
·Investigation· Current
Issue IF in JCR CiteScore ·Submission· In Press Recent Accepted PMC RSS
Citation: Ji YR, Zhu DQ, Zhou HF, Fan XQ. Epidemiologic characteristics and
outcomes of open globe injury in Shanghai. Int J Ophthalmol
2017;10(8):1295-1300
Epidemiologic characteristics and outcomes of open
globe injury in Shanghai
Yong-Rong Ji, Dong-Qing Zhu, Hui-Fang Zhou,
Xian-Qun Fan
Department
of Ophthalmology, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong
University School of Medicine, Shanghai 200011, China
Co-first
authors: Yong-Rong Ji and Dong-Qing Zhu
Correspondence
to: Xian-Qun Fan. Department of Ophthalmology, Shanghai Ninth
People’s Hospital, Shanghai Jiao Tong University School of Medicine, 639 Zhi
Zao Ju Road, Shanghai 200011, China.
fanxq@sh163.net
Received:
2016-12-09
Accepted: 2017-03-24
Abstract
AIM: To
investigate the epidemiologic characteristics and outcomes of open globe injury
in Shanghai.
METHODS: A
retrospective study was conducted for 148 unilateral open globe injury cases
presenting to a tertiary referral hospital of Shanghai. Electronic medical
records were reviewed and phone surveys were conducted to collect and analyze
1) background of patient; 2) setting of injury and clinical signs at
presentation; 3) treatment procedure and outcome; 4) quality of life after
injury.
RESULTS: There
were more male patients (77.03%) than females (22.97%), more temporary
habitants (79.05%) than residents (20.95%). The subjects in this study
presented a significantly lower constitutional status of education than that of
the whole Shanghai population (P<0.001). Occupational injury was the
first cause of injuries (39.86%), followed by home accident (20.27%), road
accident (16.89%), violent behavior (16.89%) and outdoor injury (6.08%). The
143 subjects (96.62%) were not wearing spectacles at the time of injury. Of all
patients, 77 subjects (52.03%) had the outcome of no vision (including
enucleation). The classification and regression tree (CART) prognosis presents
59.58% sensitivity to predict visual survival correctly and 80.19% specificity
to predict no vision correctly. The patients whose injured eye had no vision
reported more reduction of life quality.
CONCLUSION: We
found that male subject, temporary habitants, low educational status and no
eyewear are risk factors of open globe injury in Shanghai. Occupational injury
is the leading cause. CART analysis presents a certain agreement to the actual
visual outcome. The injury imposes negative impact on quality of life
especially in no vision cases. The education of eye protection may help to
avoid the injury.
KEYWORDS:
ocular injury; globe penetration; epidemiology; risk factors;
occupational injury
DOI:10.18240/ijo.2017.08.18
Citation: Ji YR, Zhu DQ, Zhou HF, Fan XQ. Epidemiologic characteristics and
outcomes of open globe injury in Shanghai. Int J Ophthalmol
2017;10(8):1295-1300
INTRODUCTION
Ocular
trauma is one of the major causes of ocular morbidity. The global incidence
rate of ocular trauma was estimated to be 3.5 per 100 000 persons per year[1]. It is one of leading indications for enucleation in
China and in USA[2-3]. Ocular
trauma has a wide spectrum according to the nature and the location of the
injury. Open globe injury, defined as a full-thickness injury of the eye wall,
presents a severe damage of the eye and often results in poor outcome. Some
prognostic models based on clinical signs at presentation, such as the ocular
trauma score (OTS) and the classification and regression tree (CART) were created
to predict the eventual vision survival[4], but
their sensitivity and specificity need to be further assessed. Another feature
of ocular trauma is that the majority of injuries can be avoided if certain
precautions are taken. The strategy for prevention is developed on basis of
knowing the causes of injuries and the conditions of their occurrences.
Previous studies have shown that socio-economic status, education, and nature
of work are all important factors, but actually the epidemiology of ocular injury
varies largely in different regions and between the populations[5-10]. Shanghai is the most populous
city in China, housing 14.3 million residents and 9.8 million temporary
habitants[11], but there is rare study available
on epidemiology and outcomes of severe ocular injury. Therefore, we conducted a
retrospective investigation on the cases of open globe injury presented in a
tertiary referral hospital in Shanghai to investigate the epidemiologic
characteristics and analyze the outcomes and quality of life after injury.
SUBJECTS AND METHODS
Study
Population and Information Collection
This study was a retrospective investigation conducted in Shanghai
Ninth People's Hospital, a tertiary referral hospital located in the centre of
Shanghai, specialized in facial trauma. The standard treatment protocol for a
diagnosed open globe injury consists of 1) urgent operative repair of globe and
removal of intraocular foreign body within 24h of injury unless there is
medical contraindication or delay in presentation; 2) continuous administration
of intravenous antibiotics before and after operation for 48h; 3) postoperative
administration of topical steroids and antibiotics. If the eye is severely
injured and considered unsalvageable, primary enucleation is discussed by
oculoplastic team with patient. Informed decision is left to patient. All
patients are educated about eye protection and the risk of sympathetic
ophthalmia during or after treatment. According to the consideration of further
treatment, patients are referred to retina team for vitrectomy and retinal
detachment repair or to oculoplastic team for enucleation. The treatment
procedures are discussed with patients and the decisions are left to them.
The
electronic medical records of all patients with the diagnosis of open globe
injury from 1st January, 2011 to 31st December, 2015 were
reviewed. Operating registers were searched for repair of open globe injury,
repair of ruptured globe and enucleation. Patients who underwent open globe
repair at a separate hospital were excluded from this study. The background of
subjects was picked up from register system, including age, gender, educational
status, residency status, current occupation. The medical records of subjects
were categorized by the following columns: 1) the setting of injury including
date of injury, cause of injury, wear of eye protective devices, use of alcohol
or drugs; 2) previous medical history of general disease or ocular disease; 3)
clinical signs at presentation including visual acuity, nature of injury,
location of injury, relative afferent pupillary defect (RAPD), lid laceration,
general status and other injury; 4) treatment after injury; 5) outcome after
the procedure of treatment including visual acuity, ocular complication, primary
or secondary enucleation and sympathetic ophthalmia.
Phone
call surveys were then conducted to collect more information from the patients
or their close family members. The survey consisted of 2 sections: 1)
supplemental information of injury; 2) quality-of-life questionnaire.
The
first section included: 1) confirmation of personal information; 2)
confirmation of cause of injury, wear of eye protective devices and use of
alcohol or drugs; 3) confirmation of ocular symptoms and general status at
presentation; 4) confirmation of the treatment procedures, patient’s decision
on further treatment and outcome; 6) confirmation of the occurrence and the
education of sympathetic ophthalmia; 7) current eye protection.
The
second section included the following questions about the quality of life after
eye injury:
1 Do you have obvious difficulty with judging distances when walking?
2 Do you have obvious difficulty with your vision when reading or
watching TV?
3 Do you feel that your appearance has obviously changed by the eye
injury?
4 Do you feel that your eye injury has an obvious negative impact on
your social life?
5 Has your employment status been changed after eye injury? (for those
who had full-time employment before injury)
A: No, I returned to my former job after treatment.
B: Yes, my job was changed after injury.
C: Yes, I’m unemployed after injury.
Patients
uncontactable by phone call or unable to answer the questions were excluded
from this study. Finally, 148 subjects were eligible for inclusion out of 171
open globe injury patients identified from the register system. The tenets of
the Declaration of Helsinki were followed. As no personal information or photo
of any certain patient was to be disclosed in publication, the Medical Ethics
Committee of Shanghai 9th people’s hospital did not require patient
consent for this retrospective study.
Definition
and Data Categorization The age of patient was defined as age at
the time of injury. The residency status of the patient was classified into
Shanghai resident and temporary habitants according to whether the registered
address on his identity card was in Shanghai.
The
education status was defined as the highest diploma of the subject, classified
into 1) primary school degree or below; 2) junior middle school degree; 3)
senior middle school degree; 4) university degree or above.
CART
is a visual prognosis system created by Schmidt et al[12]
specially for open globe injury. One model of CART is to make a prediction
between vision survival and no vision (Figure 1), which is important to guide
following treatment. The CART analysis in this study was retrospectively
conducted with the information collected from medical records and the
prediction was then compared with actual outcome to evaluate the prediction of
CART system. The clinical signs were classified in CART form. The initial
visual acuity was defined as the visual acuity of the injured eye at
presentation to hospital and was divided into 1) 20/20 to hand movement (HM);
2) light perception (LP); 3) no light perception (NLP). The wound location was
defined according to the Ocular Trauma Classification Group. Zone I injuries
were confined to the cornea and limbus. Zone II injuries involved the anterior
5 mm of the sclera (not extending into the retina). Zone III injuries involved
full-thickness scleral defects more posterior than 5 mm from the limbus[13].
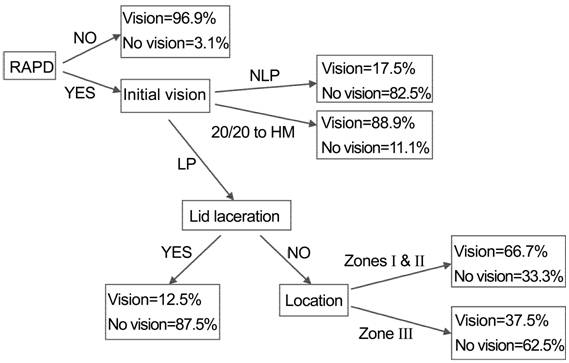
Figure
1 The prediction schema of vision survival and no vision by CART.
Statistical
Analysis The
statistical analysis was performed with Excel 2007 (Microsoft Office, Microsoft
Corporation, USA) and SPSS 14.0 (SPSS Inc, Chicago, IL, USA). The
constitutional status of education of patients in this study was compared with
that of Shanghai population. The associations of the clinical signs with the
visual outcome were respectively evaluated by Chi-square test. A P value
<0.05 can confirm a notable coherence. The sensitivity and the specificity
of CART prognosis were calculated. The questionnaires on quality of life and
employment status after eye injury were analyzed for reliability and validity.
A Cronbach’s α value >0.8 means very good reliability. A P value
<0.05 of Pearson Correlation test indicates significant validity. The
quality of life and employment status was also assessed by Chi-square test between
the vision survival group and no vision group. A P value <0.05
indicates an obvious difference between 2 groups.
RESULTS
General
Demographic Information The 148
subjects included were all Chinese. The injuries were all found unilateral, of
which 74 cases at the right side, 74 at the left side. There were more male
subjects (n=114, 77.03%) than females (n=34, 22.97%) in this
study. The median age at injury was 41.5y in males and 50y in females. The
distribution of age and gender were demonstrated with population pyramid in
Figure 2. Shanghai residents accounted for 20.95% of the total subjects and
temporary habitants accounted for 79.05%. Compared with the constitutional
status of education of the whole Shanghai population[14],
the subjects in this study presented a significantly lower educational status
(Table 1).
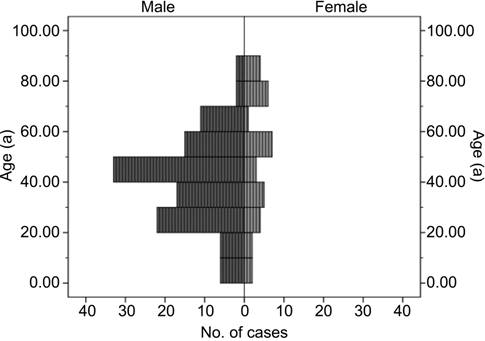
Figure
2 Graph showing the age and gender distributions of open globe injury patients.
Table
1 Comparison of the constitutional status of education of the open globe injury
patients in this study and that of the whole Shanghai population
n (%)
|
Educational
status |
Open globe
injury patients in this study |
Shanghai
population1 (million) |
Chi-square
test |
|
Primary
school degree or below |
47 (31.76) |
5.05
(14.57) |
P<0.001 |
|
Junior
middle school degree |
61 (41.22) |
4.83
(39.24) |
|
|
Senior
middle school degree |
36 (24.32) |
8.39
(22.56) |
|
|
University
degree or above |
4 (2.70) |
3.12
(23.63) |
1The constitutional status of education in Shanghai population
(including residents and temporary habitants in Shanghai) referred to the sixth
national census of population in the year 2010[14].
The open globe injury patients in this study presented a significantly lower
constitutional status of education than that of the Shanghai population
(Chi-square test, P<0.001).
Causes
of Injury The causes of open
globe injury were classified into five kinds (Figure 3). Occupational injuries
were the most common causes (39.86%) followed by home accident (20.27%), road
accident (16.89%), violent behavior (16.89%) and outdoor injury (6.08%). Home
accidents consisted of cooking accident, injury by sharp object and slip at
home. Outdoor accidents included accidents by flying or thrown objects,
firework explosions, sports etc except road accidents or assaults.
Twenty-three subjects admitted alcohol use before injury including 5 in 25 road
accident cases and 18 in 25 violent behavior cases. The 143 subjects (96.62%)
did not wear any eye protective device (safety goggles or glasses) at the time
of injury. Broken spectacles hurt the eye in 3 cases. Non-broken spectacles
hurt the eye by impact in the rest 2 cases, in which one eye had laser-assisted
in situ keratomileusis (LASIK) operation 10y before the injury, and the
other was a blind glaucomatous eye before the injury.
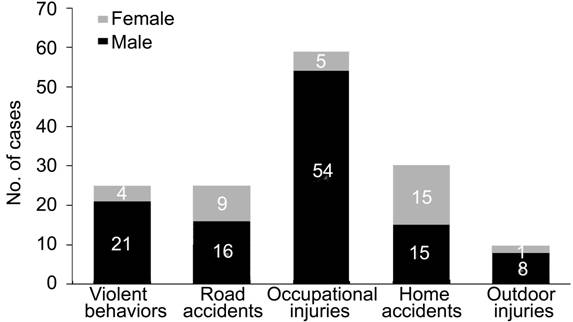
Figure
3 Graph showing the causes of open globe injury and distributions.
Prognosis
and Outcomes Of all
patients, 77 subjects (52.03%) had the outcome of no vision (including
enucleation). The presence of RAPD, the injury at the Zone III and rupture as
the mechanism of injury were significant risk factors of no vision. The rank of
initial vision was related to the visual outcome, in which group 1 (20/20 to HM)
and the group 2 (LP) showed equal indication to high possibility of visual
survival (Chi-square test, P=0.550), whereas the initial vision of NLP
is strongly related to no vision outcome compared with the first 2 groups
(Pearson Chi-square test, P<0.001). The CART prognosis showed a
certain agreement to the actual visual outcome (Chi-square test P<0.001)
with 59.58% sensitivity to predict visual survival correctly and 80.19%
specificity to predict no vision correctly (Table 2).
Table
2 The predictive values of clinical signs and CART
|
Parameters |
Final
visual outcome |
Chi-square
test |
|
|
Visual
survival |
No vision |
||
|
Total
cases |
71
(47.97%) |
77
(52.03%) |
|
|
RAPD |
|
|
P=0.018 |
|
Yes |
63 |
77 |
|
|
No |
8 |
0 |
|
|
Initial
vision |
|
|
P=0.550
between groups 1&2 P<0.001
between groups (1+2)&3 |
|
1
(20/20 to HM) |
29 |
2 |
|
|
2
(LP) |
34 |
4 |
|
|
3
(NLP) |
8 |
71 |
|
|
Lid
laceration |
|
|
P=0.101 |
|
Yes |
31 |
50 |
|
|
No |
40 |
27 |
|
|
Location |
|
|
P<0.001 |
|
Zone
I&II |
65 |
46 |
|
|
Zone
III |
6 |
31 |
|
|
Mechanism |
|
|
P=0.006 |
|
Rupture |
30 |
59 |
|
|
Laceration |
41 |
18 |
|
|
CART
prediction |
|
|
P<0.001 Visual
survival sensitivity=59.58% No vision
specificity=80.19% |
|
Visual
survival |
42.30 |
15.25 |
|
|
No
vision |
28.70 |
61.75 |
|
Fifty-one
subjects ended up by enucleation (14 primary enucleations and 37 secondary
enucleations) accounting for 34.46% of total cases and 66.23% of final no
vision eyes. All the enucleated eyes presented no light perception before
operation. Of the 14 primary enucleation cases, 4 patients had general diseases
including neurological injury, ancient cerebral vascular accident,
schizophrenia and Parkinson’s disease, 7 patients had no vision of the injured
eye before the injury because of glaucoma, severe keratits and ancient ocular
injury. The major reasons for secondary enucleation decision focused on obvious
eye atrophy (31 subjects, 83.78%), ocular pain (13 subjects, 35.14%),
prophylaxis of sympathetic ophthalmia (3 subjects, 8.11%). No sympathetic ophthalmia
was reported in this study, whereas 129 subjects (87.16%) said having the
education about sympathetic ophthalmia. After injury, only 19 patients (12.84%)
wore spectacles on purpose to protect the injured or the contralateral eye.
The
questionnaire on quality of life and employment status after eye injury showed
good reliability and validity (Tables 3, 4). The association between the visual
outcome of the injured eye and the quality of life was evaluated. The patients
whose injured eye lost vision reported more difficulties in visual function,
more changes in appearance and more inadaptabilities in social life (Table 3),
in addition, they had more risks of job change and unemployment after injury
(Table 4).
Table
3 Quality of life after open globe injury
n (%)
|
Visual
outcome of the injured eye |
No. of
subjects investigated |
Impact on
vision and stereovision |
Impact on
appearance and social life |
Two
independent samples nonparametric test |
||
|
Difficulty
in judging distances |
Difficulty
in reading or watching TV |
Obvious
appearance change |
Negative
impact on social life |
|||
|
Vision
survival |
71 |
28 (39.44) |
29 (40.85) |
7 (9.86) |
6 (8.45) |
P<0.001 |
|
No
vision |
77 |
53 (68.83) |
56 (72.73) |
49 (63.64) |
48 (62.34) |
|
|
Total
cases |
148 |
81 (54.73) |
85 (57.43) |
56 (37.84) |
54 (36.49) |
|
Reliability
analysis: Cronbach’s α=0.896 (very good reliability between item scores); Construct
validity analysis: Pearson correlation tests between each item score and total
score, P<0.01 (significant validity).
Table
4 Employment status after open globe injury n (%)
|
Visual
outcome of injured eye |
No. of
subjects1 |
Employment
status |
2P |
|
|
Job change |
Unemployed |
|||
|
Vision
survival |
45 |
6 (13.33) |
8 (17.78) |
<0.001 |
|
No
vision |
50 |
14 (28.00) |
24 (48.00) |
|
|
Total
cases |
95 |
20 (21.05) |
32 (33.68) |
|
Reliability
analysis: Cronbach’s α=0.889 (very good reliability between items scores);
Construct validity analysis: Pearson correlation tests between each item score
and total score, P<0.05 (significant validity). 1Subjects
who had full-time employment before injury. 2Two independent samples
nonparametric test.
DISCUSSION
Male
gender, young age and low socio-educational status are generally considered as
risk factors of ocular trauma[5-10].
Similar to previous studies, this study demonstrated that open globe injury
patients presented a dominant proportion of male subjects, a preponderance of
temporary habitants and a significantly lower constitutional status of
education than that of the whole Shanghai population. No laterality was found
in these unilateral cases. The prevalence in females seemed stable with age,
whereas most injuries in males happened in the range from 20y to 70y and peaked
at the decade of 40y-50y. The age peak is later than those in other studies
mainly because the first cause in this study for all subjects and for males was
occupational injuries rather than violent behaviors or road accidents which may
affect a younger population[5,7-9]. Home accidents were the second cause for all subjects
and the first cause for females, approving that home is a frequent place for
open globe injury[15-16]. The
use of alcohol was not usual but also contributed to the occurrence of injury
especially by the form of violent behaviors.
Despite
the cases of broken spectacles and those of fragile blind eyes, the ocular
injuries in this study were mostly related to non-wearing of spectacles. So we
presume that spectacles, no matter eye protective device (EPD) or eyewear for
myopia, can effectively prevent the eye from injury. Theoretically, the use of
EPD is mandatory according to the practice policy concerning works like cutting
metal, welding, grinding, drilling and hammering, but the fact revealed that
the policy was not well followed in work practice. The reason for non-use of
EPD was not investigated in this study, but strict implementation of EPD and
compliance with the practice policy may surely reduce the rate of industrial
work-related ocular injury. On the other hand, for activities not covered by
eye safety policy, wearing spectacles may be a feasible solution. Actually,
eyewear is quite common in China because of high prevalence of myopia. The
78.4% Chinese adolescents are myopic in urban area and 95.5% university
students are myopic in Shanghai[17-18].
High prevalence of myopia is related to high educational status[19]. The subjects of study presented a lower
constitutional status of education than that of Shanghai population. This may
be the reason for their less common use of spectacles and indirectly more
exposure to ocular trauma.
According
to this study, the manipulation of CART analysis is quite feasible for clinical
application. First of all, the signs of CART are all ordinary clinical signs
which are generally available from medical records and easy to get in
emergency. Secondly, the CART prognosis presented a certain agreement to the actual
visual outcome in this study. The prediction of vision survival or no vision
may help to indicate different further treatments. However, when assessing the
signs respectively, we found that the initial vision of NLP was a strong
indication to no vision outcome, whereas the presence of lid laceration made no
difference. To note, the rate of no vision outcome and enucleation seemed to be
higher in this study compared with the others[5-10,20-24]. It was
mainly because of the referral bias. The open globe injury cases referred to
Shanghai Ninth People’s Hospital were most of high severity and their poor
prognoses were also confirmed by CART prediction. In addition, the prognosis of
open globe injury is usually quite poor despite the significant improvements in
techniques of vitreoretinal surgery[23-25].
Our
survey revealed that most of the patients would not accept primary enucleation
psychologically even for a non-salvageable eye. As a result, primary
enucleation was rarely practiced unless the general status of the patient
restricted further operation or the injury was the second strike for an already
blind eye. Secondary enucleation was proposed to cases of severely damaged no
vision eye, but the decision was also left to patient. Painful eye and prophylaxis
of sympathetic ophthalmia are two indications for secondary enucleation mostly
mentioned in the literature[2,26].
But in this study, esthetic concern of obvious atrophic eye was the first
motivation for secondary enucleation and orbital implantation. Since there was
no report of sympathetic ophthalmia in this study, the morbidity was not able
to be estimated, but the awareness rate of sympathetic ophthalmia was quite
high among patients due to the education in hospital.
As
the open globe injury is unilateral in most cases, quality of life after injury
is presumed little affected as the uninjured eye can provide normal visual
acuity as before. But in this study, those whose injured eye lost vision
reported more obvious reduction of quality of life than vision survival group.
We think it was partly due to more severe defect on stereovision and change on
ocular appearance and partly due to psychological inadaptability to unexpected
blindness of one eye. According to the result of this study and those in the literature,
the subjects most affected by vision-threatening ocular injuries are of
productive age but in poor socio-economic status[5-6,10], thus the impact of injury on
employment status is of great concern. In our study, a total of 33.68% former
full-time employees did not work after injury and 21.05% had their job changed.
A previous study had the similar report that 40% patients didn’t return to
their former work after open globe injury[27].
It’s hard for us to presume whether visual defect or psychological barrier was
the major factor that made the patients unable to be employed or unwilling to
go back to work, but apparently the high unemployment brought socio-economic
burden to the patient as well as to the society.
Considering
the high risk for certain population and the poor prognosis of open globe
injury, we think that the education of eye protection is an effective solution
to avoid occurrence and recurrence of injury. However, the current
implementation of eye protection was far from satisfying. Our survey found that
most patients didn’t take any eye protective measure even after the severe
ocular injury. The ignorance of eye safety before injury as well as the neglect
of eye protection after injury reflects the unawareness of the preventability of
ocular injury. Thus, more eye care education should be given to the high risk
population and the importance of wearing spectacles should be emphasized in
workplace. On basis of the current fact revealed in this study, better
strategies for ocular injury prevention, treatment and social readaptation
after injury should be developed.
ACKNOWLEDGEMENTS
Foundations:
Supported by the National Natural Science Foundation of China
(No.31600971); The Shanghai Committee of Science and Technology, China
(No.14411968000).
Conflicts
of Interest: Ji YR, None; Zhu DQ, None; Zhou HF,
None; Fan XQ, None.
REFERENCES
1 Négrel AD, Thylefors B.
The global impact of eye injuries. Ophthalmic
Epidemiol 1998;5(3):143-169. [CrossRef] [PubMed]
2 Moshfeghi DM, Moshfeghi
AA, Finger PT. Enucleation. Surv
Ophthalmol 2000;44(4):277-301. [CrossRef]
3 Cheng GY, Li B, Li LQ, Gao
F, Ren RJ, Xu XL, Jonas JB. Review of 1375 enucleations in the TongRen Eye
Centre, Beijing. Eye (Lond)
2008;22(11):1404-1409. [CrossRef] [PubMed]
4 Yu Wai Man C, Steel D.
Visual outcome after open globe injury: a comparison of two prognostic
model-the Ocular Trauma Score and the Classification and Regression Tree. Eye (Lond) 2010;24(1):84-89. [CrossRef] [PubMed]
5 Nirmalan PK, Katz J,
Tielsch JM, Robin AL, Thulasiraj RD, Krishnadas R, Ramakrishnan R; Aravind
Comprehensive Eye Survey. Ocular trauma in a rural south Indian population: the
Aravind Comprehensive Eye Survey. Ophthalmology
2004;111(9):1778-1781. [CrossRef]
6 Qi Y, Zhang FY, Peng GH,
Zhu Y, Wan GM, Wang WZ, Ma J, Ren SJ. Characteristics and visual outcomes of
patients hospitalized for ocular trauma in central China: 2006-2011. Int J Ophthalmol 2015;8(1):162-168. [PMC free article] [PubMed]
7 Kuhn F, Morris R,
Witherspoon CD, Mann L. Epidemiology of blinding trauma in the United States
Eye Injury Registry. Ophthalmic Epidemiol
2006;13(3):209-216. [CrossRef] [PubMed]
8 Soylu M, Sizmaz S, Cayli
S. Eye injury (ocular trauma) in southern Turkey: epidemiology, ocular
survival, and visual outcome. Int
Ophthalmol 2010;30(2):143-148. [CrossRef] [PubMed]
9 Bauza AM, Emami P, Son JH,
Langer P, Zarbin M, Bhagat N. Work-related open-globe injuries: demographics
and clinical characteristics. Eur J
Ophthalmol 2013;23(2):242-248. [CrossRef] [PubMed]
10 Wang JD, Xu L, Wang YX,
You QS, Zhang JS, Jonas JB. Prevalence and incidence of ocular trauma in North
China: the Beijing Eye Study. Acta
Ophthalmol 2012;90(1):e61-e67.
[CrossRef] [PubMed]
11
http://www.shanghai.gov.cn/nw2/nw2314/nw3766/nw3783/nw3784/u1aw9.html
12 Schmidt GW, Broman AT,
Hindman HB, Grant MP. Vision survival after open globe injury predicted by
classification and regression tree analysis. Ophthalmology 2008;115(1):202-209. [CrossRef] [PubMed]
13 Pieramici DJ, Sternberg P
Jr, Aaberg TM Sr, Bridges WZ Jr, Capone A Jr, Cardillo JA, de Juan E Jr, Kuhn
F, Meredith TA, Mieler WF, Olsen TW, Rubsamen P, Stout T. A system for
classifying mechanical injuries of the eye (globe). Am J Ophthalmol 1997;123(6):820-831. [CrossRef]
14
http://www.shanghai.gov.cn/nw2/nw2314/nw3766/nw3783/nw4836/u1aw338.html
15 Bhogal G, Tomlins PJ,
Murray PI. Penetrating ocular injuries in the home. J Public Health (Oxf) 2007;29(1):72-74. [CrossRef] [PubMed]
16 Oum BS, Lee JS, Han YS.
Clinical features of ocular trauma in emergency department. Korean J Ophthalmol 2004;18(1):70-78. [CrossRef] [PubMed]
17 He M, Zeng J, Liu Y, Xu
J, Pokharel GP, Ellwein LB. Refractive error and visual impairment in urban
children in southern China. Invest
Ophthalmol Vis Sci 2004;45(3):793-799. [CrossRef] [PubMed]
18 Sun J, Zhou J, Zhao P,
Lian J, Zhu H, Zhou Y, Sun Y, Wang Y, Zhao L, Wei Y, Wang L, Cun B, Ge S, Fan
X. High prevalence of myopia and high myopia in 5060 Chinese university
students in Shanghai. Invest Ophthalmol
Vis Sci 2012;53(12):7504-7509. [CrossRef] [PubMed]
19 Guo YH, Lin HY, Lin LL,
Cheng CY. Self-reported myopia in Taiwan: 2005 Taiwan National Health Interview
Survey. Eye (Lond) 2012;26(5):684-689. [CrossRef] [PMC free article] [PubMed]
20 Soong TK, Koh A, Subrayan
V, Loo AVP. Ocular trauma injuries: a 1-year surveillance study in the
University of Malaya Medical Centre, Malaysia. 2008. Graefes Arch Clin Exp Ophthalmol 2011;249(12):1755-1760. [CrossRef] [PubMed]
21 Acar U, Tok OY, Acar DE,
Burcu A, Ornek F. A new ocular trauma score in pediatric penetrating eye injuries.
Eye (Lond) 2011;25(3):370-374. [CrossRef] [PMC free article] [PubMed]
22 Savar A, Andreoli MT,
Kloek CE, Andreoli CM. Enucleation for open globe injury. Am J Ophthalmol 2009;147(4):595-600.e1. [CrossRef] [PubMed]
23 Soni NG, Bauza AM, Son
JH, Langer PD, Zarbin MA, Bhagat N. Open globe ocular trauma: functional
outcome of eyes with no light perception at initial presentation. Retina 2013;33(2):380-386. [CrossRef] [PubMed]
24 Han YS, Kavoussi SC,
Adelman RA. Visual recovery following open globe injury with initial no light
perception. Clin Ophthalmol
2015;9:1443-1448. [CrossRef] [PMC free article] [PubMed]
25 Feng K, Wang CG, Hu YT,
Yao Y, Jiang YR, Shen LJ, Pang XQ, Nie HP, Ma ZZ. Clinical features and
prognosis of eyeball rupture: eye injury vitrectomy study. Clin Exp Ophthalmol 2015;43(7):629-636. [CrossRef] [PubMed]
26 Chu XK, Chan CC.
Sympathetic ophthalmia: to the twenty-first century and beyond. J Ophthalmic Inflamm Infect 2013;3(1):49. [CrossRef] [PMC free article] [PubMed]
27 Rofail M, Lee GA,
O'Rourke P. Quality of life after open-globe injury. Ophthalmology 2006;113(6):1057.e1-3.
[CrossRef] [PubMed]