INTRODUCTION
Retinopathy of prematurity (ROP) is a leading cause of childhood blindness worldwide and is characterized by neovascularization. The overexpression of vascular endothelial growth factor (VEGF) as a response to relative hypoxia in the avascular retina plays an important role in pathogenesis of ROP. Therefore, intravitreal injection of anti-VEGF agents such as bevacizumab has become a potential treatment of ROP.In recent studies, intravitreal bevacizumab (IVB) injection showed more favorable results than conventional laser photocoagulation in zone I ROP, with subsequent growth of normal retinal vessels onto the avascular area[1]. Additionally, recent studies reported that IVB monotherapy led to less myopia and astigmatism than conventional laser photocoagulation[2].However, there are still concerns about IVB monotherapy that the late reactivation rate is higher, and extended follow up is needed because of incomplete retinal vascularization[3].Therefore, anti-VEGF agents combined with conventional laser photocoagulation can be a better option for treatment of type I ROP. Several studies showed promising results with rapid regression of ROP and better anatomical outcome in zone I or II ROP[4-5].
However, there is no consensus on optimal dosage of anti-VEGF agents, whether used alone or combined with laser for treatment of ROP, and the long term systemic and neurodevelopmental effects after anti-VEGF treatment in premature babies were unknown.
Therefore, we compared the efficacy and safety of two different IVB doses combined with temporal retina-sparing laser photocoagulation in stage 3+ ROP
METHODS
The study followed the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of the Dongsan Medical Center (IRB file No.DSMC 2015-08-011). We retrospectively reviewed and analyzed the medical records of the 22 eyes of 11 consecutive infants with ROP stage 3+, zone I or posterior zone II who were born between April 2012 and May 2013 and admitted to the Neonatal Intensive Care Unit in the Keimyung University Dongsan Medical Center. All infants of gestational age <32wk or birth weight <1800 g underwent ROP screening examination within 4-6wk after birth. Fundus examination with binocular indirect ophthalmoscopy (Vantage plus wireless, Keeler Ltd., Windsor,UK) was performed after pupil dilatation.
Table 1 Clinical characteristics
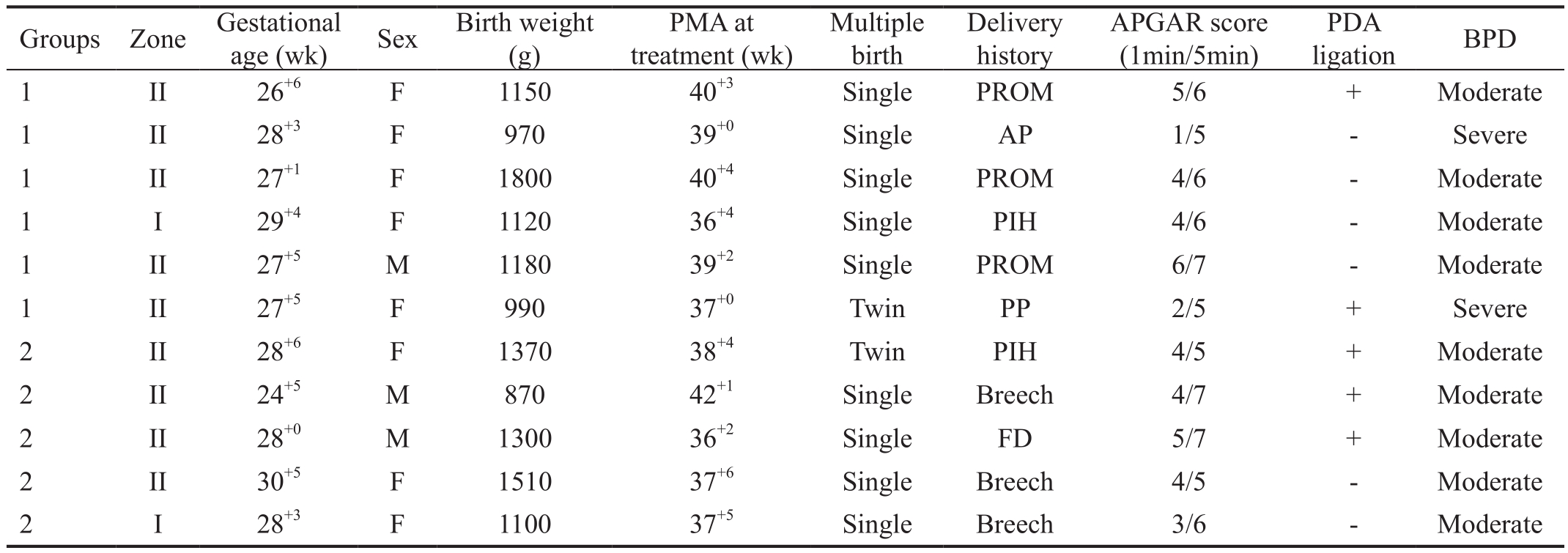
PMA: Postmenstrual age; PDA: Patent ductus arteriosus; BPD: Bronchopulmonary dysplasia; PIH: Pregnancy induced hypertension; PROM:Premature rupture of membranes; PP: Placenta previa; FD: Fetal distress; AP: Abruption of placenta.
Severity of ROP (stage, localization, plus signs) was identified according to international classification of ROP[6]. Stage 3 is defined as a ridge with neovascularization extending into the vitreous gel, and plus sign indicates that two or more quadrants of retina have dilated veins and tortuous arteries near the optic disc. The treatment criteria were based on the Early Treatment for Retinopathy of Prematurity study[7]. All procedures were performed under general anesthesia by a single operator. Nearconfluent laser photocoagulation using a 532 nm laser indirect ophthalmoscope (Zeiss Visulas Argon Laser®, Carl Zeiss Meditec AG, Jena, Germany) was applied to the avascular area anterior to the ridge, sparing the two-disc-diameter width avascular area adjacent to the ridge from superior to inferior temporal arcade (Figure 1). After disinfection with 5% povidone/iodine solution, a dose of 0.625 mg in 0.025 mL(half dose, group 1) or 0.25 mg in 0.01 mL (minimal dose,group 2) of IVB (Avastin®, Genentech Inc., San Francisco, CA,USA) was injected 1 to 1.5 mm posterior to the limbus using a 30-gauge needle after laser treatment. After the procedure,antibiotic eye solution (Cravit®, Santen, Osaka, Japan) was administered 4 times a day for 5d[1].
After the treatment, fundus examinations were performed daily for the first week, twice a week in the second week, twice a month for the next 3mo, and then monthly until complete vascularization of the spared avascular area. The follow-up examinations were performed at least 12mo.
The fundus findings, gestational age, birth weight, delivery history, general conditions including Apgar score, and presence of patent ductus arteriosus (PDA) or bronchopulmonary dysplasia (BPD) were evaluated and analyzed. Complete regression was defined as the disappearance of plus sign and extra-retinal fibrovascular proliferation (EFP). If plus sign or EFP returned, retreatment with additional IVB (0.25 mg in 0.01 mL) and laser photocoagulation was done at the clinician’s discretion.

Figure 1 Diagram of temporal retinal sparing using indirect laser photocoagulation Dark-gray colored area: Two-disc-diameter (2DD)width spared retinal avascular area; Gray circles: Laser-treated areas.
RESULTS AND DISCUSSION
A total of 22 eyes of 11 infants treated with combined temporal retina-sparing laser photocoagulation and IVB for stage 3+zone I or posterior zone II ROP were analyzed in this study(Table 1). The mean follow-up period was 21.09±6.60mo(range 12-31mo). The mean gestational age at birth was 27.7±0.99wk (range 26+6-29+4wk) in group 1 and 27.9±2.18wk(range 24+5-30+5wk) in group 2. The mean birth weight was 1201.7±305.38 g (range 970-1800 g) and 1232.0±248.43 g(range 870-1510 g), respectively. The mean postmenstrual age (PMA) at treatment was 38.7±1.67wk (range 36+4-40+4wk) and 38.4±2.23wk (range 36+2-42+1wk), respectively.There was no significant difference between the groups. Two infants were twins. The causes of prematurity were pregnancy induced hypertension, premature rupture of membranes,placenta previa, fetal distress, placental abruption, and breech presentation (Table 1).
There was no ocular complication except vitreous hemorrhage and retinal dragging and no systemic complication during follow-up. The plus sign and EFP regressed within a week in 18 of 22 eyes. However, 4 eyes of 2 infants in group 2 showed incomplete regression of plus sign and progression of EFP even after the primary intervention. Preretinal hemorrhage around the ridge developed in 3 of these 4 eyes. A second injection of IVB and additional laser photocoagulation were performed at 63 and 74d after primary treatment in each case. After retreatment, the plus sign regressed and preretinal hemorrhage was absorbed, but the tractional fibrous membrane resulted in retinal dragging at the final follow-up in 3 eyes.One infant in group 2 showed complete regression after treatment, but did not return to the hospital starting 2mo after treatment; when the infant brought back 26mo after treatment,macular dragging and a premacular membrane were observed in the right eye.
The mainstay of current treatment strategies for ROP is laser photocoagulation of avascularized retina. However,the limitations of conventional laser therapy include the irreversible and extensive destruction of peripheral retina,concomitant reduction in visual fields. Therefore, targeted pharmacologic inhibition of VEGF is an emerging treatment for acute phase ROP. Bevacizumab is most commonly used off-label agent that binds to all isoforms of VEGF, blocks VEGF-induced angiogenesis. The Bevacizumab Eliminates the Angiogenic Threat of Retinopathy of Prematurity (BEATROP) study[1]has shown that bevacizumab for zone I ROP results in a better anatomical outcome than laser treatment.However, there are still concerns of safety and efficacy of IVB as the studies of the long-term ocular and systemic effects of bevacizumab are lacking. In this study, we compared the safety and efficacy of two different doses; half dose (0.625 mg/0.025 mL)or minimal dose (0.25 mg/0.01 mL) of IVB combined with temporal retina-sparing laser photocoagulation.
This study has two distinctive features compared with previous reports.
First, we performed near-confluent laser photocoagulation on the avascular retina, sparing a two-disc-diameter width avascular area adjacent to the vascularized retinal margin or ridge, from superior to inferior temporal arcade. Conventional laser photocoagulation for zone I or posterior zone II ROP with subsequent expansion of laser scars may constrict the visual field. Kim et al[4]previously reported excellent anatomical outcomes without recurrence or adverse events after zone I-sparing laser photocoagulation combined with IVB (0.25 mg/0.01 mL), but sparing the temporal avascular retina with a twodisc-diameter width is presumed to keep the radial distance of spared area constant and preserves more of the central visual field than sparing zone 1.
Second, we compared the effects of a minimal and a half dose of IVB combined with temporal retina-sparing laser photocoagulation. Sato et al[8]reported that even a total of 0.50 mg of IVB can significantly reduce the serum VEGF level. To minimize the risk of systemic effects, there have been ongoing efforts to prove the efficacy of a minimal dose of IVB.Harder et al[9]reported that IVB injection of only 0.375 mg was sufficiently effective for treating threshold ROP. Spandau et al[10]suggested that the size-adjusted dosage in a neonate should be 0.4 mg, and showed a favorable anatomical outcome after treatment. Successful resolution of ROP has been reported with doses of IVB ranging from 0.16 to 1.25 mg[1,10-11]. In our study,whereas no additional treatment was required in the half dose group (0.625 mg/0.025 mL), 4 eyes in the minimal dose group(0.25 mg/0.01 mL) required additional laser photocoagulation and re-injection of bevacizumab after the first treatment. This surmises that when combined with laser photocoagulation,a minimal dose of IVB of 0.25 mg might be insufficient for the treatment of some ROP cases as there may be a potential risk of damage to the blood retinal barrier from laser photocoagulation[12]. Compared to IVB monotherapy, IVB combined with laser photocoagulation could result in more leakage of anti-VEGF agents into the systemic circulation,which increase systemic effects and reduce local therapeutic levels of anti-VEGF agents[5]. It is also possible that the inflammation induced by the laser treatment reduces anti-VEGF effects and expedites neovascularization and fibrosis[2].However, no difference in systemic complications between the groups was identified. This is thought that a relatively high anti-VEGF level in the systemic circulation does not easily lead to clinically-identified systemic complications.
In our study, preretinal hemorrhage around the ridge was found after the first treatment in 3 eyes of group 2 that developed a tractional fibrovascular membrane with macular dragging seen at the last follow-up. Sanghi et al[13]reported that preretinal hemorrhage before laser treatment is one of the most significant risk factors for retinal detachment in aggressive posterior ROP. Preretinal hemorrhage is likely to contribute to abnormal vitreous organization, resulting in tractional force on the retina, which is often associated with retinal detachment[14].Therefore, preretinal hemorrhage on the ridge after the treatment might be a sign of worsening ROP.
Laser treatment has been reported to have the potential of inducing postoperative intraocular hemorrhage[15]. Combination with IVB could reduce the risk of hemorrhage. Minimal dose IVB might be insufficient to prevent postoperative preretinal hemorrhage in eyes with incompletely involuted EFP.
One infant’s right eye in group 2 showed macular dragging and a premacular membrane 26mo after complete regression.
The re-exacerbation is assumed not to be associated with IVB dosing but to be caused by reactivation of neovascularization after the effect of IVB ends. The BEAT-ROP study[1]reported a case that recurred 7mo after bevacizumab monotherapy. Thus,close follow-up until normal retinal vessel growth is observed on all spared retina is recommended.
There are several limitations in this study, including retrospective design, selection bias, small sample size, and a relatively short follow-up period to evaluate the long-term safety of bevacizumab and check the visual field defect and refractive change. Further prospective studies that comparing IVB combined with laser photocoagulation and IVB monotherapy with different doses are nessasary.
In conclusion, a half dose of IVB with partial temporal retinasparing laser photocoagulation may be effective for the treatment of ROP, while a minimal dose (0.25 mg/0.01 mL) of IVB with partial retina-sparing laser photocoagulation might be insufficient for the treatment of stage 3+ ROP. Preretinal hemorrhage after treatment might be a sign of worsening ROP.
ACKNOWLEDGEMENTS
Foundations: Supported by the National Research Foundation of Korea (NRF) Grant Funded by the Korean Government(MSIP; No.2014R1A5A2010008); the Research Promoting Grant from the Keimyung University Donsan Medical Center in 2011.
Conflicts of Interest: Choi AY, None; Cho H, None; Kim YC, None.
REFERENCES
1 Mintz-Hittner HA, Kennedy KA, Chuang AZ. Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med 2011;364(7):603-615.
2 Harder BC, Schlichtenbrede FC, von Baltz S, Jendritza W, Jendritza B, Jonas JB. Intravitreal bevacizumab for retinopathy of prematurity:refractive error results. Am J Ophthalmol 2013;155(6):1119-1124.
3 Hu J, Blair MP, Shapiro MJ, Lichtenstein SJ, Galasso JM, Kapur R.Reactivation of retinopathy of prematurity after bevacizumab injection.Arch Ophthalmol 2012;130(8):1000-1006.
4 Kim J, Kim SJ, Chang YS, Park WS. Combined intravitreal
bevacizumab injection and zone I sparing laser photocoagulation in patients with zone I retinopathy of prematurity. Retina 2014;34(1):77-82.
5 Kim R, Kim YC. Posterior pole sparing laser photocoagulation combined with intravitreal bevacizumab injection in posterior retinopathy of prematurity. J Ophthalmol 2014;2014:257286.
6 Vander JF, McNamara JA, Tasman W, Brown GC. Revised indications for early treatment of retinopathy of prematurity. Arch Ophthalmol 2005;123(3):406-407; discussion 409-410.
7 Early Treatment for Retinopathy of Prematurity Cooperative Group.Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial.Arch Ophthalmol 2003;121(12):1684-1694.
8 Sato T, Wada K, Arahori H, Kuno N, Imoto K, Iwahashi-Shima C,Kusaka S. Serum concentrations of bevacizumab (Avastin) and vascular endothelial growth factor in infants with retinopathy of prematurity. Am J Ophthalmol 2012;153(2):327-333.e1.
9 Harder BC, von Baltz S, Jonas JB, Schlichtenbrede FC. Intravitreal lowdosage bevacizumab for retinopathy of prematurity. Acta Ophthalmol 2014;92(6):577-581.
10 Spandau U, Tomic Z, Ewald U, Larsson E, Akerblom H, Holmstrom G. Time to consider a new treatment protocol for aggressive posterior retinopathy of prematurity? Acta Ophthalmol 2013;91(2):170-175.
11 Connor AJ, Papastavrou VT, Hillier RJ, Shafiq A. Ultra-low dose of intravitreal bevacizumab in the treatment of retinopathy of prematurity. J Pediatr Ophthalmol Strabismus 2015;52 Online:e20-21.
12 Larsson LI, Nuija E. Increased permeability of the blood-aqueous barrier after panretinal photocoagulation for proliferative diabetic retinopathy. Acta Ophthalmol Scand 2001;79(4):414-416.
13 Sanghi G, Dogra MR, Katoch D, Gupta A. Aggressive posterior retinopathy of prematurity: risk factors for retinal detachment despite confluent laser photocoagulation. Am J Ophthalmol 2013;155(1):159-164.e2.
14 Coats DK, Miller AM, Hussein MA, McCreery KM, Holz E, Paysse EA. Involution of retinopathy of prematurity after laser treatment: factors associated with development of retinal detachment. Am J Ophthalmol 2005;140(2):214-222.
15 Steinmetz RL, Brooks HL Jr. Diode laser photocoagulation to the ridge and avascular retina in threshold retinopathy of prematurity. Retina 2002;22(1):48-52.