
·Clinical
Research··Current
Issue· ·Achieve· ·Search Articles· ·Online Submission· ·About IJO· PMC
Old canalicular laceration repair:
a retrospective study of the curative effects and prognostic factors
Fang Bai1,2, Hai Tao2, Yan Zhang2, Peng
Wang2, Cui Han2, Yi-Fei Huang1, Ye Tao1
1Department of Ophthalmology,
General Hospital of Chinese PLA, Beijing 100853, China
2The Lacrimal Center of
Ophthalmology, Armed Police General Hospital of China, Beijing 100039, China
Co-first
authors:
Fang Bai and Hai Tao
Correspondence
to: Yi-Fei
Huang and Ye Tao. Department of Ophthalmology, General Hospital of Chinese PLA,
Fu Xing St, Beijing 100853, China. huangyf301@163.com; toy1011@ 163.com
Received:
2016-10-24
Accepted: 2017-01-19
Abstract
AIM: To investigate
the epidemiology and surgical outcomes of old canalicular laceration and
analyze the variables impacting on the prognosis of reparation.
METHODS: A retrospective
review of all old canalicular laceration repairs from Jan. 1, 2008 to Dec. 30,
2015 was performed. Analyzed data included demographics, mechanisms of injury,
the time from injury to repair, causes for delayed repair, old associated
injuries, the types of surgery, and the effects of repair using canaliculus
anastomosis combined with bicanalicular stent intubation.
RESULTS: Totally 148
patients with old canalicular laceration received surgical repair and were
enrolled. The mean age at presentation was 32.52 years old (ranged from 3 to 63
years old). The 110 patients (74.32%) were male and 127 patients (85.81%) were adults
(≥18 years old). The old upper, lower, and bicanalicular lacerations were found
in 5 (3.38%), 39 (26.35%), and 104 patients (70.27%), respectively. The
mechanism of old injury was primarily due to motor vehicle accidents (n=53,
35.81%). The mean time from injury to repair was 43.61mo (ranged from 1 to
360mo). Associated old ocular and orbit injuries were found in 65 patients
(43.92%), and chronic dacryocystitis in 18 patients (12.16%). The main cause of
delayed repair was that doctors or patients didn’t pay attention to the canalicular
laceration because of the concurrent severe injuries (n=71, 47.97%).
Totally 136 patients (91.89%) with old canalicular laceration underwent
canaliculus anastomosis combined with bicanalicular stent intubation. In all of
them, 20 patients (13.51%) were combined with dacryocystorhinostomy. In these
cases, 132 patients (97.06%) attained anatomic success, 121 patients (88.97%)
reported no epiphora (functional success), 11 patients (8.09%) reported
significant epiphora anesis (functional improvement), and 4 (2.94%) reported no
significant anesis (functional failure). Rates of anatomic success and
functional success were significantly correlated with different canaliculus
involved. However, rates of anatomic success and functional success were not
significantly affected by the time from injury to repair.
CONCLUSION: The canalicular
anastomosis combined with bicanalicular stent intubation could act as an
effective therapeutics for old canalicular laceration.
KEYWORDS: old canalicular
laceration; canalicular repair; bicanalicular stent
DOI:10.18240/ijo.2017.06.11
Citation: Bai F, Tao
H, Zhang Y, Wang P, Han C, Huang YF, Tao Y. Old canalicular laceration repair:
a retrospective study of the curative effects and prognostic factors. Int J
Ophthalmol 2017;10(6):902-907
Article
Outline
INTRODUCTION
Canalicular
lacerations are commonly caused by trauma in the eyelids and periorbital area,
and occurred in 16% of eyelid lacerations[1-2].
Canalicular lacerations are involved in 70% of lacrimal duct injuries and the
lacrimal sac and/or nasolacrimal duct in 30% in lacrimal system[2]. Fayet et al[3]
reported that canalicular lacerations were associated with a 20% incidence of
eye globe injuries. The needs for repair of canalicular lacerations remain to
be controversial. Most researchers proposed that canalicular lacerations should
be repaired urgently to avoid postinjury epiphora[4-7].
In China,
because of the uneven economy and medical conditions, primary canalicular lacerations
in many patients were not repaired on time, and most of them have to undergo
operations to repair old canalicular lacerations and solve serious postinjury
epiphora. Although there was a great deal of studies on the epidemiology,
urgent repair techniques, stents and urgent repair outcomes of primary
canalicular lacerations[8], little data is
available on those of old canalicular lacerations.
The
canalicular anastomosis combined with bicanalicular or monocanalicular stent
intubation are used for primary canalicular lacerations repair[2]. Unlike primary canalicular lacerations, the surgical
techniques of old canalicular lacerations combined with eyelid scar and
deformity are more complicated. Moreover, bicanalicular stent was reported the
potential risk[5,9] and several
complications[8]. Consequently, general
ophthalmologist may be more interested in monocanalicular stent intubation.
However, bicanalicular stents can provide tension of lacerated ends, and it
might be more suitable for old canalicular laceration repair.
In this study,
we described the epidemiology of old canalicular lacerations managed at the
Lacrimal Center of Ophthalmology, Armed Police General Hospital of China and
reported the surgical outcomes of old canalicular laceration repair using
canalicular anastomosis combined with bicanalicular stent intubation.
SUBJECTS AND METHODS
Subjects With the approval of the Ethics
Committee of Armed Police General Hospital of China, a retrospective study of
all patients with old canalicular lacerations repair at the Lacrimal Center of
Ophthalmology, Armed Police General Hospital of China, from Jan. 1, 2008 to
Dec. 30, 2015 was performed. All people voluntarily joined this study with
informed consents.
All included
patients who had suffered primary canalicular laceration and had not gotten
urgent repair operation in time, underwent old canalicular laceration repair to
solve severe postinjury epiphora in 1mo after trauma. Exclusion criteria
included the lack of adequate follow up (<3mo), preinjury epiphora and
pyorrhea.
Operation
Technique and Follow-up All patients were
underwent CT three-dimensional reconstruction for the lacrimal duct examing the
lacrimal and canthal area and ultrasound biomicroscopy for some patients were
done before operation. The patients underwent canalicular anastomosis combined
with bicanalicular stent intubation or reconstruction lacrimal duty combined
with stent intubation. The old medial cut-edge of canaliculus was sought after
cut-though scar or lacrimal sac during operation. Once the cut-edge was found,
a bicanalicular stent was placed in superior and inferior canaliculi and two
cut-edge were anastomosed using one-stitch anastomosis through the skin with
5-0 silk suture. If the cut-edge couldn’t be identified, monocanaliculus
reconstruction with conjunction-flap transposition and bicanalicular stent
intubation or conjunctivodacryocystostomy and lacrimal duct stent intubation
were done. All repairs were performed by the same oculoplastic surgery
professor. Adults were under local anesthesia and pediatric patients were under
general anesthesia.
Patients were
asked postoperative follow-up and irrigation of canaliculi using
anti-inflammatory drugs once a month. The standard of stent removal was absence
of epiphora or epiphora anesis, patent canaliculus on irrigation and the time
maintained with stent between 3 to 6mo. All patients were interviewed by
telephone and got irrigation canaliculi recently for assessing the long-term
consequences of repairing the old canalicular injuries and patient
satisfaction. The data collected for analysis included general information and
demographics of patients, mechanism and canaliculus involved, time from injury
to surgery, concurrent old ocular injury, primary management after injury,
types of current operation and stent which were used, duration of follow up,
complications, and timing of stent removal and whether they still had epiphora
after removal stent and epiphora degree.
A patent
canaliculus on diagnostic probing (soft to sac) was defined as anatomic success
(patency), whereas absence of epiphora, even with environmental stressors, in
>3mo after stent removal, was defined as functional success. Moreover still
epiphora but significant anesis was defined as functional improvement. Anatomic
success (patency) for bicanalicular laceration was anatomic patency of both
upper and lower canaliculi.
Statistical
Analysis Descriptive statistics,
including the mean, standard deviation and range were calculated for different
variables. Fisher’s exact test was used to analyze clinical outcomes. The SPSS
software was used (version 19.0, IBM, Chicago, IL, USA) for statistical
analysis. Differences were considered statistically significant at P<0.05.
RESULTS
Of all the 161
patients who had undergone old canalicular laceration repair, 148 patients met
the inclusion criteria and were enrolled. The mean age of the patients was
32.52 years old (ranged from 3 to 63 years old). In these patients, 110 (74.32%)
were male and 127 (85.81%) were adults (≥18 years old). The old upper, lower,
and bicanalicular lacerations were found in 5 (3.38%), 39 (26.35%), and 104
patients (70.27%), respectively (Table 1).
Table 1
Parameters of old canalicular lacerations
|
Parameters |
n (%) |
|
Male |
110 (74.32) |
|
Age (median,
range), a |
32.52 (32.5, 3-63) |
|
Adult (≥18a) |
127 (85.81) |
|
Canaliculus
involved |
|
|
Upper |
5 (3.38) |
|
Lower |
39 (26.35) |
|
Upper and lower |
104 (70.27) |
|
Associated
old ocular or orbit injuries |
|
|
None |
83 (56.08) |
|
Old concomitant orbit fracture without repair |
37 (25) |
|
Post-repair of orbit fracture |
5 (3.38) |
|
Post-ophthalmectomy |
4 (2.7) |
|
Old optic neuropathy |
1 (0.68) |
|
Chronic dacryocystitis |
18 (12.16) |
|
Mechanism of
injury |
|
|
Motor vehicle accidents |
53 (35.81) |
|
Hard object injury |
40 (27.03) |
|
Sharp instrument injury |
22 (14.86) |
|
Dog bites |
14 (9.46) |
|
Boxing injury |
9 (6.08) |
|
Avulsion injury |
8 (5.41) |
|
Injury related to aesthetic surgery |
1 (0.68) |
|
Explosion injury |
1 (0.68) |
|
Urgent
repair |
|
|
Suturing surrounding tissues of canailculi |
144 (97.3)1 |
|
No management |
4 (2.7) |
|
The causes
of delayed repair |
|
|
Patients refused |
32 (21.62) |
|
Not found the cut ends |
39 (26.35) |
|
Not focus on canalicular laceration |
71(47.97) |
|
Time from
injury to repairs (median, range), mo |
43.61 (8.5, 1-360) |
|
1-12mo |
78 (52.70) |
|
1-5a |
39 (26.35) |
|
More than 5a |
31 (20.95) |
1One patient was performed
Jones tube placement.
The causes for
old canalicular laceration were numerous. Motor vehicle accidents was the
leading cause of injury with 53 (35.81%), and followed by hard object injury (n=40,
27.03%). The mean time from injury to this repair was 43.61mo (ranged from 1 to
360mo). The 78 (52.70%) patients was between 1mo to 12mo, 39 (26.35%) patients
was between 1 to 5y, and 31 (20.95%) patients was after 5y. The urgent repair
with single suturing surrounding tissues of canaliculi after injury were
performed in 144 (97.30%) patients, while no management were done in 4 (2.70%)
patients. The main cause of delayed repair was that doctors or patients didn’t
pay attention to the canalicular laceration because of the concurrent severe
injuries (n=71, 47.97%). Associated old ocular and orbit injuries were
found in 65 patients (43.92%), and chronic dacryocystitis in 18 patients
(12.16%) (Table 1).
Totally 136
patients (91.89%) with old canalicular laceration underwent canaliculus
anastomosis combined with bicanalicular stent intubation. In all of them, 20
patients (13.51%) were combined with dacryocystorhinostomy including 18
patients with chronic dacryocystitis and 2 patients with common canalicular
laceration (Figures 1 and 2). Only 1 patient (0.68%) had severe old
monocanaliculus injury which couldn’t be identified. This patient received the
monocanaliculus reconstruction with conjunction-flap transposition and
bicanalicular stent intubation.
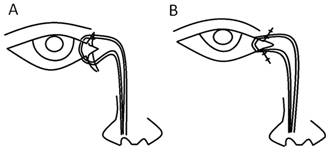
Figure 1 A
diagram depicting the intubation of bicanalicular stent into the lacerated
bicanaliculus A: Pre-anastomosis; B: Post-anastomosis.

Figure 2 Slit-lamp photograph of a patient with
old common canalicular laceration after bicanalicular stent intubation (4wk
after surgery).
There were 11
patients (7.43%) with severe old bicanalicular injuries that couldn’t be
identified and repaired, 10 patients (6.76%) underwent
conjunctivodacryocystostomy with labial mucosa transplantation, 1 patient
(0.68%) underwent conjunctivodacryocystostomy with conjunctiva-flap
transposition (Table 2).
Table 2
Type of surgery and time of removal stent
|
Parameters |
n (%) |
|
Type of
surgery |
148 |
|
Canaliculus anastomosis and bicanalicular stent intubation |
136 (91.89)1 |
|
Canaliculus reconstruction with conjunctiva-flap transposition
and bicanalicular stent intubation |
1 (0.68) |
|
Conjunctivodacryocystostomy with labial mucosa
transplantation and placement of monocanalicular stent intubation |
10 (6.76) |
|
Conjunctivodacryocystostomy with conjunctiva-flap
transposition and placement of monocanalicular stent intubation |
1 (0.68) |
|
Time of
removal stent in the cases of canaliculus anastomosis and bicanalicular stent
intubation (range), mo |
5.1 (1-6)2 |
1Totally 116 patients received
single canaliculus anastomosis and bicanalicular stent intubation, 20 patients
received canaliculus anastomosis with dacryocystorhinostomy and bicanalicular
stent intubation; 2Three patients who had severe punctal and
canalicular slitting were removed stent between 1-2.1mo, 1 patient lost the
stent in 1mo.
The mean time
of bicanalicular stent removal was 5.1mo (median 5mo, ranged from 30d to 6mo).
There was 1 patient with stent prolapse and loss in 1mo. Three patients were
removed stent relatively earlier (<3mo, mean 1.5mo, ranged 1 to 2.1mo)
because of severe punctal or canalicular slitting. After 3mo of stent removal,
the 4 patients had still epiphora but anesis, and 2 patients had clear
limitation on irrigation (anatomic failure) and the other 2 patients did not
have limitation (anatomic success).
At
following-up visits, patients were performed irrigation and asked about
epiphora. After 3mo of stent removal, in the all 136 patients, 132 (97.06%)
patients got anatomic success, 121 (88.97%) reported no epiphora (functional
success), 11 (8.09%) reported still epiphora but significant anesis (functional
improvement), and 4 (2.94%) reported no significant anesis (functional
failure). There were 4 patients who did not get anatomic success, including 1 patient
with old upper canalicular laceration, 1 patient with old bicanalicular
lacerations and 2 patients with old lower canalicular laceration. Anatomic
success rate in bicanaliculi was the highest at 98.91% compared with 94.87% in
lower canaliculus and 80% in upper canaliculus (P=0.04). The canaliculus
involved in relation to functional success and improvement was statistically
significant (P<0.05). Anatomic success rate was 97.22% (n=70)
in patients with 1-12mo time interval between injury and surgery, 100% (n=37)
with 1-5y, and 92.59% (n=25) longer than 5y. Functional success rate was
90.28% (n=65) 91.89% (n=34), and 81.48% (n=22),
respectively (P>0.05) (Table 3).
Table 3
Outcomes of canaliculus anastomosis and bicanalicular stent intubation
n
(%)
|
Parameters |
Patients |
Anatomic success |
Functional success |
Functional improvement |
|
Canaliculus
anastomosis and bicanalicular
stent intubation |
136 (100) |
132 (97.06) |
121 (88.97) |
11 (8.09) |
|
Canaliculus involved
|
|
|
|
|
|
Upper |
5 (3.68) |
4 (80) |
4 (80) |
0 |
|
Lower |
39 (28.68) |
37 (94.87) |
31 (79.49) |
5 (12.82) |
|
Upper and lower |
92 (67.65) |
91 (98.91) |
86 (93.48) |
6 (5.43) |
|
P |
- |
0.04 |
0.04 |
0.01 |
|
Time from
injury to surgery |
|
|
|
|
|
1-12mo |
72 (52.94) |
70 (97.22) |
65 (90.28) |
6 (8.33) |
|
1-5y |
37 (27.21) |
37 (100) |
34 (91.89) |
2 (5.41) |
|
More than 5y |
27 (19.85) |
25 (92.59) |
22 (81.48) |
3 (11.11) |
|
P |
- |
>0.05 |
>0.05 |
>0.05 |
DISCUSSION
In China, there
are many patients with primary canalicular lacerations didn’t receive repair
operation in time. Firstly, medical conditions are unbalanced in China. The
standard operating rooms are not always available and the doctors couldn’t
acquire formal training in these areas with poor medical conditions. Repair of
canalicular laceration couldn’t be performed in time. Secondly, some patients
do not wish to spend extra expense in this surgery just to avoid possible
posttraumatic epiphora. Thirdly, whether patients should receive the repair
surgery of urgent canalicular lacerations remains to be controversial. Many
ophthalmologists aren’t interested in repairing urgent canalicular lacerations.
In their opinions, the functional success rate of repair canalicular laceration
is low and many patients without repair canalicular laceration after injury
maintain asymptomatic. Therefore, when patients suffer from severe concurrent
injuries, doctors and/or patients always neglect primary canalicular laceration
repair. Consequently, there are numerous patients with old canalicular
laceration in China. Some of them with severe epiphora have to accept the
surgery of repair old canalicular laceration to solve this problem.
Several
studies on primary canalicular injuries found a similar trend and showed that
the single lower canalicular involvement was the most common, followed by
single upper canalicular involvement and bicanalicular involvement[8,10-12]. However,
the degree of impaired tear drainage after obstruction of monocanaliculus and
importance of the upper and lower canaliculus in lacrimal drainage is
controversial[13-14]. In this
study, patients with old bicanalicular involvement were most common (70.27%).
All patients suffered from severe epiphora after canalicular injuries without
canalicular anastomosis and stent intubation on time. An indirect evidence
suggested that lower canaliculus was more important than upper canaliculus in
overall lacrimal drainage, and the obstruction of bicanaliculi could lead to
epiphora more easily than monocanaliculus, the lower more easily than upper
canaliculus. That might be the reason why old bicanalicular laceration was most
common in this study. Additionally, in our study, old lower canalicular
laceration was more common than old upper canalicular laceration because the
primary lower canaliculus would be more easily involved at urgent situation.
In several
studies, canalicular lacerations repair were performed within 1d to 2wk[1,8,12]. Most studies
reported the poor results with late repair of canalicular lacerations[4,8]. In this study, all old canalicular
lacerations were performed repaired from 1mo to 20y after injury, and most
cases (52.7%) were performed within 1 to 12mo after injury. However, the
difference between those earlier and later repair in terms of the anatomic and
functional success rate or functional improvement rate wasn’t significant.
Traumatic
chronic dacryocystitis is secondary to nasolacrimal duct injury and always
happened 4wk after trauma. That is why it is frequently found in old lacrimal
duct traumatic, but not in urgent traumatic. In this study, 18 patients
suffered from traumatic chronic dacryocystitis.
The
monocanalicular versus bicanalicular stent remains to be controversial[7,14-17]. One of the
perceived disadvantages of bicanalicular stent is the risk of potential injury
to uninvolved canaliculus[5,9]
and several complications including punctal or canalicular slitting, granuloma
formation, and chronic nasal irritation. In the present study, 3 patients had
severe punctal or canalicular slitting. However, one potential advantage of
bicanalicular stent is the ability to maintain distal tension while the
surrounding soft tissue is repaired. That is very important for old canalicular
lacerations repair. It would be beneficial for the connection between the
proximal and distal canaliculus breakages[5,9].
Bicanalicular stent would be more suitable for old canalicular lacerations.
Primary
dacryocystorhinostomy isn’t often performed at urgent canalicular lacerations.
However, literatures advised that it could be performed if the urgent lesion of
lacrimal duct involved a common canaliculus or lacrimal sac[6].
In this study, dacryocystorhinostomy was performed at 18 patients who had
traumatic chronic dacryocystitis with injury of lacrimal sac or nasolacrimal
duct and 2 patients with canalicular lacerations. The stents were in place for
3 to 6mo, the canaliculus heal and form an epithelialized channel around the
stent and there would be a channel when the stent is removed[18].
There is no
consensus regarding the exact duration of canalicular stent to achieve
long-term canalicular patency. However, the majority of studies still tend to
propose for longer duration[5,8,12,19-21]. In this
study, bicanalicular stents were maintained for 5.1mo. Our standard of stent
removal was absence of epiphora or epiphora anesis and patent canaliculus on
irrigation between 3 to 6mo. But there were 4 patients who have anatomic
failure. Of these 4 patients, 2 patients had canalicular block at site, and 2
patients had serious stenosis. The stents of these 2 patients with serious
stenosis were removed early (1mo). Therefore, the failure to achieve
canalicular patency might be correlated with the time of stent removal.
We defined
functional success as the lack of postoperative epiphora and anatomic success
as softly diagnostic probing to sac. Most studies showed that primary
canalicular laceration repair with canalicular stent intubation could retain a
high success rate (from 58% to 100%) in avoiding posttraumatic epiphora[9,19-20,22-25]. Compared with urgent canalicular laceration, old
canalicular laceration repair is knottier and success rate would be lower in
most opinions. Lower success rate should be ascribed to two reasons: firstly,
severe scar surrounding canaliculus, deformity of eyelid and canthus could
result in displacement of lacerated canaliculus; Secondly, severe derogative
canaliculi could not be found, and need to reconstruct tear drainage.
This study
concentrated on 136 cases of repair canalicular lacerations using canalicular
anastomosis and bi-canalicular stent intubation with dacryocystorhinostomy or
not. Compared with previous studies[5,8-9,11,14,23-24] about urgent canalicular lacerations with anatomical
success rate (25%-94.1%) and functional success rate (58%-100%), this study had
higher anatomical success rate (97.06%) and lower functional success rate
(88.97%). The former study is based on the prophylactic surgery, and this study
is based on the therapeutic surgery. The functional success in urgent
canalicular lacerations maybe overestimated operation results because many
patients were asymptomatic even if canalicular block, but for old canalicular
lacerations were underestimated. In this study, functional effective rate (functional
success and functional improvement) has reached 97.06%. In this study, CT
three-dimensional reconstruction of the lacrimal duct and ultrasound
biomicroscopy were performed to clarify the location of canalicular lacerations
and the lever of canalicular injury before surgery. Taking advantages of these
examinations, the appropriate surgical approach was selected. Patients received
regular follow-up after surgery. Once precursor of punctal and canalicular
slitting or severe canalicular stenosis were found, anti-inflammatory drug and
canalicular dilatation would be performed timely. Thus, higher anatomical
success rate of this study was associated with preoperative adequate
examination, the appropriate surgical approach, surgical experience of
operators and standardized postoperative follow-up.
In this study,
there are 4 patients of anatomic failure, including 2 patients who suffered
removal stent early (severe canalicular stenosis, 1 patient who suffered from
recurrent allergic conjunctivitis (canalicular block in site, with old lower
canalicular lacerations), and 1 patient who suffered from recurrent
iridocyclitis (extensive canalicular block, with old upper canalicular
lacerations). We conjectured that extensive canalicular block and recurrent
iridocyclitis might be the outcome of systemic disorders. Moreover, long-term
topical medications toxicity might be one reason of extensive canalicular
block. Therefore, failure to achieve canalicular patency might be correlated
with the early removal of stent, recurrent allergic conjunctivitis, and
recurrent iridocyclitis. Patients with severe canalicular stenosis (anatomic
failure) might suffer from epiphora anesis.
ACKNOWLEDGEMENTS
Foundations: Supported by the National
Natural Science Foundation of China (No.81600767); the National Key Basic
Research Program of China (973 Program: No.2013CB967001); Postdoctoral Science
Foundation of China (No.2015M582852).
Conflicts
of Interest: Bai F, None; Tao H, None; Zhang Y, None; Wang P, None;
Han C, None; Huang YF, None; Tao Y, None.
REFERENCES
1
Herzum H, Holle P, Hintschich C. Eyelid injuries: epidemiological
aspects.<ii> Ophthalmologe</ii> 2001;98(11):1079-1082. [CrossRef]
2
Ducasse A, Arndt C, Brugniart C, Larre I. Lacrimal traumatology. <ii>J Fr
Ophtalmol</ii> 2016;39(2):213-218. [CrossRef]
3
Fayet B, Bernard JA, Ammar J, Karpouzas Y, Hamici S, Hamache F, Pouliquen Y.
Recent wounds of the lacrimal duct. Apropos of 262 cases treated as
emergencies. <ii>J Fr Ophtalmol</ii> 1988;11(10):627-637. [PubMed]
4
Dortzbach RK, Angrist RA. Silicone intubation for lacerated lacrimal canaliculi.
<ii>Ophthalmic Surg</ii> 1985;16(10):639-642. [PubMed]
5
Murchison AP, Bilyk JR. Canalicular laceration repair: an analysis of variables
affecting success. <ii>Ophthal Plast Reconstr Surg</ii> 2014;30(5):
410-414. [CrossRef]
6
Ejstrup R, Wiencke AK, Toft PB. Outcome after repair of concurrent upper and
lower canalicular lacerations. <ii>Orbit</ii> 2014;33(3):169-172. [CrossRef]
7
Tavakoli M, Karimi S, Behdad B, Dizani S, Salour H. Traumatic canalicular
laceration repair with a new monocanalicular silicone tube. <ii>Ophthal
Plast Reconstr Surg</ii> 2017;33(1):27-30. [CrossRef]
8
Naik MN, Kelapure A, Rath S, Honavar SG. Management of canalicular lacerations:
epidemiological aspects and experience with Mini-Monoka monocanalicular stent.
<ii>Am J Ophthalmol</ii> 2008;145(2):375-380. [CrossRef]
9
Leibovitch I, Kakizaki H, Prabhakaran V, Selva D. Canalicular lacerations:
repair with the Mini-Monoka<supsup>®</supsup> monocanalicular intubation
stent. <ii>Ophthalmic Surg Lasers Imaging</ii> 2010;41(4):472-477.
[CrossRef]
10
Jordan DR, Ziai S, Gilberg SM, Mawn LA. Pathogenesis of canalicular
lacerations. <ii>Ophthal Plast Reconstr Surg</ii>
2008;24(5):394-398. [CrossRef]
11
Rosser PM, Burt B, Osborne SF. Determination of the function of a repaired
canaliculus after monocanalicular injury by placing a punctal plug in the non-involved
punctum on the affected side. <ii>Clin Experiment Ophthalmol
</ii>2010;38(8):786-789. [CrossRef]
12
Murchison AP, Bilyk JR. Pediatric canalicular lacerations: epidemiology and variables
affecting repair success. <ii>J Pediatr Ophthalmol Strabismus</ii>
2014;51(4):242-248. [CrossRef]
13
Linberg JV, Moore CA. Symptoms of canalicular obstruction.
<ii>Ophthalmology</ii> 1988;95(8):1077-1079. [CrossRef]
14
Wu SY, Ma L, Chen RJ, Tsai YJ, Chu YC. Analysis of bicanalicular nasal
intubation in the repair of canalicular lacerations. <ii>Jpn J
Ophthalmol</ii> 2010;54(1):24-31. [CrossRef]
15
Wu AY, Tucker NA. Bicanalicular laceration repair via an endoscopic retrograde
approach. <ii>Ophthal Plast Reconstr Surg</ii>
2011;27(6):e165-e167. [CrossRef]
16
Hawes MJ, Segrest DR. Effectiveness of bicanalicular silicone intubation in the
repair of canalicular lacerations. <ii>Ophthal Plast Reconstr
Surg</ii> 1985;1(3):185-190. [CrossRef]
17
Nam SM. Microscope-assisted reconstruction of canalicular laceration using
Mini-Monoka. <ii>J Craniofac Surg</ii> 2013;24(6):2056-2058. [CrossRef]
18
Kwitny A, Baker JD. Functional results of the surgical repair of a lacerated
canaliculus in children. <ii>J Pediatr Ophthalmol Strabismus</ii>
2011;48(2):117-119. [CrossRef]
19
Kersten RC, Kulwin DR. “One-stitch” canalicular repair. A simplified approach
for repair of canalicular laceration. <ii>Ophthalmology</ii>
1996;103(5):785-789. [CrossRef]
20
Drnovsek-Olup B, Beltram M. Trauma of the lacrimal drainage system:
retrospective study of 32 patients. <ii>Croat Med J</ii>
2004;45(3):292-294. [PubMed]
21
Liang T, Zhao KX, Zhang LY. A clinical application of laser direction in
anastomosis for inferior canalicular laceration. <ii>Chin J
Traumatol</ii> 2006;9(1):34-37. [PubMed]
22
Reifler DM. Management of canalicular laceration. <ii>Surv
Ophthalmol</ii> 1991;36(2):113-132. [CrossRef]
23
Anastas CN, Potts MJ, Raiter J. Mini Monoka silicone monocanalicular lacrimal
stents: Subjective and objective outcomes. <ii>Orbit</ii> 2001;20(3):
189-200. [CrossRef]
24
Lee H, Chi M, Park M, Baek S. Effectiveness of canalicular laceration repair
using monocanalicular intubation with Monoka tubes. <ii>Acta
Ophthalmol</ii> 2009;87(7):793-796. [CrossRef]
25
Tao H, Wang P, Han C, Zhang J, Bai F, He ZY. One-stitch anastomosis through the
skin with bicanalicular intubation: a modified approach for repair of
bicanalicular laceration. <ii>Int J Ophthalmol</ii>
2013;6(5):656-658. [PMC free article] [PubMed]