Dear Editor,
I am Dr. Khay Wei Poh from Department of Ophthalmology,Hospital Kuala Lumpur, Malaysia. I write to share a case of diffuse choroidal haemangioma in a child with Sturger-Weber syndrome who showed resolution of exudative retinal detachment after a course of photodynamic therapy (PDT)with vertepor fin.
Choroidal haemangiomas are a benign vascular tumour of the choroid, which can be either circumscribed or diffuse[1].Circumscribed choroidal haemangiomas have no systemic association while diffuse choroidal haemangiomas are often associated with Sturge-Weber syndrome. The presentation of a choroidal haemangioma is dependent on its location, with diffuse haemangiomas more likely to cause retinal detachment[2]. Many however are asymptomatic and found incidentally. Treatment is indicated if a patient’s vision is affected or threatened due to exudative retinal detachment, macular oedema or the lesions proximity to the fovea. Haemangiomas that involve the macula often cause reduced vision, metamorphopsia and progressive hypermetropia.
Diffuse choroidal haemangiomas have been treated with many modalities including radiotherapy, anti-vascular endothelial growth factor (VEGF), PDT and argon laser treatment. PDT is an ideal treatment option as it selectively destroys tumour vasculature while sparing the overlying retina[3]. We present our experience in treating a patient who had underlying Sturge-Weber syndrome who presented to us with an exudative detachment secondary to a diffuse choroidal hemangioma. Her condition resolved after one session of PDT with vertepor fin.A 10 years old girl with underlying Sturge-Weber syndrome and epilepsy was referred to us for a right diffuse choroidal haemangioma. She presented with 5-year history of poor vision in her right eye. She was previously treated elsewhere with intravitreal anti-VEGF injections. However, there was no improvement in her condition with gradual worsening of vision.
On examination, she had a port wine stain on the right side of her face involving the ophthalmic and maxillary distribution of trigeminal nerve (Figure 1). Her visual acuity was counting fingers OD, and 20/25 OS. Anterior segments of both eyes were normal with an intraocular pressure of 19 mm Hg OD and 14 mm Hg OS and no evidence of neovascularization or glaucoma. Fundus examination of the right eye revealed a large, diffuse-choroidal haemangioma involving the macula with an inferior exudative retinal detachment, tortuous vessels and a choroidal scar nasal to the optic disc (Figure 2). The left eye had a pink optic disc, cup-to-disc ratio of 0.3 and normal macula. A B-scan ultrasound of the right eye revealed a diffusely thickened choroid (Figure 3). Optical coherence tomography (OCT) of the right eye demonstrated macula oedema with subretinal fluid and intraretinal oedema (Figure 4A).The central retinal thickness of the right eye was 636 µm as compared to 207 µm in the left eye. Fundus fluorescein angiography showed diffuse early hyper fluorescence. She was diagnosed with Sturge-Weber syndrome with diffuse choroidal haemangioma complicated with exudative retinal detachment.As the child was very cooperative, PDT was performed in a clinic setting. One cycle of PDT with vertepor fin (Visudyne),6 mg/m² body-surface area was administered followed immediately by laser treatment at 689 nm delivered at intensity of 600 mW/cm² over 3 contiguous areas each lasting 83s.The area of laser therapy was guided by tumour landmarks obtained with fundus fluorescein angiography.
The patient was reviewed 2wk after the procedure (Figure 4B). Her vision remained counting fingers nevertheless the retinal detachment showed regression with improvement of the macula oedema. Serial OCT scanning was used to monitor treatment response. At 3mo post-procedure, there was further reduction in the macular oedema (Figure 4C) however her vision was status quo until 6mo post procedure when it improved to 20/400 OD. At 10mo post procedure, OCT showed complete resolution of the subretinal exudation. Her vision improved to 20/200 one year post-PDT (Figure 4D).PDT was not repeated in this child as she had stable disease on close clinic monitoring. Her intraocular pressure remains normal with no evidence of neovacular glaucoma.

Figure 1 Photo of this patient with facial naevus flammeus.
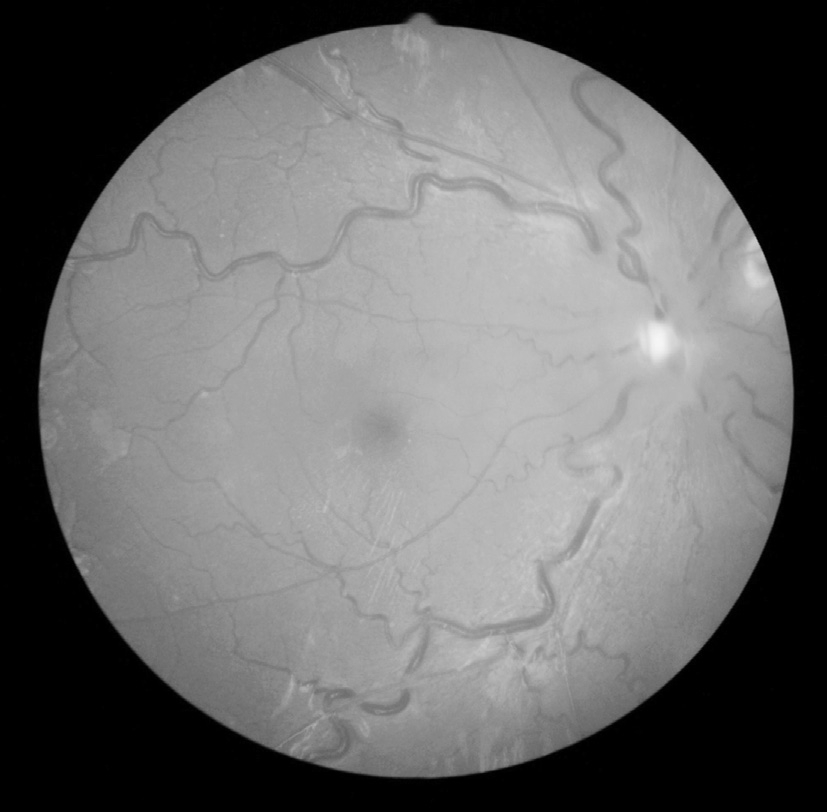
Figure 2 Fundus photo of right eye showing diffuse choroidal haemangioma with exudative retinal detachment involving macula and optic disc swelling.
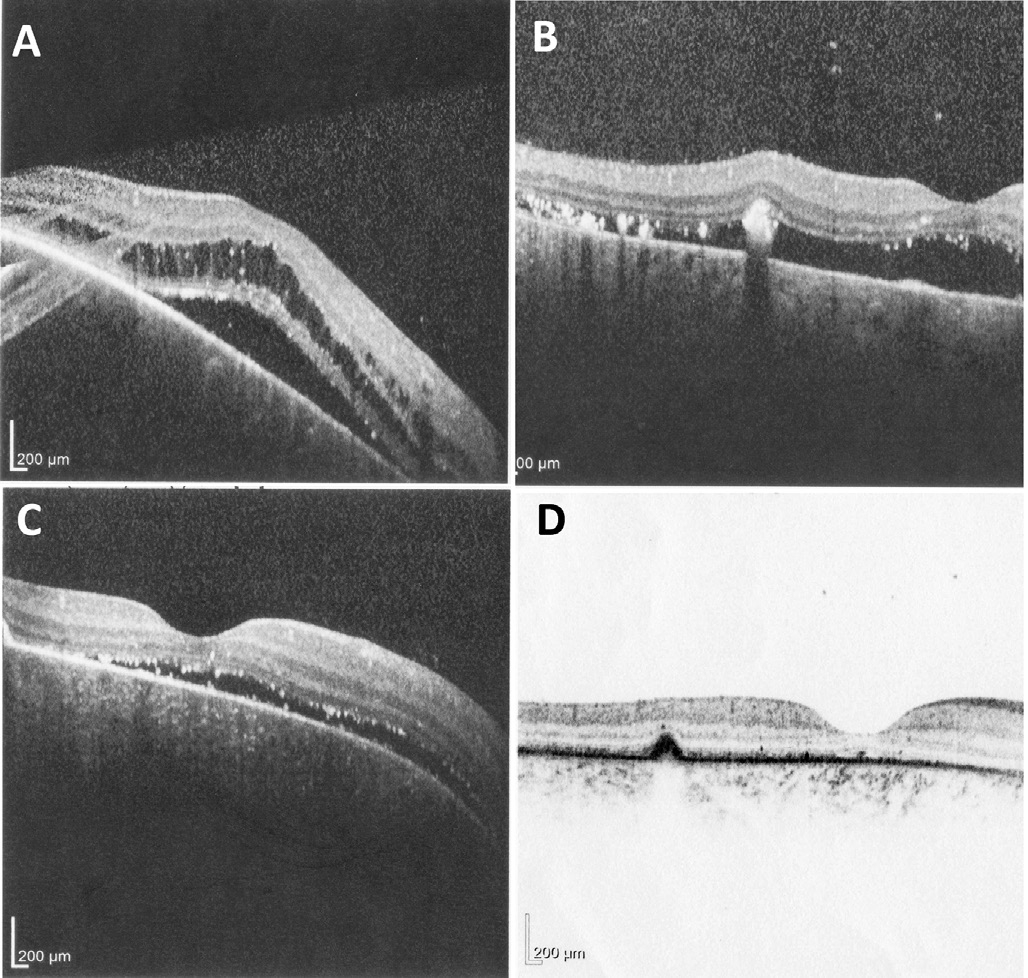
Figure 4 Progression of disease shown on OCT A: OCT of right eye showed macula oedema with subretinal fluid and intraretinal oedema; B: OCT of right eye 2wk after procedure; C: OCT of right eye 3mo after procedure; D: OCT macula of right eye taken one year after PDT.
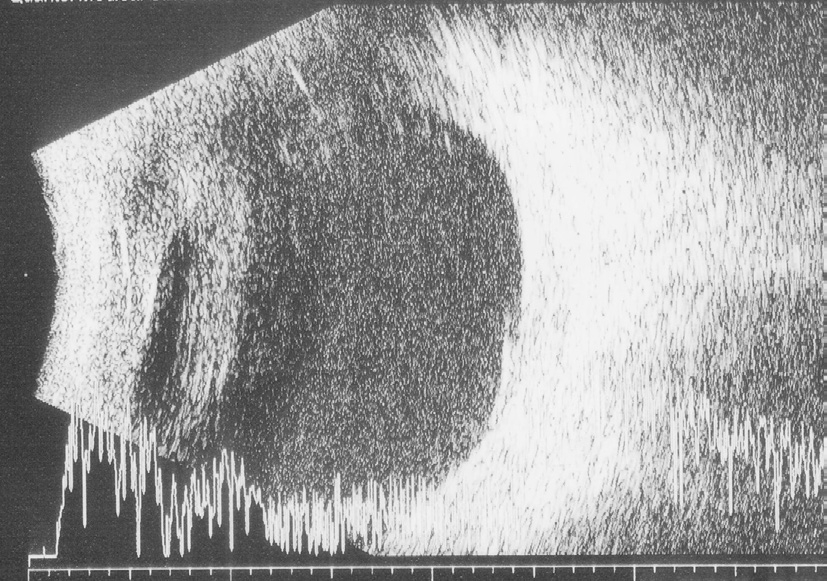
Figure 3 B scan of right eye showing diffuse thickened choroid.
Sturge-Weber syndrome is a rare sporadic disorder that occurs at a frequency of 1 in 50 000 live births. It is characterized by a cutaneous angioma in the distribution of the trigeminal nerve,leptomeningeal angioma and choroidal haemangioma[4].
In Sturge-Weber syndrome, choroidal haemangiomas are often diffuse and ipsilateral to the skin angioma[2]. It often causes severe visual disturbance when complicated with exudative retinal detachment. Treatment of the diffuse choroidal hemangioma and exudative detachment is aimed at improving vision and preventing complications such as neovascular glaucoma[5]. Our treatment goal was to induce tumour atrophy,resolution of subretinal fluid and reduction in tumour induced foveal distortion without destroying the overlying retina.
Treatment options available include laser photocoagulation,radiotherapy, PDT, and anti-VEGF intravitreal injections. PDT has been used successfully in the treatment of circumscribed choroidal haemangioma[6]. It has also been used for the treatment of diffuse choroidal haemangioma and reported cases have demonstrated good outcome in terms of resolution of subretinal fluid, decrease in tumour thickness and improvement in visual outcome. Tumour regression is most dramatic following thefirst session of therapy and should be evident within 3mo. Clinician can consider additional PDT after 3mo if the tumour or fluid persists[7].
Our experience in this case proves that exudative retinal detachment with underlying diffuse choroidal haemangioma can be successfully treated with a single multifocal session of PDT. This is further evidenced by the fact that there complete resolution of subretinal fluid and improvement in visual acuity where the anti-VEGF injections given prior to this had failed.
ACKNOWLEDGEMENTS
Conflicts of Interest: Poh KW, None; Wai YZ, None;Rahmat J, None; Shunmugam M, None; Alagaratnam J,None; Ramasamy S, None.
REFERENCES
1 Witschel H, Font RL. Haemangioma of choroid. A clinicopathologic study of 71 cases and a review of the literature. Surv Ophthalmol 1976;20(6):415-431.
2 Tsipursky MS, Golchet PR, Jampol LM. Photodynamic therapy of choroidal hemangioma in sturge-weber syndrome, with a review of treatments for diffuse and circumscribed choroidalhemangiomas. Surv Ophthalmol 2011;56(1):68-85.
3 Schmidt-Erfurth UM, Michels S, Kusserow C, Jurklies B, Augustin AJ.Photodynamic therapy for symptomatic choroidal hemangioma: visual and anatomic results. Ophthalmology 2002;109(12):2284-2294.
4 Sullivan TJ, Clarke MP, Morin JD. The ocular manifestations of the sturge-Weber syndrome. J Pediatr Ophthalmol Strabismus 1992;29(6):349-356.
5 Monteiro S, Casal I, Santos M, Meireles A. Photodynamic therapy for diffuse choroidal hemangioma in sturge-weber syndrome. Case Rep Med 2014;2014:452372.
6 Medena CA, Singh AD. Diagnosis and management of choroidal hemangiomas. Retinal Physician 2013;10:32-37.
7 Heimann H, Damato B. Congenital vascular malformation of the retina and choroid. Eye (Lond) 2010;24(3):459-467.