INTRODUCTION
Refractory surgeries bring us many advantages as well as some complications, such as dry eye and reduced corneal sensation. The corneal nerves are cut during the flap creation and stromal ablation, which reduce the corneal sensation, tear production and increase tear evaporation[1]. The exact pathophysiology of dry eye after refractive surgery still remains uncertain. However, neurotrophic epitheliopathy due to the damage of sub-basal nerve plexus has been considered one of the major contributing factors[2]. Refractive surgery is very popular for myopia in recent years, especially small incision lenticule extraction (SMILE) and femtosecond laserassisted in situ keratomileusis (FS-LASIK).
The rapid development of femtosecond lasers over the past two decades has opened up new applications in ophthalmic surgery.The femtosecond laser has been widely applied in LASIK,which offers the creation of more predictable fl aps with regard to flap thickness, diam eter, and hinge width[3]. Although this technique has improved a lot nowadays, many studies have found that some side effects could not be avoided, such as astigmatism, aningeresting, changes of corneal hysteresis(CH), corneal resistance factor (CRF), photaesthesia or total higher order aberration (tHOAs), due to the damaged corneal surface[4-6].
SMILE has been considered as advanced technology to correct myopia and myopic astigmatism. Contrary to LASIK, the fl ap is needless in the process of SMILE with the replacement of the shorter side cut, which is used for lenticule extraction and about 3 to 4 mm[7]. This all-in-one surgery no longer needs a full fl ap cut. Agca et al[8] found that SMILE is better in the nerve fiber regeneration. Some studies have reported that patients applied with SMILE surgery have low incidence of dry eye syndrome and central corneal sensation reduction,although others don’t stay the same[9].
In order to evaluate the ocular surface function after refractive surgeries, many clinical studies have been carried out.However, SMILE, an advanced technique carried out in recent years, whether is superior to FS-LASIK in ocular surface function, remains unclear. And the comparison of these two kinds of techniques in dry eye and corneal sensation is not available. The objective of this Meta-analysis was to analyze the incidence of dry eye and changes in corneal sensitivity after these two kinds of refractive surgeries.
MATERIALS AND METHODS
The Meta-analysis was performed following the methods which has been universally accepted[10].
Search Strategy We searched on PubMed with language restriction from inception to March 2016. The key words we used for searching were “SMILE”, “LASIK”, “femtosecond”,“SMILE and LASIK”, “dry eye”, “corneal sensation”, “corneal sensitivity” and “ocular surface”. The potentially eligible articles were identif i ed according to the reference lists after our fi ltering.Inclusion and Exclusion Criteria We formulated inclusion and exclusion criteria to screen the retrieved articles. The four inclusion criteria were shown below. At first, either randomized or nonrandomized trials were included in our analysis. Secondly, we chose the myopic patients with or without astigmatism, and the myopic degree ranged from -2 to-10 degrees. Thirdly, the studies with the comparison between SMILE and FS-LASIK were accepted. In addition, the main outcomes we observed included Ocular Surface Disease Index(OSDI) scores, tear fi lm break-up time (TBUT), Schirmer Test and corneal sensitivity. We extracted the datum before surgery and within the six month follow-up. The exclusion criteria included reviews, meetings, letters, studies without complete data, with inconsistent or erroneous data and some duplicate publications.
Screening Process Two independent reviewers (Cai WT and Wei QQ) search on the database and fi lter the studies according to our predef i ned criteria. We reach the agreements after our discussion. We exclude the studies which report the same clinical trials and select the one latest.
Quality Assessment We used the validated Downs and Black scale to conduct our quality assessment because the studies included both randomized and nonrandomized ones[11]. The evaluation indexes are shown as followed, such as reporting,external validity, internal validity (bias and confounding), and power[12]. Two authors (Ren CD and Liu QY) independently assessed the studies and reached the consensus after negotiation. We considered the studies with the score more than sixteen had suff i cient quality[13].
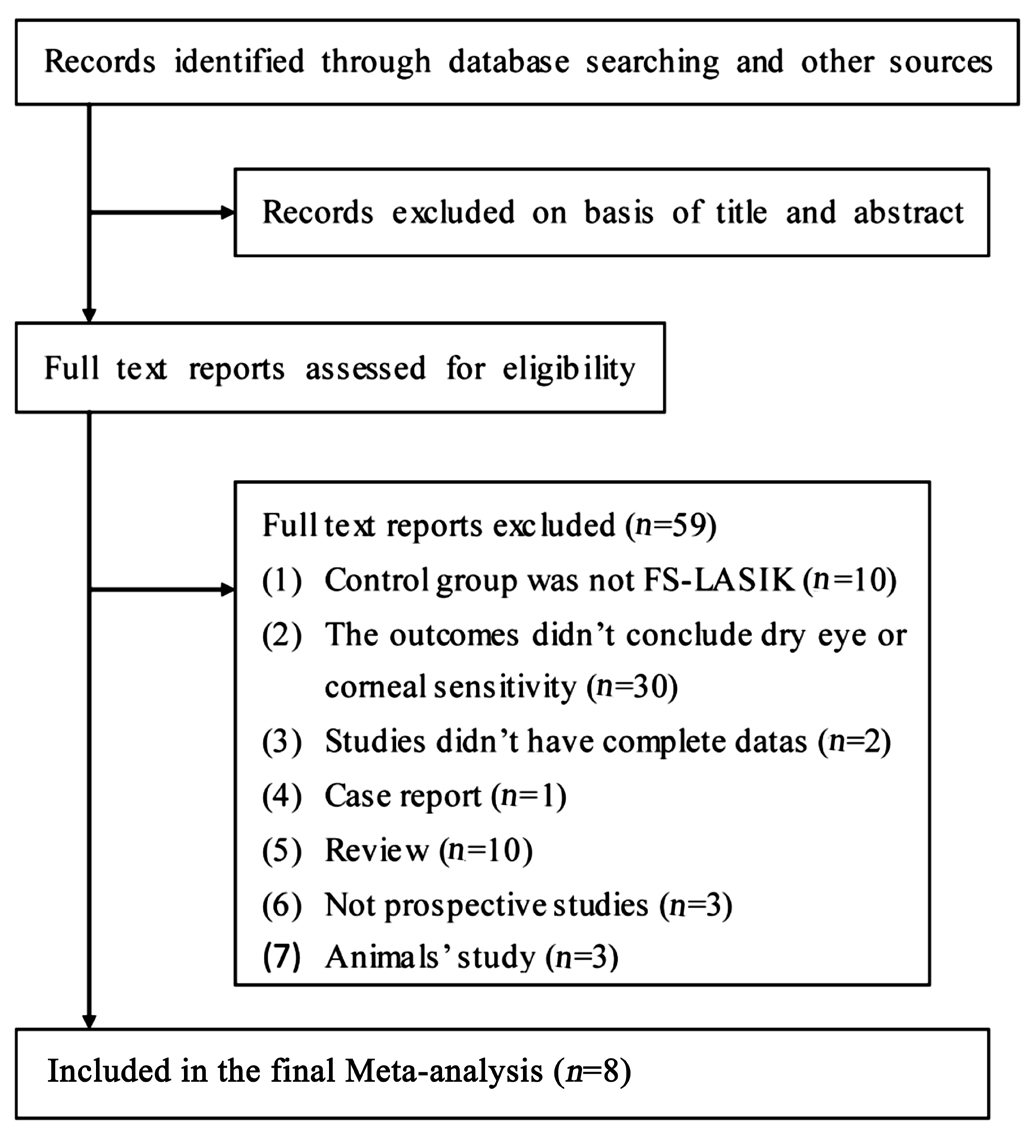
Figure 1 Flow diagram of the literature search in this Meta-analysis.
Data Extraction We extracted the following information:name, publication year, trial location, study design, follow-up period, intervention, characteristics of population, preoperative spherical equivalent. A second reviewer double-checked all data.Statistical Analysis RevMan5.3 software was used to perform this Meta-analysis. The follow-up intervals included preoperation, one week, one month, three months and six months post-operation. Heterogeneity was assessed by calculat ing the I2 statistic and by performing a Chi-square test (assess ing the Ρ-value). I2>50% is considered to be indicative of signif i cant heterogeneity. Both random-effects and fixed-effects models could be applied in our analysis, which was dependent on the heterogeneity between two comparable groups. We examined the Ρ-value and the degree of overlap in conf i dence intervals(CIs)[14]. The Ρ-value less than 0.05 suggested the statistically significance. And we also made the forest plot to show the comparison clearly.
RESULTS
Literature SearchFigure 1 is the flowchart showing our literature retrieval process. After our detailed searching on the database according to the key terms, totally 153 reports were retrieved. We identif i ed 67 eligible studies on basis of titles and abstracts and got the full text of articles. We detailedly browsed the full text of articles and fi nally, 59 reports were excluded.The comparisons in ten studies were not SMILE versus FSLASIK so they were ruled out. Thirty studies’ outcomes didn’t conclude dry eye or corneal sensitivity, two didn’t have complete datum, one was case report, ten were review, three were not prospective studies and three were animals’ study. As a result, eight eligible articles were included.
Table 1 Characteristics of included studied
SMILE: Small incision lenticule extraction; FS-LASIK: Femtosecond laser-assisted in situ keratomileusis; SE: Spherical equivalent; D: Diopter;NR: Non-randomize; Quality (reporting, external validity, bias, confounding, power).
Characteristics of Included Studies Table 1 showed characteristics of our included studies. We identif i ed 772 eyes totally, and of these, SMILE was applied to 386 eyes and FS-LASIK was applied to others. The average age ranged from 23.96 to 32.2 years old. Seven studies in our analysis were nonrandomized observational studies and one was randomized. The followup periods were more than three month and less than one year.In addition, these eight studies were carried out in different countries. Six studies were applied with Chinese, one with French and the other with Turks[7,15-21].
Quality Assessment The quality assessment was showed in Table 1. In the reporting section, all of these trials received scores of more than eight points, which meant that they all clearly described the details of the trials. For the external validity section, all studies received full scores, which meant they had a good representativeness of the researchers, subjects and devices. The bias section could address biases in the measurement of the intervention and the outcome. Just one study is randomized controlled trial (RCT) so others were relatively low. The confounding section addressed bias in the selection of study subjects. We considered the quality index more than sixteen as adequate quality so all of our eight studies met suff i cient quality. We used the proper statistical methods and calculated the results exactly, which reached the adequate score in the power section.
Comparison of Outcome
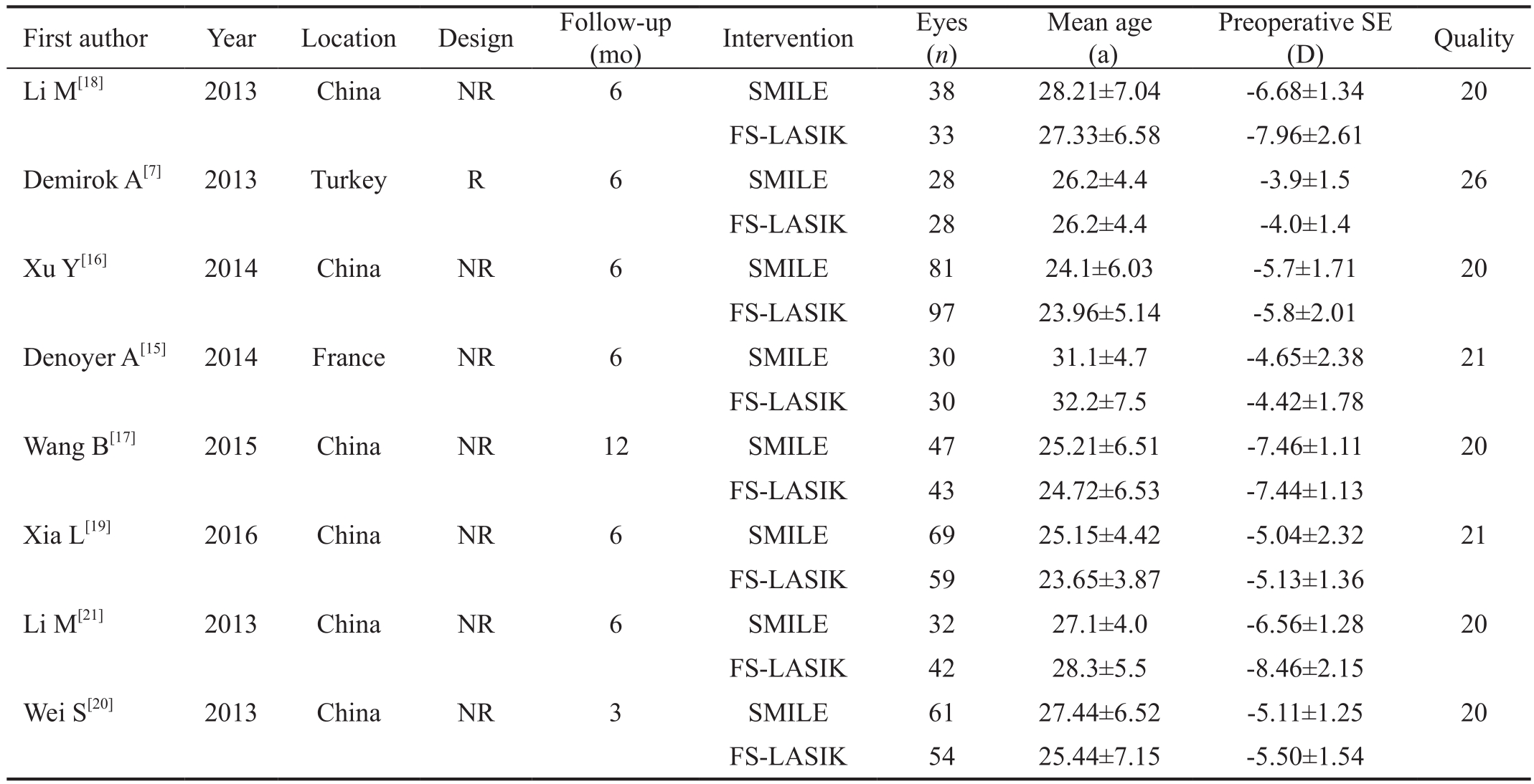
Ocular Surface Disease Index scores Through the Metaanalysis, we found the increase of OSDI score between SMILE and FS-LASIK, which means that the refractive surgery may lead to the symptoms and signs of dry eye. At fi rst, there was no difference in OSDI score between two groups before operation (WMD: 0.36, 95%CI: -0.98 to 1.70, Ρ=0.60). The OSDI score in SMILE group was signif i cantly less than FS-LASIK group at one month (WMD: -5.48, 95%CI: -6.71 to -4.25,Ρ<0.00001) and three months (WMD: -5.67, 95%CI: -6.77 to-4.57, Ρ<0.00001) after surgery, the score at 1wk and 6mo was not calculated (Figure 2).
Tear film break-up time There were six studies reporting TBUT at different time points. No significant difference was observed (WMD: -0.12, 95%CI: -0.48 to 0.23, Ρ=0.50)between two groups preoperatively. The TBUT was longer in SMILE group at one month (WMD: 1.23, 95%CI: 0.05 to 2.41,Ρ<0.05) and three months (WMD: 0.66, 95%CI: 0.36 to 0.96,Ρ<0.0001) postoperatively, while at one week and six months,the difference was not statistically signif i cant (Figure 3).
Schirmer test There were fi ve studies reporting the Schirmer Test results at different time points. Schirmer Test is one of the indexs to diagnose dry eye. This index decreased after two kinds of refractive surgeries. And no signif i cant difference of Schirmer Test was observed in two groups preoperation, at one week, approximately one month, three months and six months postoperatively (Ρ>0.05) (Figure 4).
Corneal sensitivity Totally five studies reported corneal sensitivity. Both SMILE and FS-LASIK refractive surgery damaged the corneal nerve fiber, and corneal sensation was very important to evaluate the corneal function. We could not observe the obvious difference was observed preoperatively (Ρ=0.20). We found the superiority of SMILE in corneal sensation at 1wk (WMD: 18.96, 95%CI: 7.00 to 30.91, Ρ=0.002), 1mo (WMD: 18.48, 95%CI: 9.59 to 27.36,Ρ<0.0001) and 3mo (WMD: 15.39, 95%CI: 9.43 to 21.35,Ρ<0.00001) postoperatively, while at 6mo, the two groups was not statistically signif i cant (Figure 5).
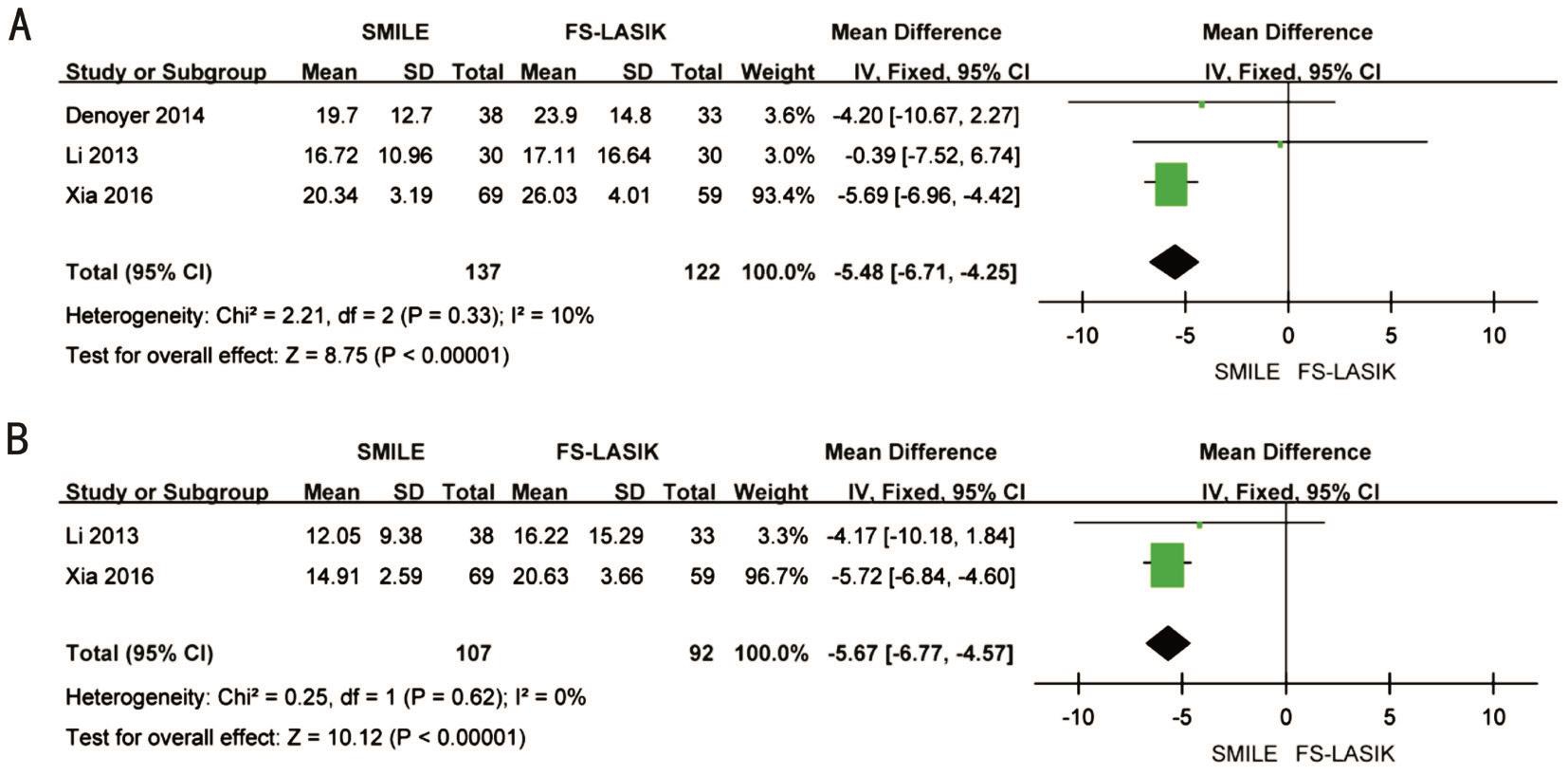
Figure 2 Forest plot comparison of OSDI scores after treatment with SMILE and FS-LASIK A: One month postoperatively; B: Three months postoperatively.
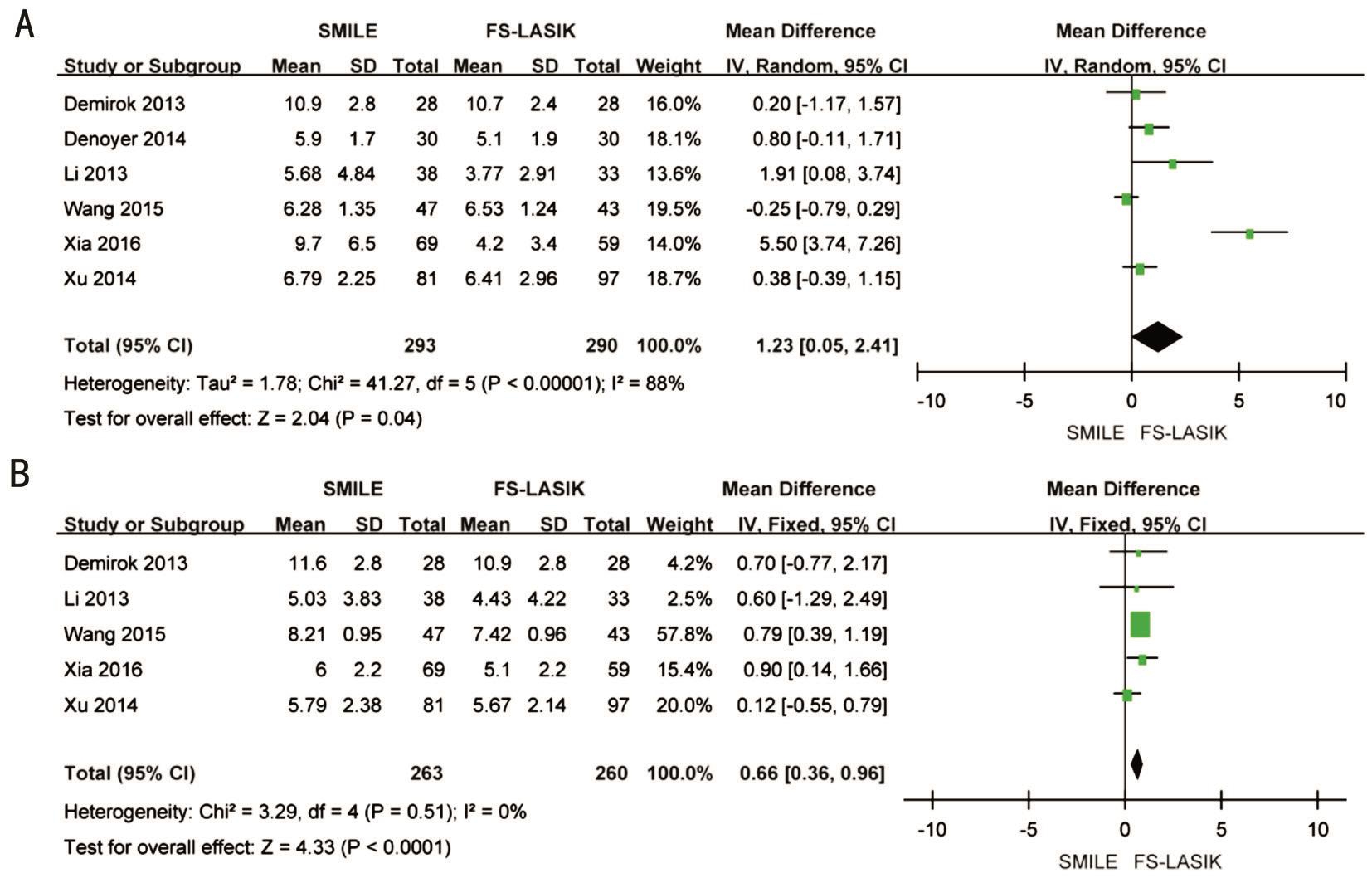
Figure 3 Forest plot comparison of TBUT between SMILE and FS-LASIK A: One month postoperatively; B: Three months postoperatively.
DISCUSSION
The fi elds of refractive surgery develop rapidly in recent years,in order to meet different people’ requirements, mainly for myopia. Small incision lenticule extraction, a novel procedure,has been prevalent in clinical treatments. Reinstein et al[22]retrospect the history, fundamentals and clinical outcomes of SMILE, and fi nd that patients who take the SMILE may have similar corrected distance visual acuity (CDVA) with FSLASIK, which at least can reach the desired visual outcome for patients. Femtosecond laser was applied to create corneal fl ap and excimer laser was used to ablat stroma[23]. The LASIK with the mechanical microkeratome for creating a corneal fl ap has been demonstrated inferior to femtosecond laser including FS-LASIK and SMILE. What’s more, the incidence of dry eye may occur less in SMILE because of the small incision on the anterior stroma, which can decrease the damage of tear film and the corneal nerves. FS-LASIK has been mature in the refractive sector. We now use femto-second lasers to make corneal fl aps, which can grasp the thickness of fl aps accurately and avoid some complications[24].

Figure 4 Forest plot comparison of Schirmer Test after treatment with SMILE and FS-LASIK A: One month postoperatively; B: Three months postoperatively.
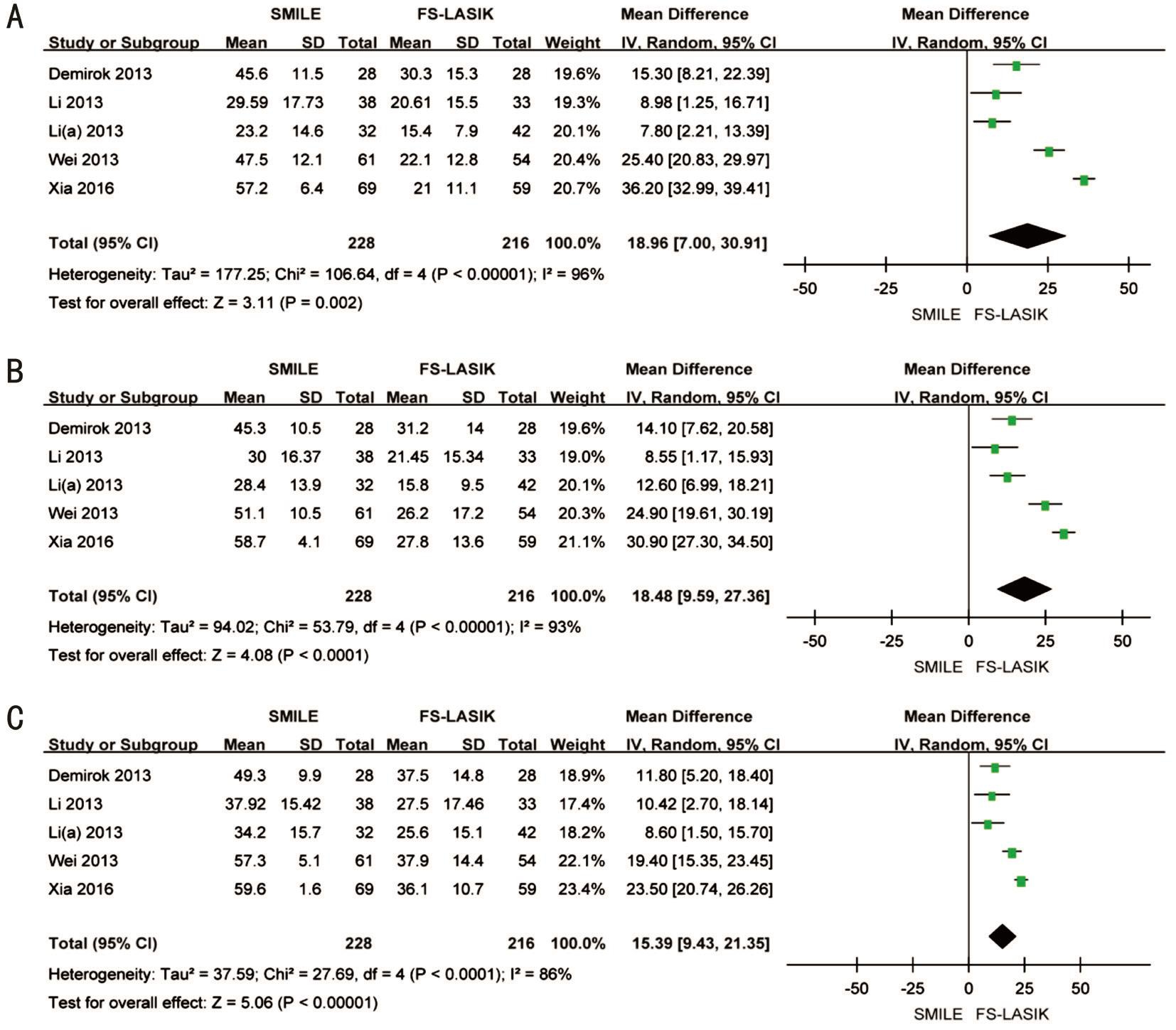
Figure 5 Forest plot comparison of corneal sensitivity after treatment with SMILE and FS-LASIK A: One week postoperatively; B: One month postoperatively; C: Three months postoperatively.
Dry eye is a syndrome of blurry vision and burning pain of the eyes, which is related with a loss, or reduction of the 3-layered tear film[25]. Many patients may feel uncomfortable and dissatisfied after refractive operations due to the occurrence of dry eye syndrome. Several studies have reported that the incidences and degrees of dry are lower following SMILE rather than FS-LASIK[26]. One study has proved that changes in ocular surface are severe in FS-LASIK due to the involvement of some inf l ammatory factors such as IL-6 and nerve growth factor (NGF)[27]. However, some studies fi nd that no obvious differences are found in occurrence of dry eye in these two surgeries.In this Meta-analysis, we conclude eight appropriate studies,extract related datum, and make analysis. We choose three parameters closely related with the diagnosis of dry eye,respectively concluding OSDI scores, TBUT, Schirmer Test.Before the refractive surgery, the heterogeneity of these three parameters in both groups has no obvious difference, which can approve the accuracy of the results. We also found that the OSDI score of SMILE patients was lower than that of FSLASIK patients at one and three months’ postoperation (both Ρ<0.00001). What’s more, the TBUT was higher of SMILE patients at 1 and 3mo postoperatively (Ρ<0.05). However,the Schirmer Test has no significant difference between two surgeries. According to the analysis above, we can find that compared with FS-LASIK, SMILE may have more advantages in decreasing the occurrence of dryness, photophobia and tearing. And the recovery of the tear film function occurs at 3mo, so we can consider that 3-months’ post-operation can get the reliable results of dry eye.
As the results above, the damages of corneal nerve fiber are less with SMILE patents in the first three months. Although at six months, they don’t have the significant difference, the SMILE is still much better. And they are gradually recovery to the previous level. An animal study keeps the same viewpoint with our analytical results, which demonstrates that SMILE is better in nerve fiber recovery, such as the sub-basal nerve length and density (SLD). After 4-weeks’ observation,the stromal nerve in rabbits which underwent the SMILE recovered faster than the ones in FS-LASIK group[28].
This Meta-analysis reliable to assess ocular surface complicates of these surgeries. Firstly, we search for the studies cautiously and finish the searching by two authors. Secondly, we filter the eligible studies in our analysis, and all of them have been satisfied with the quality assessment. Thirdly, we choose the fixed or random model according to the heterogeneity.Fourthly, the studies are applied in different countries, which increase the reliability. There are also some limitations in this Meta-analysis. Firstly, most studies are non-randomized trials.So the risk of various bias will increase and reliability may decrease. Secondly, some indexes are not complete, so the numbers are not enough. Thirdly, the numbers of the included eyes are not enough. Finally, the outcomes we extract don’t contain the visual results because of the incomplete datum.Thus more clinical trials need to be carried out.
In conclusion, this Meta-analysis suggests that the dry eye symptom occurred and the corneal sensitivity decreased between SMILE and FS-LASIK, and latter had higher occurrence rate. The incidences of dry eye recovery better in the SMILE groups, mainly within the three months postoperatively. The corneal sensitivity also recoveries better in SMILE patients in the fi rst three months after surgeries. The comparisons at 6mo have no signif i cant difference.
ACKNOWLEDGEMENTS
Foundation: Supported by the National Natural Science Foundation of China (No.81470648).
Conflicts of Interest: Cai WT, None; Liu QY, None; Ren CD, None; Wei QQ, None; Liu JL, None; Wang QY, None;Du YR, None; He MM, None; Yu J, None.
REFERENCES
1 Ambrosio R Jr, Tervo T, Wilson SE. LASIK-associated dry eye and neurotrophic epitheliopathy: pathophysiology and strategies for prevention and treatment. J Refract Surg 2008;24(4):396-407.
2 Lee JK, Chuck RS, Park CY. Femtosecond laser refractive surgery:small-incision lenticule extraction vs. femtosecond laser-assisted LASIK.Curr Opin Ophthalmol 2015;26(4):260-264.
3 Kim P, Sutton GL, Rootman DS. Applications of the femtosec ond laser in corneal refractive surgery. Curr Opin Ophthalmol 2011;22(4):238-244.
4 Li X, Wang Y, Dou R. Aberration compensation between anterior and posterior corneal surfaces after Small incision lenticule extraction and Femtosecond laser-assisted laser in-situ keratomileusis. Ophthalmic Ρhysiol Opt 2015;35(5):540-551.
5 Agca A, Ozgurhan EB, Demirok A, Bozkurt E, Celik U, Ozkaya A,Cankaya I, Yilmaz OF. Comparison of corneal hysteresis and corneal resistance factor after small incision lenticule extraction and femtosecond laser-assisted LASIK: a prospective fellow eye study. Cont Lens Anterior Eye 2014;37(2):77-80.
6 Chan TC, Ng AL, Cheng GP, Wang Z, Ye C, Woo VC, Tham CC, Jhanji V. Vector analysis of astigmatic correction after small-incision lenticule extraction and femtosecond-assisted LASIK for low to moderate myopic astigmatism. Br J Ophthalmol 2016;100(4):553-559.
7 Demirok A, Ozgurhan EB, Agca A, Kara N, Bozkurt E, Cankaya KI,Yilmaz OF. Corneal sensation after corneal refractive surgery with small incision lenticule extraction. Optom Vis Sci 2013;90(10):1040-1047.
8 Agca A, Cankaya KI, Yilmaz I, Yildirim Y, Yasa D, Olcucu O,Demircan A, Demirok A, Yilmaz OF. Fellow eye comparison of nerve fi ber regeneration after SMILE and femtosecond laser-assisted LASIK: a confocal microscopy study. J Refract Surg 2015;31(9):594-598.
9 He M, Huang W, Zhong X. Central corneal sensitivity after small incision lenticule extraction versus femtosecond laser-assisted LASIK for myopia: a meta-analysis of comparative studies. BMC Ophthalmol 2015;15:141.
10 Egger M, Smith GD, Phillips AN. Meta-analysis: principles and procedures. BMJ 1997;315(7121):1533-1537.
11 Ye J, Xu YF, He JJ, Lou LX. Association between aspirin use and agerelated macular degeneration: a meta-analysis. Invest Ophthalmol Vis Sci 2014;55(4):2687-2696.
12 Samoocha D, Bruinvels DJ, Elbers NA, Anema JR, van der Beek AJ.Effectiveness of web-based interventions on patient empowerment: a systematic review and meta-analysis. J Med Internet Res 2010;12(2):e23.
13 Wang W, Zhou M, Huang W, Zhang X. Ex-PRESS implantation versus trabeculectomy in uncontrolled glaucoma: a meta-analysis. ΡLoS One 2013;8(5):e63591.
14 Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327(7414):557-560.
15 Denoyer A, Landman E, Trinh L, Faure JF, Auclin F, Baudouin C. Dry eye disease after refractive surgery: comparative outcomes of small incision lenticule extraction versus LASIK. Ophthalmology 2015;122(4):669-676.
16 Xu Y, Yang Y. Dry eye after small incision lenticule extraction and LASIK for myopia. J Refract Surg 2014;30(3):186-190.
17 Wang B, Naidu RK, Chu R, Dai J, Qu X, Zhou H. Dry eye disease following refractive surgery: a 12-month follow-up of SMILE versus FSLASIK in high myopia. J Ophthalmol 2015;2015:132417.
18 Li M, Zhao J, Shen Y, Li T, He L, Xu H, Yu Y, Zhou X. Comparison of dry eye and corneal sensitivity between small incision lenticule extraction and femtosecond LASIK for myopia. ΡLoS One 2013;8(10):e77797.
19 Xia L, Zhang J, Wu J, Yu K. Comparison of corneal biological healing after femtosecond LASIK and small incision lenticule extraction procedure. Curr Eye Res 2016;41(9):1202-1208.
20 Wei S, Wang Y. Comparison of corneal sensitivity between FS-LASIK and femtosecond lenticule extraction (ReLEx flex) or small-incision lenticule extraction (ReLEx smile) for myopic eyes. Graefes Arch Clin Exp Ophthalmol 2013;251(6):1645-1654.
21 Li M, Niu L, Qin B, Zhou Z, Ni K, Le Q, Xiang J, Wei A, Ma W, Zhou X. Confocal comparison of corneal reinnervation after small incision lenticule extraction (SMILE) and femtosecond laser in situ keratomileusis(FS-LASIK). ΡLoS One 2013;8(12):e81435.
22 Reinstein DZ, Archer TJ, Gobbe M. Small incision lenticule extraction(SMILE) history, fundamentals of a new refractive surgery technique and clinical outcomes. Eye Vis (Lond) 2014;1:3.
23 Shortt AJ, Allan BD. Photorefractive keratectomy (PRK) versus laserassisted in-situ keratomileusis (LASIK) for myopia. Cochrane Database Syst Rev 2006;(2):CD005135.
24 Mysore N, Krueger R. Advances in refractive surgery: May 2013 to June 2014. Asia Ρac J Ophthalmol (Ρhila) 2015;4(2):112-120.
25 Conrady CD, Joos ZP, Pate BC. Review: the lacrimal gland and its role in dry eye. J Ophthalmol 2016;2016:7542929.
26 Ganesh S, Gupta R. Comparison of visual and refractive outcomes following femtosecond laser- assisted lasik with smile in patients with myopia or myopic astigmatism. J Refract Surg 2014;30(9):590-596.
27 Gao S, Li S, Liu L, Wang Y, Ding H, Li L, Zhong X. Early changes in ocular surface and tear inflammatory mediators after small-incision lenticule extraction and femtosecond laser-assisted laser in situ keratomileusis. ΡLoS One 2014;9(9):e107370.
28 Mohamed-Noriega K, Riau AK, Lwin NC, Chaurasia SS, Tan DT,Mehta JS. Early corneal nerve damage and recovery following small incision lenticule extraction (SMILE) and laser in situ keratomileusis(LASIK). Invest Ophthalmol Vis Sci 2014;55(3):1823-1834.