INTRODUCTION
Trabeculectomy is the mainstay of glaucoma surgery.It may be combined with phacoemulsification, which when done alone, achieve intraocular pressure (IOP)reduction[1-2]. The additive effect of phacoemulsification and trabeculectomy should presumably render better IOP control.However, whether additional surgical intervention leads to more intense inflammation and reduces the successful rate of the filtration surgery remains questionable. Previous studies to compare the effect of IOP control of trabeculectomy and phacotrabeculectomy achieved inconsistent results[3-6]. In this study, we aimed to compare the effects of these 2 procedures in term of IOP control, change in visual acuity (VA) and complications in Chinese patients with suboptimal IOP control.
METHODS
It is a retrospective, comparative case series. The study adhered to the tenets of the Declaration of Helsinki. Due to the retrospective nature of the study, informed conssent was waived. Thirty-eight consecutive patients who underwent either trabeculectomy or combined phacotrabeculectomy from October 2009 to September 2010 by a single surgeon at a hospital in Hong Kong were reviewed. The post-operative IOP and VA (logMAR) between the two groups were compared with independent t-test, and the VA and IOP at 3mo were compared with the baseline with dependent t-test. Number of patients with VA change, bleb morphology and complications were analysed with Fisher exact test or Chi-square test. Postoperative data at 1d, 1wk, 1 and 3mo were analysed.
RESULTS AND DISCUSSION
Among the 38 eyes (38 patients), 20 eyes underwent phacotrabeculectomy and 18 eyes underwent trabeculectomy.All patients were Chinese. They were on maximally-tolerated glaucoma medications which failed to control the IOP to below 21 mm Hg prior to filtration surgery. There were 11 males and 9 females in the phacotrabecullectomy group; and 12 males and 6 females in the trabeculectomy group. The mean age was 65.7±14.8y and 62.4±12.0y in the phacotrabeculectomy and trabeculectomy groups respectively (P=0.47). The baseline VA was 0.96±1.04 in the phacotrabeculectomy group and 0.47±0.48 in the trabeculectomy group (P=0.07). The baseline IOP was 27.18±8.48 mm Hg and 27.86±10.55 mm Hg in the phacotrabeculectomy and trabeculectomy groups respectively(P=0.83). In the trabeculectomy group, 9 (45%) of the patients had primary open angle glaucoma (POAG), 5 (25%) had chronic angle-closure glaucoma (CACG), and 6 (30%) had uveitic glaucoma; whereas in the trabeculectomy group,11 (61%) had POAG, 5 (28%) had CACG, 1 (5.6%) had angle recession glaucoma and 1 (5.6%) had steroid-induced glaucoma.IOP was not significantly different between 2 groups from post-operative 1d to 3mo (Table 1). Complete success(defined as IOP<22 mm Hg without the use of any glaucoma medications) was achieved in 65% of phacotrabeculectomy cases, and 66.7% of trabeculectomy cases. Qualified success(IOP<22 mm Hg with the use of glaucoma medications)was achieved in 25% of phacotrabeculectomy, and 16.7% of trabeculectomy cases. There was 16.7% of failure (uncontrolled IOP>21 mm Hg despite the use of glaucoma medications) in phacotrabeculectomy cases, and 10% of trabeculectomy cases at 3mo. However, there were no statistical difference between the 2 groups in the success/failure rates at 3mo (P=0.68, Fisher exact test). Compared to baseline, IOP at 3mo was significantly reduced in both groups (P<0.01).
Table 1 Post-operative IOP and IOP reduction from baseline (mean±SD; mm Hg)

Table 2 Post-operative VA change n (%)
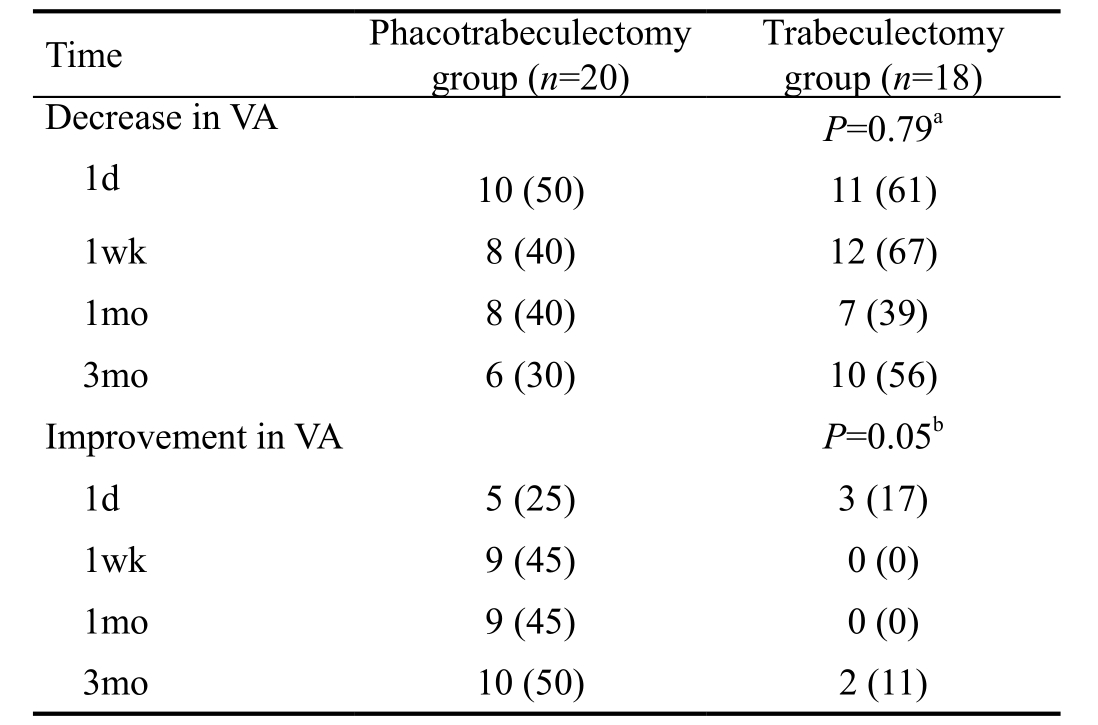
aChi-square test; bFisher exact test.
In 6 (30%) of the patients in the phacotrabeculectomy group, topical glaucoma medications were resumed postoperatively to achieve optimal IOP control; while in only 3 patients (16.7%) among the trabeculectomy patients glaucoma medications were resumed.
Needling was performed in 11 (55%) of the patients in the phacotrabeculectomy group, and 9 (50%) in the trabeculectomy group.
VA at post-operative 1d to 3mo were not significantly different between 2 groups. The percentage of patients with reduction in VA throughout the studied period were comparable between the 2 groups except at 3mo, reduction in VA was observed in 30% of the patients following phacotrabeculectomy, but was identified in 55.6% of the trabeculectomy patients (Table 2).
In term of change in VA compared to baseline, the phacotrabeculectomy group consistently performed better than the trabeculectomy group up to 3mo. The difference in the improvement of VA between 2 groups was statistically significant (P=0.05; Table 2). However, there were no significant difference between the VA at baseline compared to at 3mo in both phacotrabeculectomy (P=0.49) and trabeculectomy (P=0.72) groups.
Trabeculectomy resulted in higher proportion of diffuse bleb and less flat bleb than phacotrabeculectomy. Diffuse bleb occurred in 13 (65%) of the phacotrabeculectomy group and 15(83%) after trabeculectomy. Flat bleb was present in 7 (35%)and none of the phacotrabeculectomy and trabeculectomy groups respectively. The difference in bleb morphology was statistically significant (P=0.02, Fisher exact test).
Surgical complications were rare in both groups. The only complication was hypotony (IOP<6 mm Hg), which was present in 5% of phacotrabeculectomy, and none of the trabeculectomy cases.
The study showed that both trabeculectomy and phacotrabeculectomy are effective in reducing IOP in patients on maximally-tolerated glaucoma medications.Similar IOP reduction was observed in both groups. It is consistent with other studies[4-6]. It is expected that cataract progression would hasten after filtration procedure, therefore phacotrabeculectomy offers an additional benefit to the patients by removing the cataract in a single stage procedure.It improves the visual outcome than trabeculectomy alone by cataract extraction. However, phacotrabeculectomy did not offer additional IOP lowering and it seemingly led to a higher chance of flat bleb, requiring resumption of glaucoma medications and additional procedure to achieve adequate IOP control. It is possibly due to inflammation induced by the additional phacoemulsification. Therefore, only in patients with visually significant cataract who prefer two surgeries to be performed simultaneouosly, phacotrabeculectomy should be offered with the potential benefits and disadvantages explained to patients. In patients with narrow angle and suboptimal IOP control, phacoemulsification alone is effective in IOP reduction[7-8]. Therefore, phacoemulsification, which is associated with less risks, should be offered to these patients.Additional trabeculectomy might be done at second stage,if the IOP control is still suboptimal. However, in patients with visually significant cataract, phacotrabeculectmy may be a preferred option. Studies have shown that cataract surgery following trabeculectomy increased the failure rate of trabeculectomy[9-10].
The limitation of our study includes it consisted of a heterogeneous group of patients with various etiologies of glaucoma. Secondary glaucoma, including uveitic glaucoma,increases surgical failure. However, in our study, although there were more uveitic patients (n=6) in the phacotrabeculectomy group, it was unrelated to the surgical failure. None of the 6 uveitic patients had surgical failure, and 4 of them had diffuse bleb morphology at 3mo. Furthermore, the follow up period is relatively short to determine the long term successful rate of filtration surgery although the difference in bleb morphology is already statistically significant. A study showed that bleb height was related to IOP in phacotrabeculectomy at 2y[11].We expect that more cases would have surgical failure in the phacotrabeculectomy group given a longer time of follow up.Moreover, the patients were not randomized regarding the type of surgery they received although the baseline characteristics of the 2 groups were comparable.
In conclusion, phacotrabeculectomy and trabeculectomy achieved equally effective post-operative IOP control up to 3mo. However, phacotrabeculectomy cases performed better in terms of improvement in VA. On the other hand, patients who underwent trabeculectomy alone had better diffuse bleb morphology, less requirement on resumption of glaucoma medications, and less additional procedure, although there was no significant difference in IOP reduction in this group of Chinese patients.
ACKNOWLEDGEMENTS
Conflicts of Interest: Choy BNK, None.
REFERENCES
1 Chen PP, Lin SC, Junk AK, Radhakrishnan S, Singh K, Chen TC. The effect of phacoemulsification on intraocular pressure in glaucoma patients:a report by the American Academy of Ophthalmology. Ophthalmology 2015;122(7):1294-1307.
2 Slabaugh MA, Bojikian KD, Moore DB, Chen PP. The effect of phacoemulsification on intraocular pressure in medically controlled openangle glaucoma patients. Am J Ophthalmol 2014;157(1):26-31.
3 Ogata-Iwao M, Inatani M, Takihara Y, Inoue T, Iwao K, Tanihara H. A prospective comparison between trabeculectomy with mitomycin C and phacotrabeculectomy with mitomycin C. Acta Ophthalmol 2013;91(6):e500-e501.
4 Wang M, Fang M, Bai YJ, Zhang WZ, Lin MK, Liu BQ, Hao YT, Ling YL, Zhuo YH, Ge J. Comparison of combined phacotrabeculectomy with trabeculectomy only in the treatment of primary angle-closure glaucoma.Chin Med J 2012;125(8):1429-1433.
5 Murthy SK, Damji KF, Pan Y, Hodge WG. Trabeculectomy and phacotrabeculectomy, with mitomycin-C, show similar two-year target IOP outcomes. Can J Ophthalmol 2006;41(1):51-59.
6 Guggenbach M, Mojon DS, Bohnke M. Evaluation of phacotrabeculectomy versus trabeculectomy alone. Ophthalmologica 1999;213(6):367-370.
7 Tham CC, Kwong YY, Leung DY, Lam SW, Li FC, Chiu TY,Chan JC, Lam DS, Lai JS. Phacoemulsification versus combined phacotrabeculectomy in medically uncontrolled chronic angle closure glaucoma with cataracts. Ophthalmology 2009;116(4):725-731,731.e1-3.
8 Tham CC, Kwong YY, Leung DY, Lam SW, Li FC, Chiu TY,Chan JC, Chan CH, Poon AS, Yick DW, Chi CC, Lam DS, Lai JS.Phacoemulsification versus combined phacotrabeculectomy in medically controlled chronic angle closure glaucoma with cataract. Ophthalmology 2008;115(12):2167-2173.e2.
9 Nguyen DQ, Niyadurupola N, Tapp RJ, O'Connell RA, Coote MA,Crowston JG. Effect of phacoemulsification on trabeculectomy function.Clin Exp Ophthalmol 2014;42(5):433-439.
10 Longo A, Uva MG, Reibaldi A, Avitabile T, Reibaldi M. Long-term effect of phacoemulsification on trabeculectomy function. Eye (Lond)2015;29(10):1347-1352.
11 Smith M, Chipman ML, Trope GE, Buys YM. Correlation between the indiana bleb appearance grading scale and intraocular pressure after phacotrabeculectomy. J Glaucoma 2009;18(3):217-219.