INTRODUCTION
Pseudoexfoliative glaucoma (PEG) is the most common type of secondary open angle glaucoma[1-2]. The clinical signs of PEG are well known. This type of glaucoma is more aggressive than primary open angle glaucoma (POAG);intraocular pressure (IOP) is higher, IOP fluctuations are excessive, and there is substantial damage to the optic nerve and visual field[3-4]. Moreover, PEG has a limited response to medical treatment[5]. In addition to these clinical differences,vasculopathy of the iris and disruption of the blood-aqueous barrier may cause postoperative fibrin exudation, and microneovascularization of the iris may cause intraoperative and late-onset hyphema[6-8]. Variations in this condition’s course and response to medical treatment suggest that response to surgical treatment may also vary.
Some studies have compared the success of trabeculectomy to treat PEG and POAG. Ehrnrooth et al[9]investigated immediate and mean 4y follow-up outcomes after trabeculectomy and reported lower success in PEG patients. However, Serguhn and Spiegel[10]found no differences with respect to surgical success in patients with PEG or POAG, while Törnqvist and Drolsum[11]reported high success in PEG patients during a long-term follow-up period.
Although the results in the literature vary, IOP <21 mm Hg was considered to indicate a successful procedure[7-10]. However,this is currently considered to be a rather high pressure for patients who have undergone trabeculectomy, and it is also higher than the target IOP. Thus, whether this IOP value truly indicates a successful procedure is subject to debate.
The purpose of this study was to compare the long-term results of trabeculectomy in PEG and POAG patients with respect to three different success criteria.
SUBJECTS AND METHODS
We retrospectively analyzed the records of patients who underwent primary trabeculectomy in the Trakya University Ophthalmology Department in 1993-2013. Patients diagnosed with PEG and POAG who had no additional glaucoma surgery in the postoperative period, regular records, and were followed up for at least 24mo were included in the study. To definitively diagnose PEG, pseudoexfoliative material should be seen in the anterior segment, IOP should be >21 mm Hg, and typical glaucomatous visual field damage must be present[1-2].
Table 1 Clinical characteristics of patients with PEG and POAG

aIndependent t-test;bChi-square test with Yates correction;cMann-Whitney U test. IOP: Intraocular pressure; PEG:Pseudoexfoliative glaucoma; POAG: Primary open angle glaucoma.
Patients with a history of cataract surgery or any other ocular surgery before trabeculectomy, ocular trauma, or any ocular disease other than glaucoma were excluded from the study.A total of 115 eyes from 115 patients matching the inclusion criteria were evaluated. One randomly selected eye was enrolled in the study for patients who underwent bilateral trabeculectomy.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study
Patients’ data were examined for age at the time of trabeculectomy,gender, preoperative medical treatment and duration, and preoperative IOP measured by Goldmann applanation tonometer. Patients with high IOP despite the maximum tolerated medical therapy or ongoing glaucomatous damage underwent trabeculectomy. All operations were performed with the same technique. A limbus-based conjunctival flap was prepared, and then a 3×3 mm2half-scleral-thickness scleral flap was dissected up to the transparent cornea mitomycin-C(MMC) applied innecessary cases under the conjunctiva. A 2×2 mm2trabecular block was removed with the help of a razor blade, and a peripheral iridectomy was performed. The scleral flap was sutured with 2-4 pieces of 10/0 nylon suture, and the conjunctiva was sutured with 8/0 vicryl suture. Postoperatively,topical cycloplegic agents, antibiotics, and steroid drops were applied to the patients. Postoperative needling and argon laser sutureless treatments were recorded. Postoperative 1d,1, 3, 6mo, and 1y and later annual examination outcomes were evaluated. During follow-up, events in which glaucoma medication was added and cataract surgeries were performed were also examined. Increased IOP despite medical treatment and requirements for a second glaucoma surgery were considered as “end of the follow-up period”.
The success of the trabeculectomy was evaluated by three criteria: A) IOP ≤21 mm Hg and decrease in IOP ≥20%; B)IOP ≤18 mm Hg and decrease in IOP ≥30%; C) IOP≤15 mm Hg and decrease in IOP ≥50%. Patients that met these criteria without medical treatment were considered to be“complete success”, while those that met these criteria with medical treatment were considered “qualified success”[12-14].
Statistical Analysis Normality distribution of the variables was tested by one sample Kolmogorov Smirnov test. The Students’ t-test was used for normally distributed, and Mann-Whitney U test was used for non-normally distributed data.Also, categorical variable were compared by Chi-square (Yates of Fisher exact) tests. The Kaplan-Meier survival analysis was carried out to calculate survival curves, and Log-rank test was used for group comparisons (POAG vs PEG). P<0.05 was assumed significant for all analysis.
RESULTS
Sixty-four eyes from 64 patients with PEG and 51 eyes from 51 patients with POAG were included in the study. Fifty-six of the patients (48.7%) were males, and 59 of the patients (51.3%)were females. The mean age at the time of the trabeculectomy was 65±10y. There was no significant difference between PEG and POAG patients with respect to mean age, gender,mean preoperative IOP, mean postoperative first IOP values,initiation time of medical treatment in postoperative period,and follow-up time (P=0.49, 1.00, 0.75, 0.47, 0.07 and 0.11,respectively). However there was a significant difference between PEG and POAG patients with respect to duration of preoperative medical treatment and final IOP (P=0.03, 0.01)(Table 1). In addition, there was no significant difference between PEG and POAG patients with respect to number of cases peroperative MMC usage, postoperative needling,subconjunctival 5 fluorouracil injection, laser suture lysis and hypotony (P=0.68, 0.34, 0.36, 0.85, 0.87, respectively)(Table 2).1Chi-square test with Yates correction. MMC: Mitomycine C; 5-FU:5 fluorouracil; PEG: Pseudoexfoliative glaucoma; POAG: Primary open angle glaucoma.
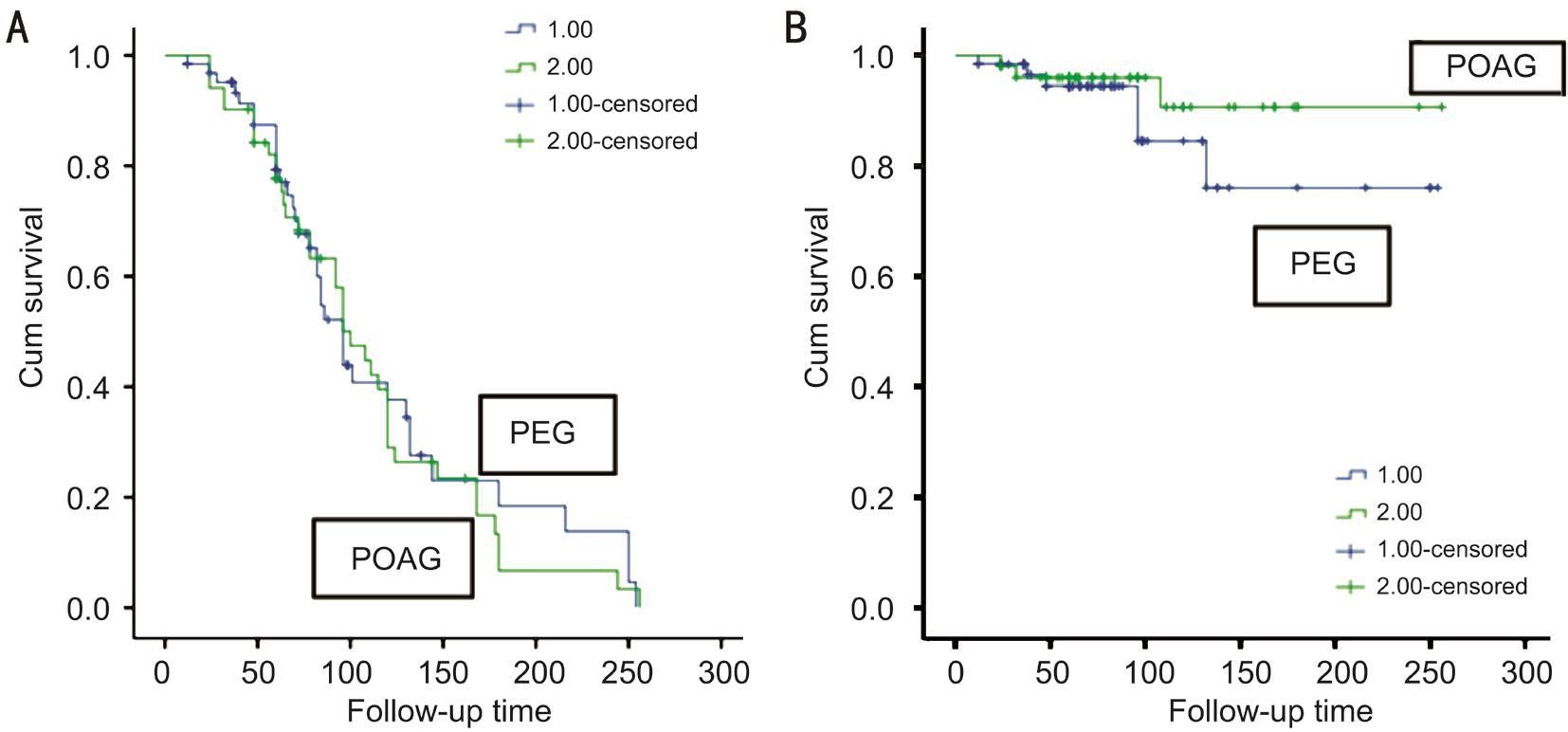
Figure 1 Kaplan-Meier survival analysis of full (A) and partial (B) success of trabeculectomy in patients according to criterion A in PEG and POAG groups.
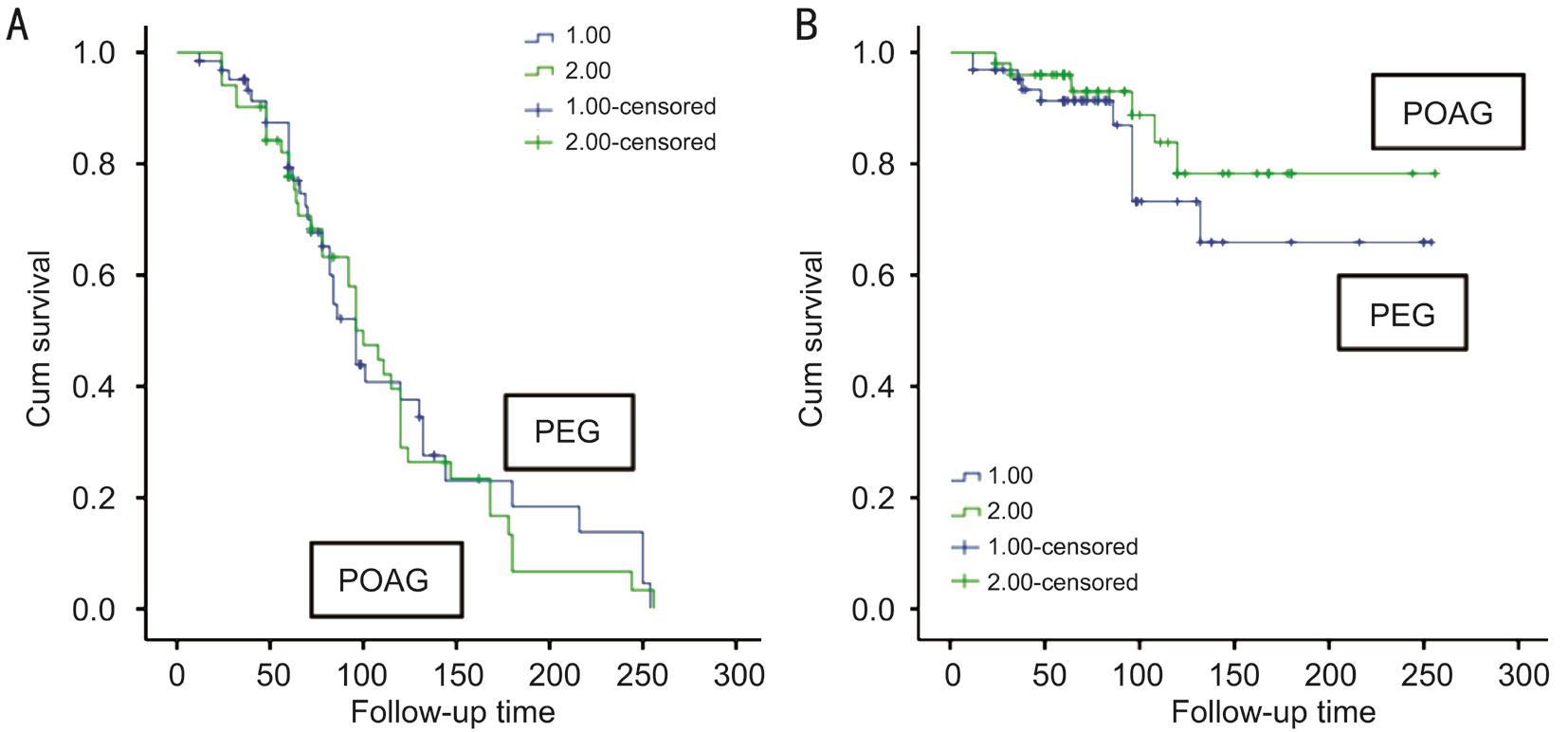
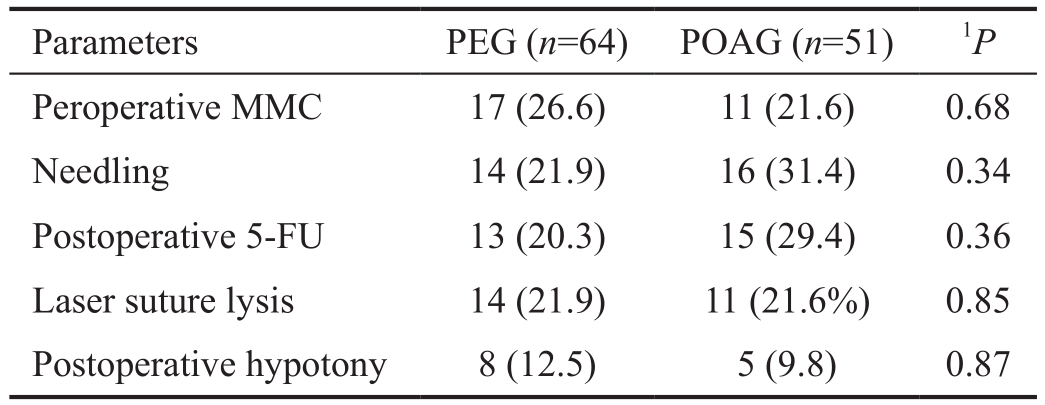
Figure 2 Kaplan-Meier survival analysis of full (A) and partial (B) success of trabeculectomy in patients according to criterion B in PEG and POAG groups.
Table 2 Peroperative and postoperative characteristics of patients with PEG and POAG n (%)
The number of with complete success that met criterion A was 28 (43.8%) in the PEG group and 12 (23.5%) in the POAG group. The number of complete success cases that met criterion B was 28 (43.8%) in the PEG group and 13 (25.5%)in the POAG group. The number of complete success cases that met criterion C was 24 (37.5%) in the PEG group and 10(19.6%) in the POAG group (Table 3).
When we compared surgical success by the log-rank test between PEG and POAG groups with respect to criteria A-C,we found no significant differences in complete and qualified success between the two groups (Figures 1, 2 and 3; Table 4).
DISCUSSION
We investigated the long-term results of 115 eyes from 115 patients who underwent trabeculectomy for PEG or POAG. By 81±56 (min 12-max 254)mo post-trabeculectomy in the PEG group and 94±54 (min 24-max 256)mo post-trabeculectomy in the POAG group, according to our three criteria, there was no difference with respect to surgical success between the two groups.
Previous studies have compared the success of trabeculectomy to treat PEG and POAG. Mietz et al[15]evaluated the trabeculectomy outcomes of 709 eyes from 506 patients with variable types of glaucoma at the end of a mean 27.9mo follow-up period. They concluded that there was no difference in surgical success between PEG and POAG cases.
Ehrnrooth et al[9]compared the success of trabeculectomy in 138 eyes (55 POAG cases and 83 PEG cases) after 2-5y of follow-up. They found a significantly higher rate of full success for patients with POAG and demonstrated that in patients with PEG, an IOP of >30 mm Hg in the early postoperative period had a negative impact on the success of trabeculectomy.However, in this study, the meanages of patients, preoperative IOPs and differences between follow-up periods were not compared. In addition, patients who underwent additional surgery after trabeculectomy were not excluded from study.
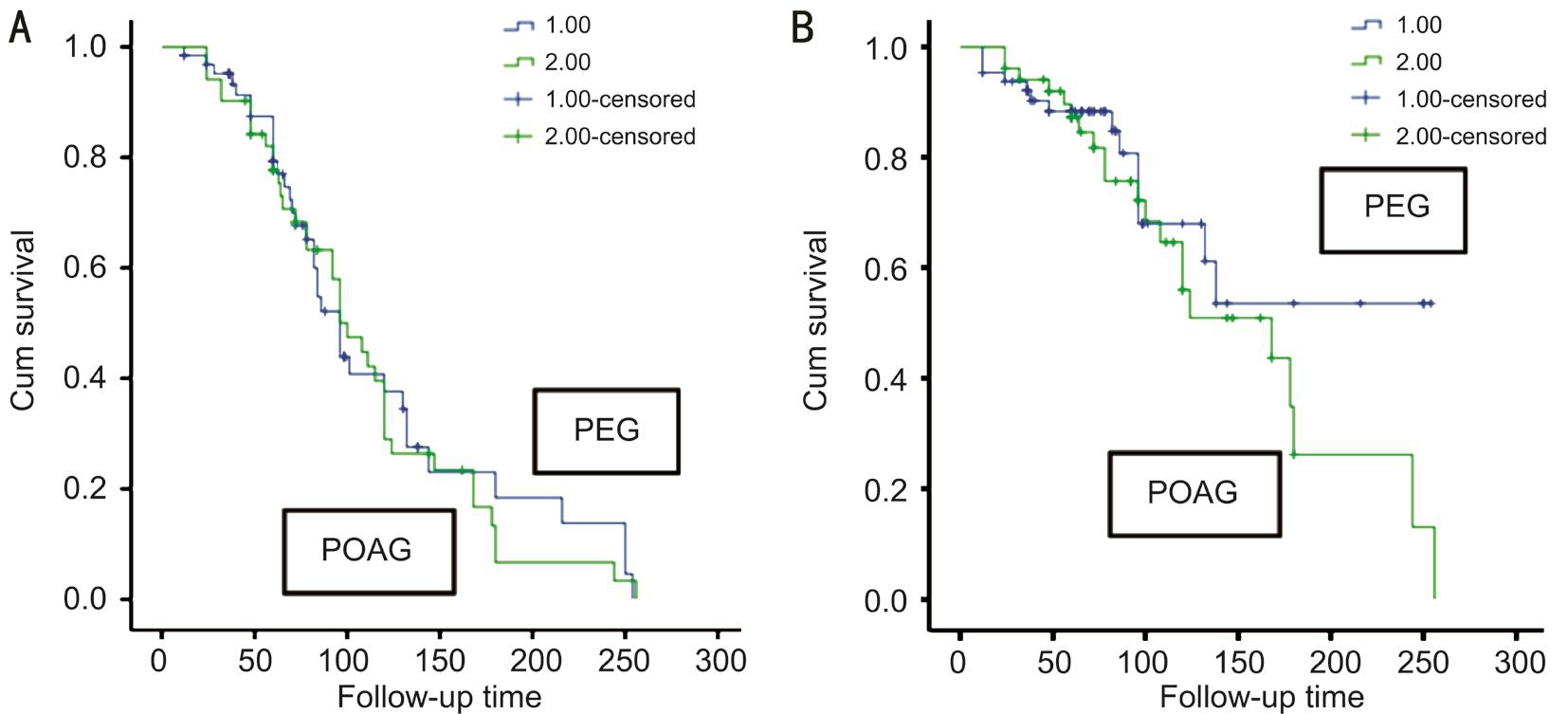
Figure 3 Kaplan-Meier survival analysis of full (A) and partial (B) success of trabeculectomy in patients according to criterion C in PEG and POAG groups.
Table 3 Complete and qualified success rates of trabeculectomy according to criteria A-C in patients with PEG or POAG n (%)

PEG: pseudoexfoliative glaucoma; POAG: primary open angle glaucoma.
Table 4 Comparison of success of trabeculectomy between PEG and POAG groups1P

1Log-rank test. PEG: Pseudoexfoliative glaucoma; POAG: Primary open angle glaucoma.
Törnqvist and Drolsum[11]reported that in 43% of cases with POAG and 64% of patients with PEG, no additional treatment was required 10y after trabeculectomy. But Törnqvist and Drolsum[11]have not done survival analysis for the statistical evaluation.
Fernández et al[16]found surgical success rates of 99.3% at the end of 1y, 90.6% at the end of 5y, 76.7% at the end of 10y,70.1% at the end of 15y, and 45.9% at the end of 20y in 956 eyes that had undergone trabeculectomy and been followed for 3-20y. This study included POAG, PEG, and primary angleclosure glaucoma (PACG) patients. In the full-success group,PACG patients had the lowest surgical success. When the authors evaluated partial success in the first 5y period, they found no significant difference among the three glaucoma types with respect to surgical success, but they did find a significant difference after 10y for POAG and after 15y for PEG.The reason for differences in the success of trabeculectomy in patients with PEG and POAG may be due to variations in patient selection. In some of these studies, the mean ages of the patients were different. In addition, surgical techniques,success criteria and the follow-up period were quite variable in the studies.
Another important factor when determining the success of trabeculectomy is the follow-up period. Patients with a longer follow-up period have decreased surgical success. To the best of our knowledge, this has been the result of all studies that have investigated the success of trabeculectomy[9,17-21].
Although the results of the studies were different, all of the studies used the same success criteria; namely, an IOP of<21 mm Hg without additional treatment was considered a full success, while the same IOP with medical treatment in the postoperative period was considered a partial success.However, in clinical practice, an IOP of ≤21 mm Hg in the eye with glaucoma is generally not considered to be an acceptable value. Most clinicians would prefer an IOP of <14 mm Hg in these cases. Of particular concern is the decreased thickness in the lamina cribrosa that may accompany PEG, which can make the eye more sensitive to pressure[22]. The ideal way to determine surgical success is to consider the target IOP of each individual. However, this makes it difficult to perform statistical analyses. The solution may be to use more than one criterion to evaluate success, which is why we evaluated IOP values according to three different success criteria.
In the literature, there are studies that compares PEG patients treatment outcomes other than trabeculectomy and POAG[22-24].Ting et al[22], compared the results of ab interno trabeculectomy(by the trabectome tecnique) in 450 patients with POAG and 67 patients with PEG. At the end of 1y follow up period,better results were obtained in PEG group. In their study to evaluate the success of trabectome, Jordan et al[23]did not find any difference for complete success between POAG and PEG group, but they detected stastically significant increased qualified success in PEG group. In these studies to perform trabecular aspiration during trabectome application might be the reason of increased success in PEG group.
In summary, we found that there was no difference in the long-term success of trabeculectomy between PEG and POAG patients whose clinical characteristics are otherwise the same. The limitation of the study was that we were unable to investigate the presence of concomitant diabetes, vascular disease and presence of cataract. In our study, there were no significant differences in the mean age and follow-up periods of the PEG and POAG patients. Moreover, these patients had not had another ocular surgery, disease, or trauma prior to trabeculectomy, and this was the first trabeculectomy that they had undergone. There are some differences for clinical course and response to medical treatment between PEG and POAG group. Although, there is no difference for the success of trabeculectomy between two groups.
ACKNOWLEDGEMENTS
The authors thank to Professor Necdet Sut.
Conflicts of Interest: Pelitli Gürlü V, None; Güçlü H, None;Özal A, None; Benian Ö, None; Alimgil L, None.
REFERENCES
1 Ritch R, Schlötzer-Schrehardt U. Exfoliation syndrome. Surv Ophthalmol 2001;45(4):265-315.
2 Vesti E, Kivelä T. Exfoliation syndrome and exfoliation glaucoma. Prog Retin Eye Res 2000;19(3):345-368.
3 Moghimi S, Johari M, Mahmoudi A, Chen R, Mazloumi M, He M, Lin SC. Predictors of intraocular pressure change after phacoemulsification in patients with pseudoexfoliation syndrome. Br J Ophthalmol 2017;101(3):283-289.
4 Kristianslund O, Østern AE, Råen M, Sandvik GF, Drolsum L. Does cataract surgery reduce the long-term risk of glaucoma in eyes with pseudoexfoliation syndrome? Acta Ophthalmol 2016;94(3):261-265.
5 Sein J, Galor A, Sheth A, Kruh J, Pasguale LR, Karp CL. Exfoliation syndrome: new genetic and pathophysiologic insights. Curr Opin Ophthalmol 2013;24(2):167-174.
6 Conway RM, Schlötzer-Schrehardt U, Küchle M, Naumann GO.Pseudoexfoliation syndrome: pathological manifestations of relevance to intraocular surgery. Clin Exp Ophthalmol 2004;32(2):199-210.
7 Küchle M, Nguyen NX, Hannappel E, Naumann GO. The bloodaqueous barrier in eyes with pseodoexfoliation syndrome. Ophthalmic Res 1995;27(Suppl 1):136-142.
8 Imamoglu S, Sevim MS, Alpogan O, Ercalik NY, Kumral ET, Pekel G,Bardak H. In vivo biometric evaluation of Schlemm's canal with spectraldomain optical coherence tomography in pseuduexfoliation glaucoma.Acta Ophthalmol 2016;94(8):e688-e692.
9 Ehrnrooth P, Lehto I, Puska P, Laatikainen L. Long-term outcome of trabeculectomy in terms of intraocular pressure. Acta Ophthalmol Scand 2002;80(3):267-271.
10 Serguhn S, Spiegel D. Efficacy of trabeculectomy for pseudoexfoliation glaucoma and primary open angle glaucoma. Klin Monatsb Augenheilkd 1999;215(11):281-286.
11 Törnqvist G, Drolsum LK. Trabeculectomies. A long-term study. Acta Ophthalmol (Copenh) 1991;69(4):450-454.
12 Shaarawy TM, Sherwood MB, GrehnF. Guidelines on Design and Reporting of Glaucoma Surgical Trials. World Glaucoma Association.Amsterdam: Kugler Publications; 2009.
13 European Glaucoma Society. Terminology and guidelines for glaucoma, 2008. Available at: www.eugs.org/eng/EGS_guidelines.asp.Accessed on June 8, 2014.
14 Meyer LM, Graf NE, Philipp S, Fischer MT, Haller K, Distelmaier P, Schönfeld CL. Two-year outcome of repeat trabeculectomy with mitomycin C in primary open-angle and PEX glaucoma. Eur J Ophthalmol 2015;25(3):185-191.
15 Mietz H, Raschka B, Krieglstein GK. Risk factors for failures of trabeculectomies performed without antimetabolites. Br J Ophthalmol 1999;83(7):814-821.
16 Fernández S, Pardiñas N, Laliena JL, Pablo L, Díaz S, Pérez S,Honrubia FM. Long-term tensional results after trabeculectomy. A comparative study among types of glaucoma and previous medical treatment. Arch Soc Esp Oftalmol 2009;84(7):345-351.
17 Shigeeda T, Tomidokoro A, Chen YN, Shirato S, Araie M. Long-term follow-up of initial trabeculectomy with mitomycin C for primary openangle glaucoma in Japanese patients. J Glaucoma 2006;15(3):195-199.
18 Landers J, Martin K, Sarkies N, Bourne R, Watson P. A twentyyear follow-up study of trabeculectomy: risk factors and outcomes.Ophthalmology 2012;119(4):694-702.
19 Zaidi AA. Trabeculectomy: a review and 4-year follow-up. Br J Ophthalmol 1980;64(6):436-439.
20 Mills KB. Trabeculectomy: a retrospective long-term follow-up of 444 cases. Br J Ophthalmol 1981;65(11):790-795.
21 Kim S, Sung KR, Lee JR, Lee KS. Evaluation of lamina cribrosa in pseudoexfoliation syndrome using spectral-domain optical coherence tomography enhanced depth imaging. Ophthalmology 2013;120(9);1798-1803.
22 Ting JL, Damji KF, Stiles MC; Trabectome Study Group. Ab interno trabeculectomy: outcomes in exfoliation versus primary open-angle glaucoma. J Cataract Refract Surg 2012;38(2):315-323.
23 Jordan JF, Wecker T, van Oterendorp C, Anton A, Reinhard T,Boehringer D, Neuburger M. Trabectome surgery for primary and secondary open angle glaucomas. Graefes Arch Clin Exp Ophthalmol 2013;251(12):2753-2760.
24 Öztürker ZK, Öztürker C, Bayraktar S, Altan C, Yılmaz OF. Does the use of preoperative antiglaucoma medications influence trabeculectomy success? J Ocul Pharmacol Ther 2014;30(7):554-558.