INTRODUCTION
Trabeculectomy is still the gold standard and most frequently performed type of surgery to lower intraocular pressure (IOP) for glaucoma patients[1-3]. As Cairns[4] first described that the main goal of this filtering surgery is to create an aqueous drainage pathway between the anterior chamber and sub-Tenon space; forming a subconjonctival bleb.
The success rates of trabeculectomy mainly depends on a well functioning bleb, meaning adequate wound healing to balance external resistance and maintenance of filtration.Hypotony is the major complication occurs when the healing is insufficient. In contrast, if the healing is excessive, high IOP will present postoperatively. Adjunctive antimetabolites, such as mitomycin C (MMC) and 5-fluorouracil (5-FU) are widely used to modulate wound healing, and decrease the rate of postoperative hypotony-associated complications[5].
The scleral flap suturing technique also plays a major role for maintenance of filtration. The surgeon should adjust the suture tension, loose enough to permit aqueous humor outflow, but tight enough to prevent postoperative complications[6]. Among with permanent sutures, various techniques for releasable sutures, adjustable sutures and laser suture lysis have been introduced and widely accepted[7-13].
In some cases of high postoperative IOP, withdrawal of releasable sutures is not always sufficient to lower the pressure. In this context, Figus et al[14] described an everting suture technique that helps to lift the flap and create an efficient aqueous outflow. Here, we present a novel suturing technique to lift up the scleral flap by an even pulling pressure on the edges,in order to prevent the flap obstruction, provide adequate and desired aqueous flow.
SUBJECTS AND METHODS
Our study group consisted of 8 eyes of 8 patients with neovascular glaucoma as a consequence of central retinal vein occlusion or proliferative diabetic retinopathy. All patients underwent MMC augmented trabeculectomy in Department of Ophthalmology, Faculty of Medicine, Uludag University between June 2015 and July 2016.
We collected data for each subject in terms of sex, age, IOP before and after trabeculectomy (using Goldmann applanation tonometer), releasable suture removal time postoperatively,number of pressure-lowering medications used before and after trabeculectomy, complications and follow-up periods.
All procedures were performed by the same surgeon(Baykara M). Concisely, trabeculectomy was performed as follows: a fornix-based conjunctiva and Tenon’s capsule flap was created. After adequate hemostasis, one-half thickness rectangular (4 mm×2 mm) scleral flap was dissected. Two surgical sponges (2 mm×2 mm) soaked with 0.4 mg/mL MMC were applied over the dissected bed, the scleral flap and conjunctiva-Tenon layer were draped over the sponges.After 3min, the sponges were removed and the surgical area was irrigated with balanced salt solution. Subsequently, the trabecular block was removed and a peripheral iridectomy was performed.
The scleral flap closure is performed with three separate sutures, initially, our accordion suture through the center of the flap, and two releasable sutures on both corners. The 10-0 nylon is the suture of choice for the procedure.
The description of the accordion suture technique is as follows:first, the suture is passed through the mid-distal edge of the scleral flap, internal to external and then through mid-left edge of the flap, external to internal; next, the suture is passed through clear cornea at the limbus, and again through the clear cornea creating a U-shaped loop; afterwards, the suture is passed through mid-right edge of the scleral flap, internal to external and finally again through the mid-distal edge of the flap, external to internal (Figure 1). At this point, both ends of the suture are placed underneath the scleral flap and subsequently they are finely tied with a 3-1-1 slip knot manner after adjustment of desired tension (Figure 2). Two releasable sutures are then performed on both left and right distal corners of the scleral flap using the technique described by Kolker et al[6] (Figure 3). After conjunctival closure, U-shaped anterior loop of our acccoridon suture and the ends of two releasable sutures are now visible on the clear cornea (Figure 4).
By means of our technique, postoperative IOP reduction may be obtained by a step-by-step manner. The surgeon first removes the two side releasable sutures and if this maneuver is not sufficient; the loop of the accordion suture may be pulled by a tying forceps in order to achieve desired IOP (Figure 5).The flap cannot be lifted unless the first two side releasable sutures are removed in front. An even lifting pressure is applied on both left and right edges of the flap by pulling the loop of the suture. The flap opens up in an accordion manner and we can see a bleb is rapidly formed with a substantive decrease of IOP. Afterwards, gentle ocular massage is applied in order to flatten the flap.
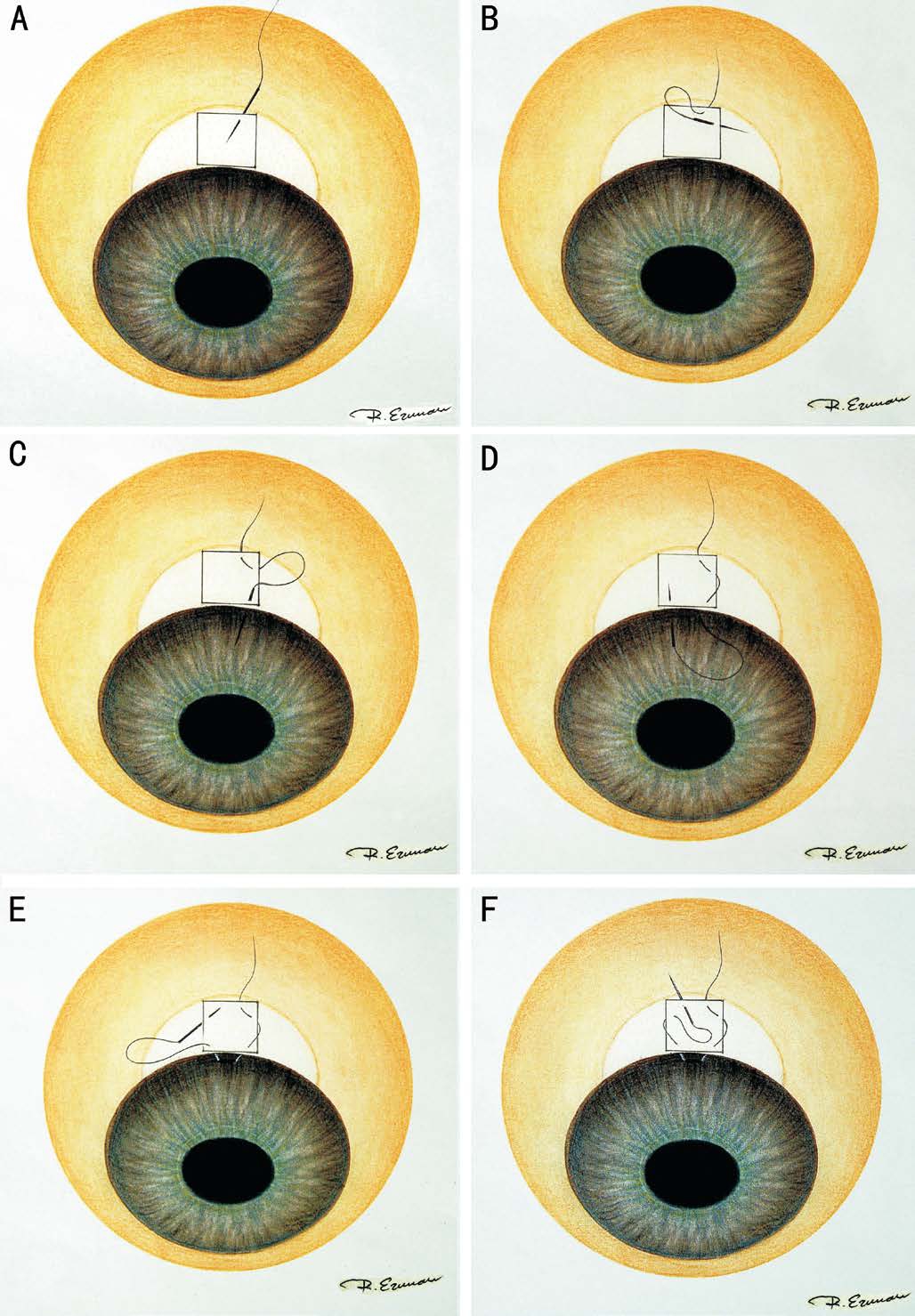
Figure 1 Description of the accordion suture A: The suture is passed through the mid-distal edge of the scleral flap internal to external; B: The suture is passed through mid-left edge of the flap,external to internal; C-D: The suture is passed through clear cornea at the limbus, and again through the clear cornea creating a U shaped loop; E: The suture is then passed through mid-right edge of the scleral flap, internal to external; F: The suture is passed through the mid-distal edge of the flap, external to internal.
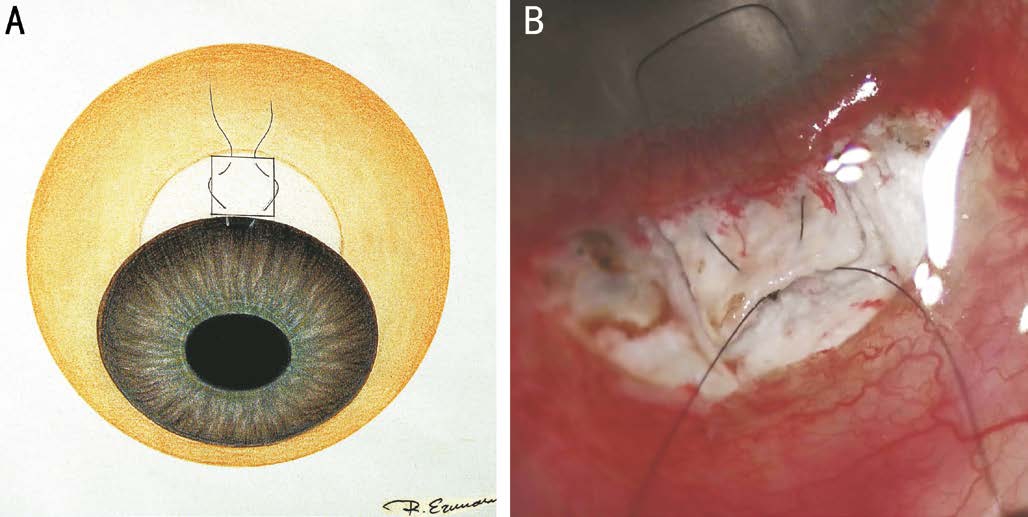
Figure 2 Knot technique for the accordion suture A: Both ends of the suture are underneath the scleral flap; B: Subsequently, they are tied with a 3-1-1 slip knot manner after adjustment of desired tension.
RESULTS
Hereby, we present our preliminary results of 8 eyes of 8 patients who underwent trabeculectomy with our accordion suture technique.
Mean age of the subjects was 67.42±8.21y and female/male ratio was 4/4. The mean IOP of the eyes at the day before trabeculectomy was 37±7.48 (range 23-45) mm Hg. No intraoperative complications occurred during the surgeries.

Figure 3 Performance of two side releasable sutures A: Two releasable sutures are then put on both left and right distal corners of the scleral flap using the technique described by Kolker et al[6]; B:Final image of the accordion suture along with two side releasable sutures before conjunctival closure.
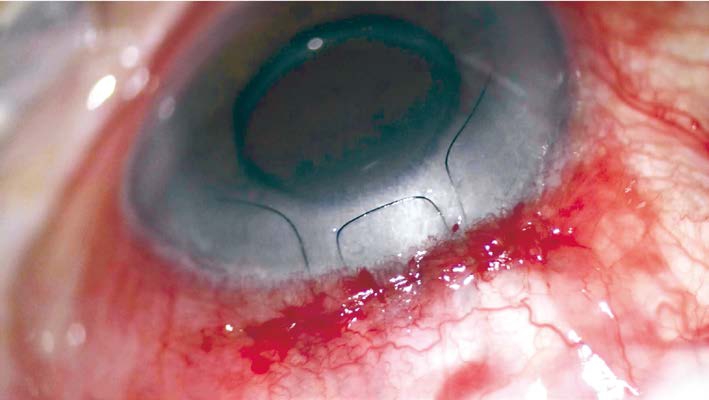
Figure 4 After conjunctival closure, the ends of two releasable sutures and between them, U-shaped anterior loop of our everting suture are now visible on the clear cornea.

Figure 5 The loop of the accordion suture may be pulled by a tying forceps in order to achieve desired IOP.
Postoperative control visits planned as weekly for the first month and monthly later on. The mean IOP at the postopertive first day was 10.87±1.88 (range 8-14) mm Hg.During the follow up period, the mean IOP at the 1, 2, 3wk was 13.87±1.96 (range 12-17), 15.87±2.75 (range 12-19),19.25±2.82 (range 15-23) mm Hg, respectively.
All patients received removal of both side releasable sutures and traction of the accordion suture at the same time without any complications. The mean removal time was 3.5±0wk postoperatively. The mean IOP of the eyes before and after the procedure was 22.63±2.06 (range 19-25) and 11.12±2.64 (range 8-15) mm Hg, respectively.
The mean follow up period was 5.75±1.41mo. All the subjects received 4 IOP-lowering agents preoperatively, which were discontinued in the early postoperative period. Despite the traction of the accordion suture with removal of releasable sutures, four subjects had persistent high IOP which was controlled with 1 anti-glaucomatous agent. The accordion suture was pulled once for each subject, and the mean postoperative IOP at the final visit was 11.37±2.72 (range 8-16) mm Hg. No further interventions were needed for any of the eyes.
DISCUSSION
Trabeculectomy is the most extensive choice of surgical intervention for uncontrolled glaucoma patients, particularly when a low IOP is targeted[3]. In course of time, adjunctive antimetabolites have been widely accepted and the surgical technique for flap suturing has been modified for optimal postoperative results.
The releasable suture techniques have advantages over permanent conventional sutures; these include minimalizing early postoperative complications related to hypotony as well as restrained long-term control of IOP[9]. With comparison to laser suture lysis, releasable sutures may decrease postoperative shallow anterior chamber and hypotony risks[10].One disadvantage of releasable sutures is increased risk of infection, furthermore endophthalmitis[15-16]. With regard to the accordion suture technique; there is no knot left exposed,providing minimal risk of infection and foreign body sensation.We did not observe any complications arise from infection related causes for any of the eyes.
The crucial step to surgical postoperative success is the IOP control. Early removal of releasable sutures cause postoperative aqueous leak and hypotony related complications, whereas late removal might end with scarring of the scleral flap and late high IOP. The timing of releasable suture removal must be adjusted individually for each patient with the consideration of factors that have an affect on fibrosis, such as existence of other ocular and systemic diseases, taken medications,Tenon thickness, presence of neovascularization, the dose and timing of intraoperative anti-metabolite usage. Our surgical experience is to remove the releasable sutures by 3 to 6wk postoperatively, as described in the previous literature.Removal of the releasable sutures are not always sufficient to reopen the scleral flap and create the aqueous drainage[14]. The accordion suture gives us the chance to overcome this issue and successfully lift up the flap even at the presence of visible scarring. The main principle of the accordion suture is to allow the flap move by an uniformly applied traction pressure on both sides, as an alternative to the everting suture technique previously described[14].
Traction of the accordion suture, concomitant with removal of releasable sutures were performed without any complications.By means of adequate pressure and cautious technique, the traction may be performed trouble free. However, the suture broke during this process with one of our early patients and we were able to remove the exposed part of the suture smoothly,without any further long term complications.
The main limitation of our technique is the number of our subjects. Although limited, the sample size provides us encouraging, safe and effective postoperative surgical data. On the ground that we intended to compose a homogenous group of eyes; single surgeon and lack of type of disease might be listed as other limitations. Therefore, further studies with larger number of eyes and long-term follow-up periods are needed to establish more accurate data of the accordion suture and its comparability with other techniques.
We believe this technique can be the suture of choice for filtering glaucoma surgery in experienced hands by its easy learning curve for precisely indicated patients.
ACKNOWLEDGEMENTS
Conflicts of Interest: Baykara M, None; Can Ermerak B,None; Sabur H, None; Genc S, None.
REFERENCES
1 Wells AP, Bunce C, Khaw PT. Flap and suture manipulation after trabeculectomy with adjustable sutures: titration of flow and intraocular pressure in guarded filtration surgery. J Glaucoma 2004;13(5):400-406.
2 Patel S, Pasquale LR. Glaucoma drainage devices: a review of the past,present, and future. Semin Ophthalmol 2010;25(5-6):265-270.
3 Sawchyn AK, Slabaugh MA. Innovations and adaptations in trabeculectomy. Curr Opin Ophthalmol 2016;27(2):158-163.
4 Cairns JE. Trabeculectomy. Preliminary report of a new method. Am J Ophthalmol 1968;66(4):673-679.
5 Loon SC, Chew PT. A major review of antimetabolites in glaucoma therapy. Ophthalmologica 1999;213(4):234-245.
6 Kolker AE, Kass MA, Rait JL. Trabeculectomy with releasable sutures.Arch Ophthalmol 1994;112(1):62-66.
7 Simsek T, Citirik M, Batman A, Mutevelli S, Zilelioglu O. Efficacy and complications of releasable suture trabeculectomy and standard trabeculectomy. Int Ophthalmol 2005;26(1-2):9-14.
8 de Barros DS, Gheith ME, Siam GA, Katz LJ. Releasable suture technique. J Glaucoma 2008;17(5):414-421.
9 Raina UK, Tuli D. Trabeculectomy with releasable sutures: a prospective,randomized pilot study. Arch Ophthalmol 1998;116(10):1288-1293.
10 Kobayashi H, Kobayashi K. A comparison of the intraocular pressure lowering effect of adjustable suture versus laser suture lysis for trabeculectomy. J Glaucoma 2011;20(4):228-233.
11 Savage JA, Condon GP, Lytle RA, Simmons RJ. Laser suture lysis after trabeculectomy. Ophthalmology 1988;95(12):1631-1638.
12 Kapetansky FM. Laser suture lysis after trabeculectomy. J Glaucoma 2003;12(4):316-320.
13 Aykan U, Bilge AH, Akin T, Certel I, Bayer A. Laser suture lysis or releasable sutures after trabeculectomy. J Glaucoma 2007;16(2):240-245.
14 Figus M, Posarelli C, Nasini F, Casini G, Martinelli P, Nardi M.Scleral flap-everting suture for glaucoma-filtering surgery. J Glaucoma 2016;25(1):128-131.
15 Burchfield JC, Kolker AE, Cook SG. Endophthalmitis following trabeculectomy with releasable sutures. Arch Ophthalmol 1996; 114(6):766.
16 Cohen JS, Osher RH. Endophthalmitis associated with releasable sutures. Arch Ophthalmol 1997;115(2):292.