
·Review· Current
Issue IF in JCR CiteScore ·Submission· In Press Recent Accepted PMC RSS
Citation: Dhiman R, Devi S, Duraipandi K, Chandra P,
Vanathi M, Tandon R, Sen S. Cysticercosis of the eye. Int J Ophthalmol
2017;10(8):1319-1324
Cysticercosis of the eye
Rebika Dhiman, Saranya Devi, Kavitha Duraipandi,
Parijat Chandra, Murugesan Vanathi, Radhika Tandon, Seema Sen
Dr
Rajendra Prasad Centre for Ophthalmic Sciences, All India Institute of Medical
Sciences, New Delhi 110029, India
Correspondence
to: Murugesan Vanathi. Dr Rajendra Prasad Centre for
Ophthalmic Sciences, All India Institute of Medical Sciences, New Delhi 110029,
India. vanathi_g@yahoo.com
Received:
2016-01-14
Accepted: 2017-05-16
Abstract
Cysticercosis
is a preventable and eradicable cause of blindness endemic in the Indian
subcontinent, South- East Asia and other developing countries. Ocular and
orbital cysticercosis has varied presentations depending upon the site of
involvement, number of lesion and the host immune response. In this article we
present a review of the various clinical manifestations, diagnosis and
management protocol for orbital and ocular cysticercosis. Owing to its varied
presentation, cysticercosis may pose a diagnostic challenge to the health
professionals. Early diagnosis and management can prevent the vision loss and
optimize visual outcomes.
KEYWORDS:
cysticercosis; orbital cysticercosis; ocular cysticercosis;
intracameral cysticercosis
DOI:10.18240/ijo.2017.08.21
Citation: Dhiman R, Devi S, Duraipandi K, Chandra P, Vanathi M, Tandon R, Sen S.
Cysticercosis of the eye. Int J Ophthalmol 2017;10(8):1319-1324
INTRODUCTION
Cysticercosis
is a preventable cause of blindness endemic in India[1].
It is a parasitic infestation caused by Cysticercus cellulosae, which is the
larval form of Taenia solium. In 1829, Soemmering[2]
reported first case of a live anterior chamber cysticercosis. World Health
Organization recognized neural cysticercosis as an international public health
issue and major cause of epilepsy. Neurocysticercosis was found to be the most
common cause of epilepsy in a study from South India[3].
A review of literature on orbital and adnexal cysticercosis shows predilection
for children and young adults with no sex predilection[4-5].
PATHOPHYSIOLOGY
Taenia
solium belongs to the class of cestodes. Human beings are definitive hosts that
harbor the adult parasite in the intestine and pigs are the intermediate hosts
harboring the larvae. Human cysticercosis occurs when they act as intermediate
host by ingesting the eggs via following modes of infestation: 1) contaminated
food and water with the Taenia solium eggs (hetero-infection); 2) reinfection
by ingestion ova of the existing parasite (external auto-infection); 3)
retrograde peristalsis causing the transport of mature proglottids bearing eggs
from bowel to stomach (internal auto-infection).
After
ingestion, the eggs of Taenia solium hatch into larvae, which pierce the gut to
reach the blood stream and enter various tissues (particularly the central
nervous system, eyes and striated muscle)[5] where
they develop into cysts producing the clinical syndrome of cysticercosis.
Neurocysticercosis can coexist in up to 24% of the cases[6].
Cysticercus
celluosae mainly has three stages of evolution. The live or vesicular cyst is
the living cyst with a well-defined scolex (Figure 1). It causes minimal or no
inflammation in the tissue. As larva begins to die the cyst wall becomes leaky,
releasing toxins and causing varying degrees of inflammation. This is the
colloidal vesicular stage. Eventually, the larvae die and are either totally
resorbed or calcified. This is the calcified nodular stage[7].
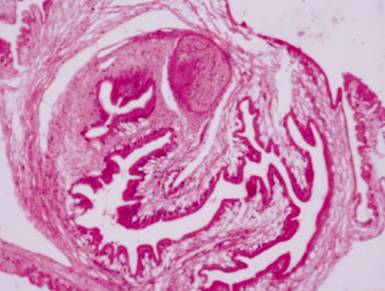
Figure 1
Histopathological appearance of cysticercus showing scolex with sucker and
hooklets surrounded by a well-defined cyst wall.
Cysticercosis
is found in the areas with poor sanitation and is endemic in South East Asia,
Indian subcontinent, Mexico, South America and sub-Saharan Africa[5]. Ocular cysticercosis has a varied presentation
depending upon the site of involvement, number of lesion and the host immune
response. In contrast to Western literature, Indian studies have reported
ocular adnexa as the most common site of involvement. While the most common
site of localization reported in Western studies is the posterior segment, in
the Indian literature the ocular adnexa is the most common site[8-10]. In a study reported by
Kruger-Leite et al[11], 35% of the cysts
were found in the subretinal space, 22% in the vitreous, 22% in the
subconjunctival space, 5% in the anterior segment, and only 1% in the orbit. In
India, 78% of the cases with ocular cysticercosis have been reported from
states of Andhra Pradesh and Pondicherry[10-12].
ORBITAL
CYSTICERCOSIS
Orbital
and adnexal cysticercosis have varied clinical presentation. The extraocular
muscle form is the commonest type of orbital and adnexal cysticercosis.
Lodgment of cysts in the subconjunctival space is another common site, followed
by the eyelid, optic nerve and retro-orbital space. Lacrimal sac cysticercosis
has also been reported[13]. Association
between orbital and systemic cysticercosis is uncommon.
The
common clinical complains are periocular swelling, proptosis, ptosis, pain,
diplopia, restriction of ocular motility, strabismus, decreased vision, lid
edema and orbital cellulitis like clinical picture. In cases of extraocular
muscle involvement (Figure 2) superior rectus muscle is the most common site[14]. Subconjunctival presentation could be a secondary
stage in those cases in which the cyst may have extruded from the primary extra
ocular muscle site[15]. It has to be
differentiated from other benign and malignant conditions presenting as ocular
mass. One or more extraocular muscles may be simultaneously involved, although
a propensity for the involvement of superior rectus muscle complex and lateral
rectus muscles has been reported[14-15].
An unusual association of multiple brain neurocysticercosis with ocular
cysticercosis involving levator palpebrae superioris and superior rectus muscle
has been reported[16]. Another study
has reported an unusual case of ocular cysticercosis involving the levator
palpebrae superioris and superior rectus muscle[8,17].

Figure 2
Clinical photograph showing subconjunctival cysticercosis.
Optic
nerve involvement is rare. Optic nerve compression by the cyst may be
associated with decrease in vision and disc edema[18].
A large cyst may cause axial proptosis and restricted ocular motility. A case
of cyst with hooklets on the optic disc has been reported who also had
sub-cutaneous and cerebral involvement[19].
The
differential diagnosis of orbital cysticercosis includes idiopathic myositis,
tumours or metastasis, muscle abscess or haematoma, and other parasitic
infections like hydatid cyst.
Diagnosis
of Orbital Cysticercosis The
diagnosis of orbital and adnexal cysticercosis is based on clinical,
serological, and radiological findings. The clinical findings may occasionally
be non-specific and hence, non-diagnostic. Serological tests used for the
specific diagnosis are indirect hemagglutination, indirect immunofluorescence,
and immune electrophoresis such as enzyme-linked immunosorbent assay (ELISA)[20]. The serology may show false positive reports. Thus,
imaging studies are the most helpful in establishing the diagnosis. High
resolution ultrasonography (USG), computed tomography (CT) and magnetic
resonance imaging (MRI) help in detection of the orbital cyst. Stool
examination for the adult worm may be performed in cases of suspected
cysticercosis.
On
B-scan ocular ultrasonography, a well-defined cyst with a hyperechoic scolex is
seen[21]. On A-scan, high amplitude spikes
corresponding to the cyst wall and scolex is appreciated (Figure 3). The scolex
shows a high amplitude spike due to presence of calcareous corpuscles[7]. Ocular ultrasonography is a useful tool for diagnosis
and monitoring of the cyst during treatment.
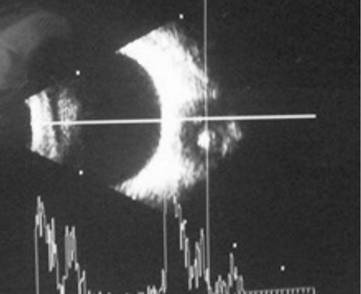
Figure 3
Ultrasonography of orbit showing a well-defined cyst lined by a cyst wall and a
hyperreflective scolex.
CT
scan of the orbits reveal a hypodense mass with a central hyperdensity
suggestive of scolex. Adjacent soft-tissue inflammation may be present (Figure
4). The scolex may not be visible if the cyst is dead or ruptured and has
surrounding inflammation. Concurrent neurocysticercosis should be excluded[5]. MRI reveals a hypointense cystic lesion and
hyperintense scolex within the extraocular muscle. A complete blood count may
reveal eosinophilia[22].

Figure 4 CT
scan of the orbit showing well defined cyst involving the right sided medial
rectus muscle suggestive of myocysticercosis (arrow).
ELISA
for Follow-up In a recent
study[23], ELISA using larval somatic and
excretory secretory (ES) antigens was positive in 32.5% and 45% cases
respectively. Anti-ES antibodies were detected more frequently in cases having
extra ocular cysts compared to intraocular location. These indigenous serum IgG
ELISAs might be useful as an adjunct to existing tools for diagnosis and in
post treatment follow up of extraocular form of cysticercosis in particular.
Management
of Orbital Cysticercosis In case of
subconjunctival cyst, excision biopsy is done to confirm the diagnosis followed
by CT scan imaging to rule out neurocysticercosis. In cases with proptosis,
restricted motility, inflammation or ptosis CT imaging must be performed to
rule out any cystic intramuscular lesion with scolex. If such a lesion is
present or ELISA is positive, oral albendazole[24] (15
mg/kg) and oral steroid (prednisolone 1 mg/kg) are given. In the presence of a
cystic lesion without scolex or when ELISA is negative, oral steroids must be
prescribed.
In
case of recurrence, repeat CT scan is required, and if there is a cystic
lesion, a repeat course of albendazole and steroid is to be given. When there
is no evidence of a cystic lesion then biopsy is indicated.
Medical
therapy is the recommended treatment for the extraocular muscle form and
retro-orbital cysticercosis[25].Surgical removal
is advocated for subconjunctival and eyelid cysticercosis. Treatment of optic
nerve and lacrimal gland cysticercosis is controversial due to the limited
number of cases involving the optic nerve and lacrimal gland.
OCULAR
CYSTICERCOSIS
Intraocular
cysticercosis can involve either the anterior or the posterior segment. While
anterior segment cysticercosis is rarely seen, posterior segment involvement
common.
Posterior
Segment Cysticercosis In the
posterior segment of the eye, vitreous cysts are more common than retinal or
subretinal cysts and the inferotemporal subretinal cyst is most frequently
encountered[26].
It
is hypothesized that the parasite reaches the posterior segment of the eye via
the high flow choroidal circulation through the short ciliary arteries. The
macular region being the thinnest and most vascularized, the larvae lodges
itself in the subretinal space from where it perforates and enters into the
vitreous cavity. In this process, the parasite can cause a retinal detachment,
macular hole or incite an inflammatory response. As the cyst develops, it
causes atrophic changes of the overlying retinal pigment epithelium. Sometimes,
it may cause exudative retinal detachment and focal chorioretinitis. The central
retinal artery is the most likely route for cysticercosis involving the optic
nerve head. Very few cases of optic nerve cysticercosis have been reported in
literature[27]. In a case report, surgical
removal of the cyst was attempted for the optic nerve cyst near the entrance of
the optic canal with remarkable visual recovery[28].
A
dying cysticercosis cyst can incite a severe inflammatory response, due to the
leakage of the toxins from the micro perforations present in the cyst wall[4]. Inflammatory reaction can be present even with living
parasite, and more so with vitreous cysts than subretinal cysts. Complications
of intraocular cysticercosis include severe inflammation (vitreous exudates,
organized membranes in vitreous), severe anterior chamber reaction, retinal
haemorrhages, retinal detachment, proliferative vitreoretinopathy, secondary
glaucoma, complicated cataract, hypotony and phthisis. Hence, differential
diagnosis of posterior segment cysticercosis includes the various causes of
leukocoria, choroidal tumours, serous retinal detachment and other parasitic
infections like toxoplasmosis and rarely diffuse unilateral subacute
neuro-retinitis.
Diagnosis
of Posterior Segment Cysticercosis The
diagnosis of cysticercosis is made by the clinical findings and supported by
other tests like serological tests (ELISA), USG (A and B scan), CT scan and MRI
scan.
On
indirect ophthalmoscopic examination, a live cyst can be seen as a translucent
white cyst with dense white spot formed by the invaginated scolex with typical
undulating movements (Figure 5). Serodiagnostic test is helpful but not
specific.
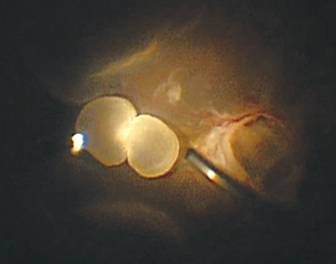
Figure 5
Intraoperative clinical photograph showing a posterior segment cysticercosis in
the vitreous.
A
scan ultrasonography shows high amplitude spikes corresponding to the cyst wall
and scolex, and B scan ultrasonography shows hanging drop sign i.e.
echoes corresponding to the cyst with the scolex attached to the inner wall
(Figure 6)[29]. CT scan of the orbit
is an effective technique to establish a diagnosis of ocular cysticercosis. It
is fast and economical when compared to MRI. Cysticercus is seen as a hypodense
mass with a central hyperdense scolex[30]. The
scolex may not be picked up if the cyst is dead or ruptured and has surrounding
inflammation. Neurocysticercosis must be excluded by MRI or CT scan.
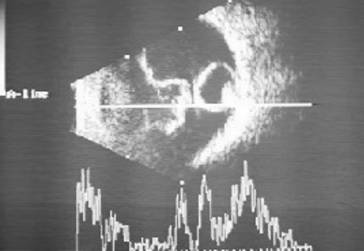
Figure 6
Ultrasonography of the globe revealing a well-defined cystic lesion with a
hyper-reflective scolex suggestive of intravitreal cysticercosis. There is
associated complete posterior vitreous detachment with attached retina.
Treatment
of Posterior Segment Cysticercosis Untreated
intraocular cysticercosis incites severe ocular inflammation, more so when the
cyst dies. Hence, surgery is the treatment of choice.
Intravitreal cysts Various modalities have been described in the surgical management of
intravitreal cysticercosis such as diathermy, photocoagulation and cryotherapy.
But these methods have now become obsolete as it results in the release of
toxins from the cyst causing severe intraocular inflammation. Surgical removal
of the cyst can be through either the transretinal or transscleral route.
Earlier, it was recommended that the cyst could be removed intoto
through one of the ports. The rationale was that the intoto removal
would help prevent any rupture of the cyst and release of toxic cyst products
into the ocular cavity that may induce severe vitritis.
In
the era of microincision vitrectomy surgery (MIVS), removal of the cysts using
the vitreous cutter is advocated. The high speed cutting rates with the maximum
suction ensures that the cyst contents barely come in contact with the ocular
structures with minimum release of toxins. Systemic corticosteroids are used
before and after surgical removal of the cysticercosis cyst. Medical therapy
other than corticosteroids is not advocated.
Subretinal cyst Earlier, small subretinal cysticercus was treated with xenon or argon
photocoagulation. Subretinal cysts anterior to the equator may be removed
transsclerally, whereas subretinal cysts posterior to the equator are best
removed transvitreally[6]. The cyst has
to be localized with indirect ophthalmoscopy, the exact site marked with
diathermy. A radial sclerotomy of adequate size is made at this site, and
preplaced sutures are placed. The choroid is exposed and obvious blood vessels
cauterized. Indirect ophthalmoscopy should be repeated to confirm that the
parasite had not moved. The cyst can be removed through the choroidal incision
with gentle pressure on the globe.
Pars
plana vitrectomy is the safest and effective technique to remove the cyst by
creating a retinotomy and bringing the cyst into the vitreous cavity. This
method ensures complete removal of the toxin and the remnants of the parasite.
Also, it avoids extensive periorbital dissection ensuring adequate retinopexy
and retinal reattachment with faster recovery.
Communicating cysticercosis Kumar et al[31] first described a
viable intravitreal cysticercus cellulosae in communication with subretinal
space. The cyst was removed intoto via the direct scleral approach
without incident. Multiple cysts in the same eye at different locations may be
present[32]. There may be a rhegmatogenous
retinal detachment associated with it. The current modality of treatment is
pars plana vitrectomy. Post-surgery, 86% of cases had attached retina after
10mo. The visual acuity correlated with preoperative visual acuity. A vision
loss of two lines was noted in 25% patients[6].
With timely pars plana vitrectomy, good visual acuity can be achieved in
patients with intravitreal and sub retinal cysticercosis without macular
involvement.
Anterior
Segment Cysticercosis Anterior
chamber cysticercosis is an unusual presentation and the occurrence of a live
free floating cyst in the anterior chamber is a rarer occurrence with very few
sporadic case reports of intracameral cysticercosis in literature[33].
The route
entry of the cyst in the anterior chamber is debatable. It can enter the
anterior chamber from posterior segment through the pupil in aphakes, through
vessels supplying the ciliary body[34-35]
or through the anterior chamber angle[8]. Ocular
cysticercosis is commonly seen in the younger age group of first or second
decade with no definite gender predilection[36].
The cyst may
be adherent to the adjacent structures like the iris, anterior lens capsule or
corneal endothelium by a stalk[37], or rarely
remains freely floating in the anterior chamber[38].
The patient remains asymptomatic if the cyst is small or may present with
complaints of diminution of vision, floater or leukocoria. There may be pain
and redness with associated iridocyclitis[39-40] or glaucoma. Glaucoma may be inflammatory in the
presence of iridocyclitis[39] or due to pupillary
block caused by the cyst[41]. Intracameral
cysticercosis has been confused with cataract[41]
or anteriorly dislocated lens[42].
The clinical
diagnosis of live intraocular cysticercosis is based on the morphology of the
parasite as visualized with the ophthalmoscope or slit-lamp biomicroscope. The
cyst and the scolex show characteristic undulating movements. When the scolex
is invaginated, a dense white spot called the receptaculum capitis[43] indicates its location within the cyst (Figure 7).
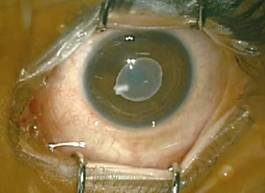
Figure
7 Clinical photograph showing an intracameral cysticercosis with invaginated
scolex.
As long as
the cyst is live, the anterior chamber reaction is absent or minimal. The
degenerative stage of dead scolex results in release of large amount of toxins
and heterologous protein causing a significant fibrinous reaction at the site
of the cyst[4].
Laboratory
studies are of limited value in intraocular cysticercosis. Eosinophilia is
usually absent unless there is widespread dissemination of the parasite.
Serological tests lack sensitivity[44]. The
indirect haemagglutination test shows cross reactivity between cysticercosis
and echinococcosis. Evidence of intestinal Taenia solium is seldom found in
human cysticercosis. Imaging like ultrasonography of the posterior segment and
orbit, CT scan or MRI of the brain helps to rule out other sites of involvement
by the cyst- both ocular as well as systemic, especially neurocysticercosis.
As
anthelminthic therapy can lead to severe inflammation in the event of a live
cyst degenerating, surgical removal of the parasite intoto is the mainstay of
treatment. Systemic cysticercosis should be ruled out especially
neurocysticercosis with the adequate neurosurgical examination and management
of the same, as it would require anthelminthic therapy with steroid cover after
intracameral cyst removal. The different surgical modalities of surgical
removal of anterior chamber cysticercosis cyst include paracentesis,
cryoextraction, erysiphake extraction, extraction with capsule forceps and viscoexpression[33].
Viscoexpression
is the treatment of choice as it is a simple and safe technique with minimal
surgical manipulation in the anterior chamber, minimal risk of cyst rupture and
does not require any sophisticated instrumentation or machinery. Beri et al[33] first described this procedure through a single 3 mm
supero-temporal incision. Another modification of this technique is a
double-incision viscoexpression method described by Kai et al[38] for the removal of a large intracameral cyst. Intracameral
cysticercosis is a rare occurrence and a timely diagnosis and intervention can
optimize the visual outcome.
Cysticercosis
is a disease closely related to improper hygiene and sanitary conditions.
Therefore prevention by health education of the population is an important
aspect of disease control. Prevention is possible by avoiding the consumption
of undercooked or raw pork, proper washing of hands after using toilets and
before food handling and by washing and peeling of raw vegetables and fruits before
eating. Ocular and orbital cysticercosis has varied clinical manifestations
depending upon the site of involvement, stage of the cyst and the host-immune
responses. With the advent of the new imaging techniques, ocular and orbital
cysticercosis is now increasingly diagnosed even in non-endemic zones. A high
index of suspicion along with characteristic features on imaging helps us to
establish an accurate diagnosis and initiate appropriate treatment depending
upon the site of involvement.
ACKNOWLEDGEMENTS
Conflicts
of Interest: Dhiman R, None; Devi S, None; Duraipandi K,
None; Chandra P, None; Vanathi M, None; Tandon R, None; Sen
S, None.
REFERENCES
1
David S, Mathai E. Ocular cysticercosis--a review of 25 cases. J Assoc Physicians India 2000;48(7):704-707.
[PubMed]
4
Lombardo J. Subretinal cysticercosis. Optom
Vis Sci 2001;78(4):188-194. [CrossRef]
[PubMed]
5
Pushker N, Bajaj MS, Betharia SM. Orbital and adnexal cysticercosis. Clin Exp Ophthalmol 2002;30(5):322-333.
[CrossRef] [PubMed]
6
Sharma T, Sinha S, Shah N, Gopal L, Shanmugam MP, Bhende P, Bhende M, Shetty
NS, Agrawal R, Deshpande D, Biswas J, Sukumar B. Intraocular cysticercosis:
clinical characteristics and visual outcome after vitreoretinal surgery. Ophthalmology 2003;110(5):996-1004. [CrossRef]
7
Rahalkar MD, Shetty DD, Kelkar AB, Kelkar AA, Kinare AS, Ambardekar ST. The
many faces of cysticercosis. Clin Radiol
2000;55(9): 668-674. [CrossRef]
[PubMed]
8
Sekhar GC, Lemke BN. Orbital cysticercosis. Ophthalmology
1997;104: 1599-1602. [CrossRef]
9
Malik SR, Gupta AK, Choudhry S. Ocular cysticercosis. Am J Ophthalmol 1968;66(6):1168-1171. [CrossRef]
10
Reddy PS, Satyendran OM. Ocular cysticercosis. Am J Ophthalmol 1964;57:664-666. [CrossRef]
11
Kruger-Leite E, Jalkh AE, Quiroz H, Schepens CL. Intraocular cysticercosis. Am J Ophthalmol 1985;99(3):252-257. [CrossRef]
12
Sen DK, Mathur RN, Thomas A. Ocular cysticercosis in India. Br J Ophthalmol 1967;51(9):630-632. [CrossRef]
14
Rath S, Honavar SG, Naik M, Anand R, Agarwal B, Krishnaiah S, Sekhar GC.
Orbital cysticercosis: clinical manifestations, diagnosis, management, and
outcome. Ophthalmology
2010;117(3):600-605. [CrossRef]
[PubMed]
15
Sundaram PM, Jayakumar N, Noronha V. Extraocular muscle cysticercosis-a
clinical challenge to the ophthalmologists. Orbit
2004; 23(4):255-262. [CrossRef]
[PubMed]
17
Agrawal S, Ranjan S, Mishra A. Ocular myocysticercosis: an unusual case of
ptosis. Nepal J Ophthalmol
2013;5(2):279-281. [CrossRef]
18
Goyal JL, Das S, Kumar S, Chauhan D, Baheti U, Sangit V. Retrobulbar
cysticercosis masquerading as optic nerve glioma. Orbit 2007;26(1):61-63. [CrossRef]
[PubMed]
19
Bawa YS, Wahi PL. Cysticercosis cellulosae of the optic disc with generalized
cysticercosis. Br J Ophthalmol
1962;46(12):753-755. [CrossRef] [PMC free article] [PubMed]
20
Diwan AR, Coker-Vann M, Brown P, Subianto DB, Yolken R, Desowitz R, Escobar A,
Gibbs CJ Jr, Gajdusek DC. Enzyme-linked immunosorbent assay (ELISA) for the
detection of antibody to cysticerci of Taenia solium. Am J Trop Med Hyg 1982;31(2):364-369. [CrossRef]
21
Honavar SG, Sekhar CG. Ultrasonological characteristics of extraocular
cysticercosis. Orbit
1998;17(4):271-284. [CrossRef]
[PubMed]
22
Murthy GR, Rao AV. Sub-conjunctival cysticercosis. Indian J Ophthalmol 1980;28(2):77-78. [PubMed]
24
Sihota R, Honavar SG. Oral albendazole in the management of extraocular
cysticercosis. Br J Ophthalmol 1994;78(8):621-623.
[CrossRef] [PMC free article] [PubMed]
25
Mohan K, Saroha V, Sharma A, Pandav S, Singh U. Extraocular muscle
cysticercosis: clinical presentations and outcome of treatment. J Pediatr Ophthalmol Strabismus
2005;42(1):28-33. [PubMed]
27
Madan VS, Dhamija RM, Gill HS, Boparai MS, Souza PD, Sanchete PC, Bhardwaj JR.
Optic nerve cysticercosis: a case report. J
Neurol Neurosurg Psychiatr 1991;54(5):470-471. [CrossRef]
28
Gurha N, Sood A, Dhar J, Gupta S. Optic nerve cysticercosis in the optic canal.
Acta Ophthalmol Scand
1999;77(1):107-109. [CrossRef]
29
Gulani AC. Sonographic diagnosis of orbital cysticercus cyst: The "Hanging
Drop Sign". J Diagn Med Sonography
1998;14(3):122-124. [CrossRef]
30
Sekhar GC, Honavar SG. Myocysticercosis: experience with imaging and therapy. Ophthalmology 1999;106(12):2336-2340. [CrossRef]
31
Kumar A, Verma L, Khosla PK, Tewari HK, Jha SN. Communicating intravitreal
cysticercosis. Ophthalmic Surg
1989;20(6):424-426. [PubMed]
32
Topilow HW, Yimoyines DJ, Freeman HM, Young GA, Addison R. Bilateral multifocal
intraocular cysticercosis. Ophthalmology
1981;88(11): 1166-1172. [CrossRef]
33
Beri S, Vajee RB, Dhingra N, Ghose S. Managing anterior chamber cysticercosis
by viscoexpression: a new surgical technique. Arch Ophthalmol 1994;112(10):1279-1280. [CrossRef]
34
Aracena T, Roca FP. Macular and peripheral subretinal cysticercosis. Ann Ophthalmol 1981;13(11):1265-1267. [PubMed]
35
Bartholowmew RS. Subretinal cysticercosis. Am
J Ophthalmol 1975; 79(4):670-673. [CrossRef]
36
Pushker N, Kashyap S, Gautam VP, Bajaj MS. Ocular cysticercosis-a profile. Trop Doct 2004;34(4):256. [CrossRef]
[PubMed]
38
Kai S, Vanathi M, Vengayil S, Panda A. Viscoexpression of large free floating
Cysticercus cyst from the anterior chamber of the eye by double incision
technique. Indian J Med Microbiol
2008;26(3):277-279. [CrossRef]
39
Mahendradas P, Biswas J, Khetan V. Fibrinous anterior uveitis due to
cysticercus cellulosae. Ocul Immunol
Inflamm 2007;15(6):451-454. [CrossRef]
[PubMed]
40
Takkar B, Chandra P, Kumar K, Vanathi M. Toxic granulomatous anterior uveitis
in live intracameral cysticercosis masquerading as leukocoria. Can J Ophthalmol 2014;49(6):e140-e141. [CrossRef]
[PubMed]
41
Chandra A, Singh MK, Singh VP, Rai AK, Chakraborty S, Maurya OP. A live
cysticercosis in anterior chamber leading to glaucoma secondary to pupilary
block. J Glaucoma 2007;16(2):271-273.
[CrossRef] [PubMed]
42
Kapoor S, Sood GC, Aurora AL, Sood M. Ocular cysticercosis. Report of a free
floating cysticercus in the anterior chamber. Acta Ophthalmol (Copenh)
1977;55(6):927-930. [CrossRef]
44
Wadhwa V, Kharbanda P, Rai S. How reliable are serological tests in diagnosis
of cysticercosis? Indian J Med Microbiol
2006;24(1):78-79. [CrossRef] [PubMed]