INTRODUCTION
Acute symptomatic posterior vitreous detachment(ASPVD) is defined as posterior vitreous detachment(PVD) accompanied with a new onset of symptoms (flashes,floaters) within one month of presentation and Weiss ring found during clinical examination[1-2]. ASPVD is prone to complications, most common are retinal tears and vitreous hemorrhage[1,3]. Consensus opinion regarding the etiology and pathogenesis of these is that vitreous, while retracting from retina, can cause retinal tear. If a blood vessel is affected, vitreous hemorrhage occurs. Although initiation and progression of the PVD were studied extensively and a body of knowledge exists, still there are a number of issues in need of elucidation.
A recently published study reported retinal tears occurring in 8.2%-47.6% of patients with ASPVD[1]. When ASPVD is complicated with vitreous hemorrhage incidence of retinal tears increases to 70%[4]. Nearly one half of symptomatic,untreated retinal tears with persistent traction will cause retinal detachment[2,5-7].
The latest revision of preferred practice pattern guidelines for PVD, retinal breaks, and lattice degeneration still singles out indirect ophthalmoscopy with scleral indentation as the golden standard diagnostic method[8]. Optical coherence tomography,alone or concurrently with ultrasound, is used for evaluation and staging of the PVD[3,9]. As in certain cases ASPVD can be accompanied by vitreous hemorrhage or cells in vitreous,retina cannot be visualized by indirect ophthalmoscopy.Other causes of optical media opacification (e.g. keratopathy,synchisis scintillans, cataract, etc.) or poor pupil dilatation can aggravate retina visualization and retinal tears detection. In these cases, the method of choice is B-scan ultrasound.
The aim of this study was to assess the reliability of ultrasound in detection of retinal tears in ASPVD.
METHODS
Cross-sectional study of seventy five consecutive patients presenting with ASPVD symptoms was conducted at University Eye Clinic, Faculty of Medicine, University Josip Juraj Strossmayer in Osijek, University Hospital "Sveti Duh",Zagreb, between May 2014 and June 2015. The study was conducted with the approval of the local research Ethics committee and by complying with the tenets of the Declaration of Helsinki. Informed oral consent was obtained from all patients prior to their inclusion in the study. Descriptive statistics was used for data evaluation (Microsoft Office Excel 2010, Version 14.0.7106.5003).
The study inclusion criterion was ASPVD. In each patient,transpalpebral ultrasound of the eye and the orbit was performed using 10 MHz probe (UltraScan, Alcon) followed by indirect ophthalmoscopy initially and in 6wk period.
Patients whose optical media were not transparent enough for fundus visualization were not included in the study, as in these cases indirect ophthalmoscopy was not possible. Ultrasound and fundus photos were documented.
On ultrasound, retinal tear was defined as a short discontinued highly reflective membranous reflection adhering to the peripheral posterior wall, exerting wavy after-movement. It is attached to the thin high reflective membranous reflection with echographic characteristics of posterior hyaloid membrane[10](Figure 1).
RESULTS AND DISCUSSION
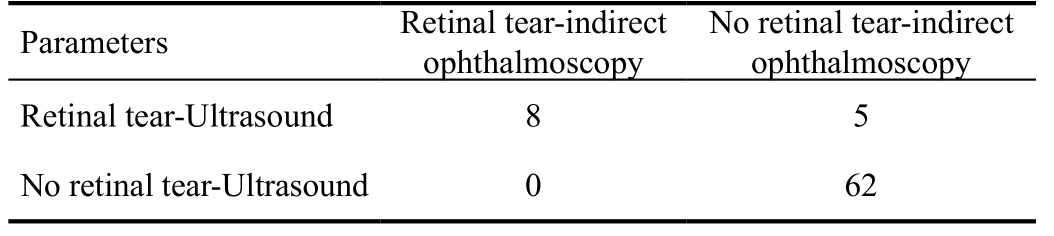
In 13 (17%) patients membranous lesion with ultrasound characteristics of retinal tear described in METHODS section was detected. Clinical examination of the fundus confirmed the diagnosis in 8/13 patients. In those patients laser photocoagulation was performed. In the rest 5/13 patients localized vitreous condensation was detected. However, in one patient with vitreous condensation laser photocoagulation was performed due to secondary retinal traction changes. In 62/75 patients neither ultrasound nor clinical examination revealed any complication of PVD.
Data presented in Table 1 were used to calculate diagnostic test reliability parameters. Sensitivity was 100% (95% CI 60%-100%),specificity 92%, positive predictive value 62% (95% CI 32%-85%), and negative predictive value 100% (95% CI 93%-100%). Positive likelihood ratio was found to be 13.4(95% CI 5.8-31.1), while negative likelihood ratio was 0.
In our study, B-scan ultrasound showed sensitivity and specificity of 100% and 92%, respectively, while positive and negative predictive value were 62% and 100%. Though the sample size was small, results still indicate on high sensitivity and negative predictive value, and somewhat lower specificity and positive predictive value.
In line with results of other studies[6,11-13], B-scan ultrasound proved to be a reliable diagnostic method in detecting possible retinal tears in patients with ASPVD-patients without retinal tear will not be misclassified, but most of the patients with possible tears will be recognized. In 1992, DiBernardo et al[15]reported sensitivity of 91% and specificity of 97% for B-scan ultrasound as a method for the same clinical entity as in our study. Since 1992, important improvements in ultrasound diagnostics have been introduced, and we assume that these upgradings have contributed to even higher reliability of the ultrasound than previously reported[11-12].
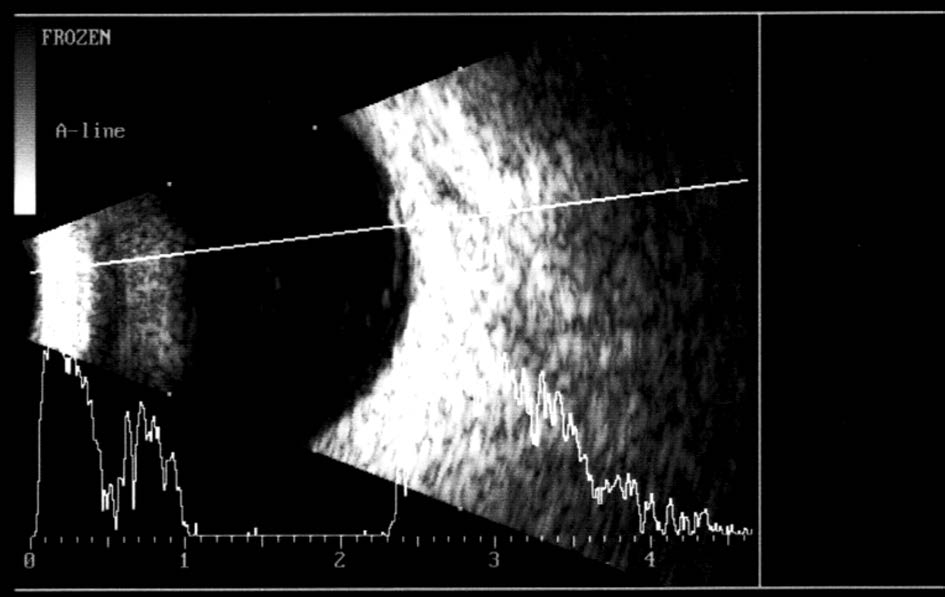
Figure 1 Retinal tear is anchored to the detached posterior hyaloid membrane.
Table 1 Data for diagnostic test reliability parameters calculation
Lorenzo-Carrero et al[6] performed the ultrasound examination by placing the probe directly on ocular surface, while in our case, the probe was placed on the eyelid. Regardless of the difference in the probe placement, both studies showed similar results.
In five cases, we presumed retinal tear on ultrasound examination.However, on clinical examination it was verified as preretinal vitreous condensation. Subsequently, ultrasound photos were revised in order to set distinction criteria between retinal tear and vitreous condensation. The latter was defined as a discontinued medium reflective membranous reflection adhering to the peripheral posterior wall, without attachment to the posterior hyaloid membrane and displaying no wavy aftermovement[10].
Our study was performed with 10 MHz probe. Similar study[6]also describes 10 MHz probe results. Hewick et al[11] compared 10 MHz probe with 20 MHz probe and found that 20 MHz probe offers higher resolution of chorioretina, sclera, optic nerve sheaths and extraocular muscles than 10 MHz probe. It would be of interest to perform a research with 20 MHz probe,to establish if it offers even more reliable findings of retinal diseases, due to lower interference with vitreous opacities[11-12].
In all patients included in the study, the follow-up examination was performed in 6wk. Although, Coffee et al[1] recommend follow up examination only in higher risk cases, consensus on the matter is still not reached[1,4]. In our clinic, patients with ASPVD are briefed with their condition as well as possible complications in case of which they should return immediately.Otherwise, they are advised to have fundus and ultrasound examination repeated in 6wk.
In case of optical media opacification, B-scan ultrasound is a readily available method for evaluating retinal status. Ahmed et al[7] reported that among 48 eyes with vitreous hemorrhage impairing adequate visual assessment, posterior segment pathology was found in 34 eyes. Sharma et al[4] reports that 70% of patients with ASPVD accompanied by vitreous hemorrhage have retinal tears, as opposed to only 2%-3% of patients without vitreous hemorrhage. These findings indicate on necessity of ultrasound examination in patients with PVD complicated with vitreous hemorrhage-when the visualization of the retina by indirect ophthalmoscopy is mostly impaired is exactly when it is most important.
The main limitation of the study is relatively small sample size. However, data in the literature on the subject are scarce,and each study contributes to elucidation of the issues remained[6,9,13-15].
In conclusion, B-scan ultrasound is a reliable and accurate method for detection of retinal tears in ASPVD. Given the high sensitivity and negative predictive value, negative result on B-scan ultrasound excludes the probability of the retinal tear with a high degree of certainty. We call upon further research on a larger sample and possibly with 20 MHz probe that could offer even higher level of reliability of B-scan ultrasound for retinal tears detection in acute symptomatic PVD.
ACKNOWLEDGEMENTS
Conflicts of Interest: Kuzmanović Elabjer B, None; Bušić M, None; Bišćan Tvrdi A, None; Miletić D, None; Bosnar D,None; Bjeloš M, None.
REFERENCES
1 Coffee RE, Westfall AC, Davis GH, Mieler WF, Holz ER. Symptomatic posterior vitreous detachment and the incidence of delayed retinal breaks:case series and meta-analysis. Am J Ophthalmol 2007;144(3):409-413.
2 Goh YW, Ehrlich R, Stewart J, Polkinghorne P. The incidence of retinal breaks in the presenting and fellow eyes in patients with acute symptomatic posterior vitreous detachment and their associated risk factors. Asia Pac J Ophthalmol (Phila) 2015;4(1):5-8.
3 Pop M, Gheorghe A. Pathology of the vitreomacular interface.Oftalmologia 2014;58(2):3-7.
4 Sharma MC, Regillo CD, Shuller MF, Borrillo JL, Benson WE.Determination of the incidence and clinical characteristics of subsequent retinal tears following treatment of the acute posterior vitreous detachment-related initial retinal tears. Am J Ophthalmol 2004;138(2):280-284.
5 Takkar B, Azad S, Shashni A, Pujari A, Bhatia I, Azad R. Missed retinal breaks in rhegmatogenous retinal detachment. Int J Ophthalmol 2016;9(11):1629-1633.
6 Lorenzo-Carrero J, Perez-Flores I, Cid-Galano M, Fernandez-Fernandez M, Heras-Raposo F, Vazquez-Nuñez R, Lopez-Fuentes M. B-scan ultrasonography to screen for retinal tears in acute symptomatic age-related posterior vitreous detachment. Ophthalmology 2009;116(1):94-99.
7 Ahmed J, Shaikh FF, Rizwan A, Memon MF. Evaluation of vitreo-retinal pathologies using B-scan ultrasound. Pak J Ophthalmol 2009;25:4.
8 American Academy of Ophthalmology. Posterior Vitreous Detachment,Retinal Breaks, and Lattice Degeneration PPP, 2014. Available at: http://www.aao.org/preferred-practice-pattern/posterior-vitreous-detachmentretinal-breaks-latti-6
9 Abdolrahimzadeh S, Piraino DC, Scavella V, Abdolrahimzadeh B,Cruciani F, Gharbiya M, Recupero SM. Spectral domain optical coherence tomography and B-scan ultrasonography in the evaluation of retinal tears in acute, incomplete posterior vitreous detachment. BMC Ophthalmology 2016;16:60.
10 Kuzmanović Elabjer B, Bušić M, Bosnar D. Atlas of ultrasoundultrasound presentations of eye and orbit pathology. Croatia: Cerovski d.o.o.; 2013.
11 Hewick SA, Fairhead AC, Culy JC. A comparison of 10 MHz and 20 MHz ultrasound probes in imaging the eye and orbit. Br J Ophthalmol 2004;88(4):551-555.
12 Bottós JM, Torres VL, Kanecadan LA, Martinez AA, Moraes NS,Maia M, Allemann N. Macular hole: 10 and 20-MHz ultrasound and spectral-domain optical coherence tomography. Arq Bras Oftalmol 2012;75(6):415-419.
13 Zvornicanin J, Jusufovic V, Cabric E, Musanovic Z, Zvornicanin E,Popovic-Beganovic A. Significance of ultrasonography in evaluation of vitreo-retinal pathologies. Med Arch 2012;66(5):318-320.
14 Parchand S, Singh R, Bhalekar S. Reliability of ocular ultrasonography findings for pre-surgical evaluation in various vitreo-retinal disorders.Semin Ophthalmol 2014;29(4):236-241.
15 DiBernardo C, Blodi B, Frazier Byrne S. Echographic Evaluation of Retinal Tears in Patients With Spontaneous Vitreous Hemorrhage. Arch Ophthalmol 1992;110(4):511-514.