INTRODUCTION
Silicone oil was first used as an intraocular tamponade in humans by Cibis et al[1]in 1962 in retinal detachments with proliferative vitreoretinopathy (PVR). Silicone oils are hydrophobic compounds constituted of silicone and oxygen bonds. Silicone oils are chemically inert which is advantageous for intraocular use as they can remain in situ for an extended period of time.
Silicone oil tamponade is intended to be temporary as prolonged intraocular duration may lead to ocular complications, such as oil emulsification, band keratopathy, elevated intraocular pressure and cataract formation[2]. They are also potentially retinotoxic with reported cases of permanent central vision loss following removal of silicone oil (ROSO)[3]. In certain patients ROSO may not be appropriate due to patient preference,fitness for surgery or eyes with a high risk of redetachment or no visual potential.
The main indications for silicone oil tamponade are retinal detachment (RD) complicated by PVR, giant retinal tears(GRT), traumatic RD and certain cases of proliferative diabetic retinopathy (PDR) with combined tractional rhegmatogenous retinal detachment (TRRD).
PVR, the most common indication for oil tamponade, is a disease that complicates rhegmatogenous retinal detachment(RRD). The critical factor in developing PVR is the presence of a full thickness retinal break. PVR involves the migration of retinal pigment epithelial (RPE) and glial cells through a retinal break and proliferation on the retinal surface. They form a contractile fibrocellular membrane on the surface of the retina and beneath it leading to fibrosis, traction and subsequent RD[4]. PVR can occur in longstanding primary RD (primary PVR) but the majority of cases occur with redetachment after initial RD repair. Risk factors for PVR include uveitis, vitreous haemorrhage, giant or multiple retinal tears, aphakia, pre-or post-operative choroidal detachments, large detachment involving greater than two retinal quadrants[4-5]. PVR complicates 5%-10% of RD surgery and is the most common cause of surgical failure in RRD[4]. Classification of PVR is currently based on the updated Retina Society Guidelines 1991[6].
The primary objective of this study was to report anatomic and visual outcome following silicone oil removal at varying duration of tamponade in a cohort of patients with complex RD requiring silicone oil. Secondary objectives were to compare patients with oil removed and those with oil in situ in terms of associated factors.
SUBJECTS AND METHODS
All procedures performed in this study were in accordance with the guidelines set out by the Irish Council for Bioethics on audit studies section 2.2 and with the principles outlined in the 2008 Declaration of Helsinki.
All retinal detachments that underwent silicone oil tamponade over a four years period were retrospectively examined. This case series included 143 eyes of 143 patients who underwent pars plana vitrectomy (PPV) with intraocular silicone oil injection from January 2012 to December 2015 at a Tertiary Ophthalmology Referral Centre. All surgeries were carried out by two vitreoretinal surgeons. Data was gathered on patient demographics, baseline vision, indications for and duration of oil tamponade, number of surgeries required, final anatomic and functional status. Best corrected visual acuity(BCVA) was measured by Snellen visual acuity at each clinic visit. Inclusion criteria were patients who underwent silicone oil tamponade for each of the following clinical scenarios:1) retinal detachment with PVR; 2) GRT associated RD; 3)traumatic retinal detachment; 4) other, as specified. Exclusion criteria were patients with tractional retinal detachment (TRD)as a consequence of PDR. The primary outcome measures were anatomic success and visual outcome following silicone oil removal. Anatomic success was defined as complete retinal attachment following oil removal at 6mo or at patients most recent follow up visit. Significant improvement or deterioration in BCVA was based on ≥0.3 logMAR unit change in BCVA[7].Ambulatory visual acuity (VA) was defined as 1.7 logMAR unit or better[8]. Secondary outcome measures were retinal status in patients with oil in situ.
Statistical Analysis Data was collected using Microsoft®Excel for Mac Version 15.22 and statistical analysis was carried using Prism 7©for Mac. Snellen acuity was converted to logMAR units for analysis[9]. A BCVA of count fingers(CF), hand motions (HM), perception of light (PL), and no perception of light (NPL) were assigned 2.1, 2.4, 2.7 and 3.0 respectively, in keeping with those values used by the United Kingdom National Ophthalmology Database study of vitreoretinal surgery[10]. Univariate analysis to determine association with an attached retina following oil removal and improved or stable vision was carried out using Fisher’s exact test and unpaired two tailed t-test. A P value of <0.05 was considered statistically significant for all tests.

Figure 1 Breakdown of overlapping indication for silicone oil tamponade.
RESULTS
Patient Demographics Of 143 patients, 52 patients (36.4%)were female and 91 patients (63.6%) were male. The median age of the cohort was 58y (range 12-91 years old; Table 1).The indication for silicone oil tamponade was: 1) retinal detachment with PVR [n=90 patients (62.9%)]; 2) GRT or multiple retinal tear associated RD [n=19 patients (14%)]; 3)traumatic retinal detachment [n=21 patients (14.7%)]; 4) other 18 patients (12.6%), as specified (Figure 1).
The specific oil tamponade used was identified in 111 cases,77 (69.4%) had 1000-CentiStoke (CS) (company and city),16 (14.4%) 5000-CS silicone oil (Company and city) and 18 (16.21%) had heavy silicone oil (Densiron-68®, Fluoron,Ulm, Germany).
Eighty-two patients (91.1%) had grade C PVR, 2 patients had grade B (2.2%), 6 patients had grade A or early PVR (6.7%).At the time of this review, 106 out of 143 patients (76.2%)had undergone silicone oil removal, 21 remained under oil tamponade,14 patients (9.8%) underwent oil exchange for redetachment under oil and 2 patients (4.9%) have insufficient follow up data. The duration of intraocular oil tamponade ranged from 1.5 to 30mo with a mean of 7.2mo. The criteria for silicone oil removal were a complete and stable attached retina with no active proliferation. The number of vitreoretinal surgeries ranged from 1 to 5 with a mean of 2.3 surgeries.There are 3 patients who remain under oil tamponade awaiting removal of silicone oil at the time of review and 3 patients with insufficient data.
Primary Outcome Measures
Anatomic outcomes Anatomic success after silicone oil removal, defined as a complete and stable attached retina for a minimum of 6mo was achieved in 96 out of 106 patients(90.6%). Retinal redetachment occurred in 10 patients following ROSO (9.4%) including 4 patients with traumatic retinal detachment and 6 patients with PVR. All 10 patients were reoperated on with replacement of silicone oil tamponade and all remain attached with oil in situ at time of review. The mean duration of intraocular oil tamponade in the attached group was 7.4mo and in the redetached group was 4.8mo.There was no statistically significant difference between the attached and the redetached group in relation to duration of intraocular tamponade using an unpaired two tailed t-test[P=0.19, 95% confidence interval (CI) -1.2729 to 6.4729]. The mean number of surgeries in the attached group was lower(2.316±0.05214), and in the redetached group was 3.0921±0.2981 which was statistically significant (P=0.004, 95% CI 0.3137 to 1.055). At the time of this review 44 out of 143 (30.8%)patients remained under oil tamponade, including 13 (9.1%)patients who underwent oil exchange for redetachment under oil and 9 patients (6.3%) who redetached following silicone oil removal. The duration of remaining under oil tamponade ranges from 11 to 71mo in the oil in situ group. Out of the 44 patients, 31 had an attached retina under oil, 8 had a detachedretina, 3 out of 8 of which were stable peripheral detachments,5 out of 8 had macular detachment, which was defined as a final anatomic failure and 5 patients were lost to follow up. Comparing the three tamponade agents, no significant difference in anatomic outcome, oil removed versus in situ at final follow up was found (P=0.402).
Table 1 Baseline demographics, surgical procedures anatomic and visual outcomes
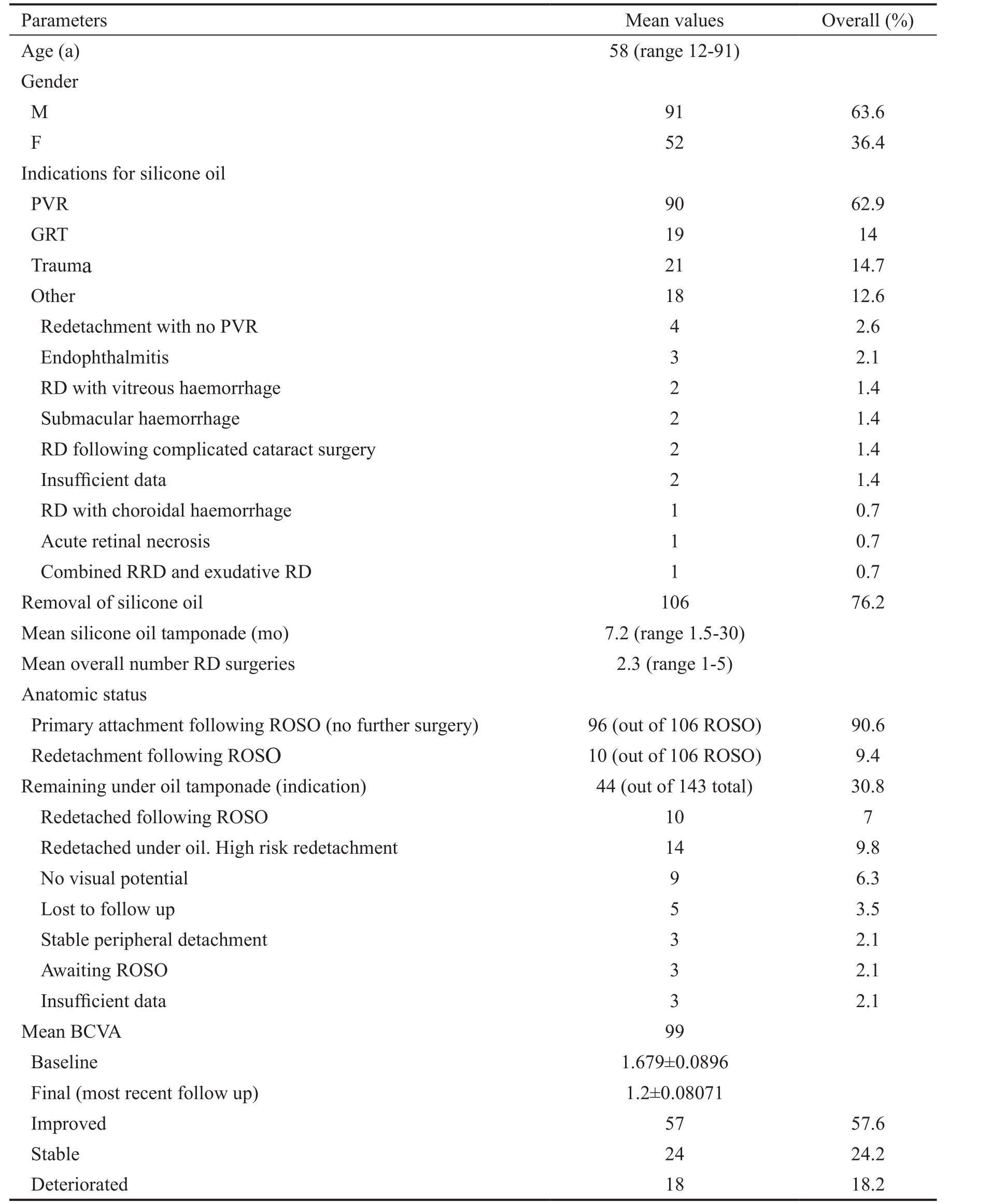
Table 2 Analysis of visual outcomes
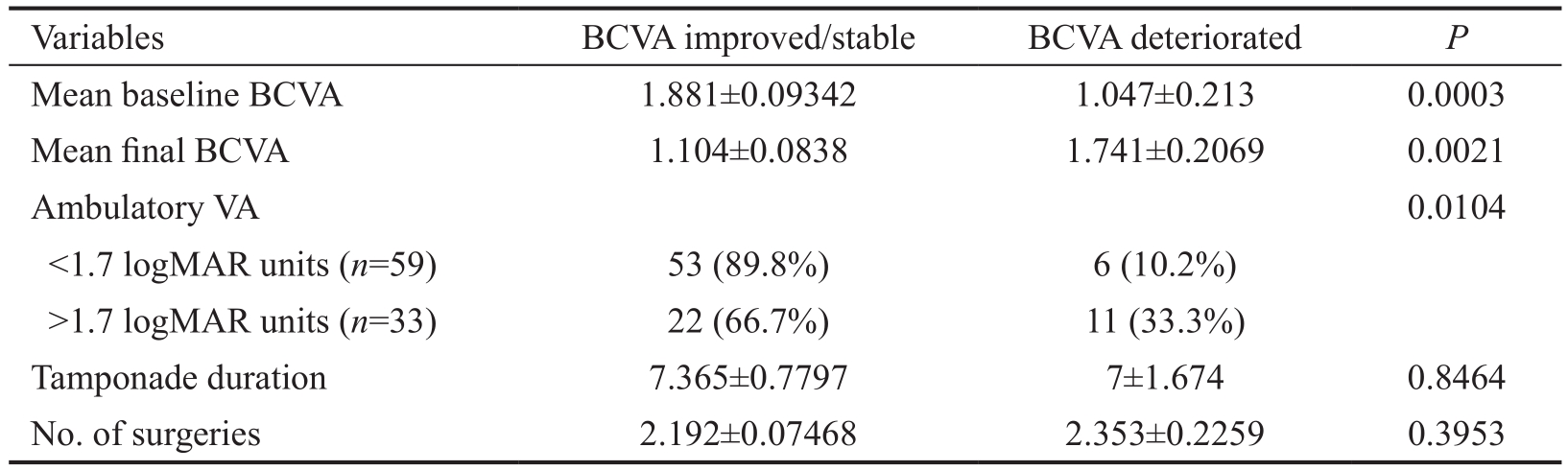
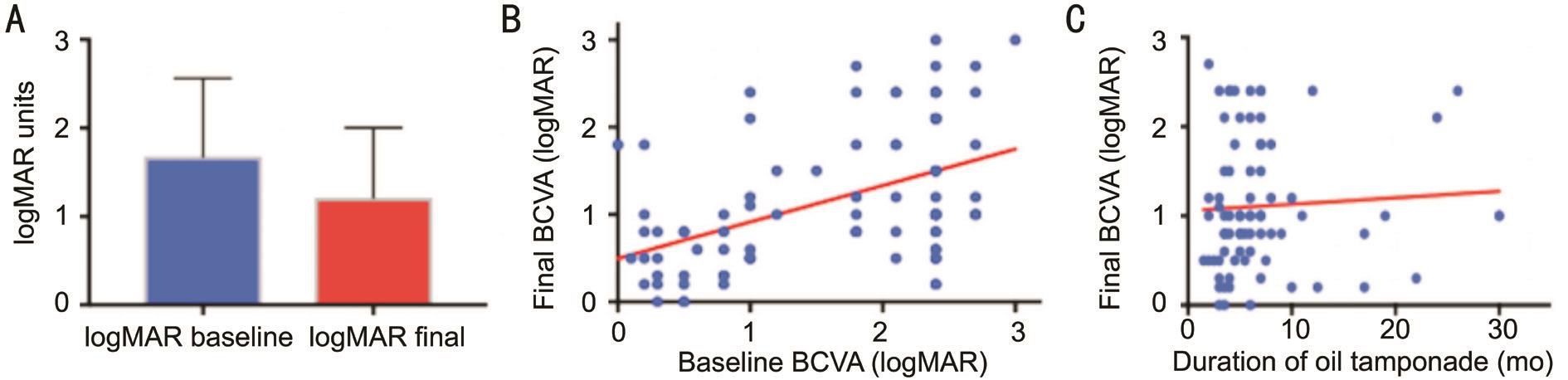
Figure 2 Overall visual outcomes in logMAR units based on BCVA at most recent follow up visit A: Mean baseline (1.679±0.0896 logMAR) versus final BCVA (1.214±0.08071 logMAR) (P=0.0002, 95% CI 0.7038 to -0.2278); B: A positive correlation was found between baseline BCVA and final BCVA, patients with better baseline BCVA had better final BCVA (r2=0.2201, P=0.0001); C: No significant correlation was found between duration of oil tamponade and final BCVA (r2=0.0036, P=0.5990).
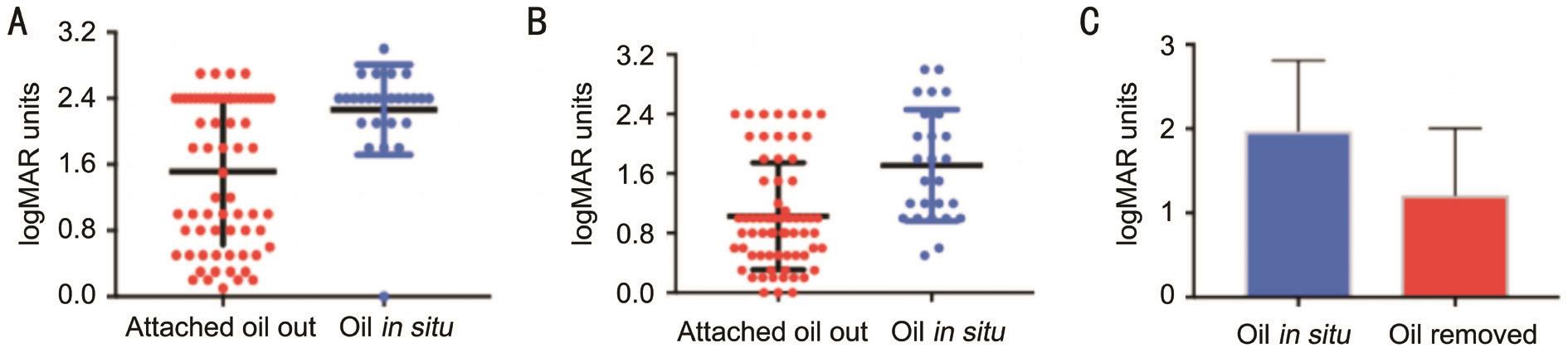
Figure 3 Visual outcomes based on oil tamponade status: oil removed versus oil remaining in situ A: The mean baseline BCVA was significantly better in the oil out group compared to oil in situ group (P=0.0001 unpaired two tailed t-test); B: The mean final BCVA was significantly better in the oil out group compared to oil in situ group (P≤0.0001 unpaired two tailed t-test); C: Mean BCVA of patients with oil in situ versus those with oil removed.
Visual outcomes Complete visual data was recorded in 99 patients. Comparing preoperative BCVA to BCVA at most recent follow up 57 out of 99 patients (57.6%)showed an improvement, 24 (24.2%) remained stable and 18 (18.1%) patients showed a deterioration in BCVA based on a 0.3 logMAR change as significant. The mean duration of oil tamponade in the improved and stable vision group combined was 7.365±0.7797mo, and in the deteriorated group was 7±1.674mo which was not statistically significant(P=0.8464). A statistically significant difference was found between overall baseline BCVA (1.679±0.0896 logMAR)and final BCVA (1.214±0.08071 logMAR) irrespective of oil status (P=0.0002, 95% CI 0.7038 to -0.2278; Figure 2A).Final BCVA was also significantly better in patients following oil removal (1.104±0.0838) compared to those under oil tamponade (1.741±0.2069; P=0.0021), both using an unpaired two tailed t-test (Table 2). Linear regression analysis showed a correlation between baseline BCVA and postoperative BCVA(r2=0.2201, P=0.0001; Figure 2B). No correlation was found between duration of oil tamponade and final BCVA (r2=0.0036,P=0.5990; Figure 2C).
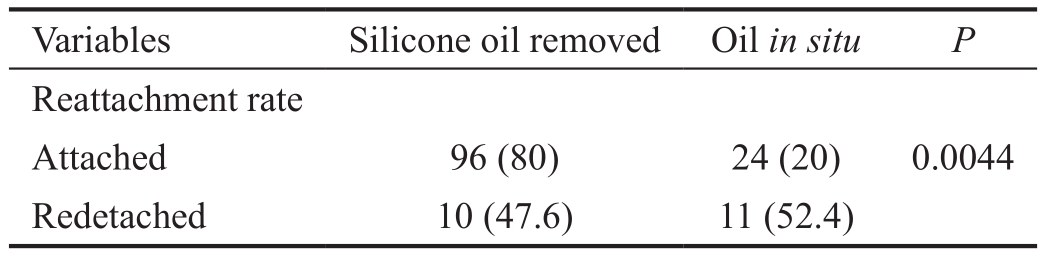
Secondary Outcome Measures Results of analysis between patients with oil removed and oil in situ are summarised in Table 3. The mean baseline and final BCVA was significantly better in those with oil removed (P=0.0001 and <0.0001,respectively; Figure 3). Tamponade duration, the number of surgeries and presence of PVR in this series were not statistically significant. The final attachment rate is significantly higher(80%) of those with oil removed compared to those under tamponade (20%) (P=0.0044) as summarised in Table 4. Those with oil in situ include patients who underwent ROSO and redetached.
Table 3 Analysis of anatomic outcomes n=141 with sufficient data

Table 4 Attachment rate following silicone oil removal n (%)
DISCUSSION
Silicone oil tamponade is the method of choice for management of high risk/complex retinal detachment complicated by PVR,due to a giant retinal tear, post trauma ± intraocular foreign body (IOFB) and combined TRD/RRD in diabetic retinopathy.Despite surgical advances, redetachment following removal of oil is still common and the prospect of a deterioration in vision post oil removal is now well described. We sought to determine the risk of redetachment and long term VA based on duration of tamponade by assessing the practice, patient profile and outcomes at an Irish Tertiary Retinal Centre.
This study presents the results of 143 patients diagnosed with complex retinal detachments treated with intraocular silicone oil tamponade. In terms of anatomic outcome the retinal redetachment rate following silicone oil removal of 9.4% in this series, corresponds favourably with redetachment rates reported in the literature of 6% to 34%[11-23]. A large case series by Teke et al[24]reported 897 eye showed a redetachment rate of 12.2% in 2014, and an Irish series in 2007 reported final redetachment rate of 13.9%[25]. In this series mean number of surgeries was higher in the redetached group but number of surgeries was not associated with final attachment status(P=0.2015, Fisher’s exact test). The optimal timing for silicone oil removal remains unclear on literature review.Recommendations range from 3 to 6mo of sustained retinal attachment[26-27]. In this series, the duration of oil tamponade had no significant effect on anatomic outcomes which corresponds with other reported studies[19-20,28]. Others reported a higher redetachment rate with shorter duration of tamponade,such as Lam et al[21], in which tamponade of less than 2mo was associated with higher risk of redetachment. This is a shorter duration compared to our series in which, 96.5% had tamponade of >2mo duration.
In terms of visual outcomes, in this series an improvement or stability in BCVA at final up compared to baseline was seen in 80.8% of patients. This corresponds favourably with others reported were 38.9%[29], 64.2%[28]and 84%[30]. A better baseline BCVA correlated positively to a better final BCVA using linear regression (r2=0.2201, P=0.0001).
Comparing the oil removed to oil in situ cohort both baseline and final BCVA was significantly better in the oil removed cohort. The refractive error induced by oil may be a factor in final BCVA and as we have shown above a better baseline BCVA correlates to better final vision. Also the redetachment rate was significantly lower in the oil out cohort. These results correlate with another Irish study comparing patients with oil removed versus oil in situ[30].
The main limitation of this study is its retrospective and noncomparative design and patient’s records were not standardised.In this study, we report on 143 patients who underwent silicone oil tamponade for complex retinal detachments. Our outcomes are in keeping with those reported in the literature. Favourable visual outcomes were seen with oil removal. Duration of oil tamponade did not correlate with anatomic success or visual outcome. To conclude, based on these findings, the optimal timing of silicone oil removal should be managed on a case by case basis guided by individualised risks, patient preference and surgeon preference.
ACKNOWLEDGEMENTS
Conflicts of Interest: Rhatigan M, None; McElnea E, None;Murtagh P, None; Stephenson K, None; Harris E, None;Connell P, None; Keegan D, None.
REFERENCES
1 Cibis PA, Becker B, Okun E, Cannan S. The use of liquid silicone in retinal detachment surgery. Arch Ophthalmol 1962;68:590-599.
2 Federman JL, Schubert HD. Complications associated with the use of silicone oil in 150 eyes after retina-vitreous surgery. Ophthalmology 1988;95(7):870-876.
3 Tode J, Purtskhvanidze K, Oppermann T, Hillenkamp J, Treumer F,Roider J. Vision loss under silicone oil tamponade. Graefes Arch Clin Exp Ophthalmol 2016;254(8):1465-1471.
4 Chaudhary R, Dretzke J, Scott R, Logan A, Blanch R. Clinical and surgical risk factors in the development of proliferative vitreoretinopathy following retinal detachment surgery: a systematic review protocol. Syst Rev 2016;5(1):107.
5 Pastor JC. Proliferative vitreoretinopathy: an overview. Surv Ophthalmol 1998;43(1):3-18.
6 Di Lauro S, Kadhim M, Charteris D, Pastor J. Classifications for proliferative vitreoretinopathy (PVR): an analysis of their use in publications over the last 15 years. J Ophthalmol 2016;2016:7807596.
7 Sparrow JM, Taylor H, Qurehi K, Smith R, Birnie K, Johnson RL; UK EPR user group. The Cataract National Dataset electronic multi centre audit of 55567 operations: risk indicators for monocular visual acuity outcomes. Eye (Lond) 2012;26(6):821-826.
8 Lucke K. Silicone oil in the surgery of complicated retinal detachment.Ophthalmologe 1990;90(3):215-238
9 Holladay JT. Proper method for calculating average visual acuity. J Refract surg 1997;13(4):388-391.
10 Jackson TL, Donachie PH, Sparrow JM, Johnston RL. United Kingdom National Ophthalmology Database study of vitreoretinal surgery: report 2, macular hole. Ophthalmology 2013;120(3):629-634.
11 Elsar AM, Albish SM, Cangave D. Outcome of temporary silicone oil tamponade in complex rhegmatogenous retinal detachment repair. Eur J Ophthalmol 2003;13(5):474-481.
12 Bassat IB, Desatnik H, Alhalel A, Treister G, Moisseiev J. Reduced rate of retinal detachment following silicone oil removal. Retina 2000;20(6):597-603.
13 Flaxel CJ, Mitchell SM, Aylward GW. Visual outcome after silicone oil removal and recurrent retinal detachment repair. Eye (Lond) 2000;14(Pt 6):834-838.
14 Assi I, Woodruff S, Gotzaridis E, Bunce C, Sullivan P. Combined phacoemulsification and transpupillary drainage of silicone oil: results and complications. Br J Ophthalmol 2001;85(8):942-945.
15 Jonas JB, Knorr HL, Rank RM, Budde WM. Retinal redetachment after removal of intraocular silicone oil tamponade. Br J Ophthalmol 2001;85(10):1203-1207.
16 Falkner CI, Binder S, Kruger A. Outcome after silicone oil removal. Br J Ophthalmol 2001;85(11):1324-1327.
17 Unlu N, Kocaoglan H, Acar MA, Sargin M, Aslan BS, Duman S.Outcome of complex retinal detachment surgery after silicone oil removal.Int Ophthalmol 2004;25(1):33-36.
18 Jiang F, Krause M, Ruprecht KW, Hille K. Management and results of retinal detachment after silicone oil removal. Acta Ophthalmol 2002;216(5):341-345.
19 Jain N, McCuen BW 2nd, Mruthyunjaya P. Unanticipated vision loss after pars plana vitrectomy. Surv Ophthalmol 2012;57(2):91-104.
20 Nagpal MP, Videkar RP, Nagpal KM. Factors having implications on re-retinal detachments after silicone oil removal. Indian J Ophthalmol 2012;60(6):517-520.
21 Lam RF, Cheung BTO, Yuen CYF, Wong D, Lam DSC, Lai WW. Retinal redetachment after silicone oil removal in proliferative vitreoretinopathy: a prognostic factor analysis. Am J Ophthalmol 2008;145(3):527-533.
22 Scott IU, Flynn Jr HW, Murray TG, Smiddy WE, Davis JL, Feuer WJ.Outcomes of complex retinal detachment repair using 1000- vs 5000-centistoke silicone oil. Arch Ophthalmol 2005;123(4):473-478.
23 Soheilian M, Mazareei M, Mohammadpour M, Rahmani B.Comparison of silicone oil removal with various viscosities after complex retinal detachment surgery. BMC Ophthalmol 2006;6:21.
24 Teke MY, Balikoglu-Yilmaz M, Yuksekkaya P, Citirik M, Elgin U, Kose T, Ozturk F. Surgical outcomes and incidence of retinal redetachment in cases with complicated retinal detachment after silicone oil removal: univariate and multiple risk factors analysis. Retina 2014;34(10):1926-1938.
25 James M, O’Doherty M, Beatty S. The prognostic influence of chronicity of rehagmatogenous retinal detachment on success after redetachment surgery. Am J Ophthalmol 2007;143(6):1032-1034.
26 Casswell AJ, Gregor ZJ. Silicone oil removal. II. Operative and postoperative complications. Br J Ophthalmol 1987;71(12):898-890.
27 Zilis JD, McCuen BW, de Juan E Jr, Stefansson E, Machemer R.Results of silicone oil removal in advanced proliferative vitreoretinopathy.Am J Ophthalmol 1989;108(1):15-21
28 Tavares RLP, Nobrega MJ, Nobrega FAJ, De Novelli FJ, De Oliviera CC. Timing and outcomes after silicone oil removal: a retrospective clinical series. Int J Retina Vitreous 2015;1:2.
29 Wong R, Luca M, Shumugam M, Williamson T, Laidlaw A, Vaccaro V. Visual outcomes after removal of silicone oil in patients undergoing retinectomy for complex retinal detachment. Int J Ophthalmol 2016;9(1):108-110.
30 Dooley IJ, Duignan ES, Kilmartin DJ. Long term heavy intraocular silicone oil tamponade. Int Ophthalmol 2015;36(1):3-7.