INTRODUCTION
The Right To Sight is the global initiative program launched by WHO to eliminate avoidable blindness by 2020; hence it is called VISION 2020. Telemedicine is a connection between medicine and available technology.It transfers medical information through the virtual world.Telemedicine is not just a research tool but has been evolved into a clinical service, especially in underserved areas[1].
Reviewing the literature demonstrates that this technique has been successfully used in ophthalmology and established a connection between specialists and people in remote locations[2-5]. American Telemedicine Association (ATA)set required standards for teleophthalmology to improve healthcare delivery through telecommunication[6]. The majority of suggested models in this field were focused on patient screening, appropriate referral to experts, and efficient follow-up systems[7]. Bursell et al[6] reported that this innovative method could provide equal satisfaction compared with the conventional method, probably due to increased accessibility, saving cost and time, and minimize hospital visits. Also, Ribeiro et al[8] showed that teleophthalmology has an important role in emergency eye care services in rural areas with sensitivity and specificity of 93% and 82%,respectively. Smartphones are coming inseparable part of the daily life with high penetration rate all around the world. The International Telecommunication Union reported that 95.5 percent of the global population are mobile subscribers in 2014 with a mobile-broadband penetration rate of 84% and 21% in developed and developing countries, respectively[9].
It is interesting that developed areas had much more growth than developing areas in an overall number of active mobilebroadband subscriptions (reaching from 20% in 2008 to 55%in 2014)[9]. Smartphones can be handy in fulfilling the goals of the project; By taking high-resolution photos and sending them to an expert for interpretation. Thus, not only diagnosis and treatment become easier, but it also saves money and time. On the other hand, by using appropriate mobile apps,patients can do self-testing and seek treatment, long before the disease occurs or proceeds. In this way, teleophthalmology with the aid of smartphones can prevent diseases causing blindness. Considering its ease of accessibility and its potential for utilization of highly innovative applications, it could be a promising device for teleophthalmology. Here, we demonstrated the use of smartphones in teleophthalmology and its utility in fulfilling the VISION 2020 project.
Smartphone as an Essential Instrument The primary tool for every ophthalmologist would be definitely, a slit lamp biomicroscope. It is not only used for examination, but also photo-documentation can be done through equipped devices.However, in remote areas and developing countries where ophthalmologist access is limited and even slit lamp may not be available, teleophthalmology can be helpful[10-11]. Previously,we reported the use of an iPhone 6 with iOS operating system smartphone with additional lenses for anterior segment imaging. We found that the application of standard macro lens 90 diopters on smartphones provides more precise images of the cornea and anterior segment than the one without macro lens[12]. Figure 1 shows different types of images that were captured by smartphone (iPhone 6). Peek@[10] is another kind of smartphone ophthalmoscope which can capture a clear retinal image with the portable kit. In general, any smartphone with the high-resolution camera if used with an appropriate accessory, can provide us with clear images of different components of the eye even without mydriasis; the images may be sent to research centers or specialists via email or networks instead of face to face examination[13].
VISION 2020
In 1999, the World Health Organization (WHO) launched a global initiative called VISION 2020, that aimed elimination of avoidable causes of blindness by 2020 through disease control and treatment, human resource development, developing appropriate infrastructure and technology development[14-15].Foster and Resnikoff[15] in 2005 worked on the subject and mentioned four main strategies; creating general awareness,providing new sources for the development of eye care service along with the efficient use of existing sources,sustainable and equitable eye care services at the district level,and prioritizing avoidable causes of blindness and existing resources. Communication technologies not only provide masses of professional, public, and political awareness but also has the potential of being a new source of eye care services.Indeed, the ability of documentation (by imaging or recording a movie), transferring the data to where ever you want, and even automatic analysis of the data brought these technologies into focus, commonly known as teleophthalmology.

Figure 1 Different types of images were captured by smartphone(iPhone 6) A: Cataract; B: Retinal detachment; C: IOL implantation;D: Diabetic retinopathy; E: Ocular surface.
Later in 2015, project goal was redefined for the last five years of the project; 25% reduction in visual impairment and avoidable blindness by 2019 from 2010 baseline[16]. In 2010,the most prevalent causes were refractive error and cataract with estimation of 75% of all visual impairments around the world[17]. Glaucoma, age-related macular degeneration(ARMD), trachoma, diabetic retinopathy (DR) and childhood problems such as retinopathy of prematurity (ROP) were in next places[17]. Inspiring the new technologies and their application in our traditional ophthalmology practice seems to be promising in eye health system development. In Africa,Cook et al[18] reported that teleophthalmology was promising in diagnosis and treatment of eye diseases and emphasized its role in VISION 2020. This study demonstrated improvement in both visual health and quality of life[18]. Similar results were reported by John et al[19] in India, Ng et al[20] in Canada, and many other authors around the world[21]. Beneficial use of teleophthalmology through smartphones also would be useful in achieving the aim of VISION 2020[22].
SMARTPHONE IN CATARACT
Cataract is a senile process leading to the clouding of the natural lens and decreased vision by reducing the amount of light reaching to the retina. By the WHO reports, 50% of visual impairment in the world occurs due to the cataract. If doing without any intervention, the number of blind persons would be doubled in 2020[14]. The most common underlying etiology is aging, and most involved people would be more than 50 years old; from these patients, 75% could be prevented and treated appropriately[23]. These patients usually are aware of their decreased vision[24]. Congenital cataract is one of the causes of visual impairment in children; 1.4 million children under 15 are blind while 50% of them could be prevented by early detection of disease and proper treatment of congenital abnormalities[23]. In advanced stages of a cataract, surgery becomes more difficult with higher complication rate and higher cost[25]. Here, the key point is early detection of cataract by regular screening[24].
In underserved areas, the cost of imaging with a retinal camera or slit photography is high. Also, these devices are not portable and easy to use for an inexperienced person,but the use of smartphones (iOS or Android based) and their easy-to-use interfaces would save time and cost[24,26].Cell Scope[27-28], Eye Go[29], D eye[30] and Peek[31] are various devices that were reported for imaging of the eye. Peek is much more developed and can be used to perform a cataract test directly on a smartphone[32-33]. Besides that, the severity of the disease could be estimated by red reflex; the patient would be in a dark room and after natural mydriasis, the image will be shot by a camera flash which would be similar to the ophthalmoscopy[34]. Any opacity in the optical pathway leads to the abnormal red reflex[35]. This is a portable method for cataract screening in rural and limited access areas.Sanguansak et al[36] studied in postoperative cataract patients with different smartphone adaptors. Images were taken from the anterior corneal surface; 86%-100% of images were readable, and the quality was accepted in 93%-100% of cases by an expert.
SMARTPHONE IN GLAUCOMA
Increased intraocular pressure (IOP) would damage eye’s optic nerve and leads to cup formation. Glaucoma results in irreversible visual loss and the estimated prevalence are 60.5 million people around the world[37]. The estimated number of glaucoma patients in 2020 will be about 80 million, accounting for 12% of blindness all over the world[38]. The major challenge in glaucoma is that more than 50 percent of people are unaware of their disease, especially in developing populations, until the disease progresses and visual impairment occurs[30,37]. The resultant visual impairment affects patient’s life style, walking,driving, reading and social relationships[39-40]. Early diagnosis through accurate screening in high-risk populations is critical to prevent loss of vision associated with glaucoma. The screening seems to be more important in countries with limited health services like in Africa or countries with significant rural areas like India or China[38]. Considering the increasing availability of smartphones and internet around the world and their ease of access, It seems that tele-glaucoma by use of these devices would be a promising method for screening, diagnosis and follow up of patients with glaucoma.
The free Wills Eye Glaucoma Application available on Apple store smartphones includes educational materials about glaucoma, useful for patients and healthcare providers.Regarding examination, IOP is an essential part of the examination, particularly in glaucoma. Araci et al[41] applied implantable sensor to the smartphone and suggested that patients themselves could measure IOP even in their home,providing an automated 24h ambulatory recording of IOP;this design has the potential to be developed in the future for monitoring the IOP by health care providers. Another essential part of the glaucomatous patient assessment is retinoscopy for cup/disc ratio. Adding some accessories to the smartphones will be useful on image detail; Russo et al[42] attached a D-EYE adaptor to an iPhone 5s (App Inc., USA) which reduces the reflection and improves the picture quality. They reported that imaging with smartphones in the proper setting is almost equivalent to gold standard slit lamp biomicroscopy in the evaluation of cup/disc ratio[42]. However, the use of smartphones has been limited to media opacities, high level of refractive errors and patients with poor cooperation. A study by the University of Alberta reported that 24% of images in teleglaucoma method were unreadable[43]. Teleophthalmology can be recruited in remote and underserved communities or even in-house patients for screening, managing, and monitoring of glaucoma. Not only it reduces the number of false-positive referrals to an ophthalmologist, but also saves cost and time for patient and health system[44-45]. In a Meta-analysis of 1123 studies, Thomas et al[46] found that teleglucoma was more specific (79%) and less sensitive (83%) than regular examination. So it could be a useful tool for glaucoma screening.
SMARTPHONE IN VITREORETINAL DISEASES
Age-related Macular Degeneration Age-related macular degeneration (ARMD) occurs with aging. Oxidative stresses and inflammatory processes during the lifetime are accused of being the underlying etiologies. It is estimated that in 2010,2.85 millions of people blinded because of ARMD[17]. Early detection and regular follow-up of the disease have significant roles in preventing blindness. Screening of populations at risk for ARMD with positive family history or other risk factors through telemedicine would be great helpful[47-49].Some studies stated that recognition of the ARMD is possible through none mydriatic fundus camera[47]. Also, it seems that structural images based on OCT method in teleophthalmology would be useful in the prompt diagnosis of ARMD[50].With the progression of ARMD, blindness may occur due to choroidal neovascularization (CNV). Early detection of CNV by checking visual acuity with smartphones would be helpful in preventing permanent visual loss[51-52]. Also, some studies suggested home-monitoring (The ForseeHOME AMD Monitoring program) which recently approved by FDA for detecting moderate ARMD; this method is based on hyperacuity and may be useful in early detection of ARMD progression when visual acuity is still good[53-54]. Evaluation of digital retinal images in the diagnosis of neovascular AMD in comparison with specialists’ diagnosis showed high sensitivity (95%) and specificity (90%)[55]. Smartphones are available everywhere and are great tools for monitoring patients with AMD. Patients can do self-testing by using Shape-discrimination hyperacuity (SDH) and MultiBit Test(MBT). By using SDH test, Wang et al[56] found that test results were higher in patients with more advanced AMD. Also,Winther et al[57] showed comparable results with clinical tests by using MBT test in 28 patients with neovascularized AMD.Advancement in developing self-testing apps is promising for early diagnosis of CNV in AMD patients.
Diabetic Retinopathy WHO estimated that 440 million people would have diabetes in 2030 with the prevalence of 70% and 20% in developing and developed countries,respectively[58]. DR is one of the leading causes of visual impairment around the world that if be diagnosed and managed in the early stages, the risk of vision loss will be considerably reduced[59]. High blood sugar levels cause damage to the retinal blood vessel and subsequent ischemia with compensatory neovascularization[60]. The ophthalmic examination timing in diabetic patients with type 1 and type 2 varies; the screening in type 1 should be done five years after initial diagnosis,followed by annual examination while in type 2, the screening should be started immediately after diagnosis and then repeated annually[21]. In a vast country such as India, 80 million patients have diabetes mellitus from whom 23 million are at increased risk of DR[2]. On the other side, 39% of Indians live in rural areas while 70% of people have access to mobile[2].Hence, telemedicine with smartphones would be a promising method to provide proper eye health care. In Early Treatment Diabetic Retinopathy Study (ETDRS), the gold standard for screening DR was defined as 30 degrees 7-field stereo color 35 mm slides and slit lamp biomicroscopy with sensitivity and specificity of 95% and 88%, respectively[61-63]. However,digital photography camera was introduced as a useful tool for screening DR; Tele-retina is considered as a screening of patients’ retina by the digital retinal camera with mydriatic or none mydriatic pupil, capturing images by non-specialist in remote areas and finally transferring to the ophthalmic center for evaluation by an expert ophthalmologist[6,62,64]. In this method, the quality of images varies with camera resolution and mydriatic or nonmydriatic approaches[65]. Indeed, it can be said that the concept of retinal triage is going to be run but must be carefully done under surveillance. Maberley et al[66]studied the reliability of retinal photography in comparison with conventional physical examination and showed that this method was 95% sensitive. By using a module designed by the Joslin Vision Network system, Whited et al[67] reported high reliability of the method in the diagnosis of diabetic retinopathy. Also, Sensitivity analysis on data value and assessment of the power of retinal photography showed that in comparison with the usual approach, retinal photography is more cost-effective, both for patients and clinical centers[67].
Since diabetes is a chronic disease, it requires regular follow up while studies reported that 35% to 80% of diabetic patients don’t follow eye care recommendations[68-69]. Here,smartphones can play a significant role[70-71]. Smartphone ophthalmoscopy can be performed with D-Eye device (easy to use) or high image quality fundus camera which is in consistent with retinal biomicroscopy[72]. Silva et al[73] reported that with teleophthalmology, annual ophthalmic examinations increased from 50% to 70% in diabetic patients, meaning that after reduction in cost and time, patients’ cooperativity increased.Now considering smartphone utilization and more saving of cost and time, regular follow up and increased examinations would be expected which can be beneficial in the prevention of visual loss by DR through timely detection of pathology and proper referral to an ophthalmologist for management[73].
Retinopathy of Prematurity ROP is a retinal disease in which normal growth of blood vessels is interrupted and is associated with high level of additional oxygen in newborn baby; if left untreated, would cause childhood blindness[74-75]. Its incidence has been increased in recent decades as a result of neonatal intensive care unit (NICU) establishment and prematurity care[21]. The disease occurs mostly in premature infants with birth weights of <2000 gram[76]. A total of 12 million premature children have been born in the world annually with ROP incidence of 15%-30% among these[77-78], while based on American Academy of Ophthalmology data only 54% of ophthalmologists tend to screen for ROP[79-80].
Telemedicine with the use of high-resolution camera can be utilized to diagnose ROP instead of the traditional method with binocular indirect ophthalmoscopy, and this can facilitate the ophthalmic consultation via the internet[81]. It is useful for both screening and following up with ROP patients, especially in remote areas such as India or Africa. Some studies reported that in India 15%-20% of premature infants require ROP care services[76]. Long-term studies showed that teleophthalmology with modern technology could be efficient and reliable for screening and management of ROP[75,80,82]. Telemedicine systems provide early feedback to the NICU for appropriate consultation in the infantile clinical center. In this system,screening would be more cost-effective if NICU nurses can capture and interpret images themselves instead of sendingimages to the pediatric ophthalmologist[83]. Many studies have reported high accuracy and sensitivity (100%) of ROP screening by telemedicine in remote areas[73,84-86]. Castillo-Riquelme et al[83] showed that if nurses interpret the photos,the results would have 89.6% sensitivity in comparison with 90% sensitivity of what ophthalmologists would interpret;hence more cost-effective. Vinekar et al[87] used the smartphone for rapid reviewing and reporting transferred data for the specialist. It facilitates access to the data without needing a computer, and hence early diagnosis with proper subsequent follow-ups. Besides that, retinal images that are captured with smartphones can also be very helpful in parents’ education and pediatric training.
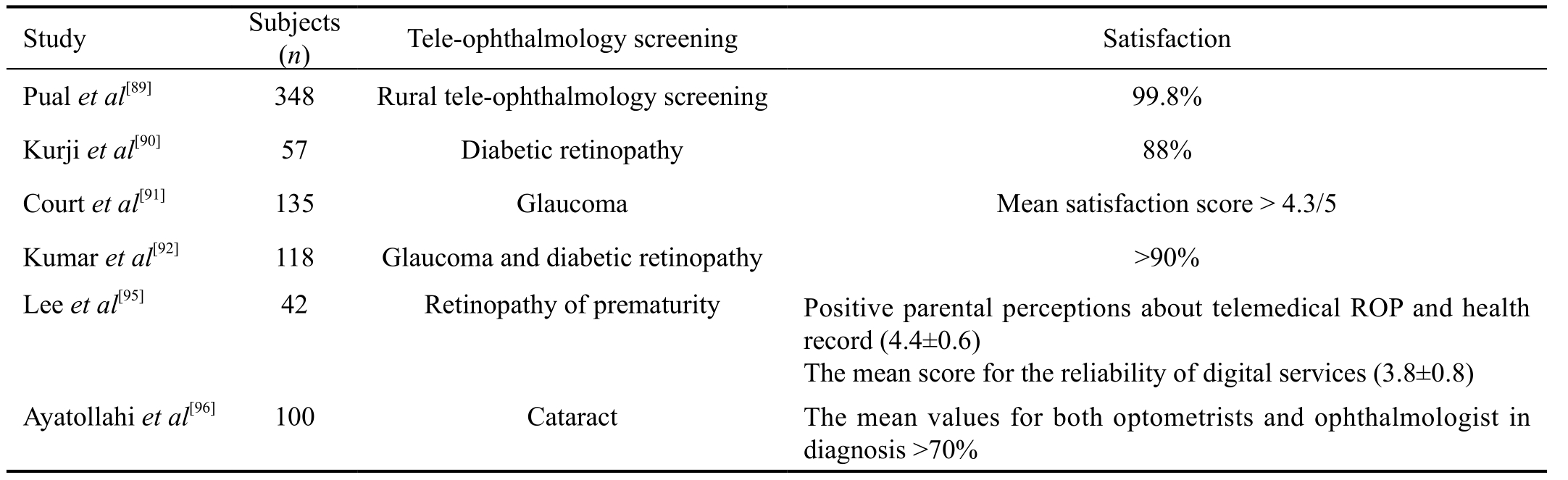
Table 1 Patient satisfaction in teleophthalmology
SMARTPHONE IN OTHER FIELDS
Although ophthalmologist accessibility in rural and remote areas is not always easy or possible, the popular smartphone technology and the photographic images for adnexal and orbital diseases would make it easy to provide everyone with proper eye health care. Verma et al[88] conducted a study in rural areas in India; optometrists evaluated the patients regarding orbital and adnexal eye diseases. The images were captured and labeled with a satellite link for connection to the outside of the village without internet access, and finally,essential information with attached pictures was sent to the ophthalmologist; patients who need further evaluation were referred to the eye health center. 25% of referral patients had sight-threatening disorders and 62% required surgical management. They found that teleophthalmology can be recruited for diagnosis, treatment, and follow up in orbital diseases; orbital and conjunctival diseases such as preseptal cellulitis, dacryocystitis, stye, chalazion, entropion and ectropion, basal cell carcinoma, proptosis and even thyroid eye disease can be diagnosed just by teleophthalmology[88].
Patient Satisfaction in Tele-ophthalmology Our final goal in health systems is providing best care of the population as much as possible. Not only we want to ensure best eye care for our patients, but we also wish to see our patients satisfied. Some studies appropriately focused on this subject,and overall they reported a reasonable level of satisfaction from teleophthalmology services (Table 1). Paul et al[89] used rural mobile teleophthalmology units for 348 patients, and the satisfaction rate was 99.8%. Almost all patients preferred teleophthalmology for their next eye examination. Kurji et al[90]ran a DR screening in a multidisciplinary diabetic clinic. 88%of patients were satisfied and preferred the teleophthalmology option for future screenings because of convenience, timesaving, and visualization of their retina. Court et al[91] studied patients in a virtual glaucoma clinic and compared with control group of healthy clinic patients. Both groups were satisfied,but patients in the virtual clinic had higher awareness than the other group. Also, other studies in this field reported similar results[92-94]. Lee et al[95] assessed the perception of parents about tele-ROP by questionnaire design; they reported that parents had positive perception about this diagnostic method.Ayatollahi et al[96] investigated the teleophthalmology usage in 100 patients with cataract in a pilot study in Iran. They assessed different parameters (such as; system capabilities and screen design) related to the optometrist and corneal specialist in the patient examination and found that the users were satisfied in different areas. Interestingly, we didn’t find any inconsistent results in our literature review regarding patient satisfaction.
Reliability of Tele-ophthalmology Examination Evaluating teleophthalmology reliability with kappa coefficient,Nitzkin et al[97] reported 86.5% reliability versus 91.2% in conventional methods and concluded close similarity between the two approaches.
In DR grading, Russo et al[72] studied 240 diabetic eyes and patients underwent smartphone D-eye lens ophthalmoscopy after dilation, followed by a conventional slit-lamp examination to grade DR and compare the results. The exact overall agreement was 85%, and the agreement within 1-step was reported as high as 96.7%. In smartphone ophthalmoscopy,the sensitivity and specificity to detect clinically significantmacular edema were 81% and 98% respectively[72]. Also,teleophthalmology by general physicians was studied, and high level of reliability and sensitivity (90%) was reported,emphasizing their role in DR screening[98].
Table 2 Cost-utility and cost-effectiveness of teleophthalmology
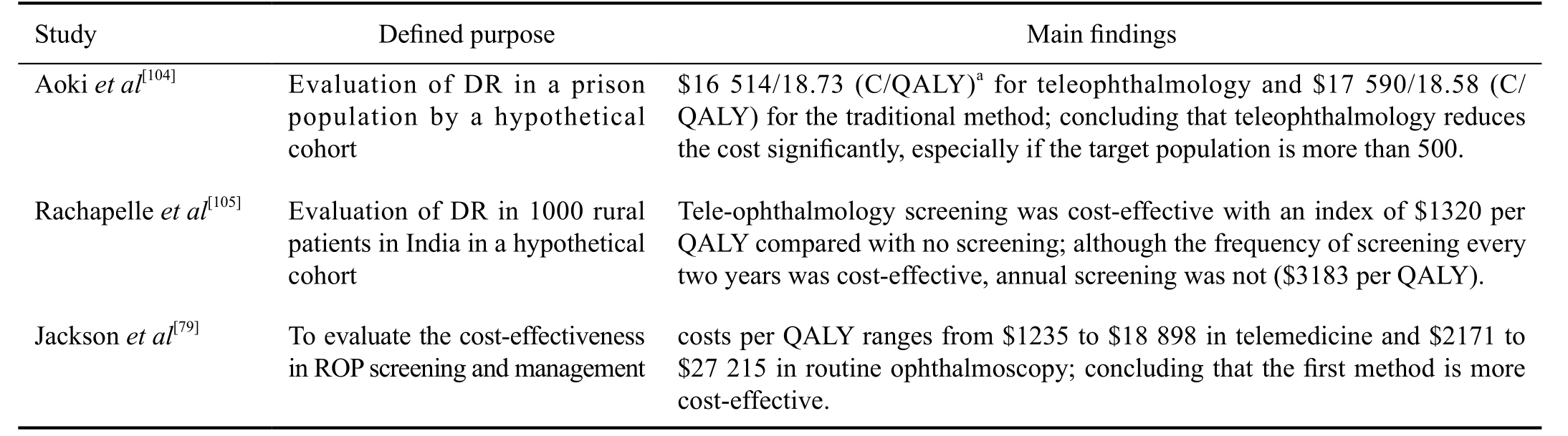
aC/QALY: Cost in U.S dollars per number of quality-adjusted life-years.
In tele-glaucoma, Russo et al[30] studied 110 patients with ocular hypertension (OHT) or primary open angle glaucoma(POAG). The goal was an estimation of the vertical cup-disc ratio (VCDR) through undilated examination in two methods.There was no statistically significant difference in mean VCDR between two approaches. The exact overall agreement was 72.4% in POAG and 66.7% in OHT[99]. In a pilot study including 32 eyes, Li et al[100] found 100% agreement on optic disc parameter. Wright et al[101] evaluated tele-glaucoma with smartphones in the UK and showed 87% agreement while optometrists had missed only 0.054% of patients. However, in remote areas like Kenya, there was the low reliability of teleglaucoma results (sensitivity=41.3% and specificity=89.6%)due to the poor quality of images and little experience of people taking them[43].
In ROP field, we didn’t find any study on reliability of smartphone pictures. However, digital retinal imaging was investigated, and the reliability reported being as high as 0.67 to 0.89[102]. We firmly suggest more studies on accuracy and reliability of smartphone imaging in different fields of ophthalmology.
Policy Making As we mentioned before, teleophthalmology is a new form of communication between patients and healthcare providers. Implementing this new method in health care system requires an evaluation of the process from these aspects: feasibility, clinical outcomes, financial resources,human resources, ease of access, equity, cultural barriers and patient satisfaction. In previous sections, indirectly or directly we talked about many of these factors. In this part, we will focus mostly on cost. A systematic review on cost-utility of telemedicine was conducted by De La Torre-Diez et al[103]in 2015. In teleophthalmology, three studies were found and reviewed (Table 2)[79,104-105]. The index was defined as cost in U.S dollars per number of Quality-Adjusted Life-Years(C/QALYs).
Another factor in successful implementation of the teleophthalmology is eye care providers’ attitude towards the subject. Woodward et al[99] carried out a survey of 58 eye care physicians, 82% of providers were willing of attending teleophthalmology, but more than half (59%) had low confidence for providing remote care. They reported that even after using teleophthalmology, providers’ attitudes did not change and they are not likely to change their practice.However, in the academic medical center, opinions were opposite, maybe because of an intrinsic feature of the academic environment and their compliance with new innovative methods[99]. As a result, academic eye care provider would be a good target for implementing large-scale programs.
CONCLUSION
Tele-based services can be used for screening common ophthalmic diseases especially in developing countries where easy access to the experts is not available for all people,especially in rural areas. We are facing with an increased number of patients with cardiovascular and metabolic diseases,and tele-screening has an important role in early diagnosis,treatment and providing better communications between patients and specialist care. Thanks to this evolution in the medicine, regarding ophthalmology, initial examination and related images can be obtained by medical staff and then be transferred instantly by social networks to the right persons to screen common preventable causes of blindness. Smartphones that are distributed increasingly even in the most deprived areas have increased the availability of social networks and healthcare system. With future advances in technology,patients might be able to manage themselves with new smartphones. Governments should think about establishing trials and programs to provide various packages for screening the prevalent diseases, and to have a suitable collaboration with health and vision-related organizations and help them in reaching the aims of VISION 2020 to accomplish the real sense of “The Right to Sight”.
ACKNOWLEDGEMENTS
Conflicts of Interest: Mohammadpour M, None; Heidari Z,None; Mirghorbani M, None; Hashemi H, None.
REFERENCES
1 Sood S, Mbarika V, Jugoo S, Dookhy R, Doarn CR, Prakash N, Merrell RC. What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemed J E Health 2007;13(5):573-590.
2 Surendran TS, Raman R. Teleophthalmology in diabetic retinopathy. J Diabetes Sci Technol 2014;8(2):262-266.
3 Strouthidis NG, Chandrasekharan G, Diamond JP, Murdoch IE.Teleglaucoma: ready to go? Br J Ophthalmol 2014;98(12):1605-1611.
4 Kandasamy Y, Smith R, Wright I, Hartley L. Use of digital retinal imaging in screening for retinopathy of prematurity. J Paediatr Child Health 2013;49(1):E1-E5.
5 Rudnisky CJ, Tennant MT, Weis E, Ting A, Hinz BJ, Greve MD. Webbased grading of compressed stereoscopic digital photography versus standard slide film photography for the diagnosis of diabetic retinopathy.Ophthalmology 2007;114(9):1748-1754.
6 Bursell SE, Brazionis L, Jenkins A. Telemedicine and ocular health in diabetes mellitus. Clin Exp Optom 2012;95(3):311-327.
7 Hautala N, Hyytinen P, Saarela V, Hagg P, Kurikka A, Runtti M,Tuulonen A. A mobile eye unit for screening of diabetic retinopathy and follow-up of glaucoma in remote locations in northern Finland. Acta Ophthalmol 2009;87(8):912-913.
8 Ribeiro AG, Rodrigues RA, Guerreiro AM, Regatieri CV. A teleophthalmology system for the diagnosis of ocular urgency in remote areas of Brazil. Arq Bras Oftalmol 2014;77(4):214-218.
9 Union IT. ICT facts and figures; the world in 2014. Printed in Switzerland,Geneva 2014.
10 Liesenfeld B, Kohner E, Piehlmeier W, Kluthe S, Aldington S, Porta M, Bek T, Obermaier M, Mayer H, Mann G, Holle R, Hepp KD. A telemedical approach to the screening of diabetic retinopathy: digital fundus photography. Diabetes Care 2000;23(3):345-348.
11 Scanlon PH, Malhotra R, Greenwood RH, Aldington SJ, Foy C,Flatman M, Downes S. Comparison of two reference standards in validating two field mydriatic digital photography as a method of screening for diabetic retinopathy. Br J Ophthalmol 2003;87(10):1258-1263.
12 Mohammadpour M, Mohammadpour L, Hassanzad M. Smartphone assisted slit lamp free anterior segment imaging: a novel technique in teleophthalmology. Cont Lens Anterior Eye 2016;39(1):80-81.
13 Myung D, Jais A, He L, Chang R. Simple, low-cost smartphone adapter for rapid, high quality ocular anterior segment imaging: a photo diary. J Mob Technol Med 2014;3(1):2-8.
14 World Health Organization. Prevention of blindness and deafness.Global initiative for the elimination of avoidable blindness WHO: Geneva 2000.
15 Foster A, Resnikoff S. The impact of Vision 2020 on global blindness.Eye (Lond) 2005;19(10):1133-1135.
16 He M, Mathenge W, Lewallen S, Courtright P. Global efforts to generate evidence for Vision 2020. Ophthalmic Epidemiol 2015;22(4):237-238.
17 Ackland P. The accomplishments of the global initiative VISION 2020:The Right to Sight and the focus for the next 8 years of the campaign.Indian J Ophthalmol 2012;60(5):380-386.
18 Cook C, Murdoch I, Kennedy C, Taylor P, Johnson K, Godoumov R. Teleophthalmology and Vision 2020 in South Africa. S Afr Med J 2004;94(9):750-751.
19 John S, Sengupta S, Reddy SJ, Prabhu P, Kirubanandan K, Badrinath SS. The Sankara Nethralaya mobile teleophthalmology model for comprehensive eye care delivery in rural India. Telemed J E Health 2012;18(5):382-387.
20 Ng M, Nathoo N, Rudnisky CJ, Tennant MT. Improving access to eye care: teleophthalmology in Alberta, Canada. J Diabetes Sci Technol 2009;3(2):289-296.
21 Sreelatha OK, Ramesh SVS. Teleophthalmology: improving patient outcomes? Clin Ophthalmol 2016;10:285-295.
22 Kumar S, Yogesan K. Internet-based eye care: VISION 2020. Am J Ophthalmol 2006;141(2):429.
23 World Health Organization. Universal Eye Health: A global action plan 2014-2019. 2013. ISBN 2015;978(92):4.
24 Chakrabarti R, Perera C. Smartphone medical imaging: applications and future considerations. J Mob Technol Med 2014;3(1):1-1.
25 Lau SL, Chan JB. Mobile cataract screening app using a smartphone.Paper presented at: 2015 IEEE Conference on e-Learning, e-Management and e-Services (IC3e) 2015.
26 Kaur M, Kaur J, Kaur R. Low cost cataract detection system using smart phone. Paper presented at: Green Computing and Internet of Things(ICGCIoT), International Conference on Oct 2015:1607-1609.
27 Fletcher D, Maamari R, Switz N, Margolis T. Retinal cellscope apparatus: United States patent application US 15/094,750; 2016.
28 Maamari RN, Keenan JD, Fletcher DA, Margolis TP. A mobile phonebased retinal camera for portable wide field imaging. Br J Ophthalmol 2014;98(4):438-441.
29 Myung D, Jais A, He L, Blumenkranz MS, Chang RT. 3D printed smartphone indirect lens adapter for rapid, high quality retinal imaging. J Mob Technol Med 2014;3(1):9-15.
30 Russo A, Mapham W, Turano R, Costagliola C, Morescalchi F, Scaroni N, Semeraro F. Comparison of smartphone ophthalmoscopy with slitlamp biomicroscopy for grading vertical cup-to-disc ratio. J Glaucoma 2016;25(9):e777-e781.
31 Chiong HS, Fang JLL, Wilson G. Tele-manufactured affordable smartphone anterior segment microscope. Clin Exp Optom 2016;99(6):580-582.
32 Bastawrous A, Giardini ME, Jordan S. Peek: Portable Eye Examination Kit. The Smartphone Ophthalmoscope. Invest Ophthalmol Vis Sci 2014;55(13):1612-1612.
33 Lamonaca F, Polimeni G, Barbé K, Grimaldi D. Health parameters monitoring by smartphone for quality of life improvement. Measurement 2015;73:82-94.
34 Litmanovitz I, Dolfin T. Red reflex examination in neonates: the need for early screening. Isr Med Assoc J 2010;12(5):301-302.
35 Red reflex examination in neonates, infants, and children. Pediatrics 2008;122(6):1401-1404.
36 Sanguansak T, Morley K, Morley M, Kusakul S, Lee R, Shieh E,Yospaiboon Y, Bhoomibunchoo C, Chai-Ear S, Joseph A, Agarwal I.Comparing smartphone camera adapters in imaging post-operative cataract patients. J Telemed Telecare 2017;23(1):36-43.
37 Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 2006;90(3):262-267.
38 Varma R, Lee PP, Goldberg I, Kotak S. An assessment of the health and economic burdens of glaucoma. Am J Ophthalmol 2011;152(4):515-522.
39 McKean-Cowdin R, Varma R, Wu J, Hays RD, Azen SP, Group LALES. Severity of visual field loss and health-related quality of life. Am J Ophthalmol 2007;143(6):1013-1023.
40 Mills T, Law SK, Walt J, Buchholz P, Hansen J. Quality of life in glaucoma and three other chronic diseases. Drugs Aging 2009;26(11):933-950.
41 Araci IE, Su B, Quake SR, Mandel Y. An implantable microfluidic device for self-monitoring of intraocular pressure. Nat Med 2014;20(9):1074-1078.
42 Russo A, Morescalchi F, Costagliola C, Delcassi L, Semeraro F. A novel device to exploit the smartphone camera for fundus photography. J Ophthalmol 2015;2015:823139.
43 Kiage D, Kherani IN, Gichuhi S, Damji KF, Nyenze M. The Muranga Teleophthalmology Study: Comparison of Virtual (Teleglaucoma) with in-person clinical assessment to diagnose glaucoma. Middle East Afr J Ophthalmol 2013;20(2):150-157.
44 Khouri AS, Szirth BC, Shahid KS, Fechtner RD. Software-assisted optic nerve assessment for glaucoma tele-screening. Telemed J E Health 2008;14(3):261-265.
45 Shahid K, Kolomeyer AM, Nayak NV, Salameh N, Pelaez G,Khouri AS, Eck TT, Szirth B. Ocular telehealth screenings in an urban community. Telemed J E Health. 2012;18(2):95-100.
46 Thomas SM, Jeyaraman MM, Hodge WG, Hutnik C, Costella J,Malvankar-Mehta MS. The effectiveness of teleglaucoma versus inpatient examination for glaucoma screening: a systematic review and meta-analysis. PLoS One 2014;9(12):e113779.
47 De Bats F, Vannier Nitenberg C, Fantino B, Denis P, Kodjikian L. Agerelated macular degeneration screening using a nonmydriatic digital color fundus camera and telemedicine. Ophthalmologica 2013;231(3):172-176.
48 Pirbhai A, Sheidow T, Hooper P. Prospective evaluation of digital nonstereo color fundus photography as a screening tool in age-related macular degeneration. Am J Ophthalmol 2005;139(3):455-461.
49 Zimmer-Galler IE, Zeimer R. Feasibility of screening for high-risk age-related macular degeneration with an Internet-based automated fundus camera. Ophthalmic Surg Lasers Imaging 2005;36(3):228-236.
50 Qureshi K. Teleophthalmology with optical coherence tomography imaging in community optometry. Evaluation of a quality improvement for macular patients. Clin Ophthalmol 2011;5:1673-1678.
51 Brown DM, Kaiser PK, Michels M, Soubrane G, Heier JS, Kim RY,Sy JP, Schneider S. Ranibizumab versus verteporfin for neovascular agerelated macular degeneration. N Engl J Med 2006;355(14):1432-1444.
52 Yu SY, Yang JH, Kim Y, Kwak HW, Blumenkranz M. Reliability of smartphone-based electronic visual acuity testing: (Applications in remote monitoring and clinical research of macular pathology). Invest Ophthalmol Vis Sci 2014;55(13):5598-5598.
53 Chew EY, Clemons TE, Bressler SB, Elman MJ, Danis RP, Domalpally A, Heier JS, Kim JE, Garfinkel RA. Randomized trial of the ForeseeHome monitoring device for early detection of neovascular age-related macular degeneration. The HOme Monitoring of the Eye (HOME) study design-HOME Study report number 1. Contemp Clin Trials 2014;37(2):294-300.
54 Loewenstein A. Use of home device for early detection of neovascular age-related macular degeneration. Ophthalmic Res 2012;48(1):11-15.
55 Maberley DA, Isbister C, Mackenzie P, Aralar A. An evaluation of photographic screening for neovascular age-related macular degeneration.Eye (Lond) 2005;19(6):611-616.
56 Wang YZ, He YG, Mitzel G, Zhang S, Bartlett M. Handheld shape discrimination hyperacuity test on a mobile device for remote monitoring of visual function in maculopathy. Invest Ophthalmol Vis Sci 2013;54(8):5497-5505.
57 Winther C, Frisen L. Self-testing of vision in age-related macula degeneration: a longitudinal pilot study using a smartphone-based rarebit test. J Ophthalmol 2015;2015:285463.
58 Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 2010;87(1):4-14.
59 Jones S, Edwards R. Diabetic retinopathy screening: a systematic review of the economic evidence. Diabet Med 2010;27(3):249-256.
60 Cogan DG, Toussaint D, Kuwabara T. Retinal vascular patterns. IV.Diabetic retinopathy. Arch Ophthalmol 1961;66:366-378.
61 Chew EY. Screening options for diabetic retinopathy. Curr Opin Ophthalmol 2006;17(6):519-522.
62 Coronado AC. Diagnostic Accuracy of Tele-ophthalmology for Diabetic Retinopathy Assessment: A Meta-analysis and Economic Analysis, 2014.
63 Williams GA, Scott IU, Haller JA, Maguire AM, Marcus D, McDonald HR. Single-field fundus photography for diabetic retinopathy screening:a report by the American Academy of Ophthalmology. Ophthalmology 2004;111(5):1055-1062.
64 Cavallerano J, Lawrence MG, Zimmer-Galler I, et al. Telehealth practice recommendations for diabetic retinopathy. Telemed J E Health 2004;10(4):469-482.
65 Group DRSR. Preliminary report on effects of photocoagulation therapy. Am J Ophthalmol 1976;81(4):383-396.
66 Maberley D, Walker H, Koushik A, Cruess A. Screening for diabetic retinopathy in James Bay, Ontario: a cost-effectiveness analysis. CMAJ 2003;168(2):160-164.
67 Whited JD, Datta SK, Aiello LM, Aiello LP, Cavallerano JD, Conlin PR, Horton MB, Vigersky RA, Poropatich RK, Challa P, Darkins AW, Bursell SE. A modeled economic analysis of a digital teleophthalmology system as used by three federal health care agencies for detecting proliferative diabetic retinopathy. Telemed J E Health 2005;11(6):641-651.
68 Mukamel BD, Bresnick HG, Wang Q, Dickey FC. Barriers to compliance with screening guidelines for diabetic retinopathy. Ophthalmic Epidemiol 1999;6(1):61-72.
69 Schoenfeld ER, Greene JM, Wu SY, Leske MC. Patterns of adherence to diabetes vision care guidelines: baseline findings from the Diabetic Retinopathy Awareness Program. Ophthalmology 2001;108(3):563-571.
70 Lord RK, Shah VA, San Filippo AN, Krishna R. Novel uses of smartphones in ophthalmology. Ophthalmology 2010;117(6):1274-1274.e3.
71 Mosa ASM, Yoo I, Sheets L. A systematic review of healthcare applications for smartphones. BMC Med Inform Decis Mak 2012;12:67.
72 Russo A, Morescalchi F, Costagliola C, Delcassi L, Semeraro F.Comparison of smartphone ophthalmoscopy with slit-lamp biomicroscopy for grading diabetic retinopathy. Am J Ophthalmol 2015;159(2):360-364.
73 Silva PS, Cavallerano JD, Aiello LM, Aiello LP. Telemedicine and diabetic retinopathy: moving beyond retinal screening. Arch Ophthalmol 2011;129(2):236-242.
74 Hellström A, Smith LE, Dammann O. Retinopathy of prematurity. The lancet 2013;382(9902):1445-1457.
75 Fierson WM, Saunders RA, Good W, Palmer EA, Phelps D, Reynolds J, Chiang MF, Ruben JB, Granet DB, Blocker RJ. Screening examination of premature infants for retinopathy of prematurity. Pediatrics 2013;131(1):189-195.
76 Kreatsoulas J. Progress in ROP management through tele-ophthalmology.Retina Today 2010.
77 Beck S, Wojdyla D, Say L, Betran AP, Merialdi M, Requejo JH,Rubens C, Menon R, Van Look PF. The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ 2010;88(1):31-38.
78 Gilbert C, Fielder A, Gordillo L, Quinn G, Semiglia R, Visintin P,Zin A. Characteristics of infants with severe retinopathy of prematurity in countries with low, moderate, and high levels of development:implications for screening programs. Pediatrics 2005;115(5):e518-e525.
79 Jackson KM, Scott KE, Graff Zivin J, Bateman DA, Flynn JT, Keenan JD, Chiang MF. Cost-utility analysis of telemedicine and ophthalmoscopy for retinopathy of prematurity management. Arch Ophthalmol 2008;126(4):493-499.e3.
80 Richter GM, Williams SL, Starren J, Flynn JT, Chiang MF.Telemedicine for retinopathy of prematurity diagnosis: evaluation and challenges. Surv Ophthalmol 2009;54(6):671-685.
81 Trese MT. What is the real gold standard for ROP screening? Retina 2008;28(3):1-2.
82 Weaver DT. Use of telemedicine in retinopathy of prematurity. Int Ophthalmol Clin 2014;54(3):9-20.
83 Castillo-Riquelme MC, Lord J, Moseley MJ, Fielder AR, Haines L.Cost-effectiveness of digital photographic screening for retinopathy of prematurity in the United Kingdom. Int J Technol Assess Health Care 2004;20(2):201-213.
84 Chiang MF, Melia M, Buffenn AN, Lambert SR, Recchia FM,Simpson JL, Yang MB. Detection of clinically significant retinopathy of prematurity using wide-angle digital retinal photography: a report by the American Academy of Ophthalmology. Ophthalmology 2012;119(6):1272-1280.
85 Dai S, Chow K, Vincent A. Efficacy of wide-field digital retinal imaging for retinopathy of prematurity screening. Clin Exp Ophthalmol 2011;39(1):23-29.
86 Weaver DT, Murdock TJ. Telemedicine detection of type 1 ROP in a distant neonatal intensive care unit. J AAPOS 2012;16(3):229-233.
87 Vinekar A, Gilbert C, Dogra M, Kurian M, Shainesh G, Shetty B,Bauer N. The KIDROP model of combining strategies for providing retinopathy of prematurity screening in underserved areas in India using wide-field imaging, tele-medicine, non-physician graders and smart phone reporting. Indian J Ophthalmol 2014;62(1):41-49.
88 Verma M, Raman R, Mohan RE. Application of tele-ophthalmology in remote diagnosis and management of adnexal and orbital diseases. Indian J Ophthalmol 2009;57(5):381-384
89 Paul PG, Raman R, Rani PK, Deshmukh H, Sharma T. Patient satisfaction levels during teleophthalmology consultation in rural South India. Telemed J E Health 2006;12(5):571-578.
90 Kurji K, Kiage D, Rudnisky CJ, Damji KF. Improving diabetic retinopathy screening in Africa: patient satisfaction with teleophthalmology versus ophthalmologist-based screening. Middle East Afr J Ophthalmol 2013;20(1):56-60.
91 Court JH, Austin MW. Virtual glaucoma clinics: patient acceptance and quality of patient education compared to standard clinics. Clin Ophthalmol 2015;9:745-749.
92 Kumar S, Tay-Kearney ML, Constable IJ, Yogesan K. Internet based ophthalmology service: impact assessment. Br J Ophthalmol 2005;89(10):1382-1383.
93 Sreelatha OK, Ramesh SV, Jose J, Devassy M, Srinivasan K. Virtually controlled computerised visual acuity screening in a multilingual Indian population. Rural Remote Health 2014;14(3):2908.
94 Tuulonen A, Ohinmaa T, Alanko HI, Hyytinen P, Juutinen A, Toppinen E. The application of teleophthalmology in examining patients with glaucoma: a pilot study. J Glaucoma 1999;8(6):367-373.
95 Lee JY, Du YE, Coki O, Flynn JT, Starren J, Chiang MF. Parental perceptions toward digital imaging and telemedicine for retinopathy of prematurity management. Graefes Arch Clin Exp Ophthalmol 2010;248(1):141-147.
96 Ayatollahi H, Nourani A, Khodaveisi T, Aghaei H, Mohammadpour M. Teleophthalmology in Practice: Lessons Learned from a Pilot Project.Open Med Inform J 2017;11:20-28.
97 Nitzkin JL, Zhu N, Marier RL. Reliability of telemedicine examination.Telemed J 1997;3(2):141-157.
98 Andonegui J, Serrano L, Eguzkiza A, Berastegui L, Jimenez-Lasanta L, Aliseda D, Gaminde I. Diabetic retinopathy screening using teleophthalmology in a primary care setting. J Telemed Telecare 2010;16(8):429-432.
99 Woodward MA, Ple-Plakon P, Blachley T, Musch DC, Newman-Casey PA, De Lott LB, Lee PP. Eye care providers' attitudes towards teleophthalmology. Telemed J E Health 2015;21(4):271-273.
100 Li Z, Wu C, Olayiwola JN, Hilaire DS, Huang JJ. Telemedicinebased digital retinal imaging vs standard ophthalmologic evaluation for the assessment of diabetic retinopathy. Conn Med 2012;76(2):85-90.
101 Wright HR, Diamond JP. Service innovation in glaucoma management: using a Web-based electronic patient record to facilitate virtual specialist supervision of a shared care glaucoma programme. Br J Ophthalmol 2015;99(3):313-317.
102 Salcone EM, Johnston S, VanderVeen D. Review of the use of digital imaging in retinopathy of prematurity screening. Semin Ophthalmol 2010;25(5-6):214-217.
103 De La Torre-Diéz I, López-Coronado M, Vaca C, Aguado JS, De Castro C. Cost-utility and cost-effectiveness studies of telemedicine,electronic, and mobile health systems in the literature: A systematic review. Telemed J E Health 2015;21(2):81-85.
104 Aoki N, Dunn K, Fukui T, Beck JR, Schull WJ, Li HK. Costeffectiveness analysis of telemedicine to evaluate diabetic retinopathy in a prison population. Diabetes Care 2004;27(5):1095-1101.
105 Rachapelle S, Legood R, Alavi Y, Lindfield R, Sharma T, Kuper H, Polack S. The cost-utility of telemedicine to screen for diabetic retinopathy in india. Ophthalmology 2013;120(3):566-573.