INTRODUCTION
I ntraocular lens (IOL) explantation is nfrequely performed but is potentially associated with serious complications. The reasons for undergoing explantation are diverse and related to multiple factors, including intraocular comorbidities[1-2]. For example, IOL explantation is sometimes performed after an uneventful cataract surgery. In other cases,it may follow a failed surgery or result from inadequate IOL selection or problems related to the quality of the IOL material or its design. Explantation may also be associated with other intraocular comorbidities that are affected by the presence of the IOL and that may cause later problems. All of the seissues can result in the decision to explant the lens. One study found that the overall rate of explantation is 0.77%[3],while other investigators have found that the incidence of surgery specifically resulting from the late dislocation of an IOL is 0.032%-0.28%[4-5]. A survey of the national China Nine-Province database revealed that the prevalence of cataract surgery in rural China was 2.09%[6]. As there are more than 1.3 billion people residing in China, the issue of cataract removal cannot be ignored in this population.
For all of these reasons, the causes of IOL explantation are epidemiologically important because they can reflect inadequate surgical practices, biomaterials, or IOL design.Further studies would provide important insights into the surgical practice of lens surgery in any given environment.However, in spite of the relevance of such research, few studies have investigated the reasons for IOL explantation in Asian countries[6-7].
The aim of this study is to analyze the demographic characteristics of explantation patients and the different reasons that patients undergo IOL explantation. We included 69 eyes in 67 Chinese patients, and we analyzed the outcomes following explantation surgery to increase our understanding of the management of these cases.
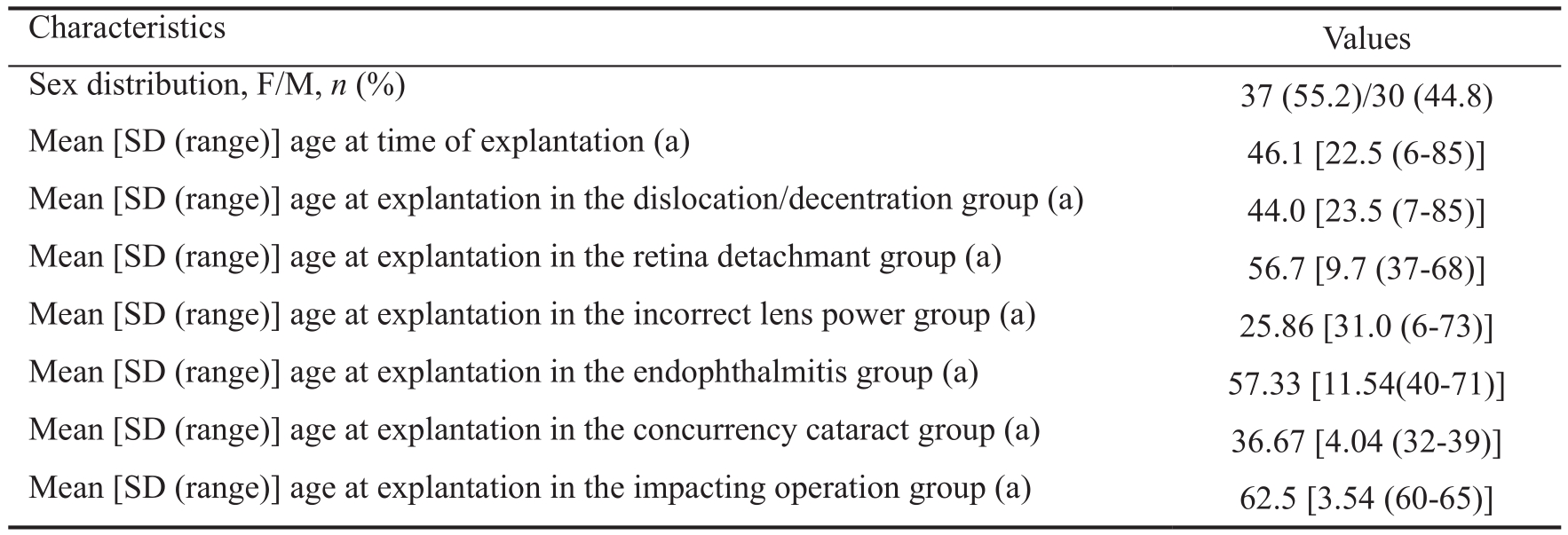
Table 1 Patients’ demographic data
SUBJECTS AND METHODS
This study was designed as a retrospective series of cases. We evaluated IOLs that were explanted in Shaanxi Ophthalmic Medical Center from 2013 to 2014. The primary procedure in these cases was cataract extraction, which was, in some cases, combined with retina surgery. Patient data and clinical data, including the cause of explantation, the date of IOL implantation, the date of IOL explantation, and the surgical treatment used for explantation were recorded based on information provided by Shaanxi Ophthalmic Medical Center ophthalmic surgeons. Informed consent was obtained from all individual participants included in the study. A degree of myopia greater than -6 D was def i ned as high myopia. The IOL explants were stored using adequate preservation conditions for further morphological studies. All IOL exchange surgeries were performed by different surgeons. The surgical approaches included the following:
1) Simple IOL explantation combined with or without IOL implantation: retrobulbar anesthesia was applied using 2% lidocaine in all cases. After a 1.0 mm-sized corneal paracentesis incision was made at the temporal side, a superior scleral tunnel incision was made with a width of approximately 5-6 mm. The ophthalmic viscoelastic device was then introduced into the anterior chamber to relieve adhesion between the lens capsule and the IOL. After the IOL was safely removed, non-IOL was implanted or a new foldable posterior chamber IOL was inserted into either the capsular bag or the ciliary sulcus. Finally, the viscoelastic device was removed using irrigation and aspiration, and the scleral wound was closed using interrupted 10-0 nylon sutures.
2) IOL explantation associated with anterior vitrectomy:same procedure with approach 1, and then a 23-gauge needle with a bent tip was used to relieve adhesion between the lens capsule and the IOL. The vitreous body in the anterior chamber was cut after the IOL was safely removed, and non-IOL was implanted or a new foldable posterior chamber IOL was inserted into either the capsular bag or the ciliary sulcus.Finally, the viscoelastic device was removed using irrigation and aspiration, and the scleral wound was closed using interrupted 10-0 nylon sutures.
3) IOL explantation associated with vitrectomy: same procedure with approach 1, and then a routine vitrectomy three-channel incision was made using a vitreous cutting operation. After vitrectomy, the IOL was floated into the plane of the pupil using heavy water, and then rotated to the iris surface in the anterior chamber and removed. Next, non-IOL was implanted or a new foldable posterior chamber IOL was inserted into either the capsular bag or the ciliary sulcus.Finally, the scleral wound was closed using 7-0 absorbable suture.
The following data were also retrieved when available: type of initial cataract surgery, power and material of the initially implanted IOL, site of IOL implantation, biometric data used for IOL calculations (for both the initial and exchange procedures), IOL calculation formula, and BCVA and refractions after the initial IOL implantation.
Statistical Analysis All data were analyzed using SPSS for Windows software (version 20.0, SPSS, Inc.). Chi-square tests were used to compare the frequencies across all causes of IOL explantation.
RESULTS
A total of 69 explanted pseudophakic IOLs were studied,including 37 in women (55.2%). The mean age of the patients at the time of explantation was 46.1 years old [SD 22.5 (range 6-85)] (Table 1).
Regarding the patients’careers, 47.8% were farmers, 23.9%were retired, 16.4% were students, 4.5% were unemployed,3.0% were workers, 1.5% were staff members, 1.5% were teachers, and 1.5% were off i cers (Figure 1).
The main cause of explantation was dislocation/decentration(Figure 2), which was observed in 41 eyes (59.4%). The second most common cause was retinal detachment (Figure 3),which was observed in 10 cases (14.5%), and the third most common cause was incorrect lens power, which was observed in 7 eyes (10.1%). The remaining causes were endophthalmitis(Figure 4) in 6 cases (8.7%), a concurrent cataract in 3 eyes(4.3%), and an impacting retinal surgery operation in 2 cases(2.9%) (Figures 5, 6).Regarding dislocation/decentration, a subanalysis revealed that the dislocations occurred in the following locations: inferior(71.0%), temporal side (11.6%), nasal side (4.3%), anterior chamber (4.3%), iris capture (1.4%), and missing information(7.2%). The information was missing in 5 eyes (7.2%) because the surgeon forgot to fill in the space regarding dislocation direction (Figure 7).
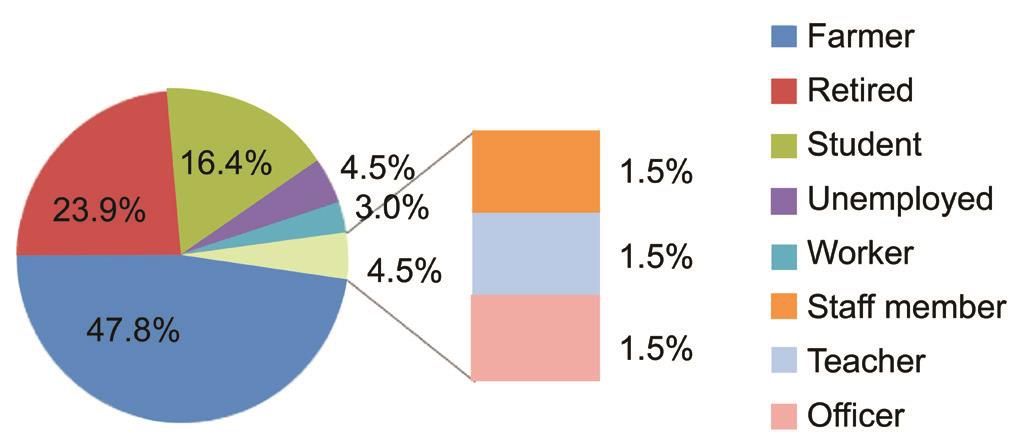
Figure 1 Profession distribution.
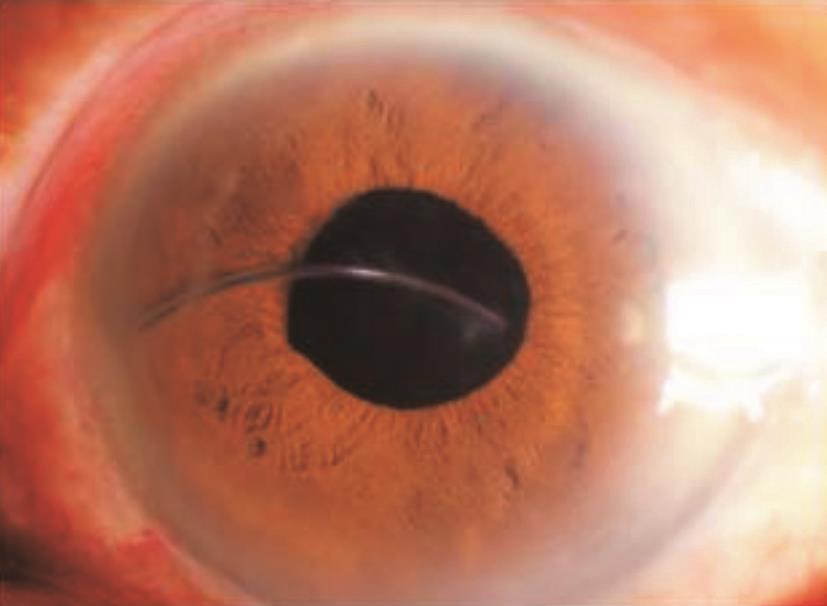
Figure 2 An IOL that dropped into the vitreous in which only the haptic lens could be seen in the anterior intraocular chamber.

Figure 3 Retinal detachment associated with an iris clip in the intraocular lens.
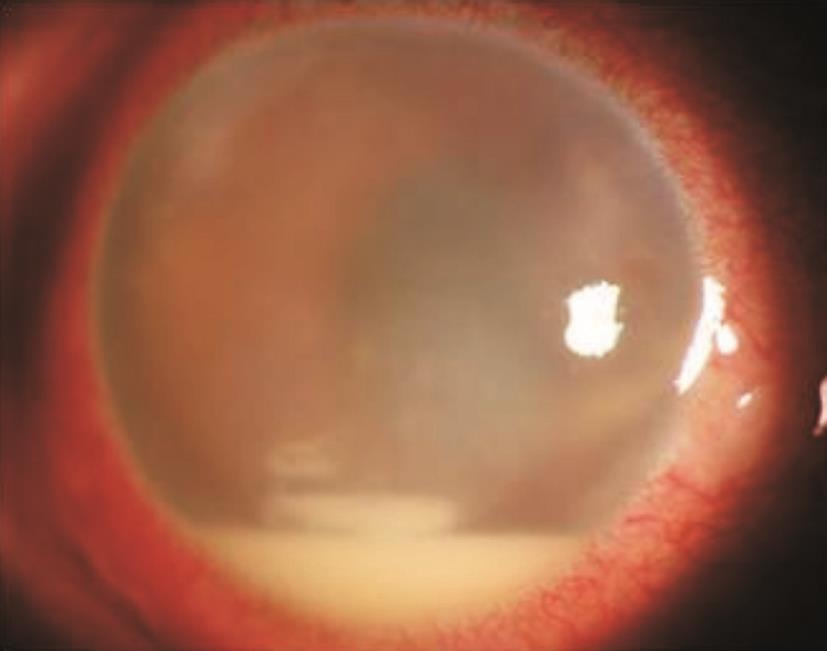
Figure 4 Endophthalmitis with hypopyon.
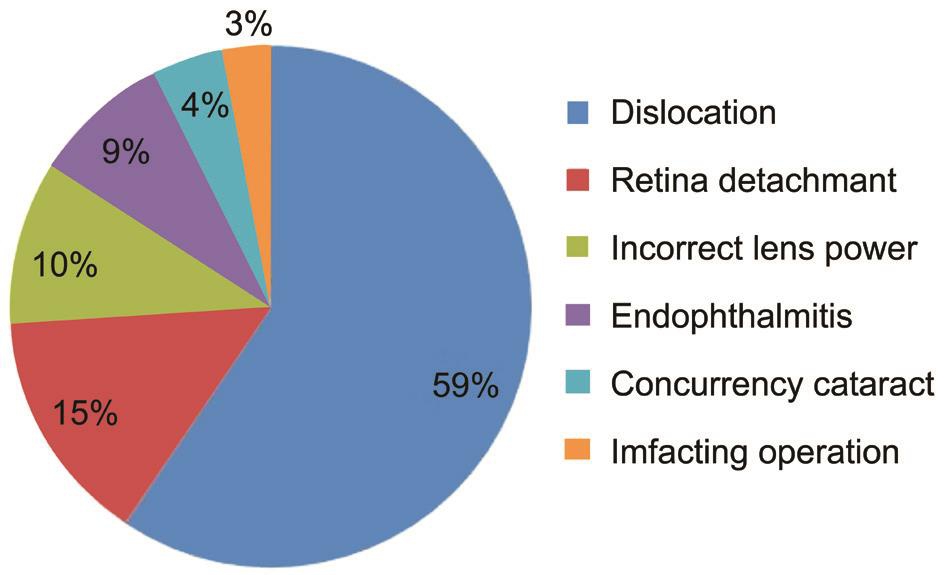
Figure 5 Explantation causes.

Figure 6 Causes of explantation and time implantation to explantation.
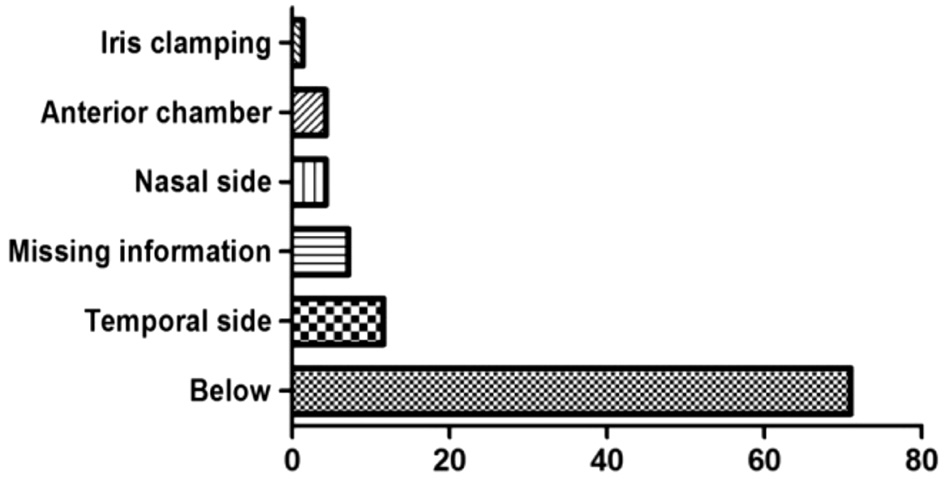
Figure 7 IOL dislocation direction percentage.
The preoperative ocular status was high myopia in 18 eyes(26.1%), trauma in 8 eyes (11.6%), retinal detachment in 6 eyes(8.7%), congenital cataracts in 8 eyes (11.6%), and Marfan’s syndrome in 2 eyes (2.9%). In all, 50 patients underwent one surgery, and 17 patients underwent more than two surgeries.The surgeries included the following procedures: cataract extraction in 64 eyes, implantation of an implantable contact lens (ICL) in 5 eyes, and retinal surgery in 10 eyes (Table 2).
The treatment applied after explantation included posterior chamber IOL implantation in 44 eyes (63.8%). Of these, inthe-bag lens surgery was performed in 12 eyes (17.4%), in-thesulcus surgery was performed in 32 eyes (46.4%), and aphakia was performed in 25 eyes (36.2%). The surgery was combined with vitrectomy or anterior vitrectomy in 40 eyes (58.0%).After the surgical treatment, the best corrected visual ability(BCVA) was improved in 50 cases (72.5%), including 28 patients (40.6%) in whom visual ability was improved by more than two lines (Table 3).
The mean time from IOL implantation to explantation was 4.0y[SD 4.2 (0.005-15)]. In cases with dislocation/decentration,the mean time from implantation to explantation was 4.46y[SD 3.92 (range 0.005-15.0)], and the mean age of the patients was 44 years old [SD 23.50 (range 7-85)]. In cases with retinal detachment, the mean time was 2.11y [SD 2.41 (range 0.05-8.0)], and the mean age was 56.7 years old [SD 9.70 (range 37-68)]. In the patients with incorrect lens power, the mean time was 4.30y [SD 3.30 (range 0.04-10.0)], and the mean age was 25.86 years old [SD 31.0 (range 6-73)]. In the endophthalmitis group, the mean time was 0.17y [SD 0.09 (range 0.005-0.42)],and the mean age was 57.33 years old [SD 11.54 (range 40-71)]. In the concurrent cataract group, the mean time was 2.28y [SD 1.25 (range 0.083-3.0)], and the patient mean age was 36.67 years old [SD 4.04 (range 32-39)]. Finally, in the impacted operation group, the mean time was 3.50y [SD 1.50(range 3.00-4.00)], and the mean age of the patients was 62.50 years old [SD 3.54 (range 60-65)] (Figure 6).
DISCUSSION
Improvements in surgical techniques, the manufacturing of IOLs and their styles have greatly reduced the incidence of major lens-related complications. However, many patients still develop postoperative complications that require IOL explantation or exchange. The preoperative ocular status of the patient is very important when predicting the fi nal clinical outcome of explantation/exchange surgeries. Patients with more severe preoperative ocular problems are more likely than patients with milder problems to achieve less satisfactory outcomes after lens removal or exchange[1,8-11].
Table 2 Preoperative data of patients n (%)
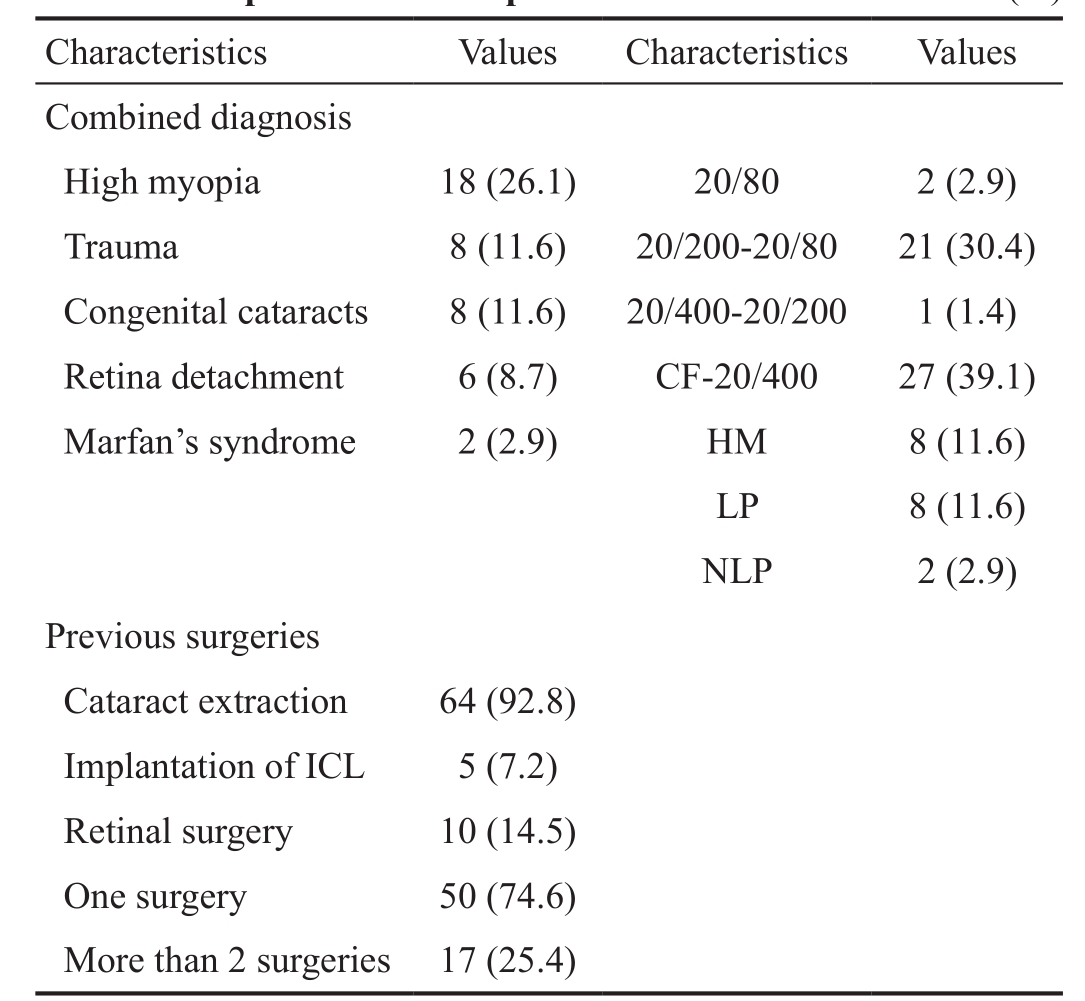
ICL: Implantable contact lens, CF: Count fi nger; HM: Hand movement;LP: Light perception.
Table 3 Postoperative data of patients n (%)
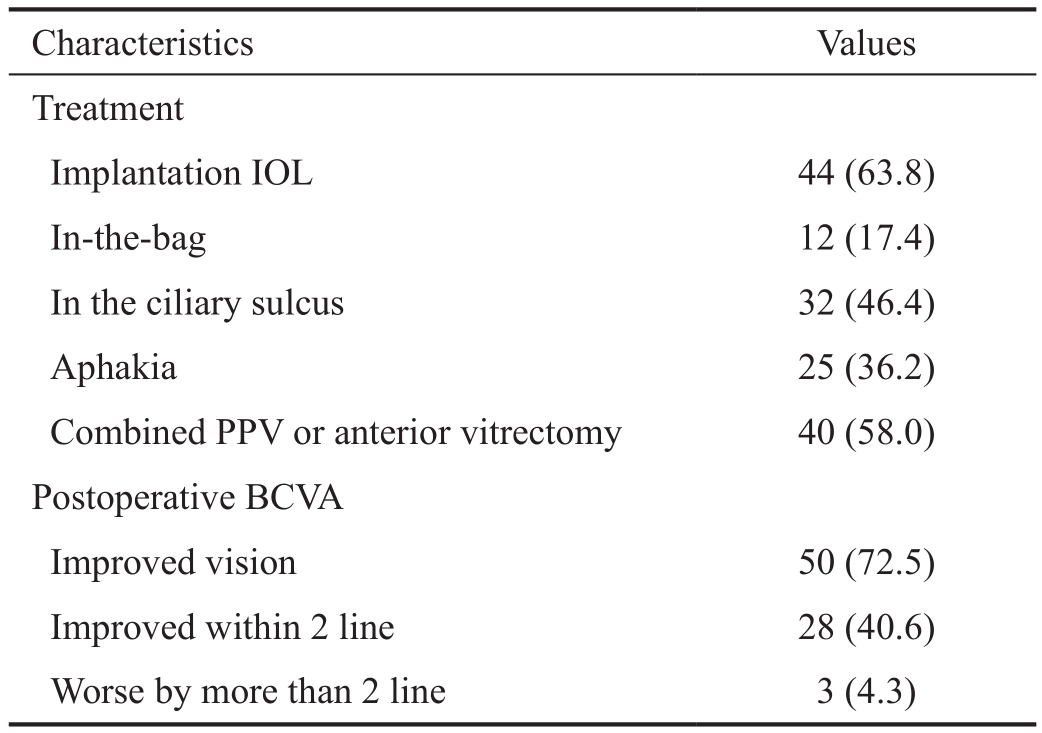
IOL: Intraocular lens; PPV: Pars plana vitrectomy; BCVA: Best corrected visual ability.
This sample population in this study was chosen to open an investigation into the causes and outcomes of explantations.We intend to include more cases based on the results of our analysis of the preliminary data obtained during the completion of this study. Our data show that the leading cause of pseudophakic explantation was IOL decentration/dislocation(59%), followed by retinal detachment (15%) and incorrect lens power (10%). In addition, we also showed that excellent visual recovery was achieved in addition to good results regarding complications.
IOL decentration/dislocation was the leading cause for explantations. The reasons for IOL decentration/dislocation were analyzed and found to include the following: first, lens capsule factors, such as the anterior capsule lacking continuity,posterior capsular rupture or a vitreous postoperative residual lens capsule that was too small and that therefore failed to support the IOL. An IOL implanted in an improper location was another risk factor[12-13]. Second, zonular factors, including suspensory ligament rupture, vitrectomy surgery, and high myopia. High myopia was recorded in 8 cases (19.5%)in dislocation/decentration group. High myopia has been considered a risk factor for late IOL dislocation in some single case reports[6,14-15]. Traumatic cataract was the second reason which was observed in 7 eyes (17.1%). Congenital cataract was observed in 4 cases (9.8%) and Marfan’s syndrome in 2 eyes (4.9%). The common feature of these patients is due to congenital or acquired causes of the abnormal of the sus-pensory ligament or capsule. In some cases, the lens capsule suspensory ligament was too weak to support the IOL, so a dislocation occurred[16-18]. Finally, after cataract surgery, trauma or strenuous exercise were mentioned in the records of 8 patients (19.5%) which lead to dislocation in this study.
Retinal detachment was the second most common cause of explantation, accounting for 15.0% of the cases. This is very different from the fi ndings reported in the American Society of Cataract and Refractive Surgery (ASCRS) and the European Society of Cataract and Refractive Surgeons (ESCRS)surveys[19-20] and other case series reports[21-22], in which the second main cause was incorrect lens. It is because in our study, part of the patients suffered from not only cataracts but also retinal detachment before the surgery. In the patients with retinal detachment, the peripheral visual fi eld was affected by the surrounding visual field along the peripheral part of the line. A combined vitrectomy with removal of the intraocular lens was therefore performed. In 10 eyes (14.5%), cataract surgery combined with vitrectomy was performed. The causes of retinal detachment after IOL implantation were determined to be the following: high myopia, retinal degeneration,intraoperative posterior capsular rupture, vitreous spills and vitreous incarceration[18,23].
Incorrect lens power was the third most common cause of explantation, accounting for 10.0% of the cases. Hence, this condition remains a significant problem, and it is important to obtain accurate IOL measurements. New biometry technologies are becoming available that will help us to obtain more accurate measurements and thereby choose the correct IOL power[24-25]. While some authors, such as Mamalis et al have found even higher rates of explantation resulting from incorrect lens power in their updated studies[26-27], our rate seems too high in the context of modern cataract surgery as it is double the rate reported in other studies[28]. We found congenital cataracts in 5 eyes in 3 children, and we found that axial length increased with age. Therefore, the surgeon had to exchange the IOL to accommodate the new axial length.The IOL parameters that led to errors primarily included axial length and corneal curvature measurement errors because such errors can cause complications following artificial IOL implantation. As children grow and develop, the axial length extends, and the intraocular lens implantation is associated with an increasing degree of myopic refractive error. Hence,the patient does not need to wear glasses to correct for artif i cial lens replacement surgery because visual acuity following IOL replacement surgery is generally good.
In patients with cataracts and complicated cataracts, fi ve eyes were obtained in this group. Three eyes were implanted with an implantable collamer lens, required a postoperative cataract surgery. Of these, one was an age-related cataract that was discovered after the initial cataract surgery, one followed a posterior chamber intraocular lens implantation in a patient with congenital subluxation correction, and refractive errors ahead of the crystallization were caused by complications associated with the cataract.
We found that the risk of IOL explantation was inf l uenced by preoperative ocular status, postoperative complications and the career of the patient. In our study, the highest incidence was observed in farmers. In this population, a lower level of education, poor compliance and limited local medical facilities contributed to this high IOL removal rate. The second mostaffected population was retired individuals, who had a higher rate of age-related cataracts. The relatively low incidence of better outcomes in staff members, teachers and off i cers could beattributable to their relatively stable jobs, fi xed incomes, and better level of medical care.
The overall mean time from implantation to explantation observed in this study was not significantly different from that observed in previous reports[15,26]. The shortest period of time between implantation/explantation was observed in two cases in which endophthalmitis occurred within two days after surgery. The longest interval is observed in one case in which the lens was explanted because the IOL dislocated after 15y.
Additional clinical outcomes that were analyzed included the BCVA, the total number of previous surgeries and the types of complications that occurred before the surgery. Postoperative visual acuity was dependent on preoperative complications that were associated with the explanted intraocular lens. The fi nal visual results observed after modern foldable intraocular lenses were exchanged were uniformly good. This is probably because there are fewer severe complications that can lead to explantation of these intraocular lenses. The BCVA was clearly improved in 50 patients (72.5%) and decreased in only 3 cases(4.3%). These fi ndings and conclusions are generally consistent with those reported in previous research studies[29-30]. Stable vision was def i ned as unchanged vision or acuity that changed within one line of letters (Snellen chart), and decreased vision was def i ned as a loss of vision of two or more lines or a change in another category (e.g. counting fi ngers to hand movements,hand movements to light perception).
Although this is a retrospective study, the size of the included sample population makes our results reliable for showing that IOL explantation is associated with the presence of concurrent cataracts and retinal surgery. We have also shown that dislocation/decentration is currently the leading cause of explantation. Some pre-disposing factors have been previously described. In most cases, a complex bag IOL decenters or dislocates for reasons independent of any surgical error. Our study also has some limitations. The results of this study are limited by the availability of information that could be collected from the clinical reports that were supplied by the referring ophthalmic surgeons. The purpose of this article was not to explore postoperative surgical outcomes following explantation surgery or the techniques used.
In summary, we studied 69 explantation cases in China and found that this population has one of the largest reported coeff i cients of cataract surgery. This demographic information requires further analysis to determine the preventive measures that can be taken to prevent the most frequent causes of explantation and to better predict the outcomes of IOL explantation procedures. In addition, serious complications of IOL implantation surgeries were the most common direct cause of IOL removal. There are many ways to avoid lensrelated complications and to thereby decrease the rate of IOL explantation/exchange. It is most important to use excellent surgical techniques and an intact curvilinear capsulorhexis and to ensure that the IOL is properly placed within the capsular bag. In addition, carefully folding, loading, and inserting the IOL may eliminate many of the problems that are associated with damage to the implant, including the tearing of the lens optic or damaging the lens haptic, both of which require explantation. It is also very important to obtain accurate IOL measurements. New biometry technologies are becoming available that will help us to obtain more accurate measurements and choose the right IOL power for each patient.Proper patient selection and preoperative counseling are important to ensuring that patients have realistic expectations.This is especially important in candidates for intraocular refractive surgery and those with preexisting ocular pathology.In these patients, it is necessary to study a larger sample to verify our hypothesis. In addition, it is also necessary to maintain ongoing vigilance by following and monitoring the development of any new IOL materials and designs because we must be aware of the possibilities of late complications.
ACKNOWLEDGEMENTS
Foundations: Supported by the National Natural Science Foundation of China Grant (No.81273902); the Project of Science and Technology of Social Development Funding(No.2016SF-100); the Construction Program of Xi’an Key Discipline Superiority Specialty (No.[2015] 228-7); the Science and Technology Research and Development Program of Shaanxi Province (No.2014K11-03-07-04).
Conflicts of Interest: Chai F, None; Ma B, None; Yang XG,None; Li J, None; Chu MF, None.
REFERENCES
1 Jin GJ, Crandall AS, Jones JJ. Changing indications for and improvingoutcomes of intraocular lens exchange. Am J Ophthalmol 2005;140(4):688-694.
2 Alió JL, Toffaha BT, Peña-Garcia P, Sádaba LM, Barraquer RI.Phakic intraocular lens explantation: causes in 240 cases. J Refract Surg 2015;31(1):30-35.
3 Stark WJ Jr, Maumenee AE, Datiles M, et al. Intraocular lenses:complications and visual results. Trans Am Ophthalmol Soc 1983;81:280-309.
4 Veselá M, Baráková D, Lenčová A. Analysis of reasons of intraocular lenses explantation. Cesk Slov Oftalmol 2013;69(4):170-173.
5 Jirásková N, Rozsíval P, Kohout A. A survey of intraocular lens explantation: a retrospective analysis of 23 IOLs explanted during 2005.Eur J Ophthalmol 2007 17(4):579-587.
6 Hayashi K, Hirata A, Hayashi H. Possible predisposing factors for inthe-bag and out-of-the-bag intraocular lens dislocation and outcomes of intraocular lens exchange surgery. Ophthalmology 2007;114(5):969-975.
7 Kamiya K, Hayashi K, Shimizu K, Negishi K, Sato M, Bissen-Miyajima H; Survey Working Group of the Japanese Society of Cataract and Refractive Surgery. Multifocal intraocular lens explantation: a case series of 50 eyes. Am J Ophthalmol 2014;158(2):215-220.
8 Zhao J, Ellwein LB, Cui H, Ge J, Guan H, Lv J, Ma X, Yin J, Yin ZQ,Yuan Y, Liu H. Prevalence and outcomes of cataract surgery in rural China. Ophthalmology 2010;117(11):2120-2128.
9 Moshirfar M, Mifflin M, Wong G, Chang JC. Cataract surgery following phakic intraocular lens implantation. Curr Opin Ophthalmol 2010;21(1):39-44.
10 Zheng D, Zhang Z, Yang W, Chen W. Foldable lens explantation and exchange: the reason and solution. Yan Ke Xue Bao 2001;17(1):54-56.
11 Fernández-Buenaga R, Alio JL, Muñoz-Negrete FJ, Barraquer Compte RI, Alio-Del Barrio JL. Causes of IOL explantation in Spain. Eur J Ophthalmol 2012;22(5):762-768.
12 Gross JG, Kokame GT, Weinberg DV. Dislocated In-The-Bag intraocular Lens Study Group. In-the-bag intraocular lens dislocation. Am J Ophthalmol 2004;137(4):630-635.
13 Davis D, Brubaker J, Espandar L, Crandall A, Werner L, Mamalis N.Late in-the-bag spontaneous intraocular lens dislocation: evaluation of 86 consecutive cases. Ophthalmology 2009;116(4):664-670.
14 Fernández-Buenaga R, Alio JL, Pérez-Ardoy AL, Larrosa-Quesada A,Pinilla-Cortés L, Barraquer R, Alio JL 2nd, Muñoz-Negrete FJ. Late inthe-bag intraocular lens dislocation requiring explantation: risk factors and outcomes. Eye (Lond) 2013;27(7):795-801.
15 Stürmer J. Lens exchange for subluxation of posterior chamber lenses implanted in the capsular bag or in the ciliary sulcus. Klin Monbl Augenheilkd 2013;230(4):317-322.
16 Lorente R, de Rojas V, Vazquez de Parga P, Moreno C, Landaluce ML,Domínguez R, Lorente B. Management of late spontaneous in-the-bag intraocular lens dislocation: retrospective analysis of 45 cases. J Cataract Refract Surg 2010;36(8):1270-1282.
17 Wilczyński M, Wilczyńska O, Omulecki W. Analysis of causes of intraocular lens explantations in the material of Department of Ophthalmology,Medical University of Lodz. Klin Oczna 2009;111(1-3):21-25.
18 Werner L, Zaugg B, Neuhann T, Burrow M, Tetz M. In-the-bag capsular tension ring and intraocular lens subluxation or dislocation: a series of 23 cases. Ophthalmology 2012;119(2):266-271.
19 Mamalis N, Davis B, Nilson CD, Hickman MS, Leboyer RM.Complications of foldable intraocular lenses requiring explantation or secondary intervention-2003 survey update. J Cataract Refract Surg 2004;30(10):2209-2218.
20 Mamalis N, Brubaker J, Davis D, Espandar L, Werner L. Complications of foldable intraocular lenses requiring explantation or secondary intervention-2007 survey update. J Cataract Refract Surg 2008;34(9):1584-1591.
21 Marques FF, Marques DM, Osher RH, Freitas LL. Longitudinal study of intraocular lens exchange. J Cataract Refract Surg 2007;33(2):254-257.22 Schmidbauer JM, Apple DJ, Auffarth GU, Peng Q, Pandey SK, Werner L, Escobar-Gomez M, Vargas LG. Complication profiles of posterior chamber intraocular lenses IOL. An analysis of 586 foldable and 2077 rigid explanted intraocular lenses. Ophthalmologe 2001;98(11):1029-1035.23 Davison JA. Capsule contraction syndrome. J Cataract Refract Surg 1993;19(5):582-589.
24 Savini G, Hoffer KJ, Barboni P, Balducci N, Schiano-Lomoriello D, Ducoli P. Accuracy of optical biometry combined with Placido disc corneal topography for intraocular lens power calculation. ΡLoS One 2017;12(2):e0172634.
25 Vasavada AR, Vasavada V. Current Status of IOL implantation in pediatric eyes: an up-date. Expert Rev Med Devices 2017;2:1-9.
26 Leysen I, Bartholomeeusen E, Coeckelbergh T, Tassignon MJ. Surgical outcomes of intraocular lens exchange: fi ve-year study. J Cataract Refract Surg 2009;35(6):1013-1018.
27 McCarthy M, Gavanski GM, Paton KE, Holland SP. Intraocular lens power calculations after myopic laser refractive surgery: a comparison of methods in 173 eyes. Ophthalmology 2011;118(5):940-994.
28 Savini G, Hoffer KJ, Carbonelli M, Barboni P. Intraocular lens power calculation after myopic excimer laser surgery: clinical comparison of published methods. J Cataract Refract Surg 2010;36(9):1455-1465.
29 Sarrafizade R, Ruby AJ, Hassan TS. A comparison of visual results and complications in eyes with posterior chamber intraocular lens dislocation treated with pars plana vitrectomy and lens repositioning or lens exchange. Ophthalmology 2001;108(1):82-88.
30 Al-Halaf i AM, Al-Harthi E, Al-Amro S, El-Asrar AA. Visual outcome and complications of pars plana vitrectomy for dislocated intraocular lenses. Saudi J Ophthalmol 2011;25(2):187-192.