INTRODUCTION
Treatment options for retinal eye diseases have expanded over the years, and the increasing number of clinical studies on the effectiveness of these treatments has raised attention to the management regime of these eye diseases.Ranibizumab (Lucentis) is a recombinant humanized monoclonal antibody fragment that binds to vascular endothelial growth factor A (VEGFA) and prevents it from binding to receptors,
thus suppressing neovascularization[1]. Ranibizumab is currently one of the most common drugs used for treating age-related macular degeneration (AMD)[2], macular edema following retinal vein occlusion[3], diabetic macular edema (DME)[3]and diabetic retinopathy[4]. Photodynamic therapy (PDT) has also been used to treat abnormal growth of blood vessels in exudative AMD[5], pathologic myopia[6] and histoplasmosis[7].Ranibizumab and PDT have been the ‘gold standard’ treatment options for AMD and polypoidal choroidal vasculopathy(PCV) in many countries, but treatment options are now more varied[1,8].
While many treatment pattern studies have been reported in other countries[9-12], the majority of these have been on patients of European descent with fewer studies investigating the treatment trends in Asian populations[8,13-14]. It is recognized that the trends in Asia might be different due to heterogeneity[15-17]since the Asian region stretches from far north-eastern Asian nations, such as Japan and Korea, through to Southeast Asian countries, such as Malaysia and Singapore, and across to India. Additionally, this heterogeneity might result in different prevalences of retinal diseases resulting in different treatment trends; for example, the prevalence of PCV in the Asian population is much higher than in the European population[13,16,18]. Such conflicting results have been reported on treatments in Asia, and generally there is a lack of information available on the treatment patterns of ranibizumab and PDT, especially in Malaysia. This prompted us to conduct this retrospective study to determine how treatment patterns of ranibizumab and PDT changed between 2010 and 2014.
SUBJECTS AND METHODS
This study is a 5-year retrospective cohort study of patients who had attended the Ophthalmology Clinic at Hospital Selayang between January 2010 and December 2014.Hospital Selayang is the most referred hospital for eye diseases in Malaysia. Approval for this study was obtained from the Medical Research Ethics Committee (MREC) of the National Medical Research Register (NMRR) (Ethics No.NMRR-14-1176-21475). The cohort was selected from the medical records stored in Hospital Selayang’s Electronic Medical Record (EMR) database. Inclusion criteria for the study were patients with eye diseases who received intravitreal ranibizumab injections and PDT at the Ophthalmology Clinic,Hospital Selayang between 2010 and 2014. Malaysian citizens were recruited who belonged to one of the nation’s three main ethnic groups: Malays, Chinese and Indians. Patients who did not receive ranibizumab injections and PDT, non-Malaysians and those whose medical records were non-retrievable or incomplete were excluded from this study.

Figure 1 Flow diagram presenting study sample selection of patient records.
All data were retrieved from the patient’s medical records, and was based on their first visit to the eye clinic in the respective year. Socio-demographic data relating to age, gender and ethnicity was obtained. In addition, data on any clinical history of co-morbidities, diagnostic procedures performed for each patient [including optical coherence tomography (OCT) and fundus angiography (FFA) or indocyanine green (ICG)] was also taken. The diagnoses of eye disease during the patient’s visit to the clinic were recorded, and treatment options given to the patients were classified into ranibizumab monotherapy,ranibizumab combined with PDT and PDT monotherapy.
All statistical analyses were undertaken using the Statistical Package for Social Sciences (SPSS version 22, Chicago, IL,USA). Findings were described by frequencies, percentages,means and standard deviations (SD). A Chi-square test was used to calculate the association between socio-demographic,co-morbidities, diagnostic procedures and treatments. Analysis of variance (ANOVA) was used to analyse associations of continuous variables. Multiple logistic regressions were used to determine the parameters associated with each treatment.Data with zero value in any treatment groups was excluded from logistic regression analyses. All cases were analysed with 95% confidence intervals (CI), and the level of significance was set at P < 0.05.
RESULTS
The broad database search of medical records from January 2010 to December 2014 retrieved a total of 4240 patients.After excluding duplicates and irrelevant records (due to patients not receiving ranibizumab or PDT therapy in the clinic, non-Malaysians and non-retrievable or incomplete medical records), a final total of 821 patients were included in this study. Details on patient selection are presented in Figure 1.
Table 1 shows the demographic and co-morbidity information of all retained subjects. Overall, the mean age was 65.9±11.73y; 63.1% of participants were male, and 74.4% were aged ≥60y. Although no significant difference was observed between the years, from the mean age of patients it can be observed that in 2014 the patients receiving treatment in the clinic were younger (64.7±11.34y) than in 2010 (68.8±10.35y).No significant difference was observed between the genders,ethnicities or age groups of patients between 2010 and 2014.The presence of co-morbidities was prevalent, with 25.2%,9.7% and 30.6% having hypertension, diabetes mellitus or a combination of hypertension and diabetes mellitus. A significant difference of P=0.003 and P=0.041 was observed between 2010 and 2014 for patients with hypertension and patients with diabetes mellitus respectively. Patients with hypertension decreased in 2014 (25.6%) compared to 2010(46.6%). Contradictorily, patients with diabetes mellitus increased from 1.7% in 2010 to 9.7% in 2014.
Table 1 Characteristics of selected patients from 2010-2014 n (%)
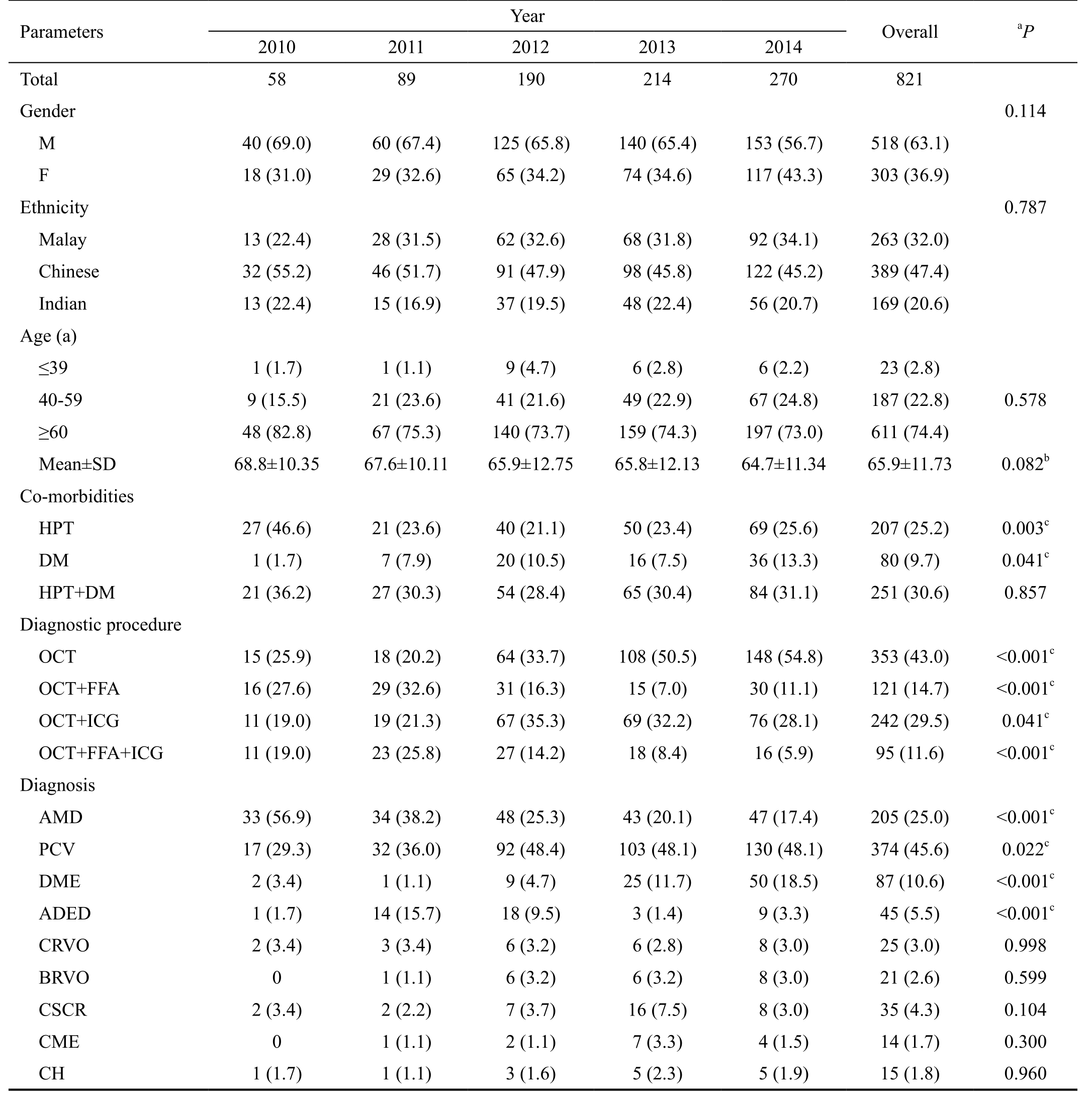
Data presented as mean±SD for age and data are reported as number of subjects with percent in parentheses. HPT: Hypertension; DM: Diabetes mellitus; OCT: Optical coherence tomography; FFA: Fundus fluorescein angiography; ICG: Indocyanine green; PDT: Photodynamic therapy;AMD: Age-related macular degeneration; PCV: Polypoidal choroidal vasculopathy; DME: Diabetic macular edema; ADED: Advanced diabetic eye disease; CRVO: Central retinal vein occlusion; BRVO: Branch retinal vein occlusion; CSCR: Central serous chorioretinopathy; CME:Cystoid macular edema; CH: Choroidal hemangioma. aChi-square test; bAnalysis of variance, ANOVA; cSignificant value, P<0.05.
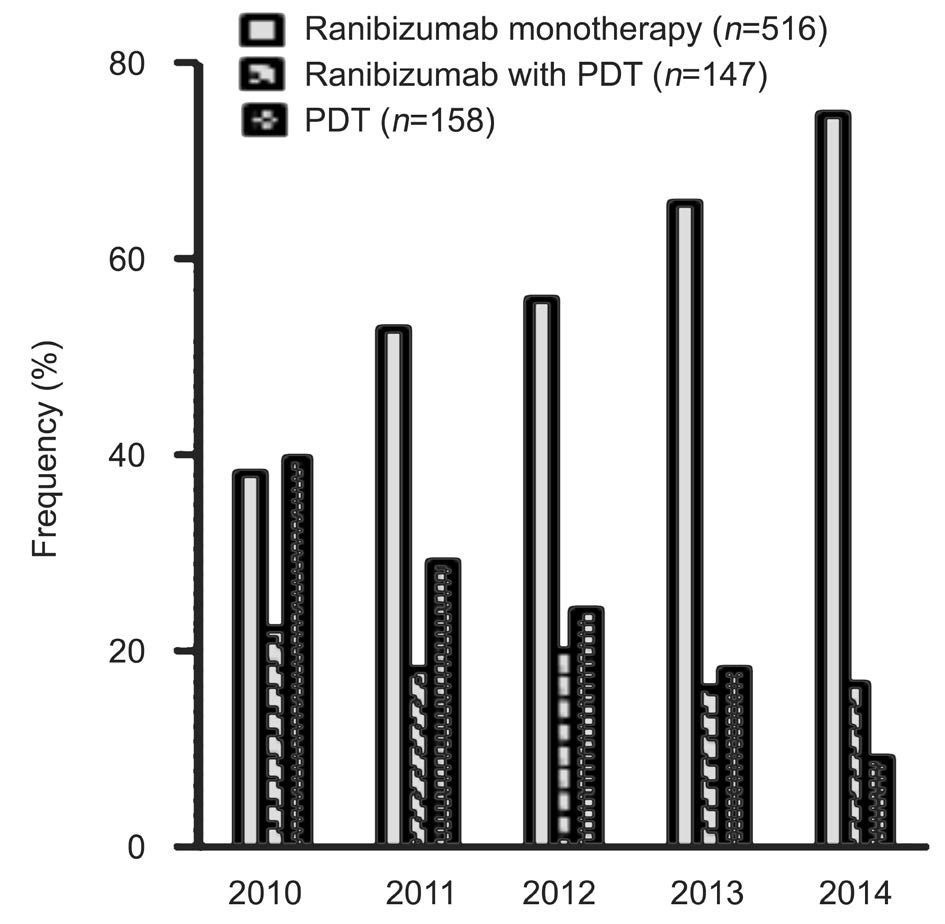
Figure 2 Trends of treatments from 2010-2014.
Overall, OCT was the most common diagnostic procedure among all the subjects with a frequency of 43.0%, followed by OCT+ICG (29.5%), OCT+FFA (14.7%) and OCT+FFA+ICG(11.6%). All of the diagnostic procedures reported a significant difference between the years recorded. The use of OCT more than doubled over the years, from 25.9% in 2010 to 54.8%in 2014. Similarly the use of OCT+ICG also doubled over this time period, from 19.0% to 28.1%. Conversely the use of OCT+FFA halved over this time period, from 27.6% in 2010 to 11.1% in 2014. Similarly, the use of OCT+FFA+ICG also halved from 19.0% to 5.9%. Overall, most patients were diagnosed with either PCV (45.6%) or AMD (25.0%),followed by DME (10.6%), advanced diabetic eye disease(ADED) (5.5%) and other retinal diseases. The number of individuals diagnosed with AMD fell by more than two-thirds,from 56.9% in 2010 to 17.4% in 2014 (P<0.001), whereas the diagnoses of PCV increased from 29.3% in 2010 to 48.1%in 2014 (P=0.022). A significant increase in trends was also observed among patients with DME (3.4% to 18.5%) and ADED (1.7% to 3.3%) across the observed time (P<0.001).Other diagnoses of patients that received ranibizumab and PDT treatments did not show any significant difference in trends from 2010 to 2014 (P>0.05).
A total of 516 ranibizumab monotherapies, 158 PDT monotherapies and 147 combinations of ranibizumab with PDT were included in this study (Figure 2). The most commonly-prescribed treatment was PDT (39.7%) in 2010,which changed over the years as ranibizumab became available in Malaysia in 2006. The use of PDT declined over the years, with only 8.9% of patients receiving this treatment in 2014. Meanwhile the use of ranibizumab was 37.9% in 2010, but 74.4% in 2014. However, the use of ranibizumab combined with PDT did not show much difference between 2010 (22.4%) and 2014 (16.7%).
As Table 2 shows, there was a significantly higher (P<0.001)mean age among subjects prescribed with ranibizumab combined with PDT treatment (69.8±8.80y) compared to those prescribed with ranibizumab monotherapy (66.2±11.04y) and PDT (61.2±14.49y). A significant difference of P<0.001 was observed among the ethnicities, whereby Chinese patientsshowed a higher frequency among all three prescribed groups of treatments (39.9% in ranibizumab, 59.9% in ranibizumab combined with PDT and 60.1% in PDT) compared to Malays and Indians. Among the co-morbidities, a significant difference was observed in hypertension with diabetes mellitus(P<0.001). Patients prescribed ranibizumab monotherapy recorded a higher frequency of hypertension with diabetesmellitus (37.2%), followed by ranibizumab combined with PDT (21.8%) and PDT (17.1%). Significant differences were also observed in the diagnostic procedures and diagnoses of patients based on different treatments prescribed to the patients. Patients prescribed with ranibizumab monotherapy had a higher frequency of undergoing OCT (P<0.001) and OCT+FFA (P<0.001) diagnostic procedures compared to the other treatment groups. Those prescribed with ranibizumab combined with PDT mostly underwent the OCT+ICG procedure (P<0.001), while PDT was higher in the OCT+FFA+ICG procedure (P=0.004). Furthermore, those receiving ranibizumab monotherapy were significantly higher among AMD patients (30.8%), DME (16.1%), ADED (8.7%),central retinal vein occlusion (CRVO) (4.8%), branch retinal vein occlusion (BRVO) (4.1%), and cystoid macular edema(CME) (2.7%). PCV patients were significantly the most prescribed with ranibizumab combined with PDT (84.4%)compared to ranibizumab monotherapy (30.6%) and PDT(58.2%) (P<0.001). Meanwhile, patients with central serous chorioretinopathy (CSCR) and choroidal hemangioma were significantly prescribed with PDT monotherapy, at frequencies of 19.0% and 7.6% respectively.
Table 2 Characteristics of patients based on treatments received n (%)
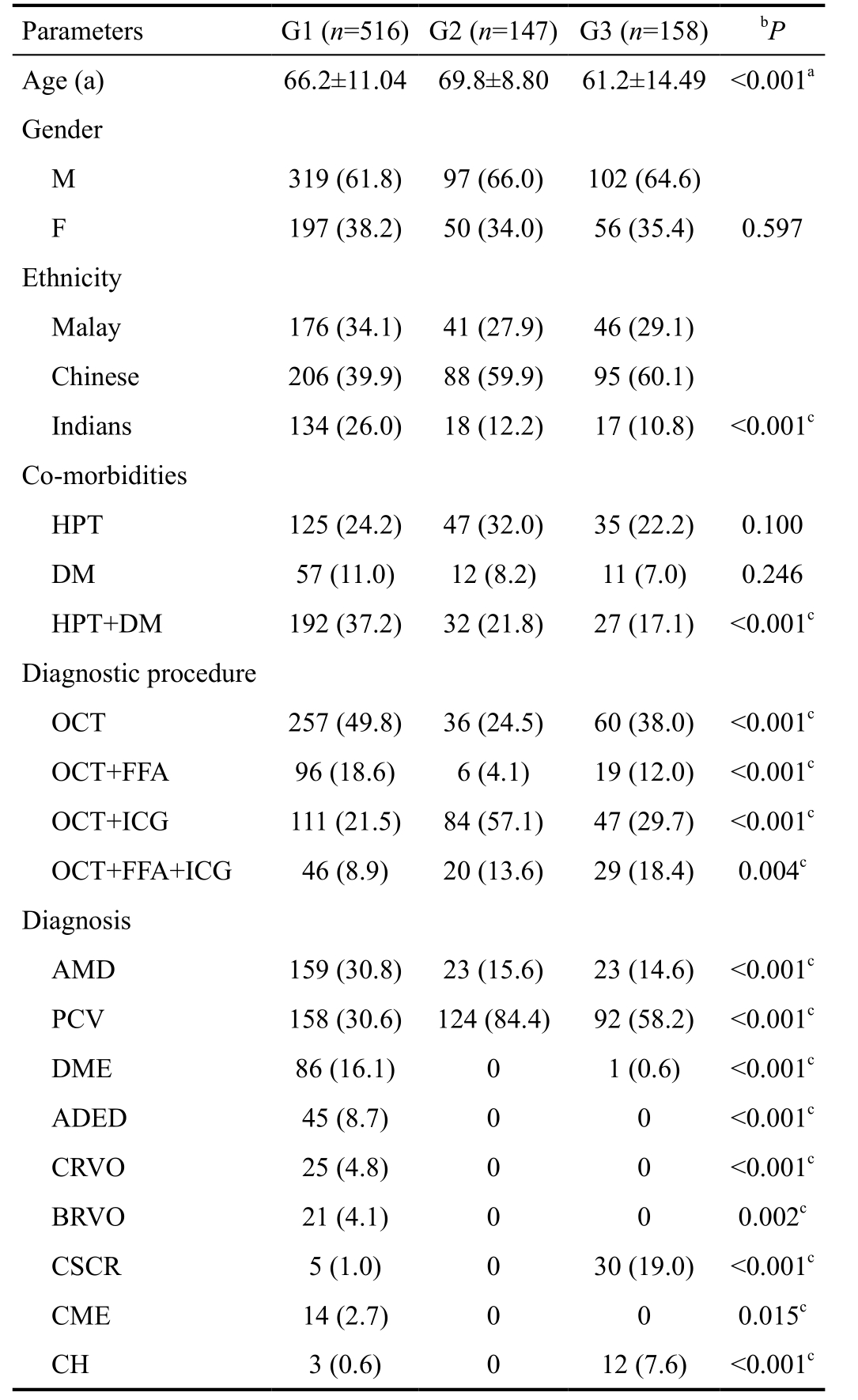
Data presented as mean±SD for age and data are reported as number of subjects with percent in parentheses, n(%). G1: Ranibizumab monotherapy; G2: Ranibizumab with PDT; G3: PDT. DM: Diabetes mellitus; HPT: Hypertension; OCT: Optical coherence tomography;FFA: Fundus fluorescein angiography; ICG: Indocyanine green;AMD: Age-related macular degeneration; PCV: Polypoidal choroidal vasculopathy; DME: Diabetic macular edema; ADED: Advanced diabetic eye disease; CRVO: Central retinal vein occlusion;BRVO: Branch retinal vein occlusion; CSCR: Central serous chorioretinopathy; CME: Cystoid macular edema; CH: Choroidal hemangioma. aAnalysis of variance, ANOVA; bChi-square test;cSignificant value, P<0.05.
Table 3 Logistic regression on parameters for each treatment
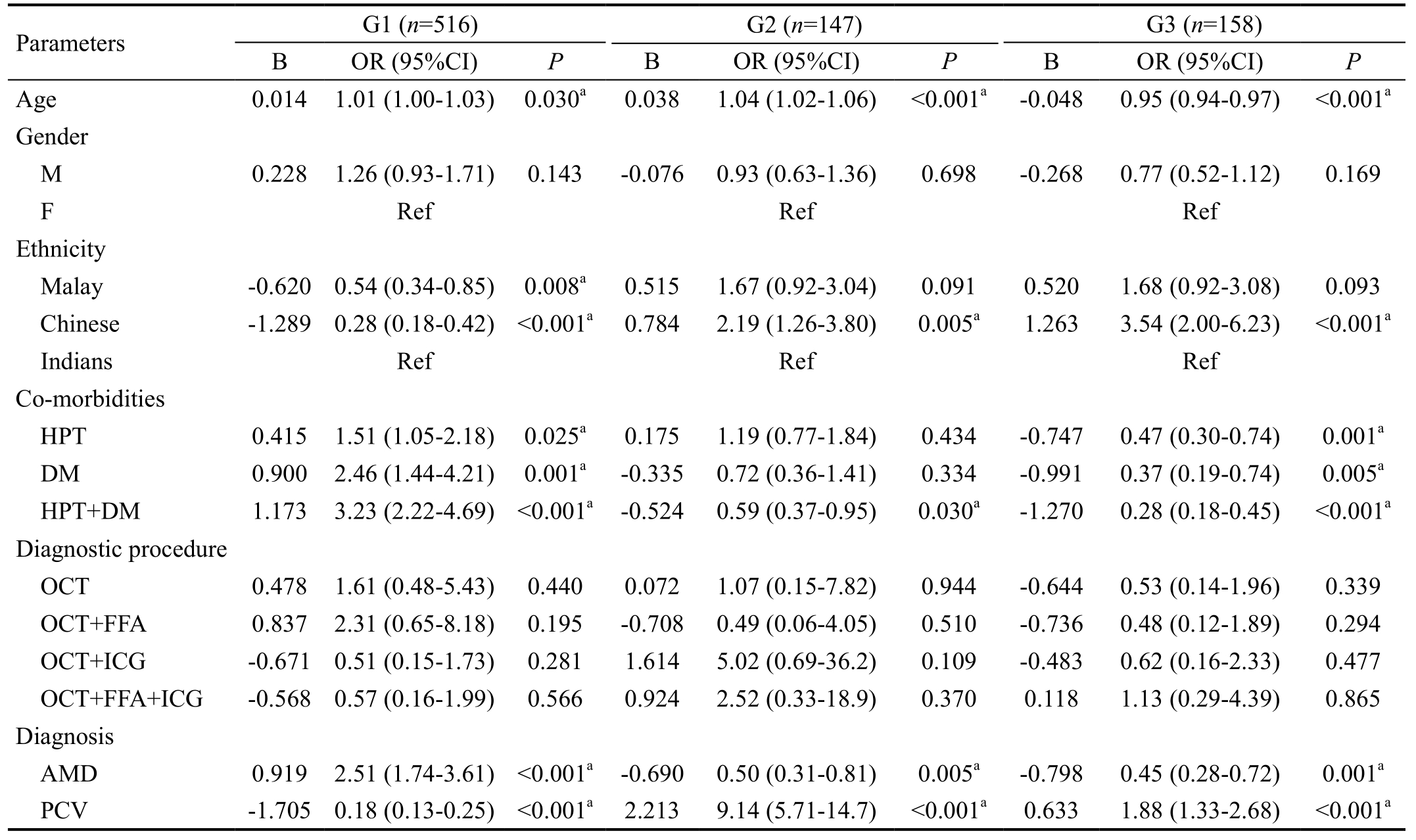
G1: Ranibizumab monotherapy; G2: Ranibizumab with PDT; G3: PDT. DM: Diabetes mellitus; HPT: Hypertension; OCT: Optical coherence tomography; FFA: Fundus fluorescein angiography; ICG: Indocyanine green; AMD: Age-related macular degeneration; PCV: Polypoidal choroidal vasculopathy; B: Coefficients for the variables; OR: Odds ratio. aSignificant value, P<0.05.
Multiple logistic regression models were performed to examine the socio-demographic factors, co-morbidities,diagnostic procedures and patient diagnoses associated with each of the treatment groups (Table 3). Among patients prescribed ranibizumab monotherapy, significant differences were observed in age and ethnicity compared to those who were not prescribed ranibizumab monotherapy. Those patients receiving ranibizumab monotherapy were at increased risk at an older age (OR=1.01, 95%CI=1.00-1.03, P=0.030), with Malays (OR=0.54, 95%CI=0.34-0.85, P=0.008) and Chinese patients (95%CI=0.28, OR=0.18-0.42, P<0.001) were at less risk of receiving the treatment than Indians. When comparing co-morbidities, patients who had hypertension with diabetes mellitus were more likely to be prescribed ranibizumab monotherapy (OR=3.23, 95%CI=2.22-4.69, P<0.001),followed by patients present with diabetes mellitus (OR=2.46,95%CI=1.44-4.21, P=0.001) and hypertension (OR=1.51,95%CI=1.05-2.18, P=0.025). Furthermore, patients diagnosed with AMD were more likely to be prescribed ranibizumab monotherapy (OR=2.51, 95%CI=1.74-3.61, P<0.001),whereas patients diagnosed with PCV were less likely to be prescribed ranibizumab monotherapy (OR=0.18, 95%CI=0.13-0.25, P<0.001).
Similarly, patients who were prescribed ranibizumab combined with PDT treatment were at an increased risk in older age(OR=1.04, 95%CI=1.02-1.06, P<0.001) as well as Chinese patients (OR=2.19, 95%CI=1.26-3.80, P=0.005). Patients who had hypertension with diabetes mellitus were reported to be less likely to receive a prescription for the combined treatment (OR=0.59, 95%CI=0.37-0.95, P=0.030) compared to those not receiving the treatment. When comparing the disease diagnoses AMD and PCV, patients with PCV(OR=9.14, 95%CI= 5.71-14.7, P<0.001) were more likely to be prescribed the combined treatment compared to patients with AMD (OR=0.50, 95%CI=0.31-0.81, P=0.005), which had fewer treatment options.
The last treatment group, PDT was reported to be received more frequently by younger patients (OR=0.95, 95%CI=0.94-0.97, P<0.001) and Chinese patients (OR=3.54, 95%CI=2.00-6.23, P<0.001). Not having hypertension, diabetes mellitus and hypertension with diabetes mellitus was associated with being prescribed PDT treatment. Similarly to those receiving combined therapy, patients with PCV (OR=1.88, 95%CI=1.33-2.68, P<0.001) were also more likely to receive PDT treatment compared to patients with AMD (OR=0.45, 95%CI=0.28-0.72,P=0.001). No significant association was observed for each diagnostic procedure in each treatment groups (P>0.05).
DISCUSSION
This retrospective study reported the current ranibizumab and PDT treatment patterns in a Malaysian tertiary care setting over a 5 year period. Hospital Selayang is a major referral point for eye diseases in Malaysia, so we reported several findings from 2010 to 2014. Since the introduction of intravitreal ranibizumab treatment, several clinical trials[19-22]have been conducted to study the effects of the treatment, and the use of ranibizumab in treating patients with AMD and other retinal diseases has increased over the years[13,23]. PDT was also reportedly effective in reducing the risk of moderate to severe vison loss, such as in subfoveal CNV due to AMD[24-26] and also in PCV[20,27]. Since these findings, researchers have studied the effects of both treatments combined and their effects in monotherapy[28-29].
The present study has shown that the number of ranibizumab and PDT prescriptions increased over the years, suggesting an increase in the number of patients with retinal diseases that require medical treatments. Both treatments displayed significantly different trends, and the use of ranibizumab increased over the years while PDT prescriptions fell. In 2010 PDT was frequently prescribed, while in 2014 ranibizumab was the most-frequently prescribed treatment. This could be because ranibizumab was only approved by the Food and Drug Administration (FDA) in 2006[30] and was phased in gradually by ophthalmologists. Since then, research has expanded from studying the efficacy and safety of anti-VEGF to investigating which anti-VEGF treatment is most efficient at improving the visual outcomes of affected patients[21-22,27,31], proving that ranibizumab has been used at an increasing rate including within the present study. The increasing trend of ranibizumab use can also be seen in the Singapore National Eye Centre from 2009 to 2012[13] and also in the United States between 2005 and 2014[10].
Unlike ranibizumab, the use of PDT monotherapy was seen to decrease in the present study. However, the combination therapy of ranibizumab and PDT displayed a similar trend over the years. Before the introduction of ranibizumab, PDT was introduced in the 1990s and was used in the treatment of CNV secondary to AMD and delaying legal blindness of patients[32].PDT was then introduced as an effective and safe treatment for subfoveal or juxtafoveal AMD and PCV, due to the minimal damage the treatment does to the retina[25-27]. However, it was observed that polypoidal lesions are highly recurrent over long periods[33], and PDT was associated with the risk of submacular hemorrhages in PCV[34]. Anti-VEGF was then introduced into the treatment of PCV[27], but was not as efficient as treating CNV in AMD[31]. The results from an ICG procedure showed a reduction in leakage but no regression in the choroidal vascular changes in PCV[35]. A revolution in combining ranibizumab and PDT treatments was thus introduced, and had positive results in reducing leakages together with inducing regression in polyps[27]. This includes the present study, as higher numbers of PCV patients were prescribed with the combination therapy (84.4%) compared to PDT (58.2%) and ranibizumab monotherapy (30.6%). Similar trends can be observed in the United States, where PDT monotherapy decreased from 12.8%in 2006 to 5.3% in 2008[9].
Apart from the trends in ranibizumab and PDT treatments, the present study also noted the different parameters associated with the prescribed treatments. Patients receiving treatments had a mean age of over 60, while the group receiving ranibizumab combined with PDT were older compared to the other two monotherapy groups. Since high levels of AMD and PCV were recorded in patients prescribed with ranibizumab and PDT, the age groups were marked high due to the fact that age is the most common risk factor for both AMD and PCV. This may merely be because of the long latent period of the disease[36]. Older patients with AMD and PCV were also reported by Krishnaiah et al[37] and Cheung et al[38].
There were significant differences among the different ethnicities. Chinese patients were the most frequent group to receive treatments in the clinic, suggesting that Chinese people have a higher incidence of retinal disease. This trend is similar to that reported by the the 4th National Eye Database in Malaysia, which found that among AMD patients in 2008 ethnically Chinese (52.1%) patients had the highest incidence, followed by Malays (33.1%) and Indians (13.6%)[39].When compared via regression analysis, Chinese people were reported to most likely to receive combination therapy and also PDT monotherapy. This could be related to the high number of PCV patients in both of these two treatment groups.Since Malaysia has a multi-ethnic population, we compared our findings with a study from a centre in Singapore. This reported that Chinese patients were alsoat a higher frequency,with 57.5%, followed by Malays (28.5%) and Indians (14.0%)among their PCV patients[40]. Another study in Singapore again with higher frequency of Chinese patients (88.2%) and 7.8%of Malays, compared to 1% of Indians[38]. Our observations that PCV may be frequent in Chinese is also supported by Wen et al[41] who reported 22.3% of 166 patients in their study were Chinese and diagnosed with PCV.
Co-morbidities of patients with hypertension and diabetes mellitus were reported to be significant in three treatment groups in the present study. Similarly, these findings are related to the risk factors of the eye diseases that require a particular treatment, in this case AMD and PCV. Hypertension and diabetes mellitus were reported to be risk factors in AMD and PCV[38,42], but not all studies reported the same associations[43-44]. Additionally, the diagnostic procedures conducted in the clinic were consistent with procedures to detect retinal diseases. OCT was also reported to be a good diagnostic tool in detecting classic CNV for newly-diagnosed patients. However, in differentiating classic CNV from occult CNV, FFA is considered to be an accurate diagnostic procedure[45-46]. This is reflected in the regression analysis findings from the present study, as OCT and FFA procedures were highest among AMD patients receiving ranibizumab monotherapy. Meanwhile, ICG procedures were frequent among those receiving the combination therapy and PDT,which is a treatment most frequently prescribed for PCV patients. ICG was shown to be more sensitive at detecting polypoidal dilation in the choroidal vascular network of PCV when compared to FFA, which may appear as occult CNV[47-48].Furthermore, findings from the present study are consistent with the types of treatments most commonly prescribed amongst AMD and PCV patients. In the clinic studied,AMD patients were being prescribed with ranibizumab monotherapy, as anti-VEGF agents give better results when treating such individuals. Rosenfeld et al[1] reported that intravitreal administration of ranibizumab prevents vision loss and improves visual acuity in AMD patients. Similarly,in Japan, Matsumiya et al[31] reported ranibizumab resulted in better visual outcomes among AMD patients compared to PCV patients. PDT monotherapy and ranibizumab combined with PDT was more commonly prescribed to PCV patients in the present study, as PDT is considered more efficacious at treating PCV patients compared to AMD, similar to the findings several studies[49-51]. Tomita et al[52] reported that when PDT is combined with ranibizumab therapy, the polypoidal lesions among PCV patients disappeared completely in 79.1%of cases, with a substantial reduction in exudative change[52].Wong et al[53] reported that when PDT was combined with ranibizumab, polyp regression or disease activity resolution was observed for at least nine months after treatment, but only in PCV patients who had a single small polyp. This supports the reason ranibizumab combined with PDT was frequently prescribed to PCV patients in this study.
In the present study, administration of ranibizumab and PDT was also prescribed to patients with other retinal diseases. The use of ranibizumab and PDT is recognized in the management of AMD and PCV. Meanwhile, the efficacy and safety of ranibizumab conducted by many clinical studies which observed the improvement in best corrected visual acuity(BCVA) of patients, meant it was also suggested for macular edema patients following retinal vein occlusions[54-56] and diabetic eye diseases[3,57]. CSCR and choroidal hemangioma patients were also observed to receive the ranibizumab treatment. However, they are more commonly prescribed with the PDT monotherapy. Erikitola et al[58] observed changes in the BCVA, OCT and FFA of CSCR patients treated with PDT, and suggested it was a useful treatment. This supports a study on choroidal hemangioma that reported an improvement in BCVA and the elimination of subretinal fluid in choroidal hemangioma patients treated with PDT monotherapy[59]. All these findings are in accordance with the use of ranibizumab and PDT in the present study.
In conclusion, we reported the patterns of ranibizumab and PDT treatment in a Malaysian population at a tertiary care setting. To our knowledge, this is the first comprehensive report on patterns of ranibizumab and PDT treatment from Malaysia. However, the present study has to be interpreted within the context of its limitations. Our study focused only on the prevalence of patterns of treatment in a single tertiary centre without following up patients in their response to the given treatment. The study’s retrospective nature and small sample size are also limitations. Moreover, the findings reported in this paper were recorded between 2010 and 2014.The prevalence of retinal diseases is expected to increase in future. The data thus needs to be updated further on the patterns of treatment, and the prevalence is needed in order to establish our findings for public health education and the prevention of retinal diseases.
ACKNOWLEDGEMENTS
The authors would like to extend their gratitude to Hospital Selayang and all the volunteers involved in this study.
Foundations: Supported by Putra Grant from Universiti Putra Malaysia (No.9409800; No.9432700).
Conflicts of Interest: Mohamad NA, None; Ramachandran V, None; Ismail P, None; Mohd Isa H, None; Chan YM,None; Ngah NF, None; Md Bakri N, None; Ching SM,None; Hoo FK, None; Wan Sulaiman WA, None.
REFERENCES
1 Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY,Kim RY; MARINA Study Group. Ranibizumab for neovascular agerelated macular degeneration. N Engl J Med 2006;355(14):1419-1431.
2 Wong TY, Liew G, Mitchell P. Clinical update: new treatments for agerelated macular degeneration. Lancet 2007;370(9583):204-206.
3 Nguyen QD, Brown DM, Marcus DM, Boyer DS, Patel S, Feiner L, Gibson A, Sy J, Rundle AC, Hopkins JJ, Rubio RG, Ehrlich JS.Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology 2012;119(4):789-801.
4 Ip MS, Domalpally A, Sun JK, Ehrlich JS. Long-term effects of therapy with ranibizumab on diabetic retinopathy severity and baseline risk factors for worsening retinopathy. Ophthalmology 2015;122(2):367-374.
5 Treatment of age-related macular degeneration with photodynamic therapy (TAP) Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: one-year results of 2 randomized clinical trials-TAP report.Arch Ophthalmol 1999;117(10):1329-1345.
6 Verteporfin in Photodynamic Therapy Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in pathologic myopia with verteporfin. 1-year results of a randomized clinical trial-VIP report no.1. Ophthalmology 2001;108(5):841-852.
7 Rosenfeld PJ, Saperstein DA, Bressler NM, Reaves TA, Sickenberg M,Rosa RH Jr, Sternberg P Jr, Aaberg TM Sr, Aaberg TM Jr. Photodynamic therapy with verteporfin in ocular histoplasmosis: uncontrolled, openlabel 2-year study. Ophthalmology 2004;111(9):1725-1733.
8 Koh A, Lim TH, Au Eong KG, Chee C, Ong SG, Tan N, Yeo I, Wong D. Optimising the management of choroidal neovascularisation in Asian patients: consensus on treatment recommendations for anti-VEGF therapy. Singapore Med J 2011;52(4):232-240.
9 Curtis LH, Hammill BG, Qualls LG, DiMartino LD, Wang F, Schulman KA, Cousins SW. Treatment patterns for neovascular age-related macular degeneration: analysis of 284 380 medicare beneficiaries. Am J Ophthalmol 2012;153(6):1116-1124.e1.
10 Parikh R, Ross JS, Sangaralingham LR, Adelman RA, Shah ND,Barkmeier AJ. Trends of anti-vascular endothelial growth factor use in ophthalmology among privately insured and medicare advantage patients.Ophthalmology 2017;124(3):352-358.
11 Ergun E, Zawinka C, Stur M. Incidence of laser photocoagulation and photodynamic therapy with verteporfin at a tertiary retinal center. Retina 2004;24(1):13-18.
12 Lad EM, Hammill BG, Qualls LG, Wang F, Cousins SW, Curtis LH. Anti-VEGF treatment patterns for neovascular age-related macular degeneration among medicare beneficiaries. Am J Ophthalmol 2014;158(3):537-543.e2.
13 Ng WY, Cheung CM, Mathur R, Chan CM, Yeo IY, Wong E, Lee SY,Loh BK, Wong D, Wong TY. Trends in age-related macular degeneration management in Singapore. Optom Vis Sci 2014;91(8):872-877.
14 Teo KY, Cheung GC, Lee SY, Koh AC, Ong SG, Wong TY. Evolving practice patterns in treatment of major retinal diseases in Singapore. Ann Acad Med Singap 2014;43(3):192-194.
15 Chan WM, Lai TY. Age-related macular degeneration and polypoidal choroidal vasculopathy in Asia. Hong Kong J Ophthalmol 2016;14(1):14-19.
16 Cheng CY, Yamashiro K, Chen LJ, et al. New loci and coding variants confer risk for age-related macular degeneration in East Asians. Nat Commun 2015;6:6063.
17 Lee JY, Moon BG, Kim M, Lee JE, Park KH, Kim SD. Results of the 2015 questionnaire survey of the korean retina society: current trends in the treatment of vitreoretinal diseases. J Korean Ophthalmol Soc 2016;57(7):1071-1079.
18 Cheung CM, Li X, Mathur R, Lee SY, Chan CM, Yeo I, Loh BK, Williams R, Wong EY, Wong D, Wong TY. A prospective study of treatment patterns and 1-year outcome of Asian age-related macular degeneration and polypoidal choroidal vasculopathy. PLoS One 2014;9(6):e101057.
19 Johnston SS, Wilson K, Huang A, Smith D, Varker H, Turpcu A.Retrospective analysis of first-line anti-vascular endothelial growth factor treatment patterns in wet age-related macular degeneration. Adv Ther 2013;30(12):1111-1127.
20 Oishi A, Kojima H, Mandai M, Honda S, Matsuoka T, Oh H, Kita M,Nagai T, Fujihara M, Bessho N. Comparison of the effect of ranibizumab and verteporfin for polypoidal choroidal vasculopathy: 12-month LAPTOP study results. Am J Ophthalmol 2013;156(4):644-651.e1.
21 Martin DF, Maguire MG, Fine SL, Ying GS, Jaffe GJ, Grunwald JE,Toth C, Redford M, Ferris FL; Group CoA-rMDTTR. Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: two-year results. Ophthalmology 2012;119(7):1388-1398.
22 Mitchell P, Korobelnik JF, Lanzetta P, Holz FG, Pruente C, Schmidt-Erfurth UM, Tano Y, Wolf S. Ranibizumab (Lucentis) in neovascular age-related macular degeneration: evidence from clinical trials. Br J Ophthalmol 2010;94:2-13.
23 Keenan TD, Wotton CJ, Goldacre MJ. Trends over time and geographical variation in rates of intravitreal injections in England. Br J Ophthalmol 2011;96(3):413-418.
24 Brown DM, Michels M, Kaiser PK, Heier JS, Sy JP, Ianchulev T.Ranibizumab versus verteporfin photodynamic therapy for neovascular age-related macular degeneration: two-year results of the ANCHOR study. Ophthalmology 2009;116(1):57-65.e5.
25 Bressler NM; Treatment of Age-Related Macular Degeneration with Photodynamic Therapy (TAP) Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: two-year results of 2 randomized clinical trials-tap report 2. Arch Ophthalmol 2001;119(2):198-207.
26 Azab M, Boyer DS, Bressler NM, Bressler SB, Cihelkova I, Hao Y,Immonen I, Lim JI, Menchini U, Naor J, Potter MJ, Reaves A, Rosenfeld PJ, Slakter JS, Soucek P, Strong HA, Wenkstern A, Su XY, Yang YC;Visudyne in Minimally Classic Choroidal Neovascularization Study Group. Verteporfin therapy of subfoveal minimally classic choroidal neovascularization in age-related macular degeneration: 2-year results of a randomized clinical trial. Arch Ophthalmol 2005;123(4):448-457.
27 Koh A, Lee WK, Chen LJ, Chen SJ, Hashad Y, Kim H, Lai TY, Pilz S,Ruamviboonsuk P, Tokaji E, Weisberger A, Lim TH. EVEREST study:efficacy and safety of verteporfin photodynamic therapy in combination with ranibizumab or alone versus ranibizumab monotherapy in patients with symptomatic macular polypoidal choroidal vasculopathy. Retina 2012;32(8):1453-1464.
28 Bradley J, Ju M, Robinson GS. Combination therapy for the treatment of ocular neovascularization. Angiogenesis 2007;10(2):141-148.
29 Krebs I, Vecsei Marlovits V, Bodenstorfer J, Glittenberg C, Ansari Shahrezaei S, Ristl R, Binder S. Comparison of Ranibizumab monotherapy versus combination of Ranibizumab with photodynamic therapy with neovascular age-related macular degeneration. Acta Ophthalmol 2013;91(3):e178-e183.
30 Lloyd R, Harris J, Wadhwa S, Chambers W. Food and Drug Administration approval process for ophthalmic drugs in the US. Curr Opin Ophthalmol 2008;19(3):190-194.
31 Matsumiya W, Honda S, Kusuhara S, Tsukahara Y, Negi A.Effectiveness of intravitreal ranibizumab in exudative age-related macular degeneration (AMD): comparison between typical neovascular AMD and polypoidal choroidal vasculopathy over a 1 year follow-up. BMC Ophthalmol 2013;13:10.
32 Schmidt-Erfurth U, Miller J, Sickenberg M, Bunse A, Laqua H,Gragoudas E, Zografos L, Birngruber R, van den Bergh H, Strong A,Manjuris U, Fsadni M, Lane AM, Piguet B, Bressler NM. Photodynamic therapy of subfoveal choroidal neovascularization: clinical and angiographic examples. Graefes Arch Clin Exp Ophthalmol 1998;236(5):365-374.
33 Leal S, Silva R, Figueira J, Cachulo ML, Pires I, de Abreu JR, Cunha-Vaz JG. Photodynamic therapy with verteporfin in polypoidal choroidal vasculopathy: results after 3 years of follow-up. Retina 2010;30(8):1197-1205.
34 Ojima Y, Tsujikawa A, Otani A, Hirami Y, Aikawa H, Yoshimura N.Recurrent bleeding after photodynamic therapy in polypoidal choroidal vasculopathy. Am J Ophthalmol 2006;141(5):958-960.
35 Kokame GT, Yeung L, Teramoto K, Lai JC, Wee R. Polypoidal choroidal vasculopathy exudation and hemorrhage: results of monthly ranibizumab therapy at one year. Ophthalmologica 2013;231(2):94-102.
36 Wong CW, Wong TY, Cheung CM. Polypoidal choroidal vasculopathy in Asians. J Clin Med 2015;4(5):782-821.
37 Krishnaiah S, Das T, Nirmalan PK, Nutheti R, Shamanna BR, Rao GN, Thomas R. Risk factors for age-related macular degeneration:findings from the Andhra Pradesh eye disease study in South India. Invest Ophthalmol Vis Sci 2005;46(12):4442-4449.
38 Cheung CM, Li X, Cheng CY, Zheng Y, Mitchell P, Wang JJ,Wong TY. Prevalence, racial variations, and risk factors of age-related macular degeneration in Singaporean Chinese, Indians, and Malays.Ophthalmology 2014;121(8):1598-1603.
39 Mohamad AZ, Goh PP. Fourth Report of the National Eye Database 2010, Kuala Lumpur 2012. National eye database (NED). http://acrm.org.my/ned. Accessed on 13th December, 2016.
40 Cheung CM, Tai ES, Kawasaki R, Tay WT, Lee JL, Hamzah H, Wong TY. Prevalence of and risk factors for age-related macular degeneration in a multiethnic Asian cohort. Arch Ophthalmol 2012;130(4):480-486.
41 Wen F, Chen C, Wu D, Li H. Polypoidal choroidal vasculopathy in elderly Chinese patients. Graefes Arch Clin Exp Ophthalmol 2004;242(8):625-629.
42 Woo SJ, Ahn J, Morrison MA, Ahn SY, Lee J, Kim KW, DeAngelis MM, Park KH. Analysis of genetic and environmental risk factors and their interactions in korean patients with age-related macular degeneration.PLoS One 2015;10(7):e0132771.
43 Sakurada Y, Yoneyama S, Imasawa M, Iijima H. Systemic risk factors associated with polypoidal choroidal vasculopathy and neovascular agerelated macular degeneration. Retina 2013;33(4):841-845.
44 Ueta T, Obata R, Inoue Y, Iriyama A, Takahashi H, Yamaguchi T,Tamaki Y, Yanagi Y. Background comparison of typical age-related macular degeneration and polypoidal choroidal vasculopathy in Japanese patients. Ophthalmology 2009;116(12):2400-2406.
45 Coscas F, Coscas G, Souied E, Tick S, Soubrane G. Optical coherence tomography identification of occult choroidal neovascularization in agerelated macular degeneration. Am J Ophthalmol 2007;144(4):592-599.
46 Sandhu SS, Talks SJ. Correlation of optical coherence tomography,with or without additional colour fundus photography, with stereo fundus fluorescein angiography in diagnosing choroidal neovascular membranes.Br J Ophthalmol 2005;89(8):967-970.
47 Silva RM, Figueira J, Cachulo ML, Duarte L, Faria de Abreu JR,Cunha-Vaz JG. Polypoidal choroidal vasculopathy and photodynamic therapy with verteporfin. Graefes Arch Clin Exp Ophthalmol 2005;243(10):973-979.
48 Spaide RF, Yannuzzi LA, Slakter JS, Sorenson J, Orlach DA.Indocyanine green videoangiography of idiopathic polypoidal choroidal vasculopathy. Retina 1995;15(2):100-110.
49 Gomi F, Ohji M, Sayanagi K, Sawa M, Sakaguchi H, Oshima Y, Ikuno Y, Tano Y. One-year outcomes of photodynamic therapy in age-related macular degeneration and polypoidal choroidal vasculopathy in Japanese patients. Ophthalmology 2008;115(1):141-146.
50 Honda S, Kurimoto Y, Kagotani Y, Yamamoto H, Takagi H, Uenishi M. Photodynamic therapy for typical age-related macular degeneration and polypoidal choroidal vasculopathy: a 30-month multicenter study in Hyogo, Japan. Jpn J Ophthalmol 2009;53(6):593-597.
51 Kang HM, Kim YM, Koh HJ. Five-year follow-up results of photodynamic therapy for polypoidal choroidal vasculopathy. Am J Ophthalmol 2013;155(3):438-447.e1.
52 Tomita K, Tsujikawa A, Yamashiro K, Ooto S, Tamura H, Otani A, Nakayama Y, Yoshimura N. Treatment of polypoidal choroidal vasculopathy with photodynamic therapy combined with intravitreal injections of ranibizumab. Am J Ophthalmol 2012;153(1):68-80.e1.
53 Wong IY, Shi X, Gangwani R, Zhao P, Iu LP, Li Q, Ng A, Li X. 1-year results of combined half-dose photodynamic therapy and ranibizumab for polypoidal choroidal vasculopathy. BMC Ophthalmol 2015;15:66.
54 Campochiaro PA, Heier JS, Feiner L, Gray S, Saroj N, Rundle AC,Murahashi WY, Rubio RG; BRAVO Investigators. Ranibizumab for macular edema following branch retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology 2010;117(6):1102-1112.e1.
55 Heier JS, Campochiaro PA, Yau L, Li Z, Saroj N, Rubio RG, Lai P.Ranibizumab for macular edema due to retinal vein occlusions: long-term follow-up in the HORIZON trial. Ophthalmology 2012;119(4):802-809.
56 Brown DM, Campochiaro PA, Singh RP, Li Z, Gray S, Saroj N, Rundle AC, Rubio RG, Murahashi WY; CRUISE Investigators.Ranibizumab for macular edema following central retinal vein occlusion:six-month primary end point results of a phase III study. Ophthalmology 2010;117(6):1124-1133.e1.
57 Salam A, Mathew R, Sivaprasad S. Treatment of proliferative diabetic retinopathy with anti-VEGF agents. Acta Ophthalmol 2011;89(5):405-411.
58 Erikitola OC, Crosby-Nwaobi R, Lotery AJ, Sivaprasad S.Photodynamic therapy for central serous chorioretinopathy. Eye(Lond)2014;28(8):944-957.
59 Madreperla SA. Choroidal hemangioma treated with photodynamic therapy using verteporfin. Arch Ophthalmol 2001;119(11):1606-1610.