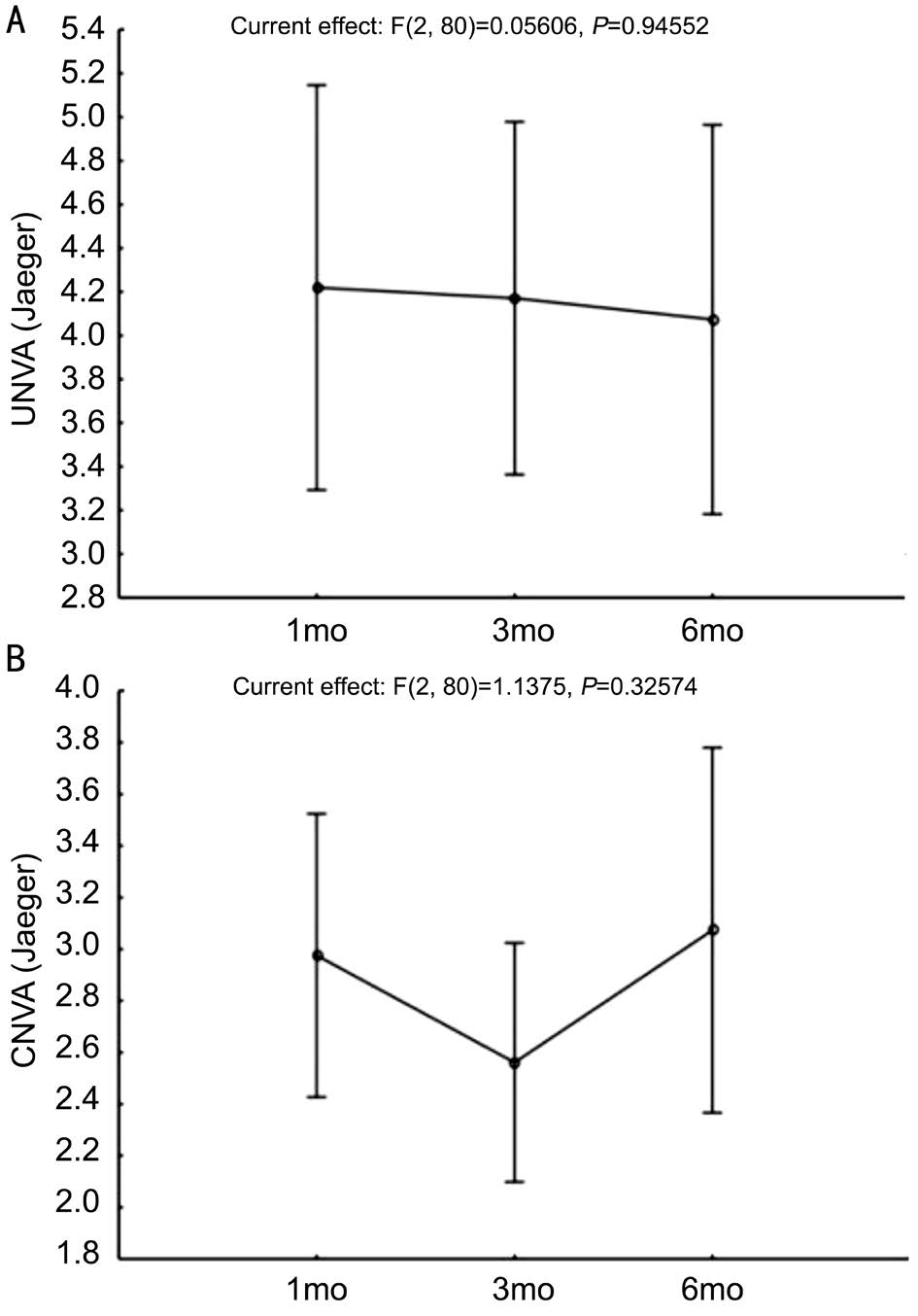
Figure 3 Near visual acuity outcome of the study group A: Re-ANOVA for UNVA, within group analysis n=40 eyes; B: Re-ANOVA for CNVA, within group analysis n=40 eyes.
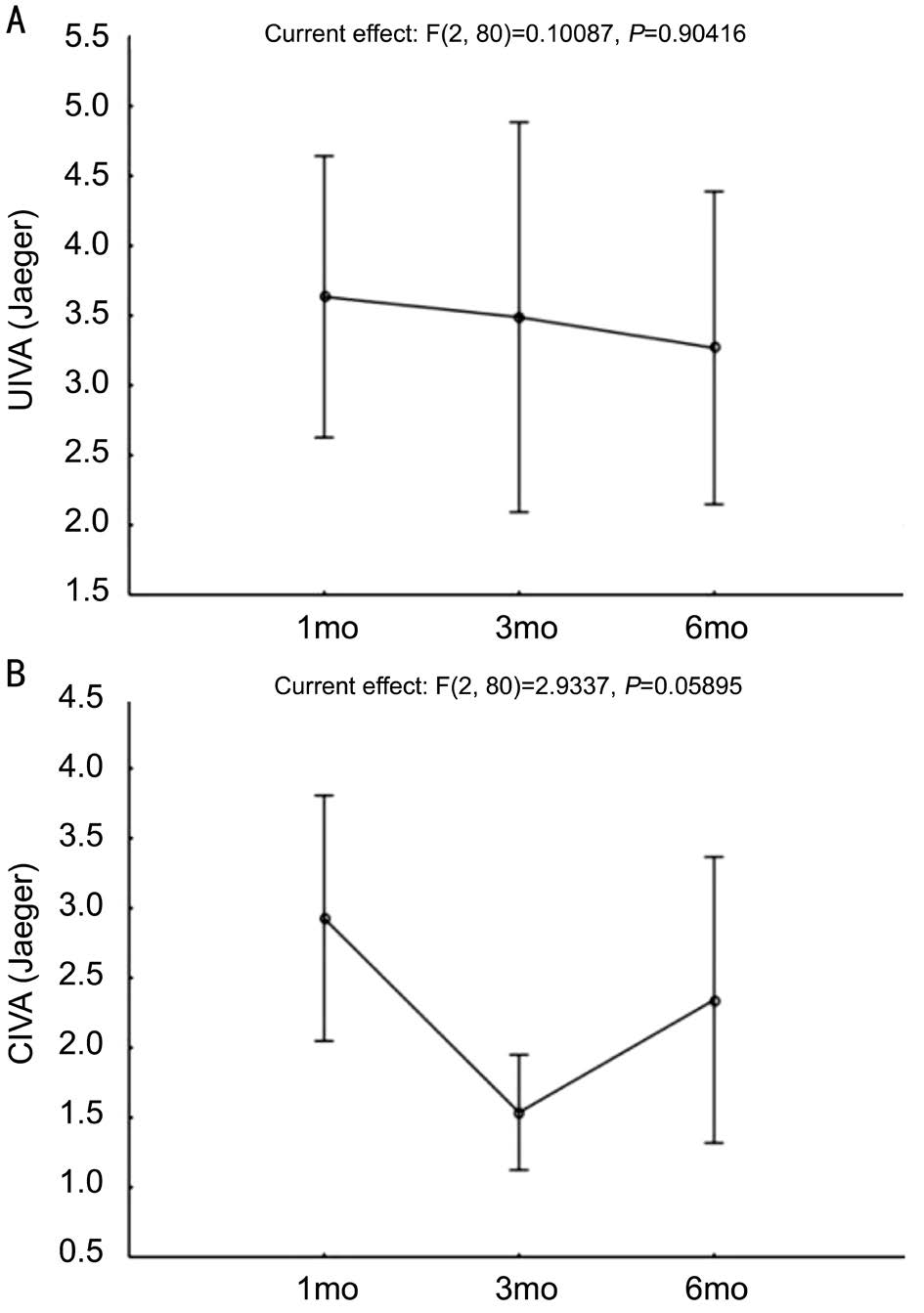
Figure 4 Intermediate visual acuity outcome of the study group A: Re-ANOVA for UIVA, within group analysis n=40 eyes; B: Re-ANOVA for CIVA, within group analysis n=40 eyes.
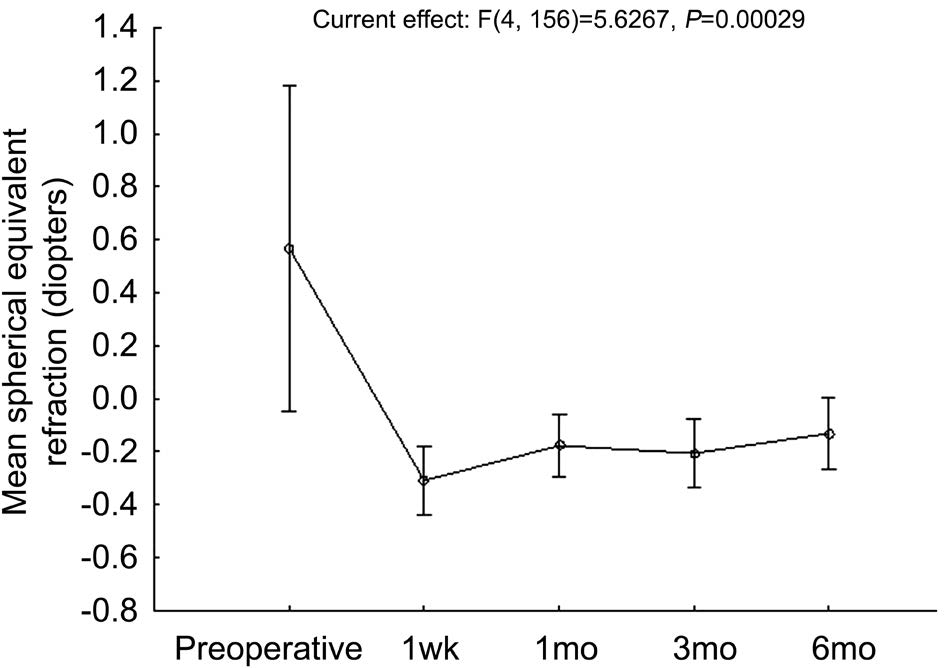
Figure 5 Re-ANOVA for mean spherical equivalent refraction,within group analysis n=40 eyes.
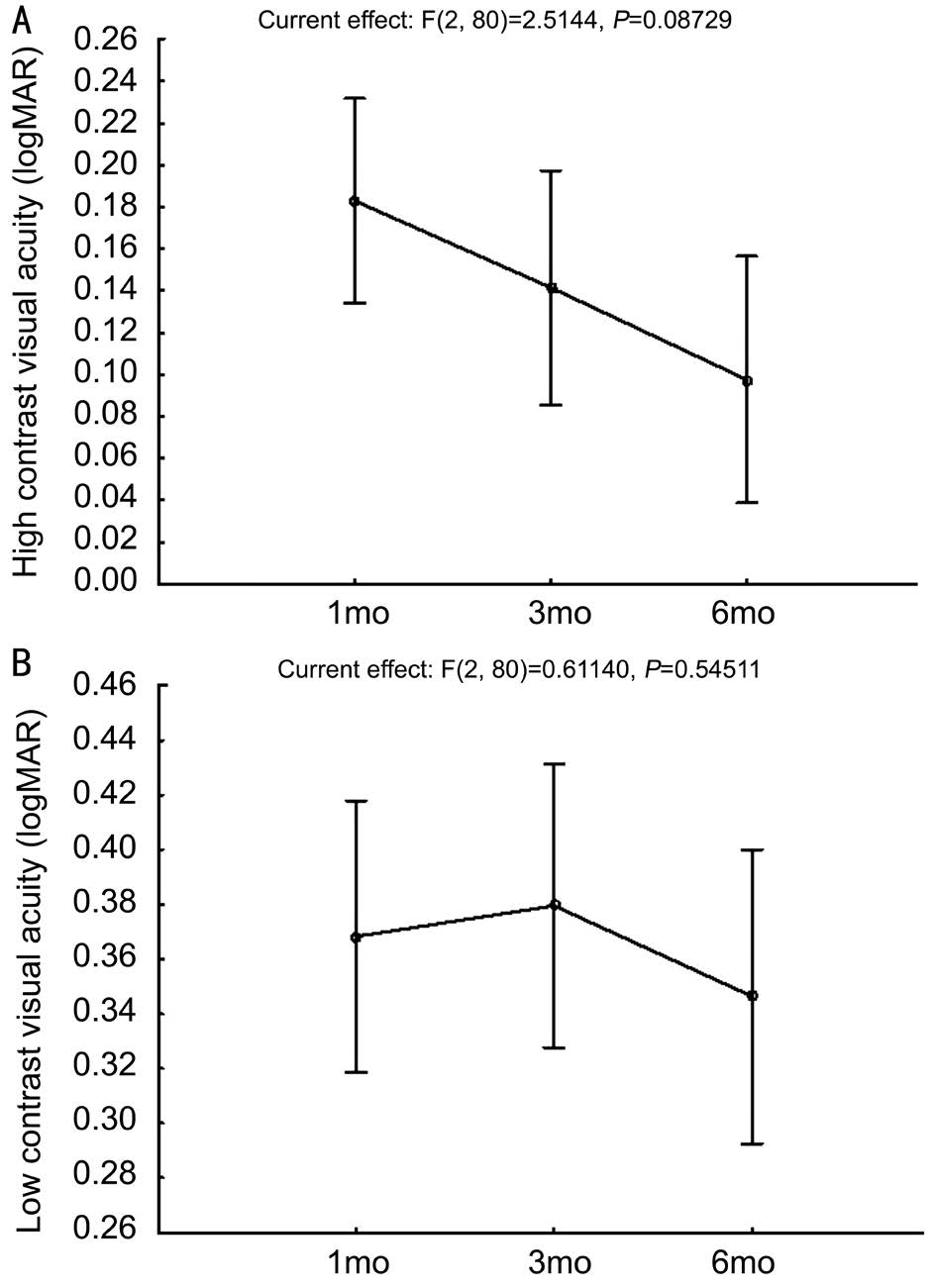
Figure 6 Contrast sensitivity outcome of the study group A: Re-ANOVA for postoperative high contrast (100%) visual acuity, within groups analysis n=40 eyes; B: Re-ANOVA for postoperative low contrast (10%) visual acuity, within groups analysis n=40 eyes.
Table 2 Postoperative contrast sensitivity results
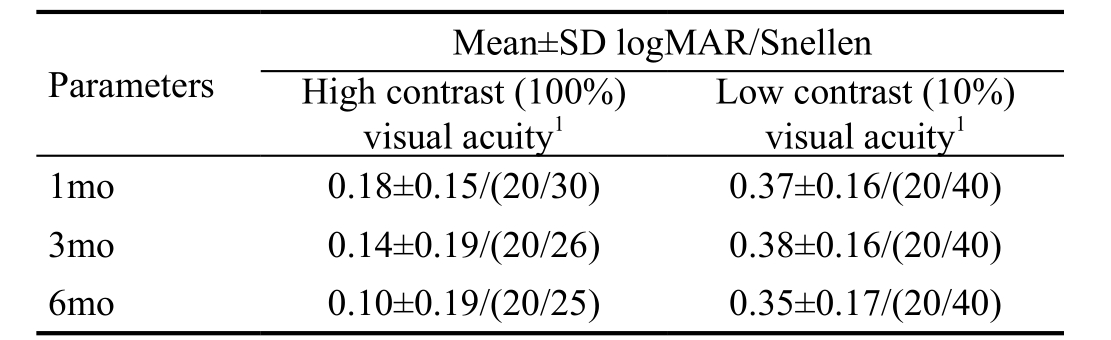
1With ETDRS chart at 100 cm, under 85 cd/m2 luminance.
In this retrospective study, Optiflex MO/HF-DO12 IOL demonstrated satisfactory visual and refractive outcomes at far, intermediate and near distances with high spectacle independence and no adverse effects. The mean UDVA was 0.19±0.19 (20/30) among the study group. This result was comparable to the mean monocular UDVA of 0.11±0.003 logMAR among 24 studies of 5570 eyes with cataract cited by Rosen et al[13] in a recent Meta-analysis of peer-reviewed studies involving implantation of a multifocal IOL. Gil et al[14] reported similar UDVA results at postoperative 3mo with 4 different multifocal IOLs: 0.04±0.08 with ReZoom NXG, 0.11±0.09 with ReSTOR +3.00, 0.14±0.11 with ReSTOR +4.00 and 0.12±0.08 with Tecnis ZMA00. In Rosen et al[13]’s Metaanalysis, the mean percentage of multifocal IOL-implanted eyes achieving a monocular UDVA of 0.30 logMAR (20/40) or better was 95.7%, based on 31 studies that reported this outcome for 3826 eyes. In our study 85% of the eyes achieved 20/40 or better UDVA at the end of 6mo after IOL implantation. Nevertheless,none of our patients required spectacles for distance vision.
Recently, the performance of intermediate distance tasks,such as computer work, has become increasingly important.Intermediate distances have often been considered a weakness for multifocal IOLs which create two or more focal points for distance and near. IOL manufacturers have sought to address this problem by introducing low-add multifocal IOLs which are designed to provide better intermediate vision without compromise in near or distance visual acuity. In a recent multicentre study with one of the latest low-add multifocal IOLs (Tecnis ZKB00), it was reported that the near add of+2.75 D still reached satisfying near results and led to high patient satisfaction for intermediate visual acuity[15]. Another study comparing the visual outcomes of a +3.00 D and a +4.00 D IOL found that the UIVA was significantly better in the +3.00 D IOL group than in the +4.00 D IOL group at 40, 50, 60 and 70 cm testing distances[16]. The Optiflex MO/HF-DO12 IOL has a +3.00 D add power at the IOL plane, equivalent to approximately 2.40 D at the spectacle plane, enabling the IOL to provide good visual acuity at intermediate distance which is suitable for using computers and electronic devices like tablets[4]. The mean UIVA at the end of 6mo was J-3 in our study, which was comparable to those results achieved with other multifocal IOLs with low addition power[17-18]. None of the patients in the current series needed spectacles for intermediate tasks.
While obtaining satisfactory distance and intermediate vision,near visual acuity was not compromised with a mean UNVA of J-4 at 6mo. Only two of our patients whose ages were 71 and 74y needed spectacles for reading. This result was comparable with other studies using multifocal IOLs with higher addition powers[19-21].
Refractive outcome was also good: at 6mo, 92% of the study eyes were within 0.50 D of target refraction and 98% were within 1.00 D. A significant reduction in preoperative MSE was observed with a mean MSE of 0.14±0.42 D at the end of follow up. These results were congruent with previous studies with different kinds of new generation multifocal IOLs[19-20,22].Although refractive outcome is satisfactory in most studies,corrective secondary procedures may be needed as reported in a study by Altaie et al[22] with Acrysof ReSTOR +4.00 addition, in which 4.4% of the subjects underwent subsequent LASIK correction to reduce residual refractive error.
In the current study, contrast sensitivity outcome was considered satisfactory, as low (10%) contrast visual acuity remained stable across the postoperative period with a mean of 0.35 logMAR at last visit. Li et al[23] assessed the contrast sensitivity outcome of an aspheric multifocal IOL (AcrySof ReSTOR SN6AD)with a similar method to the current study. They reported a mean low contrast (10%) visual acuity of 0.48 logMAR. Ang et al[24] reported monocular low contrast intermediate visual acuities of 0.36 and 0.39 logMAR with Restor +3.00 and Tecnis Multifocal respectively. Our finding was comparable to these previous studies with other new generation multifocal IOLs.
One of the most important benefits of multifocal IOLs for cataract patients is spectacle independence in their daily activities. In our study, none of our patients required spectacles for distance or intermediate vision. Overall spectacle independence rate of our study group was 90% which is in accordance with many studies with other diffractive or refractive multifocal IOLs reporting rates ranging between 76.9% and 100%[19-22,25-27]. In a recent study by Kim et al[4]reporting clinical outcomes of a diffractive multifocal IOL with varying powers of addition (+2.75, +3.25 and +4.00), the highest spectacle independence rate (87%) and overall patient satisfaction was achieved with the lowest addition (+2.75 D).This result may reflect an advantage of low addition which we have also observed in our series.
In our study group, none of the patients reported halo or glare symptoms. Several recent studies have shown that such visual disturbances are more severe with multifocal IOLs, and refractive models in particular[28-29]. Other studies have shown that halo and glare symptoms are reduced with diffractive multifocal IOLs compared to refractive multifocal IOLs[30-31].Additionally, these symptoms tend to be less frequent in patients with lower addition multifocal IOLs such as the study IOL, due to the use of fewer and wider concentric diffractive rings[4].
In their Meta-analysis, Rosen et al[13] reported overall patient satisfaction ratings ranging from 61.8% to 100%. They also stated that dissatisfaction was related to blurred vision or photic phenomena associated with residual ametropia,posterior capsular opacification, large pupil size and dry eye.In a multicentre study with a low-add (AcrySof IQ ReSTOR SN6AD1, +3.00 addition) IOL, patient satisfaction was assessed with a questionnaire consisting of questions on visual disturbances and lifestyle activities and a mean score of 8.3±1.6 (out of 10) was reported[32]. In our study, a comparable score of 93.5±6.12 (out of 100) was found with the VFQ-25 questionnaire at the 6-month postoperative visit, reflecting a high level of patient satisfaction.
The current study has several limitations. First, this study is retrospective and without a control group. Second, it is a small case series with a limited follow up. These factors dramatically limit the conclusions that can be drawn from our data. Despite this, the encouraging results suggest that better outcomes may be achieved with greater experience.
In conclusion, Optiflex MO/HF-DO12 IOL with low add power (+3.00 D) provided effective restoration of visual acuity at far, near and intermediate distances without compromising contrast sensitivity. High levels of spectacle independence and patient satisfaction were achieved. The IOL was shown to be safe and well tolerated by the ocular tissues as there were no reported adverse events or complications during the 6-month follow-up. Further long-term studies with a larger sample of patients should be performed to confirm the outcomes observed in this investigation with the Optiflex MO/HF-DO12 IOL.
ACKNOWLEDGEMENTS
Conflicts of Interest: Toygar B, None; Yabas Kiziloglu O,None; Toygar O, None; Hacimustafaoglu AM, None.
REFERENCES
1 Leyland M, Zinicola E. Multifocal versus monofocal intraocular lenses in cataract surgery: a systematic review. Ophthalmology 2003;110(9):1789-1798.
2 Chang DH. Visual acuity and patient satisfaction at varied distances and lighting conditions after implantation of an aspheric diffractive multifocal one-piece intraocular lens. Clin Ophthalmol 2016;10:1471-1477.
3 Elliott DB, Patla AE, Furniss M, Adkin A. Improvements in clinical and functional vision and quality of life after second eye cataract surgery.Optom Vis Sci 2000;77(1):13-24.
4 Kim JS, Jung JW, Lee JM, Seo KY, Kim EK, Kim TI. Clinical outcomes following implantation of diffractive multifocal intraocular lenses with varying add powers. Am J Ophthalmol 2015;160(4):702-709.
5 Moshegov CN, Skaf S. Visual outcomes after implantation of a low-add(+3.25 D) diffractive multifocal intraocular lens. Clin Exp Ophthalmol 2015;43(9):839-841.
6 Hayashi K, Ogawa S, Manabe S, Hirata A. Visual outcomes in eyes with a distance-dominant diffractive multifocal intraocular lens with low near addition power. Br J Ophthalmol 2015;99(11):1466-1470.
7 Tan N, Zheng D, Ye J. Comparison of visual performance after implantation of 3 types of intraocular lenses: accommodative, multifocal,and monofocal. Eur J Ophthalmol 2014;24(5):693-698.
8 Alfonso JF, Fernandez-Vega L, Baamonde MB, Montes-Mico R.Prospective visual evaluation of apodized diffractive intraocular lenses. J Cataract Refract Surg 2007;33(7):1235-1243.
9 Steinert RF, Aker BL, Trentacost DJ, Smith PJ, Tarantino N. A prospective comparative study of the AMO ARRAY zonal-progressive multifocal silicone intraocular lens and a monofocal intraocular lens.Ophthalmology 1999;106(7):1243-1255.
10 Javitt JC, Steinert RF. Cataract extraction with multifocal intraocular lens implantation: a multinational clinical trial evaluating clinical, functional,and quality-of-life outcomes. Ophthalmology 2000;107(11):2040-2048.
11 Pieh S, Weghaupt H, Skorpik C. Contrast sensitivity and glare disability with diffractive and refractive multifocal intraocular lenses. J Cataract Refract Surg 1998;24(5):659-662.
12 Hayashi K, Hayashi H, Nakao F, Hayashi F. Influence of astigmatism on multifocal and monofocal intraocular lenses. Am J Ophthalmol 2000;130(4):477-482.
13 Rosen E, Alio JL, Dick HB, Dell S, Slade S. Efficacy and safety of multifocal intraocular lenses following cataract and refractive lens exchange: meta analysis of peer-reviewed publications. J Cataract Refract Surg 2016;42(2):310-328.
14 Gil MA, Varon C, Rosello N, Cardona G, Buil JA. Visual acuity,contrast sensitivity, subjective quality of vision, and quality of life with 4 different multifocal IOLs. Eur J Ophthalmol 2012;22(2):175-187.
15 Kretz FT, Gerl M, Gerl R, Müller M, Auffarth GU; ZKB00 Study Group. Clinical evaluation of a new pupil independent diffractive multifocal intraocular lens with a +2.75D near addition: a European multicentre study. Br J Ophthalmol 2015;99(12):1655-1659.
16 de Vries NE, Webers CA, Montes-Mico R, Ferrer-Blasco T, Nuijts RM.Visual outcomes after cataract surgery with implantation of a + 3.00 D or + 4.00 D aspheric diffractive multifocal intraocular lens: comparative study. J Cataract Refract Surg 2010;36(8):1316-1322.
17 Pedrotti E, Mastropasqua R, Passilongo M, Parisi G, Marchesoni I,Marchini G. Comparison of two multifocal intraocular lens designs that differ only in near add. J Refract Surg 2014;30(11):754-760.
18 Alfonso JF, Fernández-Vega L, Puchades C, Montés-Micó R.Intermediate visual function with different multifocal intraocular lens models. J Cataract Refract Surg 2010;36(5):733-739.
19 Dexl AK, Zaluski S, Rasp M, Grabner G. Visual performance after bilateral implantation of a new diffractive aspheric multifocal intraocular lens with a 3.5 D addition. Eur J Ophthalmol 2013;24(1):35-43.
20 Lubinski W, Gronkowska-Serafin J, Podboraczynska-Jodko K. Clinical outcomes after cataract surgery with implantation of the Tecnis ZMB00 multifocal intraocular lens. Med Sci Monit 2014;20:1220-1226.
21 Schmickler S, Bautista CP, Goes F, Shah S, Wolffsohn JS. Clinical evaluation of a multifocal aspheric diffractive intraocular lens. Br J Ophthalmol 2013;97(12):1560-1564.
22 Altaie R, Ring CP, Morarji J, Patel DV, McGhee CN. Prospective analysis of visual outcomes using apodized, diffractive multifocal intraocular lenses following phacoemulsification for cataract or clear lens extraction. Clin Exp Ophthalmol 2012;40(2):148-154.
23 Li JH, Feng YF, Zhao YE, Zhao YY, Lin L. Contrast visual acuity after multifocal intraocular lens implantation: aspheric versus spherical design.Int J Ophthalmol 2014;7(1):100-103.
24 Ang R, Martinez G, Cruz E, Tiongson A, Dela Cruz A. Prospective evaluation of visual outcomes with three presbyopia-correcting intraocular lenses following cataract surgery. Clin Ophthalmol 2013;7:1811-1823.
25 Akaishi L, Vaz R, Vilella G, Garcez RC, Tzelikis PF. Visual performance of Tecnis ZM900 diffractive multifocal IOL after 2500 implants: a 3-year follow up. J Ophthalmol 2010;2010.
26 Packer M, Chu YR, Waltz KL, Donnenfeld ED, Wallace RB 3rd,Featherstone K, Smith P, Bentow SS, Tarantino N. Evaluation of the aspheric tecnis multifocal intraocular lens: one-year results from the first cohort of the food and drug administration clinical trial. Am J Ophthalmol 2010;149(4):577-584.e1.
27 Guo X, Sun Y, Zhang B, Zheng D. Medium-term visual outcomes of apodized diffractive multifocal intraocular lens with +3.00 D addition power. J Ophthalmol 2014;2014:247829.
28 Dick HB, Krummenauer F, Schwenn O, Krist R, Pfeiffer N. Objective and subjective evaluation of photic phenomena after monofocal and multifocal intraocular lens implantation. Ophthalmology 1999;106(10):1878-1886.
29 Leyland MD, Langan L, Goolfee F, Lee N, Bloom PA.Prospective randomised double-masked trial of bilateral multifocal,bifocal or monofocal intraocular lenses. Eye (Lond) 2002;16(4):481-490.
30 Renieri G, Kurz S, Schneider A, Eisenmann D. ReSTOR diffractive versus Array 2 zonal-progressive multifocal intraocular lens: a contralateral comparison. Eur J Ophthalmol 2007;17(5):720-728.
31 Cillino S, Casuccio A, Di Pace F, Morreale R, Pillitteri F, Cillino G,Lodato G. One-year outcomes with new-generation multifocal intraocular lenses. Ophthalmology 2008;115(9):1508-1516.
32 Kohnen T, Nuijts R, Levy P, Haefliger E, Alfonso JF. Visual function after bilateral implantation of apodized diffractive aspheric multifocal intraocular lenses with a +3.0 D addition. J Cataract Refract Surg 2009;35(12):2062-2069.