INTRODUCTION
Persistent fetal vasculature (PFV) has been described as an sporadic and congenital syndrome of cataract and progressive retinal detachment in a microphthalmic eye with eventual phthisis if left untreated[1]. Cases can further be segregated on the basis of location and classified as anterior, posterior and combined types[2]. The heterogeneity of clinical presentations of PFV makes it challenging to manage surgically, however, it is possible to eliminate amblyogenic media opacities and relieve tractional forces using a closedsystem intraocular approach[3-6]. More recent studies reported improved visual and anatomical outcomes, probably the result of earlier diagnosis, more careful case selection for surgery,improved surgical techniques, and aggressive postoperative amblyopia therapy[7-8].
Small gauge vitrectomy, a transconjunctival sutureless vitrectomy,was introduced in recent years[9-10], with its advantages including faster healing, increased patient comfort, and faster visual recovery[11-13]. In this retrospective study, we reported the surgical procedures and clinical outcomes of 105 cases of PFV treated with small gauge pars plicata vitrectomy.
SUBJECTS AND METHODS
Records of 105 patients with PFV treated by small gauge pars plicata vitrectomy between January 2010 and January 2013 at the Beijing Tongren Eye Centre were retrospectively reviewed.The study protocol was reviewed and approved by the Ethnic Committee of Beijing Tongren Hospital.
Anterior PFV was defined as fibrovascular membrane around the lens or attached to the posterior capsule involving the pupillary zone (Figure 1A), presence of retrolental vitreous membrane and stalk reaching the optic nerve without retinal traction or detachment. Posterior PFV was characterized by the presence of retrolental vitreous membrane and stalk reaching the optic nerve with retinal traction or detachment (Figure 1B).Cases in which there was posterior lens capsule opacification or fibrovascular membrane without pupillary zone involvement were also defined as posterior type. Combined type of PFV included both anterior and posterior PFV features.
Patients were all operated on by a single surgeon (Lu H).Three surgical approaches were applied to these patients:1) vitrectomy (23 or 25 gauge) through the pars plicata for posterior PFV; 2) lensectomy and vitrectomy (L+V) through pars plicata for anterior PFV of younger than 2 years old and for combined PFV with severe pathological changes of the macular, peripheral anterior lens capsule were kept intact with central anterior capsulotomy using vitrectomy probe in most eyes (Figure 2A, 2B); 3) vitrectomy through pars plicata combined with aspiration of lens cortex, intraocular lens (IOL)implantation through clear cornea incision (LA+V+IOL) and central posterior capsulotomy for eyes with anterior PFV in cases of older than 2y or combined PFV without severe pathological changes of the macular. The scleral incisions were sutured in eyes of scleral leakage (bubbles visible at the site of scleral incision after removal of trocar). Adjunctive surgical procedures included electric coagulation of the primary hyaloidal vasculature (21 eyes) and partial air-fluid exchange(87 eyes).
Cases were reviewed for demographic and ophthalmic data,including age at surgery, gender, laterality, chief complaints,PFV type, associated eye abnormalities, visual acuity (VA),intraocular pressure, surgical procedures performed, findings during the examinations, complications, and length of followup. Ancillary studies included A and/or B-scan or color doppler ultrasonography and Retcam fundus photography (Clarity Medical Systems, Pleasanton, California, USA).
VA records included perception of light, fixation, and follow ability of light, presence of nystagmus, and determination of VA using the Teller card, E-chart, or Snellen acuity cards depending on the age and cooperation of the child.Postoperative VA were compared with preoperative values and classified as stable, improve, or deteriorate. When documentable VA data were not available, visual improvement was arbitrarily defined as a change in vision from an inability to an ability to fixate on light and unsteady/eccentric fixation to central/steady fixation. To achieve standardization,documented VA was converted to logarithm of the minimum angle of resolution (logMAR) values.
Pediatric ophthalmologists and optometrists would be involved if indicated for deprivational, anisometropic, and refractive amblyopia with cycloplegic correction, spectacles and aphakic contact lens fitting, or occlusion therapy. Amblyopia therapy consisted of patching the better eye for several waking hours every day depending on the age with placement of contact lens or spectacles on the involved eye. The lens power was checked every 3 to 6mo and replaced if necessary.
Statistical Analysis Statistical analysis was performed using SPSS version 17.0 (SPSS Inc., Chicago, IL, USA). Testing of normality was performed by the Kolmogorow-Smirnow method. Dichotomous variables were compared using Chisquare test.
RESULTS
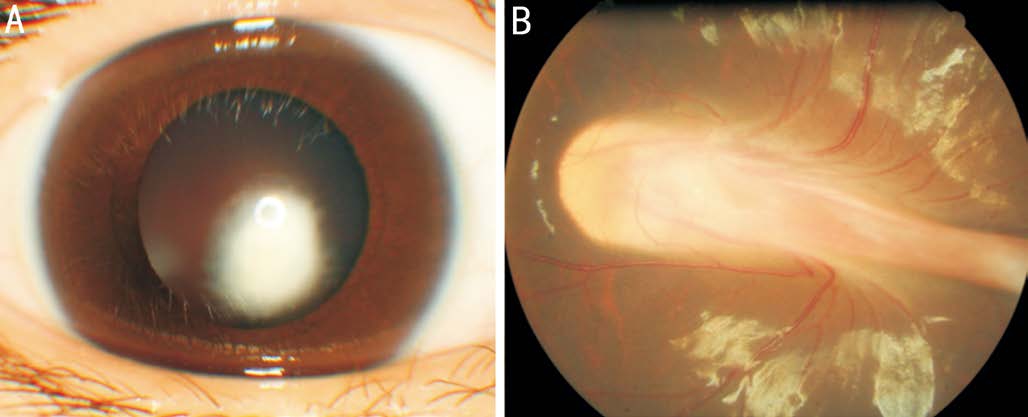
Figure 1 Anterior segment and/or fundus of PFV patients A:Patient with anterior PFV presented with fibrovascular membrane attached to the posterior capsule involving the pupillary zone; B:Posterior PFV presented with membranous vitreous stalk reaching the optic nerve with tractional retinal detachment.
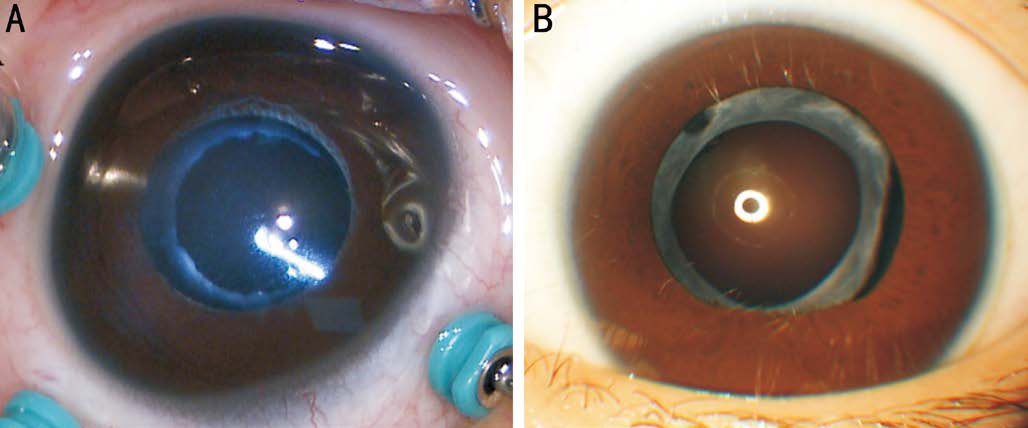
Figure 2 Preservation of anterior capsule and central anterior capsulotomy for patients underwent small gauge pars plicata vitrectomy combined with lensectomy A: Central anterior capsulotomy using 25 gauge vitrector; B: Opacified anterior capsule with clear optical media of the pupillary zone 3mo postoperatively.
A total of 118 eyes of 105 patients were identified with PFV and underwent vitrectomy during the study period, with a median follow-up of 17mo. Thirteen patients (12.4%) were bilateral. The median age at surgery was 22mo (range, 2mo-20y), with 59.0% (62/105) of the patients aged less than 2y, one female patients aged 20y complained with blurred vision because of vitreous hemorrhage caused by PFV. No systemic abnormalities were present in any of the patients.Associated eye abnormalities included microphthalmia (10 eyes), morning-glory syndrome (1 eye), macular hypoplasia and schisis (4 eyes), pupillary membrane (2 eyes), vitreous hemorrhage (2 eyes), and retinal detachment (65 eyes).Baseline characteristics of patients are summarized in Table 1.Surgical information of eyes with PFV is listed in Table 2. We performed L+V in 71.2% (84/118) of the eyes. Two eyes with anterior PFV and one eye with combined PFV received lenssparing vitrectomy because of the eccentric pupillary zone opacification of the posterior lens capsule. Four eyes with combined PFV underwent LA+V+IOL for minor tractional retinal detachment around the optic nerve with comparatively normal macula.
We performed 23 gauge vitrectomy in the earlier period since we had no 25 gauge vitrectomy system then, and we found that the percentage of sutured scleral incision of 23 gauge vitrectomy (71.7%, 33/46) was higher than that of the 25 gauge vitrectomy.
Peripheral anterior lens capsule were kept intact with central curvilinear capsulotomy using the vitrectomy probe in 59 of84 eyes (70.2%) underwent L+V. Sixteen eyes received central curvilinear posterior capsulotomy after implantation of IOL.No eye with capsular tearing or IOL dislocation was found during the study period.
Table 1 Baseline characteristics of patients with PFV
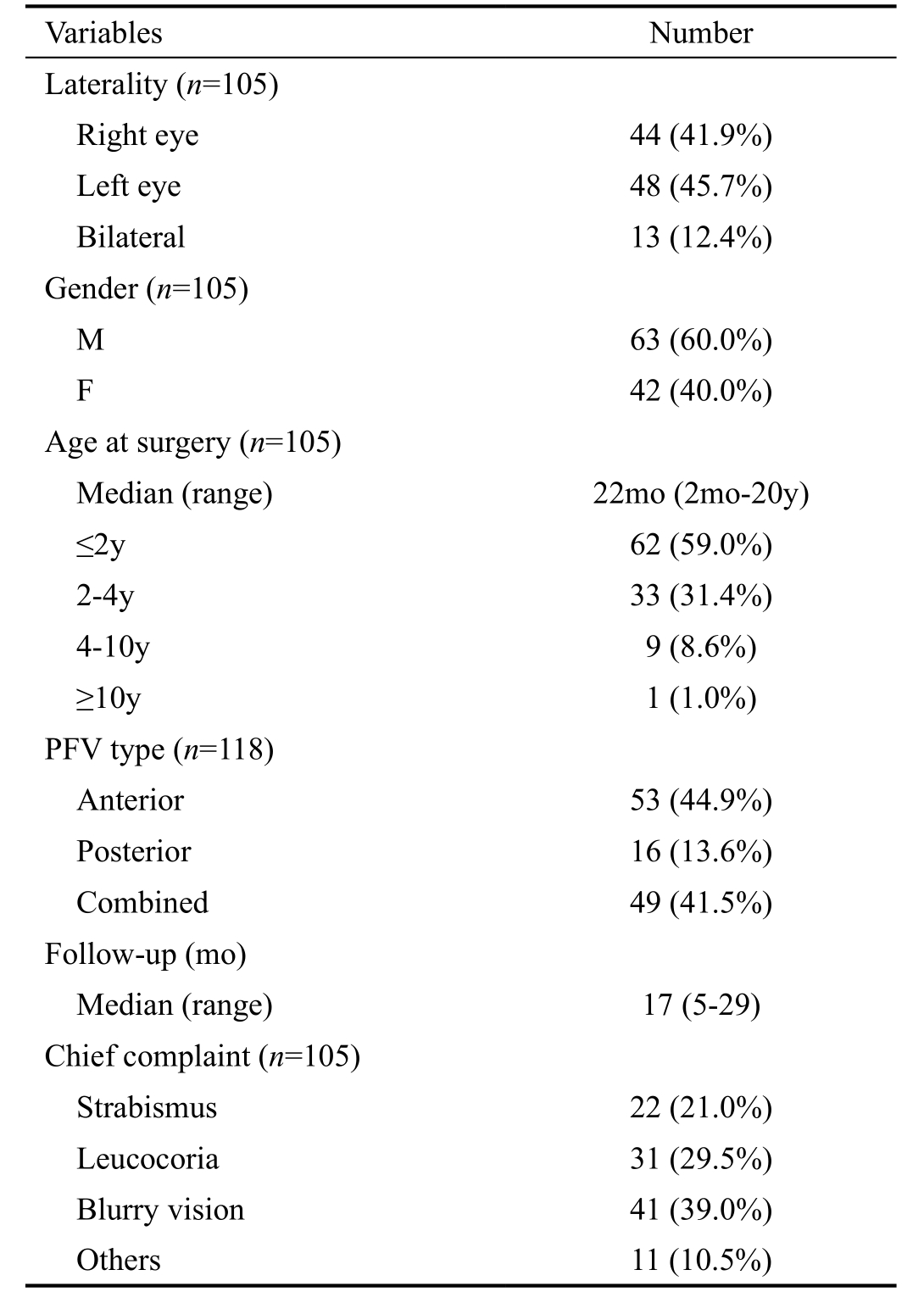
Table 2 Surgical information of eyes with PFV
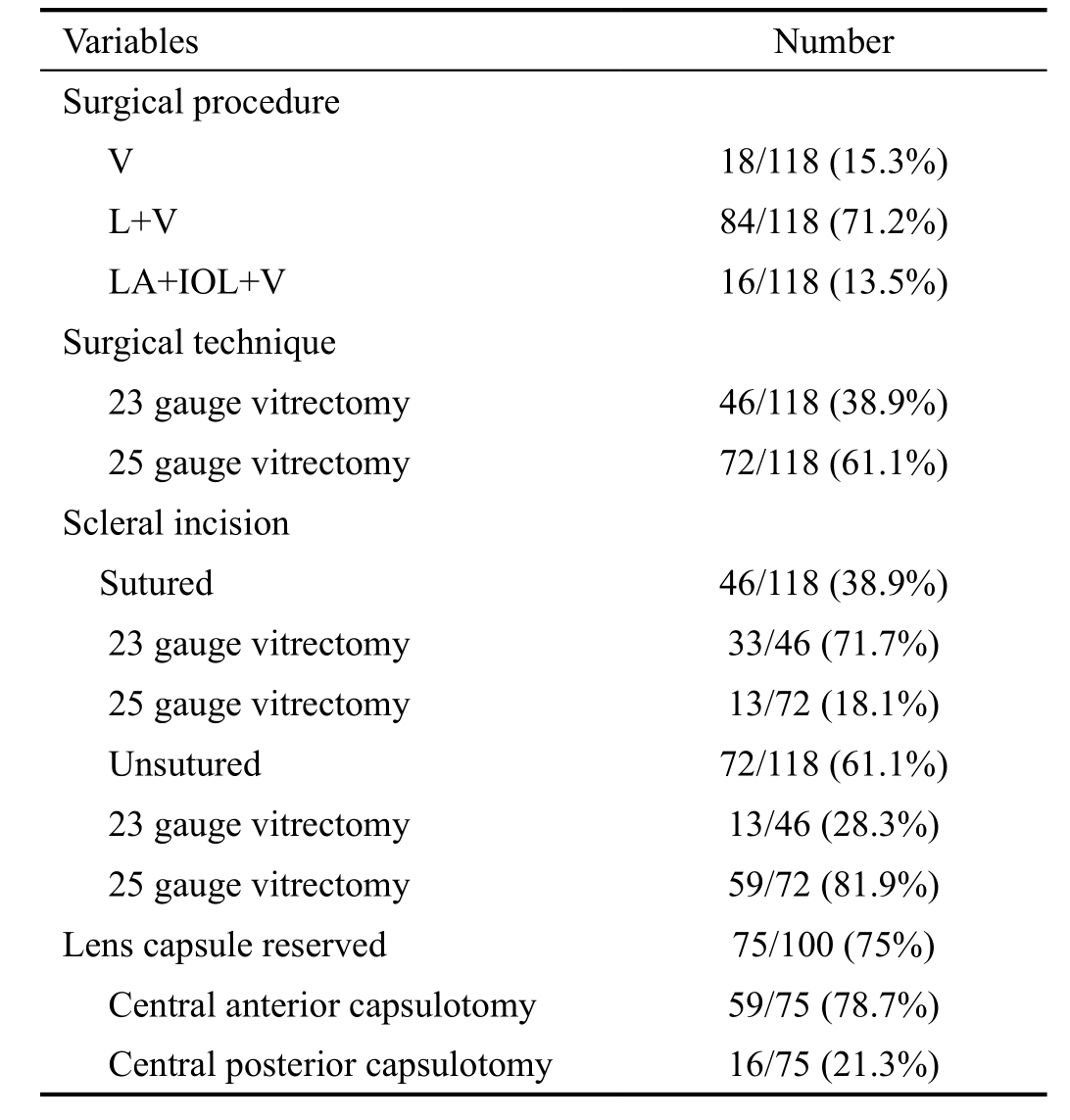
Table 3 Visual outcomes of eyes with PFV
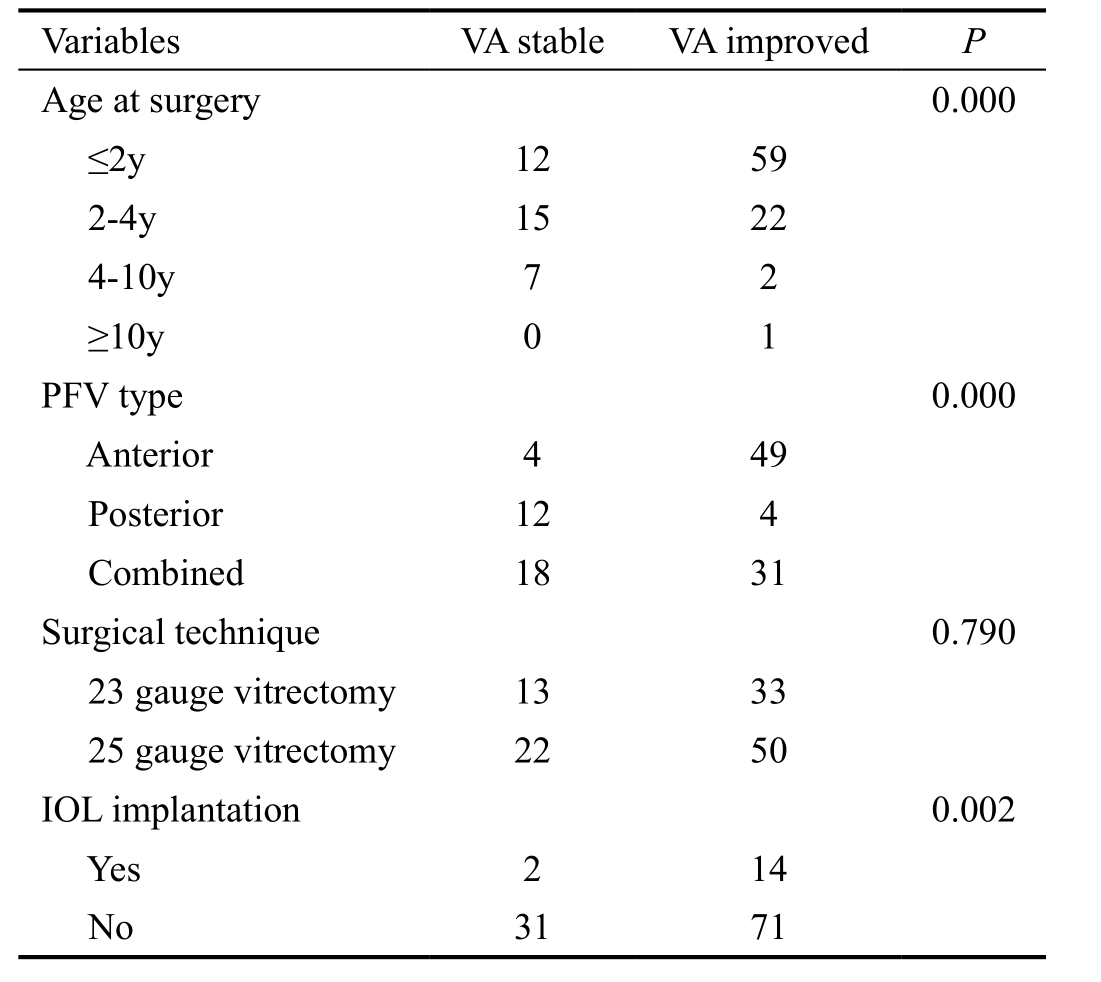
Only 10 eyes (8.5%) of 10 patients (aged≥4y) have preoperative objective records of corrected VA ranged from hand move to 0.7 logMAR, VA of 54 eyes (45.8%) were recorded as having no fix-and-follow, 25 eyes (21.2%) could follow light,17 (14.4%) had central unsteady fixation, and 12 (10.2%)had central steady fixation on a light source. At last followup, VA remained stable in 34 eyes (28.8%) and improved in 84 eyes (71.2%), age at surgery (less than 2y), anterior type of PFV, and immediate IOL implantation were associated with postoperative improved VA (P=0.000, 0.000, 0.002,respectively; Table 3).
During the last follow-up visit, best corrected VA was able to be assessed in 57 (48.3%) eyes (32 with anterior PFV, 8 with posterior PFV and 17 with combined PFV). VA was better than 0.5 logMAR in 15.8% (9/57) eyes, 1.3-0.5 logMAR in 35.1%(20/57) eyes, and worse than 1.3 logMAR in 49.1% (28/57)eyes. One eye with combined PFV and 2 eyes with posterior PFV had VA records better than 0.5 logMAR at last visit.
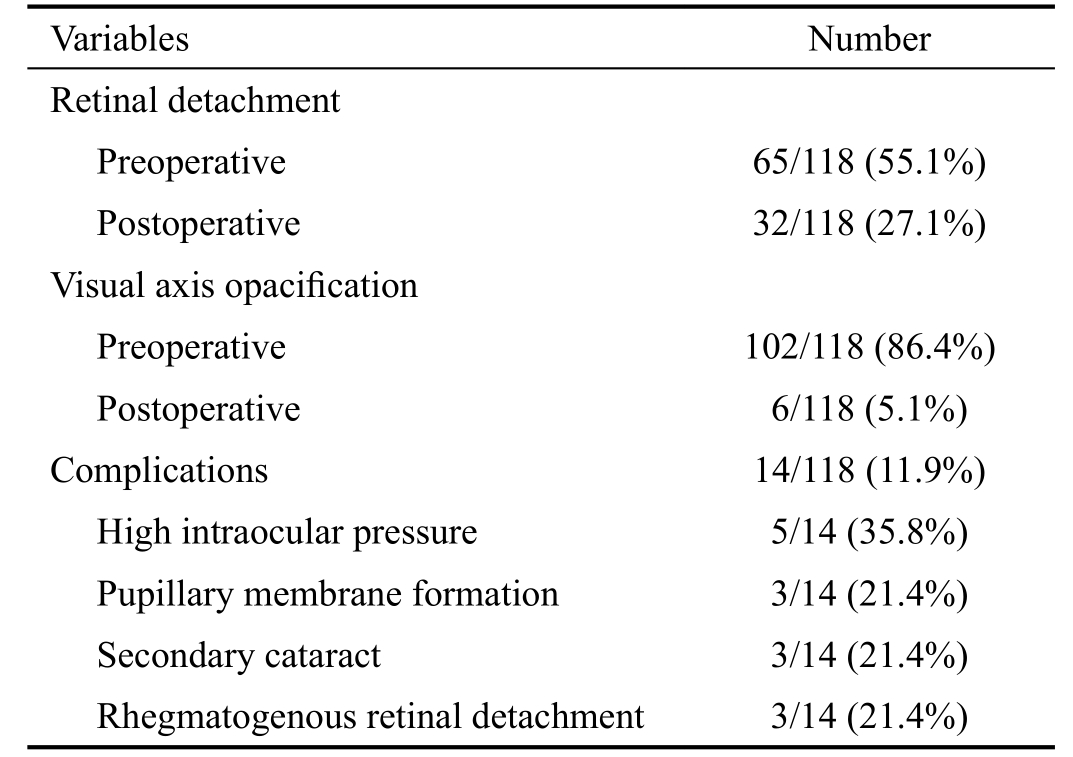
Sixty-five eyes (55.1%) had retinal detachment preoperatively(Figure 3A, 3C), among which 33 eyes (50.8%) had retinal reattachment (Figure 3B) or partial retinal reattachment after surgery (Figure 3D), and 17 eyes (26.2%) had macular reattachment at last visit, 94.1% eyes (96/102) regained clear visual axis after surgical repair. Postoperative anatomy and complications are listed in Table 4. Temporary higher intraocular pressure were controlled after medical treatment;pupillary membrane formation and secondary cataract required additional surgery and clear visual axis were achieved at last visit; rhegmatogenous retinal detachment requiring silicon oil tamponade had retinal attachment at last visit. No eyes developed endophthalmitis or required enucleation.
DISCUSSION
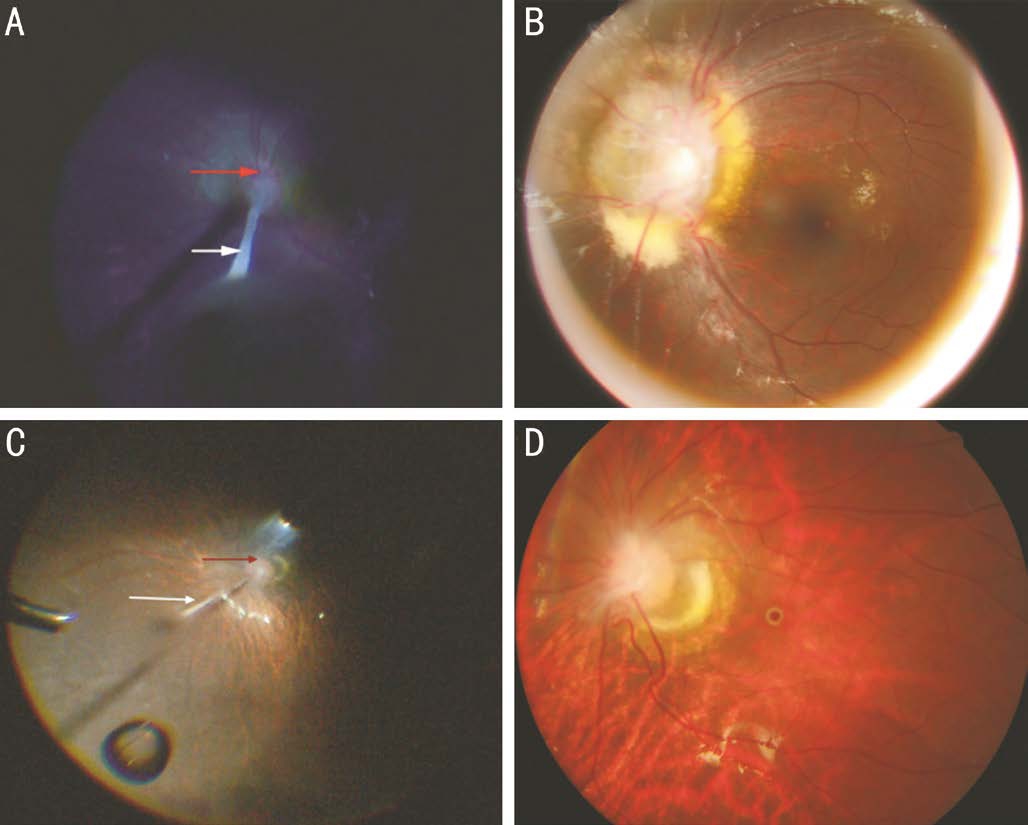
Figure 3 Fundus photographs of patients preoperatively and 6mo postoperatively A: Two-year-old girl with anterior PFV presented with membranous vitreous stalk (white arrow) starting from the optic nerve with local tractional retinal detachment (red arrow) without macular involvement; B: Retinal reattachment and normal foveal reflex 6mo postoperatively; C: Seven-year-old girl with posterior PFV presented with membranous vitreous stalk starting from the optic nerve (white arrow), tractional retinal detachment (red arrow)involving the macular; D: Relieved retinal and macular detachment 6mo postoperatively.
Table 4 Postoperative anatomy and complications of eyes with PFV
Over the years, the goal of early surgery recommended for PFV has been shifted from preventing future glaucoma and hemorrhagic complications to achieving a comparatively better visual prognosis as knowledge of the disease and surgical instrumentation have advanced. Several reports have discussed the advantages and safety of small gauge vitrectomy in patients with proliferative diabetic retinopathy, retinal detachment and retinopathy of prematurity, but very few patients with PFV were included in these reports. Our focus in the current study was to determine the surgical management and short-term postoperative outcomes in eyes with PFV using small gauge pars plicata vitrectomy .
A total of 118 eyes of 105 patients were identified with PFV and undergone small gauge pars plicata vitrectomy during the study period, which 12.4% of the patients were bilateral, but the percentage found in this study cannot be generalized given the selection bias resulting from the referral setting.
Small gauge vitrectomy is advantageous due to its less surgical trauma, faster healing, increased patient comfort and perhaps faster visual recovery[14-16], and it obviates the need for suturing of the scleral incisions, but postoperative hypotony is a common safety problem, especially for children. Lam et al[17]reported that 40% of the eyes which undergone small gauge vitrectomy but without suturing of the scleral incisions had an intraocular pressure less than 5 mm Hg on postoperative day 1. Postoperative hypotony may be of a concern in children, as they are more likely to rub their eyes after surgery,additionally, in children with vasoproliferative disorders,hypotony in the immediate postoperative period may result in an increased risk of bleeding. In our series, all the patients had PFV that might be associated with active neovascular tissue and the sclerotomies were sutured for 38.9% eyes to prevent postoperative intraocular hemorrhage induced by postoperative hypotony, of which 71.7% eyes undergone 23 gauge vitrectomy had suturing of the scleral incision compared to 18.1% eyes undergone 25 gauge vitrectomy, but further study is needed to compare the exact percentage of leakage of scleral incisions for 23 or 25 gauge vitrectomy referring patient age, PFV type or surgical time. Although it takes more time to dissect the conjunctiva and/or suture at the close of the case,we believe that these modifications improve the safety of small gauge vitrectomy in these patients. Indeed, in our series, there was no hypotony observed after surgery
There has been consensus about the surgical modality for patients with PFV, lens-sparing vitrectomy for predominately posterior PFV without axial lens opacification, and vitrectomy combined with lens surgery for anterior or combined PFV[18].However, there has been some disagreement among authors over the preferred location of incisions for lens surgery in PFV. Authors who favor a limbal approach argue that the peripheral retina and the ciliary body can be dragged anteriorly and/or centrally, and pars plicata approach could make iatrogenic injury to these structures more likely[19-20]. Other authors advocate a pars plicata approach for less disturbance of the cornea and anterior chamber angle, improved ability to remove all of the lens cortex, and reduced anterior traction on posterior retina intraoperatively by earlier transection of the persistent hyaloid[21-24]. A study showed that the choice of limbal versus pars plicata incisions produced similar safety and visual outcomes when careful case selection and perioperative planning are employed[25]. We did lensectomy through pars plicata/pars plana incisions using the vitrectomy probe for eyes without immediate IOL implantation, for less disturbance of the anterior chamber and postoperative inflammatory response and less corneal distortion that reduces visibility during vitreous surgery; and for eyes that needed immediate IOL implantation, cortical lens were aspirated through clear corneal incision in order to safely implant the IOL into the capsule bag.VA outcome in patients with PFV seems to be affected by the type and extent of PFV, age at surgery, and postoperative refractive status. In our study, VA remained stable in 34 eyes(28.8%) and improved in 84 eyes (71.2%) at last visit, which is similar to that of Vasavada et al’s[26] study of 33 patients with anterior PFV. Kuhli-Hattenbach et al[27] reported the result of visual outcome in 23 patients with PFV who underwent surgery, in which 34.7% had a VA of 6/60 or better and most of the patients were classified as anterior PFV. Others,however, reported a more modest success rate in surgically managed cases with PFV of the combined type[28-29]. In this current report, we found that postoperative improved VA was mostly seen in patients with anterior PFV. However, eyes with posterior or combined PFV could have a potential to gain better VA if the macular is relatively normal. Surgery at an early age is also reported to be a predictor for better visual outcomes[24],and we also reported in this study that age at surgery (less than 2y) was associated with improved postoperative VA.
Authors who preferred immediate IOL implantation argued that these eyes have unilateral cataract and unilateral aphakia can induce anisometropia, and IOL implantation in such eyes would provide a stable and consistent optical focus[30]. Others,however, reported higher postoperative complications such as secondary glaucoma or pupil membrane formation after immediate IOL implantation for PFV eyes[31]. We performed immediate IOL implantation in 16 eyes for patients older than 2y and 4 eyes had VA better than 0.5 logMAR whereas 1 eye complicated with pupillary membrane formation and no eye ended with glaucoma at last visit. But further study is still needed to document the optimum timing of IOL implantation for cases with PFV.
Anatomically, 94.1% (96/102) eyes in this study had regained clear visual axis after surgical repair, which is similar to Sisk et al’s[25] study; and we attribute low rate of postoperative visual axis obscuration (5.1%, 6/118) to using of vitrectomy probe to do central curvilinear posterior or anterior capsulotomy.Fifty-eight percent (33/65) of the eyes had relieved retinal detachment at last visit, of which 26.2% (17/65) had macular reattachment, and further study using optical coherence tomography is still needed to document the anatomic postoperative macular changes.
Potential limitations of the study include relatively short time of follow-up, limited data of objective VA, and its retrospective design. However, favorable anatomic and preliminary postoperative visual outcomes had been achieved with low rate of serious postoperative complications, demonstrating the feasibility of using this approach in patients with PFV. Longterm follow-up of VA results and final anatomical outcomes would still be needed in the future.
ACKNOWLEDGEMENTS
Foundations: Supported by Beijing Tongren Hospital,Capital Medical University (No.TRZDYXZY201703);Beijing Municipal Science &Technology Commission (No.Z141107002514029).
Conflicts of Interest: Liu JH, None; Lu H, None; Li SF,None; Jiao YH, None; Lin Nan, None; Liu NP, None.
REFERENCES
1 Cerón O, Lou PL, Kroll AJ, Walton DS. The vitreo-retinal manifestations of persistent hyperplastic priamy vitreous (PHPV) and their management. Int Ophthalmol Clin 2008;48(2):53-62.
2 Goldberg MF. Persistent fetal vasculature (PFV): an integrated interpretation of signs and symptoms associated with persistent hyperplastic primary vitreous (PHPV). LIV Edward Jackson Memorial Lecture. Am J Ophthalmol 1997;124(5):587-626.
3 Morrison DG, Wilson ME, Trivedi RH, Lambert SR, Lynn MJ; Infant Aphakia Treatment Study Group. Infant Aphakia Treatment Study: effects of persistent fetal vasculature on outcome at 1 year of age. J AAPOS 2011;11(5):427-431.
4 Walsh MK, Drenser KA, Capone A Jr, Trese MT. Early vitrectomy effective for bilateral combined anterior and posterior persistent fetal vasculature syndrome. Retina 2010;30(4 Suppl):S2-S8.
5 Sinha R, Bali SJ, Kumar C, Shekhar H, Sharma N, Titiyal JS, Vajpayee RB. Results of cataract surgery and plasma ablation posterior capsulotomy in anterior persistent hyperplastic primary vitreous. Middle East Afr J Ophthalmol 2013;20(3):217-220.
6 Li L, Fan DB, Zhao YT, Li Y, Cai FF, Zheng GY. Surgical treatment and visual outcomes of cataract with persistent hyperplastic primary vitreous.Int J Ophthalmol 2017;10(3):391-399.
7 Dass AB, Trese MT. Surgical results of persistent hyperplastic primary vitreous. Ophthalmology 1999;106(2):280-284.
8 Yusuf IH, Patel CK, Salmon JF. Unilateral persistent hyperplastic primary vitreous: intensive management approach with excellent outcome beyond visual maturation. BMJ Case Rep 2015;2015.pii:bcr2014206525.
9 Fujii GY, De Juan E Jr, Humayun MS, Pieramici DJ, Chang TS,Awh C, Ng E, Barnes A, Wu SL, Sommerville DN. A new 25-gauge instrument system for transconjunctival sutureless vitrectomy surgery.Ophthalmology 2002;109(10):1807-1812; discussion 1813.
10 Eckardt C, Eckert T, Eckardt U. 27-gauge Twinlight chandelier illumination system for bimanual transconjunctival vitrectomy. Retina 2008;28(3):518-519.
11 Gonzales CR, Singh S, Schwartz SD. 25-Gauge vitrectomy for paediatric vitreoretinal conditions. Br J Ophthalmol 2009;93(6):787-790.
12 Mura M, Barca F. 25-Gauge vitrectomy. Dev Ophthalmol 2014;54:45-53.
13 Kadonosono K, Yamakawa T, Uchio E, Yanagi Y, Tamaki Y, Araie M. Comparison of visual function after epiretinal membrane removal by 20-gauge and 25-gauge vitrectomy. Am J Ophthalmol 2006;142(3):513-515.
14 Khanduja S, Kakkar A, Majumdar S, Vohra R, Garg S. Small gauge vitrectomy: recent update. Oman J Ophthalmol 2013;6(1):3-11.
15 Li SY, Zhang ZP, Ji SJ, Liu HY, Si MY, Fan KS. Application of minimally invasive 23G vitrectomy via corneal approach for the treatment of pediatric cataract. Eur Rev Med Pharmacol Sci 2014;18(17):2413-2418.
16 Singh R, Kumari N, Katoch D, Sanghi G, Gupta A, Dogra MR.Outcome of 23-gauge pars plana vitrectomy for pediatric vitreoretinal conditions. J Pediatr Ophthalmol Strabismus 2014;51(1):27-31.
17 Lam DS, Fan DS, Mohamed S, Yu CB, Zhang SB, Chen WQ.25-gauge transconjunctival sutureless vitrectomy system in the surgical management of children with posterior capsular opacification. Clin Exp Ophthalmol 2005;33(5):495-498.
18 Shaikh S, Trese MT. Lens-sparing vitrectomy in predominantly posterior persistent fetal vasculature syndrome in eyes with nonaxial lens opacification. Retina 2003;23(3):330-334.
19 Shami M, McCartney D, Benedict W, Barnes C. Spontaneous retinal reattachment in a patient with persistent hyperplastic primary vitreous and an optic nerve coloboma. Am J Ophthalmol 1992;114(6):769-771.
20 Paysse EA, McCreery KM, Coats DK. Surgical management of the lens and retrolenticular fibrotic membranes associated with persistent fetal vasculature. J Cataract Refract Surg 2002;28(5):816-820.
21 Pollard ZF. Persistent hyperplastic primary vitreous: diagnosis,treatment and results. Trans Am Ophthalmol Soc 1997;95:487-549.
22 Soheilian M, Vistamehr S, Rahmani B, Ahmadieh H, Azarmina M,Mashayekhi A, Sajjadi H, Dehghan MH. Outcomes of surgical (pars plicata and limbal lensectomy, vitrectomy) and non-surgical management of persistent fetal vasculature (PFV): an analysis of 54 eyes. Eur J Ophthalmol 2002;12(6):523-533.
23 Hunt A, Rowe N, Lam A, Martin F. Outcomes in persistent hyperplastic primary vitreous. Br J Ophthalmol 2005;89(7):859-863.
24 Alexandrakis G, Scott IU, Flynn HW Jr, Murray TG, Feuer WJ. Visual acuity outcomes with and without surgery in patients with persistent fetal vasculature. Ophthalmology 2000;107(6):1068-1072.
25 Sisk RA, Berrocal AM, Feuer WJ, Murray TG. Visual and anatomic outcomes with or without surgery in persistent fetal vasculature.Ophthalmology 2010;117(11):2178-2183.e1-2.
26 Vasavada AR, Vasavada SA, Bobrova N, Praveen MR, Shah SK,Vasavada VA, Pardo AJV, Raj SM, Trivedi RH. Outcomes of pediatric cataract surgery in anterior persistent fetal vasculature. J Cataract Refract Surg 2012;38(5):849-857.
27 Kuhli-Hattenbach C, Hofmann C, Wenner Y, Koch F, Kohnen T.Congenital cataract surgery without intraocular lens implantation in persistent fetalvasculature syndrome: long-term clinical and functional results. J Cataract Refract Surg 2016;42(5):759-767.
28 Bosjolie A, Ferrone P. Visual outcome in early vitrectomy for posterior persistent fetal vasculature associated with traction retinal detachment.Retina 2015;35(3):570-576.
29 Schulz E, Griffiths B. Long-term visual function and relative amblyopia in posterior persistent hyperplastic primary vitreous (PHPV).Strabismus 2006;14(2):121-125.
30 Matsuo T. Intraocualr lens implantation in unilateral congenital cataract with minimal levels of persistent fetal vasculature in the first 18 months of life. Springerplus 2014;3:361.
31 Johnson CP, Keech RV. Prevalence of glaucoma after surgery for PHPV and infantile cataracts. J Pediatr Ophthalmol Strabismus 1996;33(1):14-17.