INTRODUCTION
Nowadays, there is a vast variety of pupillmrs or the treatment of pre-existing astigmatism at the time of surgery has become increasingly common. Although limbal or corneal relaxing incisions are still popular and are good alternatives to lens-based surgery in cases of low to moderate astigmatism, there is a growing body of literature showing the superiority of toric IOL implantation in terms of visual performance. In a recent systematic review and Metaanalysis evaluating the benefit and harms of toric versus non-toric implantation with or without relaxing incisions,the authors found high-quality evidence that toric IOL implantation provides better uncorrected distance visual acuity, lower residual astigmatism and greater distance spectacle independence than the other approaches without increased risks of complications[1]. However, even with precise preoperative biometry and IOL calculation and proper surgical IOL alignment, optimum refractive outcomes might not be achieved due to postoperative IOL rotation. Generally,though, good refractive and visual outcomes with minimal IOL rotation over a period of 6mo can be achieved with modern hydrophobic and hydrophilic acrylic toric IOLs[2-8]. However,as reported in several studies, axial length superior to 25 mm[2,9-10]and within-the-rule (WTR) astigmatism[2,11] are risk factors for IOL rotation.
In a previous report, we have shown that implantation of the Torica-aA (HumanOptics AG, Erlangen, Germany), a singlepiece hydrophilic toric IOL provided good rotational stability and visual outcomes over a 6-month follow-up period[12].At last follow-up, mean absolute IOL rotation determined by an objective method[13] was 1.99°±1.88° with no rotation exceeding 7.40°, thereby fulf i lling the requirements stated in the international standards (ISO 11979-7:2014) that defined IOL stability as 90% of IOLs rotating less than 10° between the day of surgery and 4-6mo postoperatively.
In the current report, we aim at providing an update on the rotational stability and visual outcomes of the Torica-aA IOL over a 1.5-year follow-up period.
SUBJECTS AND METHODS
This prospective, observational study was designed to evaluate the long-term rotational stability of the Torica-aA IOL(HumanOptics AG) and its efficacy to treat low to moderate astigmatism in cataract patients. The Torica-aA is a hydrophilic acrylic IOL with an optic diameter of 6.0 mm for an overall length of 12.5 mm. It features a C-loop haptic shape without angulation, with a toric meridional aspheric anterior surface(aberration-free) and a 360° sharp square-edge on the posterior surface. The dioptre range is as follows: sphere -10.0 to 35.0 D(0.5 D steps) and cylinder 1.0 to 15.0 D (0.5 D steps). The study was conducted at the Konventhospital der Barmherzigen Brüder, Linz, Austria. The study adhered to the tenets of the Declaration of Helsinki and was approved by the local Ethics Committee. All patients provided written informed consent before enrolment in the study. Patient selection and the methods have been described before[12] and will only be brief l y summarized here. Our study cohort included 40 eyes from 26 patients with senile cataract and regular corneal astigmatism of 1.00 to 2.60 D, a mean axial length (AL) of 23.17±0.88 mm(range 22.04 to 25.23) and a mean anterior chamber depth(ACD) of 3.03±0.31 mm (range 2.41 to 3.62). The mean age at the time of surgery was 72.8±7.9y (range 54 to 85y) and mean IOL power was 20.43±2.13 D (range 16.50 to 24.50) for sphere and 1.66±0.52 D (range 1.00 to 3.00) for cylinder. The majority of eyes (n=18) had WTR astigmatism while againstthe-rule (ATR) and oblique astigmatism (OBL) were present in 11 eyes in each group. Patients with previous corneal or intraocular surgery and ocular pathology other than cataract were excluded.
IOL power and axis placement were calculated using an online IOL calculator from the manufacturer (www.iol-toric-calculator.com). Three eyes were calculated for myopia as target refraction and all other eyes were calculated for emmetropia(±0.5 D). Preoperatively, with the patients sitting in an upright position, the cornea was marked with two small superficial scratches (BD Eclipse 27G needle; BD Medical, USA) in the 3 and 9 o’clock positions. These small scratches were highlighted with a sterile blue skin-marker pen (ArcRoyal, Ireland) for easier recognition intraoperatively. A secondary marking of the steep corneal meridian was made using a Mendez ring, in order to allow precise alignment of the toric IOL axis. Two experienced surgeons (Jirak P and Schönherr U) performed the surgeries. Following standard phacoemulsif i cation through a 2.6 mm superior clear corneal incision at 90°, the IOL was implanted with an Accuject 2.2 injector (Medicel AG,Switzerland) with an intended rhexis size of approximately 5 mm.After polishing the posterior capsule and anterior capsular rim, the IOL was rotated into a position circa 10° short of the marked meridian before the residual ophthalmic viscosurgical device ProVisc (Alcon, Inc., USA) was removed from behind the IOL and from the anterior chamber. Finally, the IOL was rotated to align with the reference marks on the cornea, before sutureless wound closure.
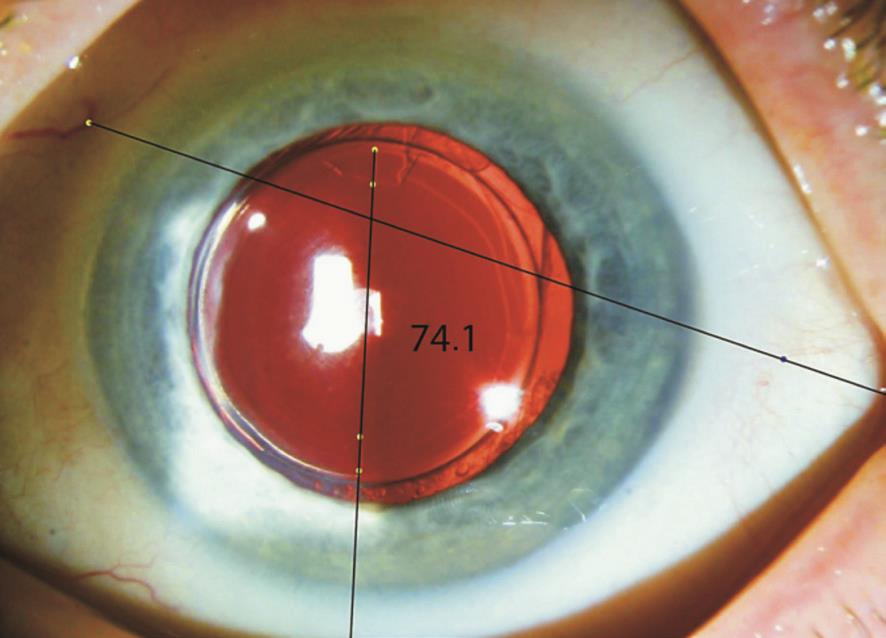
Figure 1 A retroilluminated picture of the Torica-aA IOL 1.5-year after implantation The reference axis is drawn by joining two consistently identif i able conjunctival vessels and the comparison axis is determined by joining the 2 toric markings. The software calculates the angle between the 2 axes (in this picture the angle is 74.1°). The difference between the angle measured at baseline and the angle measured at each follow-up is def i ned as the angle of rotation of the IOL.
Study Outcomes Patients were examined before surgery and at 1d, 1wk, 6mo and 1.5y after surgery. In the fi rst report,the IOL rotational stability, astigmatism correction and visual outcomes were evaluated over a 6-month follow-up period[12].Here, we examined whether there were changes in the IOL performance between the 6-month and 1.5-year visits.
Postoperative IOL position was determined using digital retroillumination images taken at each follow-up and analysed according to the objective method described by Wolffsohn and Buckhurst[13]. For each photo, the angle between the reference axis and the comparison axis was calculated with the Adobe Photoshop software (version CS5, Figure 1). IOL rotation was defined as the difference between the angles measured at baseline (24h) and at each follow-up. The same person performed the evaluation throughout the duration of the study and only good quality pictures were used. Additionally, IOL position was evaluated via slit lamp examination using an axis graticule integrated eye-piece.
Uncorrected and corrected distance visual acuity for far (UDVA,CDVA) and near (UNVA, DCNVA) was tested using the respective ETDRS charts for far (4 m) and near (40 cm) vision.Corneal and refractive astigmatism values were converted to power vectors of crossed cylinders J0 and J45 according to the method described by Thibos and Horner[14]. The J0 component expresses the power of a Jackson cross-cylinder with its axes at 180° and 90° and the J45 component expresses the power of a Jackson cross-cylinder with its axes at 45° and 135°.
Astigmatism vector analysis was determined from corneal astigmatism readings using preoperative keratometry (IOLMaster)values compared to the subjective refraction 6-month and 1.5-year postoperatively. All refractive data were adapted to the corneal plane.
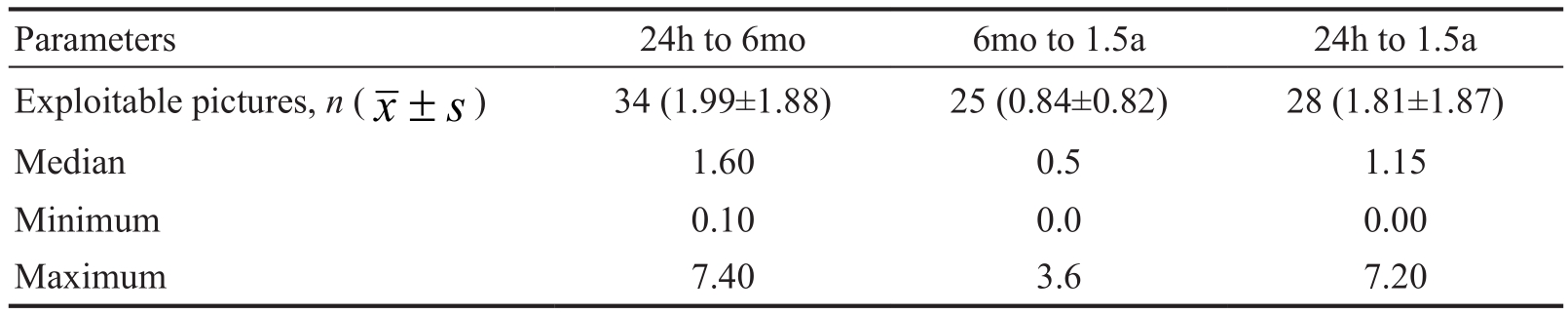
Table 1 Absolute IOL rotation (degrees) overtime (Photoshop method)
Statistical Analysis Statistical analysis was performed using Analyse-it® software, version 4.65.2 (Analyse-it Software,Ltd., Leeds, UK). Continuous variables such as age, axial length, IOL power, visual acuities and angle of IOL rotation were summarized with descriptive statistics (n, mean,standard deviation, median and range). The paired Wilcoxon test was used for comparative statistics. The Spearman rank correlation method was used to analyse potential correlations between parameters. Differences were considered statistically signif i cant when the Ρ-value was less than 0.05.
RESULTS
The study enrolled 40 eyes of 26 patients [19 women (29 eyes); mean age: 72.8±7.9y]. All patients attended the 1.5 years postoperative visit [mean follow-up period =18.2±1.1mo(range 16.7 to 24.3mo)]. One eye of a patient with bilateral IOL implantation developed severe retinal detachment between the 6-month and 1.5-year period resulting in significant decreased visual acuity. The visual outcome of this eye was therefore excluded in the data analysis. None of the eyes required neodymium: YAG laser capsulotomy.
Rotational Stability No patient required secondary IOL repositioning during the course of the study. While measurements of IOL axis position at last follow-up could be recorded for each eye on slit-lamp examination (subjective method,n=40), this was not always possible with the digital pictures because of changes in the appearance of the conjunctival blood vessels with time or too dark images. Exploitable pictures for comparison between 24h vs 6mo and 24h vs 1.5y were available in 34 eyes and 28 eyes, respectively.
Table 1 shows the absolute IOL rotation over time measured with the objective method (Photoshop). The mean IOL rotation was 1.81°±1.87° at 1.5-year with 78.6% of eyes having IOL rotation <3°, 92.9% of eyes <5° and 100% of eyes <8°.Between the 6-month and 1.5-year follow-ups, mean absolute IOL rotation was 0.84°±0.82° (median 0.5°, range 0.0° to 3.6°)and in the majority of cases (96%, n=27), IOL rotation was<2°. There was no signif i cant difference between IOL rotation between the 6-month and the 1.5-year follow-ups (Ρ=0.58).
When IOL rotation was evaluated in the same eyes on slit lamp examination (n=28), mean IOL rotation at 1.5-year was 2.21°±2.93° (median 1.75°, range 0.0° to 10°). Finally, when all eyes were included (n=40) mean absolute IOL rotation was 2.73°±2.89° (median 2°; range 0.0° to 10°). The percentage of IOLs rotating ≤5° was 85% at 1.5-year with no IOL rotating more than 10°.

Figure 2 Vector analysis of astigmatic data Scatterplot of astigmatic vectors J0 and J45, preoperatively and 1.5-year postoperatively. The origin of the graph represents an eye free of astigmatism.
There was no statistically signif i cant correlation between age,gender, astigmatism type, AL, ACD or IOL power and the degree of postoperative IOL rotation measured objectively and subjectively.
Refraction and Visual Acuity There was no significant change in any of the outcome variables between 6mo and 1.5y postoperatively. At last follow-up, mean spherical equivalent was -0.23±0.80 D (range -3.10 to 0.75) with 68% of eyes within ±0.50 D of target refraction, 92% within ±1.00 D, and 97% within ±1.25 D. Mean subjective residual refractive astigmatism was -0.60±0.40 D (range -1.50 to 0.00) and was within ±0.50 D in 69% of the eyes and within 1.00 D in 90% of eyes. The changes in astigmatic power vector (J0, J45) between preoperative corneal keratometric astigmatism (IOLMaster)and postoperative refractive astigmatism are shown in Figure 2.The vector component J0 decreased signif i cantly after surgery(Ρ<0.0001). The mean absolute change in astigmatism was 0.76±0.40 D (median 0.80, range 0.14 to 1.88 D). The mean J45 vector was close to zero preoperatively (0.06±0.36 D) and postoperatively (0.00±0.17 D) and did not change signif i cantly(Ρ=0.28).Table 2 shows the visual acuity over time. At last followup, the eyes targeted for emmetropia (n=36) achieved mean UDVA of 0.09±0.12 (20/25) with 94% of eyes having 20/40 or better and 74% of eyes having 20/25 or better. The 3 eyes with myopic target refraction achieved UNVA of 20/20 or better.Regarding CDVA, 97% of eyes (n=38) achieved 20/32 or better including 79% of eyes having 20/20 or better.
Table 2 Monocular visual acuity within 1.5-year after the Torica-aA implantation

UDVA: Uncorrected distance visual acuity; CDVA: Corrected distance visual acuity; UNVA: uncorrected near visual acuity;DCNVA: Distance-corrected near visual acuity. a1.5-year results compared with before surgery. b1.5-year results compared with 6mo results.
DISCUSSION
In the current study, the Torica-aA IOL, a 1-piece hydrophilic acrylic lens with C-loop haptics, showed good long term rotational stability over a 1.5-year follow-up period with a mean absolute rotation (vs 24h) of 1.81°±1.87° at last visit(objective technique). In the majority of cases, IOL rotation was <3° (78.6%) and no IOL rotated more than 7.2°. Between 6-month and 1-year, the mean IOL rotation was minimal(0.84°±0.82°) with IOL rotation <2° in 96% of eyes. The outcome at 1.5-year was not significantly different from the 6-month visit (1.99°±1.88°, Ρ=0.58), indicating that the IOL was stable 6-month postoperatively.
Very few studies have investigated long-term stability of toric IOLs and compared IOL rotation between different points in time. Nonetheless, our results are consistent with those of others showing that IOLs do not rotate signif i cantly beyond 3-month postoperatively when the shrinkage of the capsular bag is completed. Prinz et al[15] found mean postoperative absolute rotation between 6-month and 1-year of approximately 1.2° for the C-loop haptic IOL (Acri.Lyc 53N) and approximately 1.5° for the plate-haptic IOL (Acri.Smart 46S). Similarly, in a large study involving 378 eyes,the Acrysof IQ toric SN6AT IOL showed good stability over the long term with minimal rotation between the 3-month and 1-year visits (1.9°±2.3°) and between the 1-year and 2-year visits (1.0°±1.2°)[2]. Likewise, Mencucci et al[16] reported negligible rotation of the AT Torbi 709M IOL between 3-month and 6-month with a mean absolute IOL rotation of 0.34°±0.24°.Slightly worse outcomes have been reported by Kwartz and Edwards[17] with a mean absolute rotation of the Akreos Adapt and AcrySof SA60AT IOLs of approximately 3.2° between the 3-month and 2-year follow-up visits. Although IOL rotation was usually <10°, the authors concluded that IOLs continue to show some tendency to rotate for up to 2-year postoperatively.It seems likely that the higher IOL rotation found in the latter study results from the accuracy of measuring IOL rotation,which is dependent of the method used. Although Kwartz and Edwards[17] used digital images, the cyclorotation of the eye was not taken into account between two measurements, which has been shown to be in average 2.3° but could be as high as 11.5°[13,18-19]. Overall, the results of the aforementioned studies and ours suggest that beyond 3-month postoperatively, the lens design (1-piece vs 3-piece), the haptic design (C-loop vs plate), the lens materials (hydrophilic vs hydrophobic) and the IOL overall length (from 10.5 to 13 mm) do not seem to play a major role in IOL stability.
In the current study, the main drawback was that not all digital retroillumination images were exploitable due changes in the appearance of the conjunctival blood vessels with time and too dark images. Hence, IOL rotation through slit lamp examinations was also evaluated. If this subjective approach doesn’t allow very precise IOL alignment measurements, it has the advantages of being easy and fast to handle. Thus,when IOL rotation was subjectively measured in the eyes for which objective data were also available (Table 1), we found an absolute mean rotation of 2.21°±2.93° at 1.5-year with an absolute mean difference of 0.41° vs the objective method.Although IOL rotation measured with the slit lamp method yielded overall slightly higher values, we considered this approach satisfactory to give an estimation of the lens rotation in all eyes: we found a mean absolute rotation of 2.73°±2.89°(n=40: median 2°; range 0.0° to 10°) from 1d to 1.5-year including 85% of the IOLs rotating <5° and with no IOL rotating more than 10°.
The rotational stability of the Torica-aA beyond 6-month postoperatively was consistent with the refractive and visual outcomes. At last follow-up, mean subjective residual refractive astigmatism was not signif i cantly different from the 6-month follow-up and was 0.60±0.40 D (range -1.50 to 0.00), with 69% of the eyes within ±0.50 D and 90% within 1.00 D. As mentioned in our previous report[12], since the IOL power was not calculated taken into account the surgically induced astigmatism along the 90° meridian (0.48±0.41 D), the lens effectiveness was possibly reduced[20].
When considering visual performance, there was no signif i cant difference between the two follow-ups in terms of uncorrected and distance-corrected visual acuities. At last visit, mean UDVA and CDVA was 0.09±0.12 logMAR and -0.01±0.12 logMAR,respectively. These data compare well with those of a previous study in which the visual performance of the same IOL without toricity [Aspira-aA(Y)] was investigated 1-year postoperatively[21]. Similarly, in both studies, no significant postoperative long-term complications such as capsular fibrosis/opacification were observed. Neodymium:YAG laser posterior capsulotomy was not required in the current study and was performed 11-month postoperatively in 2 eyes only(4%, n=47) in the study by Küchle[21]. The surgical techniques(capsulorhexis size, capsule polishing) combined with an IOL with a 360° sharp square-edge barrier are likely to have contributed to these satisfactory outcomes.
The major limitations of this study are the small number of exploitable images available to measure objectively IOL rotation, particularly at the 1.5-year follow-up, as well as the narrow range of AL in our series (22.04-25.23 mm) that did not allow us to determine whether AL superior to 25 mm could be a potential risk factor[2,9-10] for the Torica-aA rotational stability.Moreover, the lack of a comparison group implanted with another model of toric IOL with C-loop haptic design may be considered as another key limitation.
In conclusion, our data show good rotational stability and visual performance of the Torica-aA over a period of 1.5-year without any postoperative complications. Additional comparative studies with larger patient cohorts are needed to strengthen our results.
ACKNOWLEDGEMENTS
Presented in part at the XXXIV Congress of the European Society of Cataract and Refractive Surgeons (ESCRS),Copenhagen, Denmark, September 11, 2016.
Conflicts of Interest: Gyöngyössy B, None; Jirak P, None;Schönherr U, None.
REFERENCES
1 Kessel L, Andresen J, Tendal B, Erngaard D, Flesner P, Hjortdal J. Toric intraocular lenses in the correction of astigmatism during cataract surgery:a systematic review and meta-analysis. Ophthalmology 2016;123(2):275-286.
2 Miyake T, Kamiya K, Amano R, Iida Y, Tsunehiro S, Shimizu K. Longterm clinical outcomes of toric intraocular lens implantation in cataract cases with preexisting astigmatism. J Cataract Refract Surg 2014;40(10):1654-1660.
3 Hirnschall N, Hoffmann PC, Draschl P, Maedel S, Findl O. Evaluation of factors influencing the remaining astigmatism after toric intraocular lens implantation. J Refract Surg 2014;30(6):394-400.
4 Ferreira TB, Almeida A. Comparison of the visual outcomes and OPD-scan results of AMO Tecnis toric and Alcon Acrysof IQ toric intraocular lenses. J Refract Surg 2012;28(8):551-555.
5 Bachernegg A, Ruckl T, Riha W, Grabner G, Dexl AK. Rotational stability and visual outcome after implantation of a new toric intraocular lens for the correction of corneal astigmatism during cataract surgery. J Cataract Refract Surg 2013;39(9):1390-1398.
6 Kasthurirangan S, Feuchter L, Smith P, Nixon D. Software-based evaluation of toric IOL orientation in a multicenter clinical study. J Refract Surg 2014;30(12):820-826.
7 Ferreira TB, Berendschot TT, Ribeiro FJ. Clinical outcomes after cataract surgery with a new transitional toric intraocular lens. J Refract Surg 2016;32(7):452-459.
8 Vale C, Menezes C, Firmino-Machado J, Rodrigues P, Lume M,Tenedório P, Menéres P, Brochado Mdo C. Astigmatism management in cataract surgery with Precizon(®) toric intraocular lens: a prospective study. Clin Ophthalmol 2016;10(1):151-159.
9 Shah GD, Praveen MR, Vasavad AR, Vasavada VA, Rampal G,Shastry LR. Rotational stability of a toric intraocular lens: inf l uence of axial length and alignment in the capsular bag. J Cataract Refract Surg 2012;38(1):54-59.
10 Zhu X, He W, Zhang K, Lu Y. Factors inf l uencing 1-year rotational stability of AcrySof Toric intraocular lenses. Br J Ophthalmol 2016;100(2):263-268.
11 Koshy JJ, Nishi Y, Hirnschall N, et al. Rotational stability of a singlepiece toric acrylic intraocular lens. J Cataract Refract Surg 2010;36(10):1665-1670.
12 Gyöngyössy B, Jirak P, Schönherr U. Rotational stability and patient satisfaction after implantation of a new toric IOL. Eur J Ophthalmol 2016;26(4):321-327
13 Wolffsohn JS, Buckhurst PJ. Objective analysis of toric intraocular lens rotation and centration. J Cataract Refract Surg 2010;36(5):778-782.
14 Thibos LN, Horner D. Power vector analysis of the optical outcome of refractive surgery. J Cataract Refract Surg 2001;27(1):80-85.
15 Prinz A, Neumayer T, Buehl W, Vock L, Menapace R, Findl O,Georgopoulos M. Rotational stability and posterior capsule opacif i cation of a plate-haptic and an open-loop-haptic intraocular lens. J Cataract Refract Surg 2011;37(2):251-257.
16 Mencucci R, Favuzza E, Guerra F, Giacomelli G, Menchini U. Clinical outcomes and rotational stability of a 4-haptic toric intraocular lens in myopic eyes. J Cataract Refract Surg 2014;40(9):1479-1487.
17 Kwartz J, Edwards K. Evaluation of the long-term rotational stability of single-piece, acrylic intraocular lenses. Br J Ophthalmol 2010;94(8):1003-1006.18 Viestenz A, Seitz B, Langenbucher A. Evaluating the eye's rotational stability during standard photography: effect on determining the axial orientation of toric intraocular lenses. J Cataract Refract Surg 2005;31(3):557-561.
19 Viestenz A, Walter S, Viestenz A, Behrens-Baumann W, Langenbucher A. Torische intraokularlinse und astigmatismuskorrektur. Ophthalmologe 2007;104(7):620-627.
20 Visser N, Berendschot TT, Bauer NJ, Nuijts RM. Vector analysis of corneal and refractive astigmatism changes following toric pseudophakic and toric phakic IOL implantation. Invest Ophthalmol Vis Sci 2012;53(4):1865-1873.
21 Küchle M. Comparison of visual function with aspheric yellow,aspheric clear and spherical clear intraocular lenses. J Emmetropia 2013;4(3):123-130.