
·Meta-Analysis· Current
Issue IF in JCR CiteScore ·Submission· In Press Recent Accepted PMC RSS
A case of non-Acanthamoeba keratitis with radial
keratoneuritis
Xiu Wang1, Patrick Glencer2,
Rui-Hua Wei1
1Tianjin Medical University Eye Hospital, Tianjin 300384, China
2Nova Southeastern University College of Optometry, 2640 S
University Dr #312 Davie, FL, USA
Correspondence
to: Rui-Hua Wei. Tianjin Medical University Eye Hospital, No.251 Fu
Kang Road Nankai District, Tianjin 300384, China. braveheart0717@sina.com
Received:
2016-02-03 Accepted: 2016-12-13
DOI:10.18240/ijo.2017.08.22
Citation: Wang X, Glencer P, Wei RH. A case of non-Acanthamoeba keratitis with
radial keratoneuritis. Int J Ophthalmol 2017;10(8): 1325-1327
Dear
Editor,
I
am Dr. Xiu Wang, from Tianjin Medical University Eye Hospital, Tianjin, China.
I write to present one case report of non-Acanthamoeba keratitis with radial
keratoneuritis (RK).
Keratitis
that is caused by free living amoeba (Acanthamoeba) can cause devastating
ocular damage. It is associated with trauma and contamination with water, soil,
sewage, etc[1]. RK is pathognomonic for
Acanthamoeba keratitis (AK) and is apparent in the early stages[2]. Because of this, RK is useful in identifying and
diagnosing AK. This case report shows suspected AK because of the presence of
RK. However, the laboratory examination, clinical progression, patient’s
symptoms, slit-lamp biomicroscopy and the effectiveness of the therapeutic
drugs finally lead to the diagnosis of non-Acanthamoeba keratitis with RK.
A
22-year-old Asian male patient presented with eye redness, tearing, mild pain
and difficulty opening in his left eye. Written informed consent was obtained
from the patient for publication of this case report and any accompanying
images. All symptoms in his left eye had occurred for two months. Symptoms
worsened dramatically four days prior to being referred to Tianjin Medical
University Eye Hospital. He stated his symptoms first occurred with an
accompanying headache after a large consumption of alcohol. At a local county
hospital, he was diagnosed with left ocular keratitis and was given topical
levofloxacin and ganciclovir. After three days with no improvement, the
treatment regimen was changed to intravenous (I.V.) antibiotics. Three days
after I.V. treatment, the patient’s tearing symptom improved, but the
discontinuation of therapy resulted in a relapse. I.V. antibiotics were resumed
for an additional six days. Once again his tearing subsided, but after
discontinuing the drugs the symptoms returned. He was then referred to our
hospital for further evaluation. The patient reported no history of ocular
trauma, contact lens wear, or exposure to contaminated water. Upon eye
examination, visual acuity was 20/80 (OD) and 20/50 (OS). The intraocular
pressures were within the normal range. The corneal sensation was decreased.
Due to eye irritation, photophobia and other severe symptoms, the best
corrected visual acuity (BCVA) was not checked. The right eye had no
significant signs or symptoms. The left eye had no secretion, but had ciliary
congestion temporally and the eyelid was swollen. A branch-like defect due to
corneal inflammation was seen around the nerve. The area affected was seen
traveling along the corneal nerves within the superior temporal corneal stroma
at about 1 o’clock position. Flakes 3×4 mm2 were seen in corneal
stroma superficially. The invasion of cells could be seen partially at the
temporal side of the central zone. The corneal stroma was mildly edematous and
cloudy (Figure 1A). The corneal epithelium showed no sodium fluorescein
staining (Figure 1B). The patient did not have any corneal deposits and the
anterior chamber was clear of cells and flare. Iris texture was normal, the
pupil was round (drug-induced mydriasis) and the lens was transparent. Corneal
scrapings detected edematous epithelial cells and a small amount of
inflammatory cells. No pathogenic microorganisms, amoebic cysts or trophozoites
were found. Culture experiments were performed with various types of media and
the results were all negative. Liver and kidney function tests, a complete
blood count (CBC), prothrombin time (PT), and routine autoimmune tests came
back negative without any conspicuous abnormalities. Due to the idiopathic
nature of the corneal inflammation, the use of topical levofloxacin was
continued. Topical pranoprofen and artificial tears (q.i.d) were added
at the beginning of treatment. The patient had a regimen of 100 mg oral
acyclovir after breakfast five times a day. After three days, the patient had
no significant changes in symptoms. Corneal staining showed that the corneal
epithelium had been repaired, but the subepithelial infiltration was still
apparent. The patient was placed on 0.1% fluorometholone (b.i.d). The
following day, the patient’s tearing symptoms improved. The application of
fluorometholone was increased to q.i.d and the use of tobradex ointment
was applied once a day at night. During the first five days, eye pain and
tearing had diminished and both eyes were able to open freely. Visual acuity
gradually increased to 20/32, with a BCVA to 20/20 (-1.75 DS). Partial temporal
branching of infiltrates became thinner and the irregular flakes in the partial
temporal were faded. Corneal edema was mitigating (Figure 2A). After using 0.1%
fluorometholone q.i.d and tobradex ointment every night, the patient was
treated with 0.1% fluorometholone once a day for another two months. After 28d
of treatment, there were no signs of corneal edema and the branching of
infiltrates was not obvious (Figure 2B). We have followed the patient for half
a year and there was no recurrence.
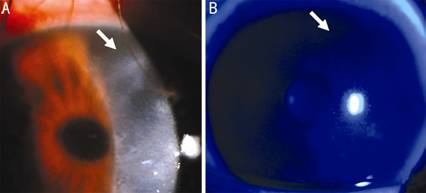
Figure
1 There were radial keratoneuritis at presentation within the corneal stroma superior temporally about 1 o’clock and
3×4 mm2 flakes were seen in corneal stroma superficially (A);
Left eye’s corneal epithelium showed no sodium fluorescein staining (B).
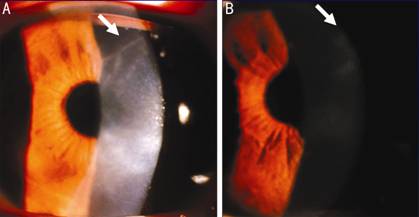
Figure
2 After 4d of topical steroids treatment, the partial temporal branching of
infiltrates became thinner and the irregular flakes in the superficial stroma were
faded (A); After 28d treatment, corneal edema was missing and the branching of
infiltrates was not as obvious (B).
Although
RK is a very helpful sign, it is not always present, especially late in the
process of AK. A study by Sun et al[3]
reported an incidence of RK in 2 (10%) of the 20 patients with AK. In another
study, Bacon et al[4] reported an incidence
of RK at presentation of 57% among 36 eyes diagnosed within 1mo of the onset,
declining to 29% among 24 eyes diagnosed after 2mo. Bernauer et al[5] summarized 70 cases of AK. Five cases showed signs of
RK (7%). Bacon et al[4] examined 72 cases
(77 eyes) with AK, nine of which were reported to have had RK (13%). At this
present time there have a few other cases of non-Acanthamoeba keratitis with
RK. Feist et al[6], Roels et al[7] and Robbie et al[8]
had reported that they diagnosed a RK in Pseudomonas keratitis.
Shinoda
et al[9] have been reported a RK case with
no evidence for any bacteria, fungi, or Acanthamoeba of these examinations, in
that case, antifungal drugs were only used for a short period of time and the
keratitis was cured. Mutoh et al[10]
reported one case which was diagnosed first as AK based on the corneal smear,
then was treated as Herpes simplex keratitis (HSK) due to lack of response to
anti-Acanthamoeba treatment, and finally was treated with topical steroids.
Kapoor et al[11] reported a case of fungal
keratitis presenting as RK.
The
patient, in this case, already had symptoms for two months prior to treatment.
The paracentral of cornea showed turbidity consistent with the infiltrates
which had invaded the stroma. In the late stage of AK a corneal opacity can
appear and can coexist with a hypopyon.
Before
the onset of symptoms, this patient had a history of heavy alcohol consumption,
but no history of trauma or foreign bodies. His signs and symptoms included
photophobia, lacrimation without mucopurulent secretion, and mild eye pain
associated with an ipsilateral migraine. Confocal microscopy was left to be
desired as our hospital is unequipped. Because of the negative corneal
scrapings, the diagnoses of a bacterial, fungal and Acanthamoeba infection
could be ruled out. The three main risk factors (use of contact lenses,
contaminated water and corneal trauma) were not associated with this patient
per the history given. No significant epithelial defects or ulcers were found
clinically. Steroid treatment proved to be effective but the RK still remained.
The patient had no autoimmune disorders, so any immunological condition that
could cause keratitis may also be excluded. In this case, a virus should be
considered given the fact that a virus can remain latent in human tissues for a
long period of time. Given the human bodies’ ability to promote homeostasis, a
virus may not cause symptoms and remain in it’s dormant state. Once the immune
system has been compromised, the virus may multiply and cause a reaction. The
predisposing factors of this patient were a relatively large consumption of
alcohol and fatigue. The fact that the other diagnoses were ruled out, the
herpes viral infections that can cause corneal disruption should be considered.
Only
one case report in the literature has been reported investigating viral
keratitis associated with RK[10]. This case
report may provide new ideas of RK analysis and differential diagnoses.
ACKNOWLEDGEMENTS
Conflicts
of Interest: Wang X, None; Glencer P, None; Wei RH,
None.
REFERENCES
1 Sharma S, Garg P, Rao GN. Patient characteristics,
diagnosis, and treatment of non-contact lens related Acanthamoeba keratitis. Br J Ophthalmol 2000;84(10):1103-1108. [CrossRef] [PMC free article] [PubMed]
2 Sasaki M, Sotozono C, Chihara H, Ueta M, Inatomi T,
Yokoi N, Shiota T, Kinoshita S. Characteristic appearance of early-stage
Acanthamoeba keratitis. Nippon Ganka
Gakkai Zasshi 2010;114(12):1030-1035. [PubMed]
3 Sun X, Zhang Y, Li R, Wang Z, Luo S, Gao M, Deng S,
Chen W, Jin X. Acanthamoeba keratitis: clinical characteristics and management.
Ophthalmology 2006;113(3):412-416. [CrossRef] [PubMed]
4 Bacon AS, Frazer DG, Dart JK, Matheson M, Ficker LA,
Wright P. A review of 72 consecutive cases of Acanthamoeba keratitis,1984-1992.
Eye (Lond) 1993;7(Pt 6):719-725. [CrossRef] [PubMed]
5 Bernauer W, Duguid GI, Dart JK. Early clinical
diagnosis of acanthamoeba keratitis. A study of 70 eyes. Klin Monbl Augenheilkd 1996;208(5):282-284. [CrossRef] [PubMed]
6 Feist RM, Sugar J, Tessler H. Radial keratoneuritis
in Pseudomonas keratitis. Arch Ophthalmol
1991;109(6):774-775. [CrossRef] [PubMed]
7 Roels D, De Craene S, Kestelyn P. Keratoneuritis is
not pathognomonic of Acanthamoeba keratitis:a case report of Pseudomonas
keratitis. Int Ophthalmol
2017;37(1):257-258. [CrossRef] [PubMed]
8 Robbie SJ, Vega FA, Tint NL, Hau S, Allan B.
Perineural infiltrates in Pseudomonas keratitis. J Cataract Refract Surg 2013;39(11):1764-1767. [CrossRef] [PubMed]
10 Mutoh T, Matsumoto Y, Chikuda M. A case of radial
keratoneuritis in non-Acanthamoeba keratitis. Clin Ophthalmol 2012;6:1535-1538. [CrossRef] [PMC free article] [PubMed]