Dear Editor,
Cavernous hemangiomas of the retina are rare benign vascular tumors, commonly diagnosed in children and young adults. They are characterized by dilated blood vessels that form cavities or caverns through which the blood flow is very low or virtually absent[1]. Retinal lesions may be associated with cerebral hemangiomas[1], which conversely,do not harbor any tissue within the malformation, the smooth muscle is impaired and there is no capsule surrounding the caverns. Cavernous hemangioma has also been associated with choroidal hemangioma[2] and ocular melanocytosis[3].Retinal lesions vary in size and location, and generally follow the course of a major retinal vein. While peripheral lesions are usually asymptomatic, loss of vision may occur in case of macular lesions. Ophthalmoscopically, the tumor appears as a cluster of blood-filled dark red saccules with associated fibroglial proliferation that involve the inner retinal layers or the surface of the optic disc[4]. Cavernous hemangiomas are generally non-progressive, but lesion growth, vitreous hemorrhage and epiretinal proliferation have been described[3].The diagnosis is based on fundus examination and confirmed by fluorescein angiography; optical coherence tomography(OCT) features are characteristic[4]. These tumors do not require treatment. Vitrectomy, cryotherapy and laser photocoagulation may be useful in case of vitreous hemorrhage[4]. Herein, we report a case of a retinal cavernous hemangioma identified by imaging optical coherence tomography angiography (OCTA).A 55-year-old woman with a previous diagnosis of cerebral cavernous hemangioma, was admitted to our outpatient clinic for a suspected retinal lesion (Figure 1). The diagnosis of cerebral involvement was made 10y ago; no systemic or retinal symptoms were referred. Her past medical history was unremarkable. The patient has consented to the submission of this Letter for submission to the journal.
Best-corrected visual acuity (BCVA) was 20/20 (Snellen equivalent) in both eyes. Anterior segment findings were unremarkable in both eyes. Fundus examination of the right eye showed, in the supero-temporal quadrant, a grape-like cluster of dark red saccules, suggesting a retinal cavernous hemangioma. There was no evidence of hemorrhage or exudate. Multicolor imaging (Heidelberg Engineering,Heidelberg, Germany) confirmed this typical aspect of the tumor (Figure 1A). The optic nerve, macula and retinal vessels were otherwise normal. The findings obtained in the left eye were unremarkable. Fluorescein angiography showed early hypofluorescence in the tumor mass due to slow filling of the saccular lesions and late staining of the tumor, which had well-defined borders (Figure 1B-1D.) Indocyanine green angiography confirmed the presence of the cavernous hemangioma, and revealed an absence of choroidal vascular involvement (Figure 1E). Spectral-domain optical coherence tomography (SD-OCT) (Heidelberg Engineering, Heidelberg,Germany) revealed hyporeflective vesicular formations within hyperreflective material that corresponded to the separation of the plasma from the blood cells and involved the inner retinal layers (Figure 1F). En face-OCT (Optovue Inc. Fremont, CA,USA) showed multiple hyporeflective lesions surrounded by a hyperrelfective-edged ring (Figure 1G). OCTA (AngioVue software RTVue, Optovue Inc. Fremont, CA, USA ) (3×3 millimeter scan) revealed rarefaction of retinal vessels overlying the tumor and the absence of a flow signal at the superficial and deep plexi (Figure 1H, 1J). No alterations at the outer retina and choriocapillaris segmentation were found. As in polypoidal choroidal vasculopathy[5], slow flow lesions were not visible at OCT. The “slow flow” nature of the lesion may explain the “no flow” aspect of the lesion, thereby confirming the diagnostic potential of OCTA.
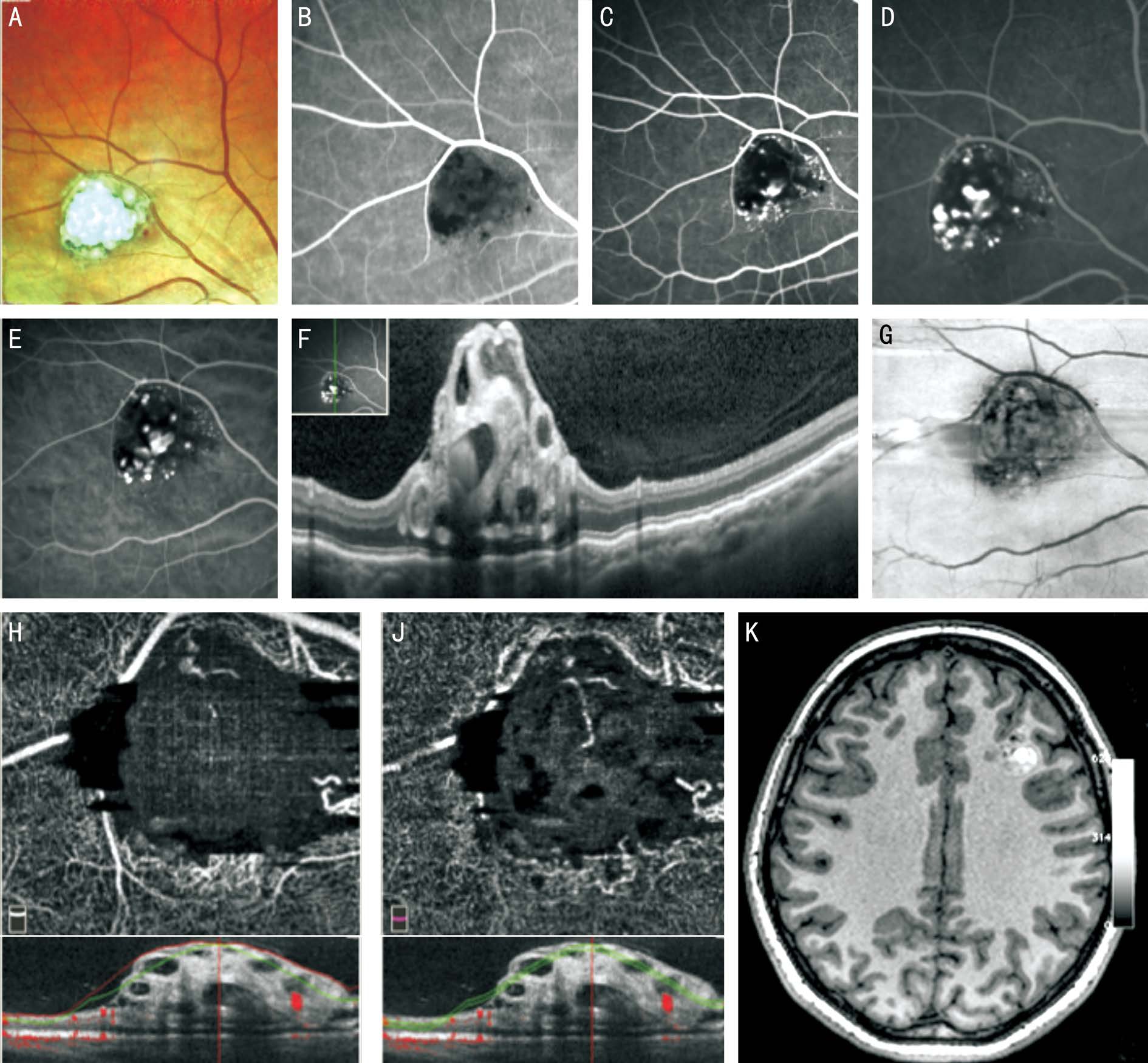
Figure 1 Multimodal imaging of a patient with a retinal cavernous haemangioma A: Multicolor image showing, in supero-temporal quadrant, a retinal cavernous hemangioma; B-E: Fluorescein and indocyanine green angiography of the supero-temporal region revealing, in early phases the slow filling of multiple saccular lesions with staining in late phases; F: SD-OCT showing the presence of multiple hyporeflective vesicular formations, within hyperreflective material, corresponding to the separation of the plasma from the blood cells, involving the inner retinal layer; G: En face-OCT (Optovue Inc. Fremont, CA, USA) showing multiple hyporeflective lesions, sourrounded by a hyperreflective edged-ring; H, J: OCTA showing rarefaction of retinal vessels overlying the tumor and the absence of a flow signal at the superficial and deep plexi; K: At MRI scan, cerebral hemangiomas show the characteristic “popcorn” or “berry” feature with a rim of signal loss due to hemosiderin:the T1 and T2 signals vary upon the entity of blood aging products.
In summary, OCTA revealed unique features in the vascular changes typical of retinal cavernous hemangioma unlike other imaging methods. However, additional studies are needed to determine if OCTA can be an alternative to fluorescein and indiocyanine green angiography in the diagnosis and follow-up cavernous hemangioma of the retina.
ACKNOWLEDGEMENTS
The authors thank Jean Ann Gilder (Scientific Communication srl., Naples, Italy) for editing the manuscript.
Conflicts of Interest: Cennamo G, None; Amoroso F, None;Solari D, None; Alfieri MC, None; de Crecchio G, None.
REFERENCES
1 Gass JD. Cavernous hemangioma of the retina. A neuro-oculo-cutaneous syndrome. Am J Ophthalmol 1971;71(4):799-814.
2 Sarraf D, Payne AM, Kitchen ND, Sehmi KS, Downes SM, Bird AC.Familial cavernous hemangioma: an expanding ocular spectrum. Arch Ophthalmol 2000;118(7):969-973.
3 Zografos L, Gonvers M. Ocular melanocytosis and cavernous haemangioma of the optic disc. Br J Ophthalmol 1994;78(1):73-74.
4 Shields JA, Shields CL. Vascular tumors of the retina and optic disc.In: Shields JA, Shields CL, editors. Intraocular Tumors. A Text and Atlas.Philadelphia: WB Saunders 1992;546-548.
5 Srour M, Querques G, Semoun EH. Optical coherence tomography angiography of idiopathic polypoidal choroidal vasculopathy. Dev Ophthalmol 2016;56:71-76.