INTRODUCTION
Severe stenosis of the extracranial segment of internal carotid artery (ICA) can cause visual disturbances associated with ocular ischemia, such as the ocular ischemic syndrome (OIS). Stenosis or occlusion of the common or ICA affects not only retinal blood flow but also choroidal blood flow, resulting in insufficient blood perfusion to the retinal inner and outer layers, which may cause ischemic ocular lesions. The most common ischemic ocular symptom is acute transient monocular blindness due to entrapment of emboli in the retinal arterial system[1]. Patients with ICA stenosis or occlusion(5%-21%) may cause chronic progressive ocular ischemia[2-3].
The in vivo structure of the choroid cannot be visualized properly with conventional methods such as fundus photography and other methods. With the development of optical coherence tomography (OCT), measurements of choroidal thickness are becoming more common, and it is a procedure in the clinic and in research[4-7]. Spectral-domainoptical coherence tomography(SD-OCT) has been used to evaluate the retinal nerve fiber layer (RNFL) thickness in various diseases, including multiple sclerosis, neuromyelitis optica, and clinical isolated syndromes[8-10]. Enhanced-depth imaging OCT (EDI-OCT) can assess the choroidal thickness[4,11]. Because the choroid is an important vascular tissue layer, certain characteristics of the choroid, such as its thickness, have been challenging to study histologically[12]. Quantitative analysis of choroidal thickness and volume is important in the evaluation of chorioretinal diseases, as well as normal physiology[13-17].
Although adult choroidal thickness has been well evaluated,choroidal thickness studies in ICA patients have been limited.SD-OCT enables deep choroidal imaging and can make the evaluation of pediatric choroidal thickness and choroidal volume easier, more comprehensive, and more objective. Still,there have been no prior studies using SD-OCT to measure choroidal thickness and volume in ICA patients. Kang et al[18]reported 3 cases of OIS patients who showed lower choroidal thickness in the affected eye.
However, previous research has not revealed any information about the effect of internal carotid artery stenosis on retinal thickness, subfoveal choroidal thickness, or choroidal volume.OIS is one of the most severe clinical illnesses caused by carotid artery stenosis. We postulated that ICA stenosis may affect the outer layers of retinal and choroidal thickness and tried to demonstrate a difference in the retinal and choroidal structure changes in ICA with 46 patients with ICA.
SUBJECTS AND METHODS
All procedures performed in studies involving human participants were in accordance with the ethical standards of the local Ethics Committee of Beijing Friendship Hospital.The Declaration of Helsinki (2008) was followed in this study.In addition, all participants provided written informed consent and received a stipend.
Study Design and Participants A retrospective review was conducted of all patients with a diagnosis of ICA stenosis greater than 65% on only one side (the opposite ICA Stenosis had less than 40% stenosis) were included at Beijing Friendship Hospital, Capital Medical University, Beijing,China, from June 2015 to June 2016. Our study was performed according to the principles of the Declaration of Helsinki. All of the participants were combined with amaurosis fugax, and all of them with normal vision acuity and vision field. The eyes were divided into two groups based on the degree of ICA stenosis. The eyes ipsilateral to the ICA with greater stenosis(>65%) were recruited as ICA Stenosis group, and the opposite eyes (which were ipsilateral to the ICA with less than 40%stenosis) were recruited as control group. The two groups were compared in terms of the percentage of ICA stenosis, retinal thickness, inner layer and outer layer of retinal thickness,choroidal thickness, retinal volume and choroidal volume.
The inclusion criteria were: all patients with head and neck computed tomography (CT) findings of ICA stenosis greater than 65% on only one side (the opposite ICA Stenosis had less than 40% stenosis). The exclusion criteria were: 1) a refractive error of >±3.00 DS or >±2.00 DC, an intraocular pressure (IOP) of >21 mm Hg, choroidal neovascularization or other macular diseases that might affect vision, active intraocular inflammation and/or infection, or a history of any type of intraocular surgery (except cataract surgery),and diabetic retinopathy; 2) patients with peripheral vascular disease, limb paralysis, serious eye disease and a treatment history (corneal disease, glaucoma, macular degeneration,ocular trauma, pathological myopia and serious cataract); 3)acute myocardial infarction, uncontrolled hypertension, stroke within a few weeks prior to this study, infectious inflammatory disease; 4) patients with ocular hemodynamics abnormality and abnormal fundus in fundus fluorescein angiography; 5)patients who were uncooperative for evaluations or test results and who underwent carotid endarterectomy before SD-OCT examination could not be analyzed.
Head-and-neck Computed Tomographic Angiography The examinations were performed by the Philips iCT (PHILIPS,Netherland). The stenosis ratio was calculated by the North American Symptomatic Carotid Endarterectomy Trial(NASCET) stenosis grading method and was used for the estimated percentage of stenosis and classification. Vascular stenosis degree%=normal vessel diameter-narrow vessel diameter, divided by the normal vessel diameter ×100%.
Ophthalmic Examinations All the patients underwent a baseline examination including refraction, best-corrected Snellen visual acuity, bilateral ophthalmic examination, a dilated fundus and slit-lamp examination, and SD-OCT.The OCT examinations were performed using a Heidelberg Spectralis SD-OCT machine (Heidelberg Engineering,Heidelberg, Germany) according to the standard protocols for obtaining macular and peripapillary images. The measurement of the segmented retinal layers was evaluated by a highspeed scan protocol, which provided the average retinal and choroidal thicknesses and choroidal volumes of 8 quadrants according to the Early Treatment Diabetic Retinopathy Study(ETDRS) (Figure 1).
Retinal thickness and volume measurement can be measured by and the automatic program in the machine. For choroidal thickness and volume measurements, we manually moved the automatically segmented internal limiting membrane line to the choroidoscleral junction. Once we changed the automatically segmented line and set a vertical line perpendicular to the center of the fovea, the choroidal thickness and volume were automatically calculated.
The choroidal and retinal volumes were manually measured by two retina specialists (Wang H and Li HY); to make the measurements, we moved the automatically segmented internal limiting membrane line to the choroidoscleral junction manually. Once we changed the automatically segmented line and set a vertical line perpendicular to the center of the fovea,the choroidal and retinal volume were automatically calculated and displayed within the ETDRS grid. We obtained nine choroidal volume and retinal volume data points within 3000 µm,3000-6000 µm in the EDTRS grid (foveal center, superior,nasal, inferior, and temporal). We analyzed the differences in choroidal volume and retinal volumes between the ICA eye and the fellow eye.
Statistical Analysis Kolmogorov-Smirnov test was used to identify the normality of distribution. The independent t-test and Mann-Whitney U test were used to compare OCT parameters between ICA stenosis eyes and fellow eyes.
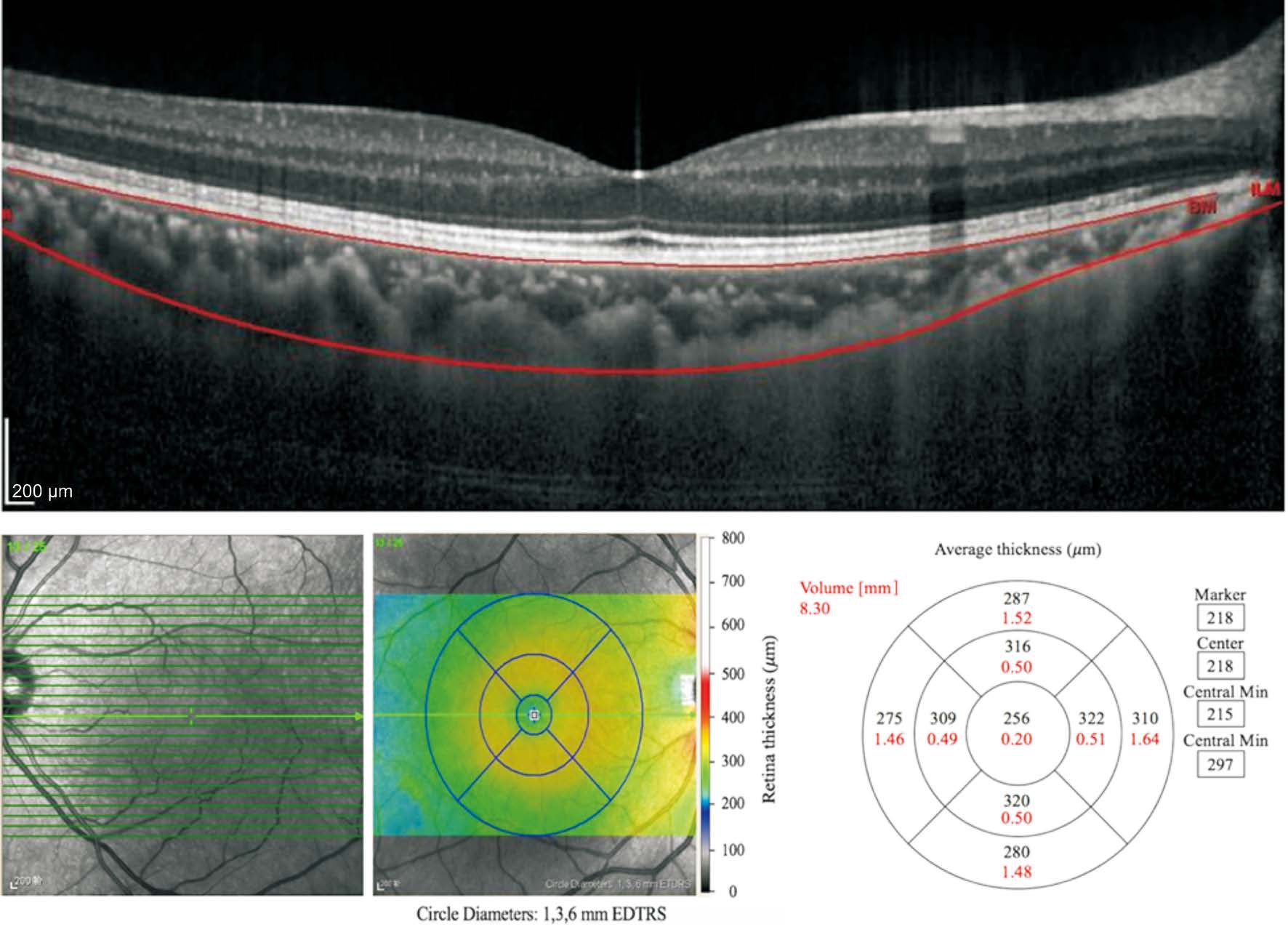
Figure 1 Retinal and subfoveal choroidal thickness, volume measurements.
Spearman rank correlation coefficient was used to evaluate associations between the measured variables. SPSS version 22.0 (SPSS Inc., Chicago, IL, USA) was used to perform all analyses, and P<0.05 was considered statistically significant.
RESULTS
We diagnosed 46 patients with unilateral ICA at Beijing Friendship Hospital, Capital Medical University, Beijing,China, from June 2015 to June 2016. Table 1 shows the clinical characteristics of ICA Stenosis group and control group. Because the we selected the ICA Stenosis group and the control group from the same patient, so the major clinical characteristics (age, sex, BMI, systemic disease situation of hypertension, hyperlipidemia and diabetes were same between the two groups). The mean age of all, including the eyes, was 61.65±10.09y. Of the 46 patients, 31 were male. The proportion of carotid stenosis of the ICA eye was 75.05%±33.63% and the proportion of the fellow eye was 36.78%±18.96%. The portion of patients with hypertension was 78.26%, the portion of hyperlipidemia was 56.52% and the portion of diabetes was 50.00%. The baseline BCVA of the ICA eye was significantly worse in ICA Stenosis group than it was in control group (ICA Stenosis group:0.92±0.55 and control group: 0.26±0.47, P=0.003). The refractive error (mean spherical equivalent) was -0.86±0.70 D in ICA Stenosis group versus -0.86±0.67 D in control group.The mean IOP was 15.06±2.24 mm Hg in ICA Stenosis group versus 15.19±3.31 mm Hg in control group. The mean axial length was 23.46±1.04 mm in ICA Stenosis group versus 23.23±1.08 mm in control group. The refractive error, the mean IOP values and axial length were not significantly different between the two groups (P=0.946, 0.825, 0.838, respectively)(Table 1).
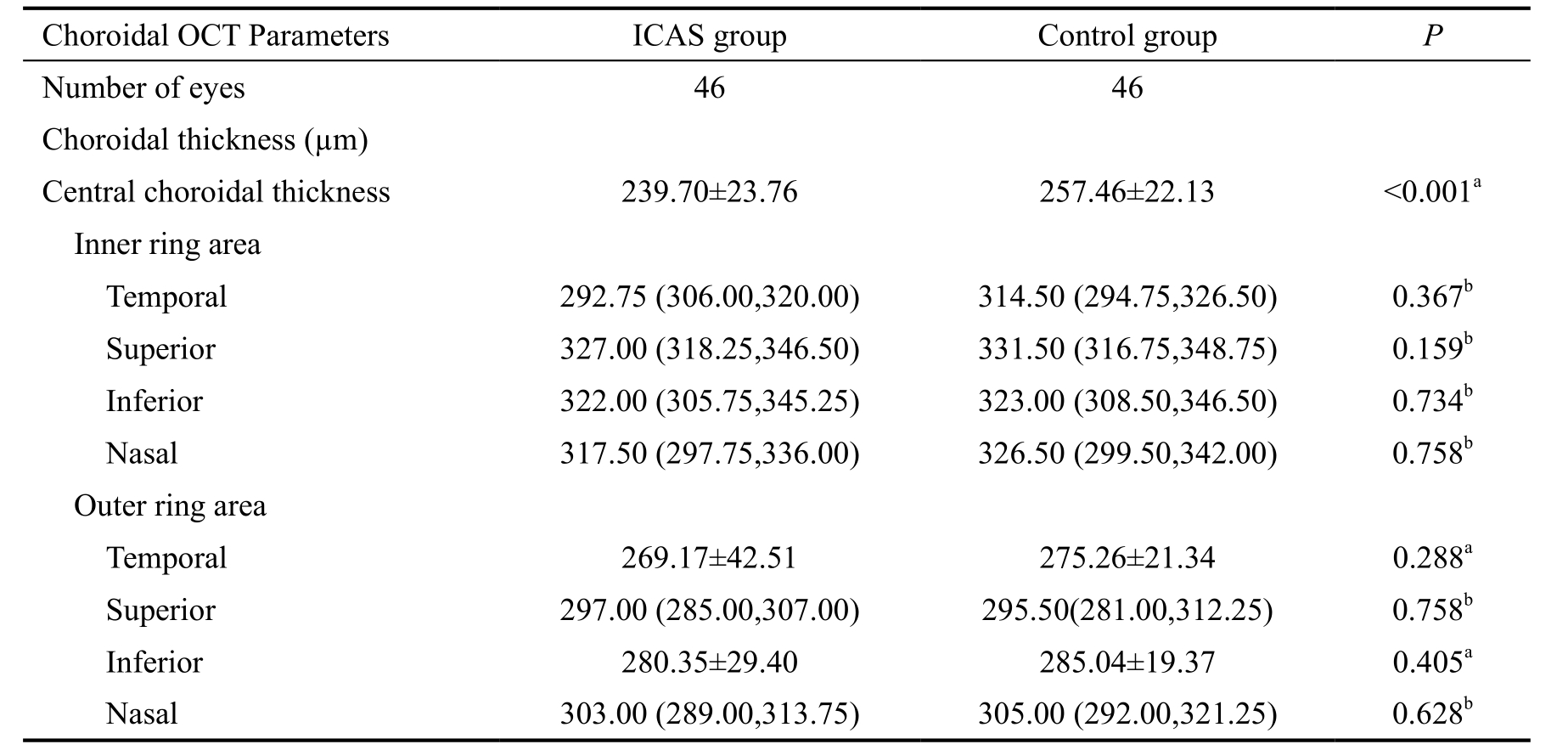
The retinal thickness, the mRNFL thickness, the inner and outer retinal thickness were not significantly between the two groups. (P=0.834, 0.285, 0.552, 0.733, respectively; Mann-Whitney U test and independent t-test respectively) (Table 2).In the ETDRS mapping of retinal and choroidal volumes, the mean central choroidal thickness of ICA Stenosis group was significantly lower than that of the control group (ICA Stenosis group: 239.70±23.76 µm and control group: 257.46±22.13 µm,P<0.001, Independent t-test) (Table 3). However, the mean macular choroid thickness values within circles of diameter 3.0 mm(temporal, superior, inferior and nasal) were not significantly different between the two groups (P=0.367, 0.159, 0.734, 0.758,respectively; Mann-Whitney U test). The mean macular choroid thickness values within circles of diameter 6.0mm (temporal,superior, inferior and nasal) were also not significantly different between the two groups (P=0.288, 0.758, 0.405, 0.628; Mann-Whitney U test and independent t-test respectively) (Table 3).
We also compared retinal and choroidal volume retinal and choroidal volumes within circles of diameter 1.0, 3.0, and 6.0 mm.The retinal and choroidal volume values in the four inner and four outer sectors were not significantly different between two groups (Table 4).
Table 1 Epidemiologic and clinical characteristics of ICA eyes
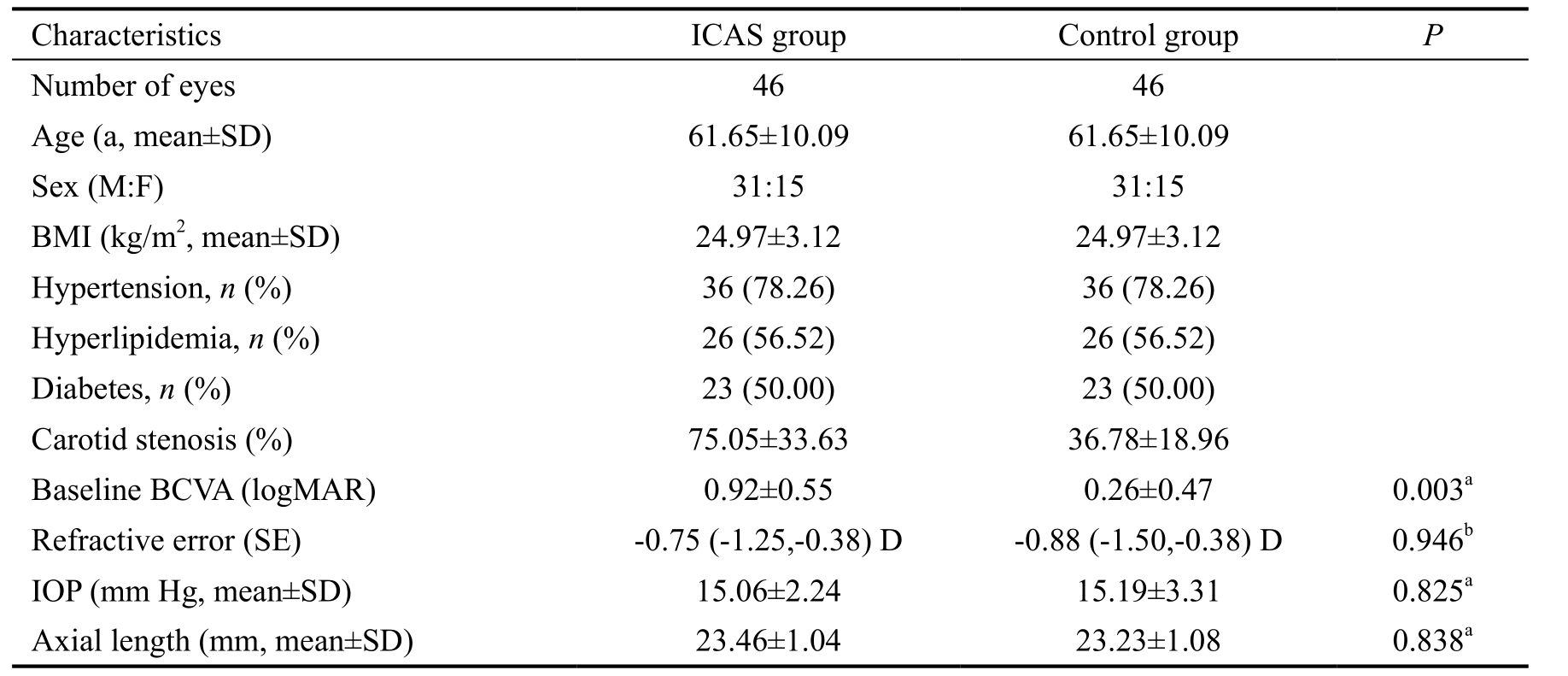
ICA: Internal carotid artery; BCVA: Best corrected visual acuity; SE: Spherical equivalent; IOP: Intraocular pressure. aP values were calculated using the independent t-test. bP values were calculated using the Mann-Whitney U test.
Table 2 Retinal thickness of unilateral ICA eyes
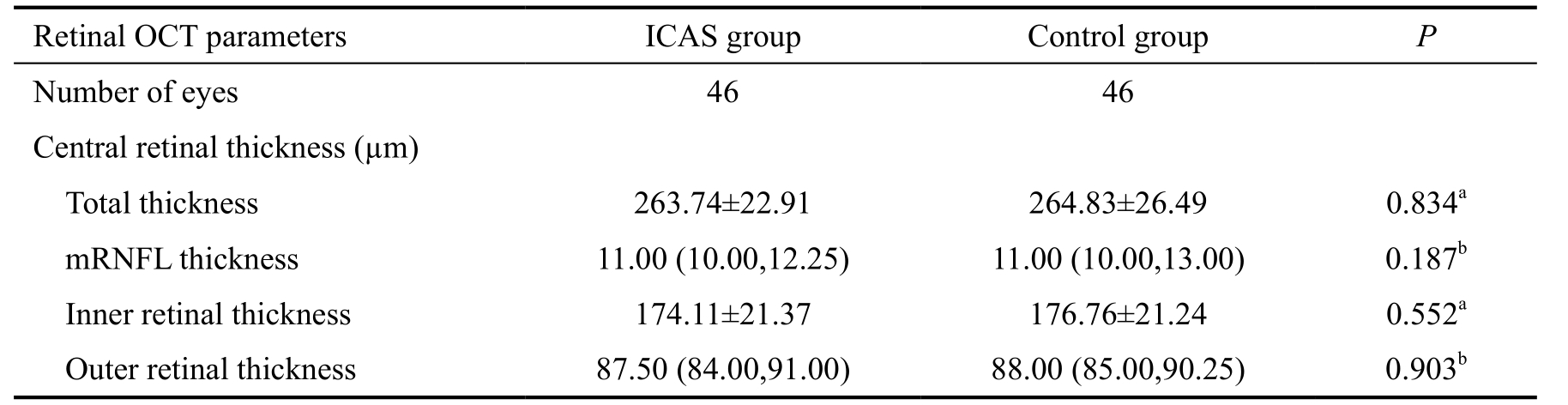
aP values were calculated using the independent t-test. bP values were calculated using the Mann-Whitney U test.
Table 3 Choroidal thickness of unilateral ICA eyes
aP values were calculated using the independent t-test. bP values were calculated using the Mann-Whitney U test.
There was a statistically significant positive correlation between the percentage of ICA stenosis and the following OCT parameters: the the central choroidal thickness, the central retinal thickness, the foveal center choroidal volume, and the foveal center retinal volume (r=0.854, 0.678, 0.729, and 0.785,respectively; P<0.001). These data were shown in a scatter plot(Figure 2).
A correlation analysis between the the percentage of ICA stenosis and the central retinal thickness, the central choroidal thickness, the foveal center choroidal volume, and the foveal center retinal volume is shown in Table 5.
DISCUSSION
The primary component of the ocular blood flow is the choroidal circulation. It alone accounts for 85% of all ocularblood flow. The choroid receives more than 70% of the blood flow that enters the uveal structures, which can get 95% of the eye blood supply[19]. The choroid is a highly vascularized tissue, provides oxygen and nourishment to the outer retina layers[20].
Table 4 Retinal volume and choroidal volume of unilateral ICA eyes
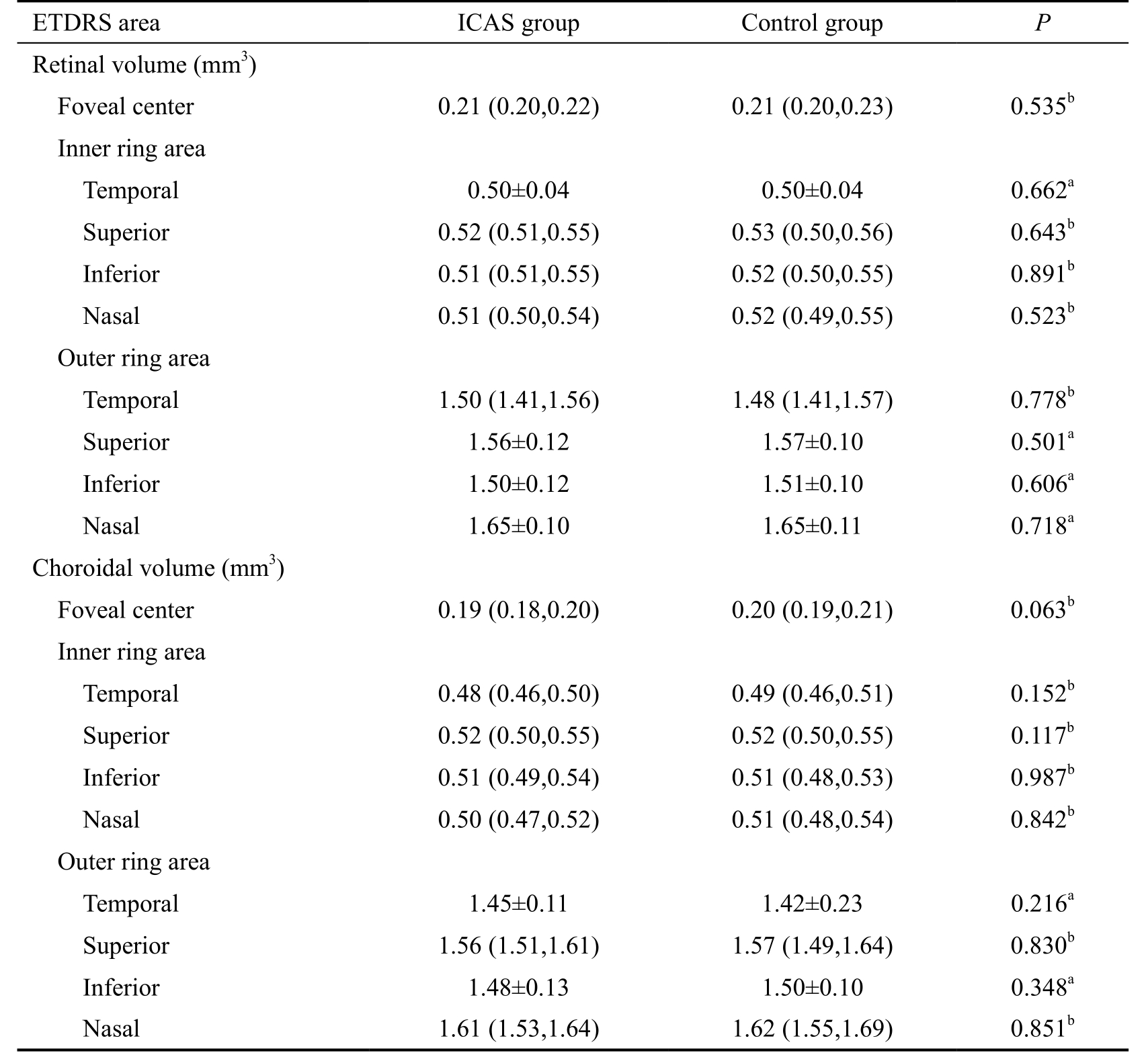
aP values were calculated using the independent t-test. bP values were calculated using the Mann-Whitney U test.
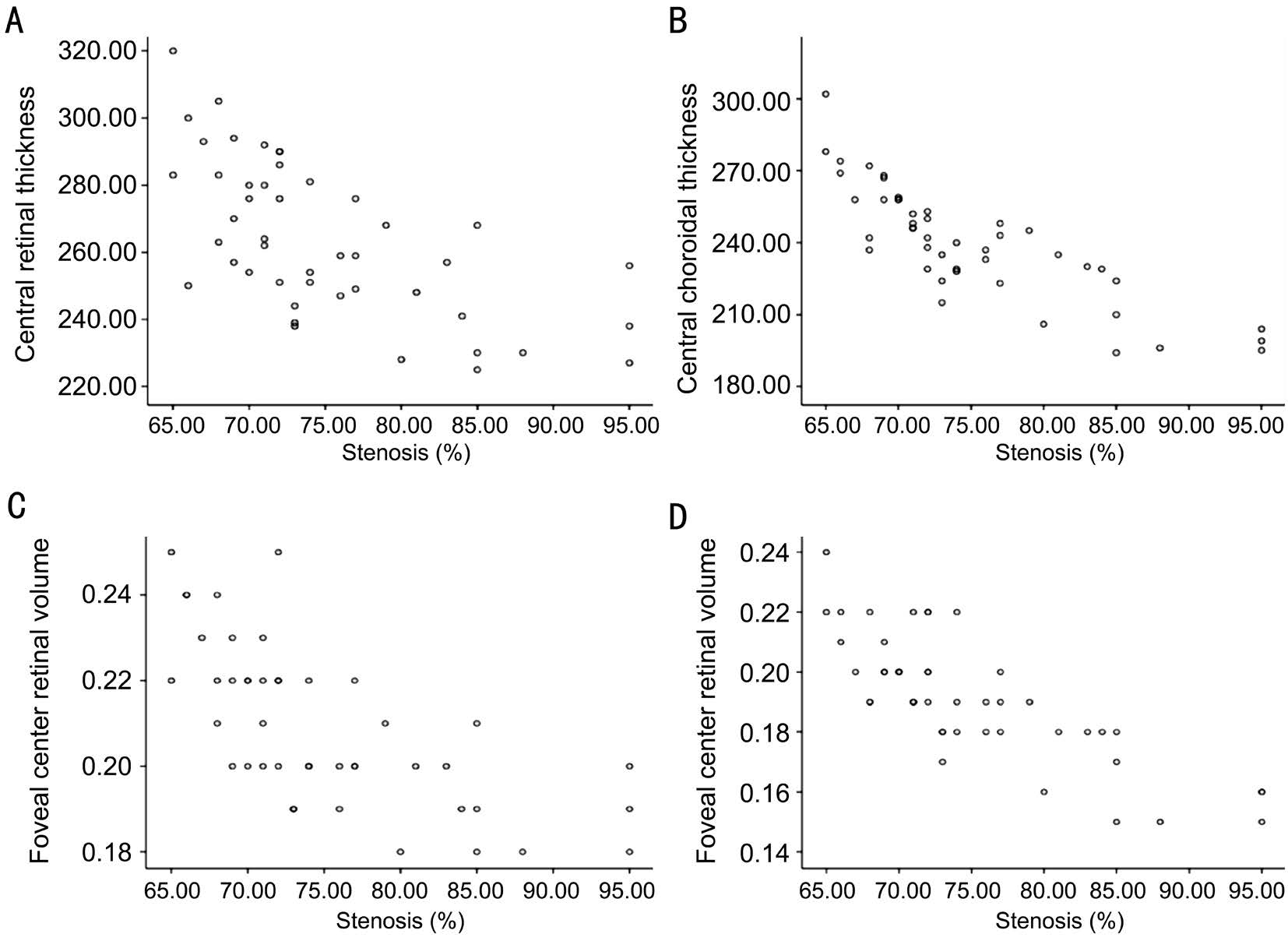
Figure 2 Scatter plot graph showing the relationship percentage of ICA stenosis and OCT parameters A: Central retinal thickness; B:Central choroidal thickness; C: The foveal center choroidal volume; D: The foveal center retinal volume.
Table 5 Spearman rank correlation analyses between the percentage of ICA stenosis and OCT parameters
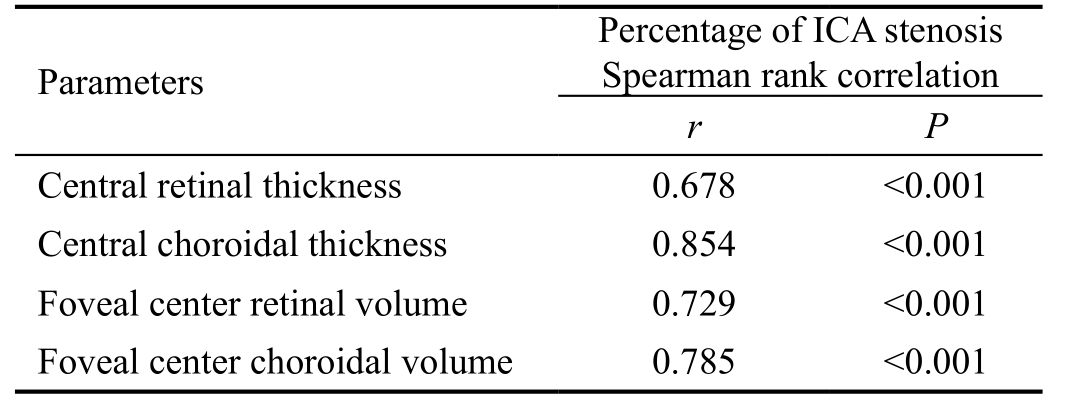
ICA: Internal carotid artery. P value of less than 0.05 was considered to be significant.
The ophthalmic artery is the first branch of the ICA, divided to form the posterior ciliary artery (PCA), which is responsible for the blood supply of the posterior choroid[21]. The PCA supply blood to the outer retinal layers and choroid. Stenosis or occlusion of the ICA may cause disturbance of the retina and choroid circulation, eventually leading to structural and function change.
Kim et al[12] reported that the baseline logMAR BCVA was significantly worse in OIS eyes than in the fellow eyes. In our study, we obtained similar results showing that the baseline logMAR BCVA was significantly worse in severe internal carotid artery stenosis eyes than in control eyes (0.92±0.55 vs 0.26±0.47; P=0.003), indicating some aspects of impaired vision in patients with severe ICA stenosis.
Stenosis or occlusion of the common or ICA affects not only retinal blood flow but also choroidal blood flow. However, it is not certain whether the choroidal thickness change occurs earlier than the retinal changes with the development of ICA stenosis. It is also not possible to know when the retina and choroid change occurs, whether the choroidal thinning occurred before the retinal changes, or whether the retinal changes occurred before the choroidal thinning with the progression of ICA stenosis. Thus, in this study, we designed methods to measure some choroidal and retinal OCT values between patients with ICA stenosis of more than 65% and the opposite eye, to evaluate whether severe ICA stenosis has an effect on retinal, choroidal thickness and volume compared to the opposite eye. We also wanted to ensure the change order of change of the choroidal thinning and retinal changes with the progression of ICA stenosis. Ahmad et al[22] reported that patients with coronary artery disease (CAD) have a thinner macular choroid than normal. Kang et al[18] reported that,compared with fellow eyes, the choroidal thickness of OIS eyes was significantly decreased. Kim et al[12] reported that in their study that the choroidal thickness and volume of OIS eyes were smaller than those of unaffected fellow eyes. We compared some choroidal and retinal OCT values between patients (38 males and 17 females) with more than 65%carotid artery stenosis on one side and less than 40% stenosis on the other side. We have demonstrated that unilateral ICA Stenosis eyes have a lower choroidal thickness than the control eyes, indicating impaired choroidal circulation in patients with severe ICA eyes. On the other hand, our results showed that no retina structure changes such as the retinal thinning and retinal volume change occurred in severe ICA Stenosis eyes.A possible explanation is that the choroidal thinning may have occurred before the retinal changes in in patients with severe ICA Stenosis. Therefore, future studies that examine a larger number of patients are needed to confirm the difference in choroidal thickness in severe ICA stenosis eyes, and it will be necessary to observe how the retina and choroid change with the progression of ocular ischemic changes due to severe ICA stenosis.
Some physiological factors may have an effect on choroidal thickness[23]. Many studies on choroidal thickness have reported that axial length, refractive error, sex, and age can influence choroidal thickness[13-14,24]. In addition, other factors such as hypercholesterolemia, diurnal variation, axial length,refractive factor, intraocular pressure may also influence it.Nagasawa et al[25] reported that choroidal thickness correlated with age, axial length, refractive error, and body mass index.Kim et al[13] reported that pediatric choroidal thickness was associated only with axial length. In our study, we chose the same group of patients that there was no difference in age,sex between the two groups. However, smoking, alcohol use, exercising, sleeping conditions, caffeine, gender was not investigated in our study. We will control those factors to draw a firm conclusion about the choroidal thickness of healthy individual’s and the ICA stenosis patients in our future studies.In the present study, there was a statistically significant positive correlation between the percentage of ICA stenosis and the central choroidal thickness, the central retinal thickness, the foveal center choroidal volume, and the foveal center retinal volume (r=0.854, 0.678, 0.729, and 0.785, respectively;P<0.001), indicating that these OCT parameters increase as the percentage of stenosis increases. This result is similar to that of our previous study, in which we found that the subfoveal choroidal thickness (SFChT) of ICA eyes was significantly lower than that of normal eyes[26].
However, there were several limitations to our study. First, the chorio-scleral border is defined manually and the accuracy of this process was not evaluated. Second, we measured only ICA Stenosis eyes and the control eyes, further studies are needed to determine whether the choroidal thickness is correlated with the body mass index, diabetes duration, hyperlipidemia course,and other factors. This question requires dedicated study.
The choroidal thickness in severe ICA stenosis eyes is lower than in fellow eyes, indicating that impaired choroidal circulation in patients with severe ICA eyes. The choroidal thinning may occur before the retinal changes in in patients with severe ICA stenosis. Knowledge of the choroidal profile and thickness in patients’ eyes may help in understanding physiological changes and evaluating chorioretinal conditions in patients with ocular ischemic changes caused by severe ICA stenosis. OCT is a reliable observation index in the clinical follow-up of patients with ICA stenosis and ocular ischemic syndrome.
ACKNOWLEDGEMENTS
The authors acknowledge Ming-Ming Li and Fan Zhang,Department of Ophthalmology, Beijing Friendship Hospital,Capital Medical University, for their assistance in collecting data.
Authors’ contributions: Li HY was involved in the conception,designing of the study and critical revision of the manuscript,she has also provided final approval of the version to be published. Wang H contributed to the acquisition, analysis and interpretation of data as well as drafting the manuscript and revising it critically. Wang YL was involved in the conception and design of the study. All authors have involved in patient management and acquisition of data; All authors have taken part in revising the manuscript for important intellectual content. All authors have given final approval of the version to be published.
Foundation: Supported by Start funding of Beijing Friendship Hospital (No.yyqdkt2016-8).
Conflicts of Interest: Wang H, None; Wang YL, None; Li HY, None.
REFERENCES
1 Dugan JD Jr, Green WR. Ophthalmologic manifestations of carotid occlusive disease. Eye (Lond) 1991;5(Pt 2):226-238.
2 Sarkies NJ, Shilling JS, Russell RW. Fluorescein angiography in carotid disease. Trans Ophthalmol Soc U K 1986;105(Pt 4):489-493.
3 Kersemakers P, Beintema M, Lodder J. Venous stasis retinopathy unlikely results from internal carotid artery obstruction alone. Cerebrovasc Dis 1992;2(5):305-307.
4 Maruko I, Iida T, Sugano Y, Ojima A, Sekiryu T. Subfoveal choroidal thickness in fellow eyes of patients with central serous chorioretinopathy.Retina 2011;31(8):1603-1608.
5 Nakayama M, Keino H, Okada AA, Watanabe T, Taki W, Inoue M,Hirakata A. Enhanced depth imaging optical coherence tomography of the choroid in Vogt-Koyanagi-Harada disease. Retina 2012;32(10):2061-2069.6 Fujiwara T, Imamura Y, Margolis R, Slakter JS, Spaide RF. Enhanced depth imaging optical coherence tomography of the choroid in highly myopic eyes. Am J Ophthalmol 2009;148(3):445-450.
7 Manjunath V, Goren J, Fujimoto JG, Duker JS. Analysis of choroidal thickness in age-related macular degeneration using spectral-domain optical coherence tomography. Am J Ophthalmol 2011;152(4):663-668.
8 Morrow MJ, Wingerchuk D. Neuromyelitis optica. J Neuroophthalmol 2012;32(2):154-166.
9 Watson GM, Keltner JL, Chin EK, Harvey D, Nguyen A, Park SS.Comparison of retinal nerve fiber layer and central macular thickness measurements among five different optical coherence tomography instruments in patients with multiple sclerosis and optic neuritis. J Neuroophthalmol 2011;31(2):110-116.
10 Trip SA, Schlottmann PG, Jones SJ, Kallis C, Altmann DR, Garway-Heath DF, Thompson AJ, Plant GT, Miller DH. Scanning laser polarimetry quantification of retinal nerve fiber layer thinning following optic neuritis. J Neuroophthalmol 2010;30(3):235-242.
11 Margolis R, Spaide RF. A pilot study of enhanced depth imaging optical coherence tomography of the choroid in normal eyes. Am J Ophthalmol 2009;147(5):811-815.
12 Kim DY, Joe SG, Lee JY, Kim JG, Yang SJ. Choroidal thickness in eyes with unilateral ocular ischemic syndrome. J Ophthalmol 2015;2015:620372.
13 Kim KH, Kim DG. The relationship among refractive power, axial length and choroidal thickness measured by SD-OCT in myopia. Journal of the Korean Ophthalmological Society 2012;53(5):626.
14 Ikuno Y, Kawaguchi K, Nouchi T, Yasuno Y. Choroidal thickness in healthy Japanese subjects. Invest Ophthalmol Vis Sci 2010;51(4):2173-2176.
15 Kim SW, Oh J, Kwon SS, Yoo J, Huh K. Comparison of choroidal thickness among patients with healthy eyes, early age-related maculopathy, neovascular age-related macular degeneration, central serous chorioretinopathy, and polypoidal choroidal vasculopathy. Retina 2011;31(9):1904-1911.
16 Cho JH, Bae SH, Han JR, Nam WH, Kim HK. Comparison of choroidal thickness in eyes with central serous chorioretinopathy,asymptomatic fellow eyes and normal eyes. Journal of the Korean Ophthalmological Society 2012;53(1):87.
17 Chung SE, Kang SW, Lee JH, Kim YT. Choroidal thickness in polypoidal choroidal vasculopathy and exudative age-related macular degeneration. Ophthalmology 2011;118(5):840-845.
18 Kang HM, Lee CS, Lee SC. Thinner subfoveal choroidal thickness in eyes with ocular ischemic syndrome than in unaffected contralateral eyes.Graefes Arch Clin Exp Ophthalmol 2014;252(5):851-852.
19 Parver LM, Auker C, Carpenter DO. Choroidal blood flow as a heat dissipating mechanism in the macula. Am J Ophthalmol 1980;89(5):641-646.
20 Nickla DL, Wallman J. The multifunctional choroid. Prog Retin Eye Res 2010;29(2):144-168.
21 Hayreh SS. Acute retinal arterial occlusive disorders. Prog Retin Eye Res 2011;30(5):359-394.
22 Ahmad M, Kaszubski PA, Cobbs L, Reynolds H, Smith RT.Choroidal thickness in patients with coronary artery disease. PLoS One 2017;12(6):e0175691.
23 Wong IY, Wong RL, Zhao P, Lai WW. Choroidal thickness in relation to hypercholesterolemia on enhanced depth imaging optical coherence tomography. Retina 2013;33(2):423-428.
24 Li XQ, Larsen M, Munch IC. Subfoveal choroidal thickness in relation to sex and axial length in 93 Danish university students. Invest Ophthalmol Vis Sci 2011;52(11):8438-8441.
25 Nagasawa T, Mitamura Y, Katome T, Shinomiya K, Naito T, Nagasato D, Shimizu Y, Tabuchi H, Kiuchi Y. Macular choroidal thickness and volume in healthy pediatric individuals measured by swept-source optical coherence tomography. Invest Ophthalmol Vis Sci 2013;54(10):7068-7074.
26 Wang H, Li H, Zhang X, Qiu L, Wang Z, Wang Y. Ocular image and haemodynamic features associated with different gradings of ipsilateral internal carotid artery stenosis. J Ophthalmol 2017;2017:1842176.