
Figure 1 Multi-diod laser TM S30-OFT device.
·Clinical Research·
Mustafa Doğan1, Anar Alizada1, Güliz Fatma Yavaş2, Orhan Kemal Kahveci3, Osman Bakan4
1Department of Ophthalmology, Faculty of Medicine, Afyon Kocatepe University, Afyonkarahisar 03200, Turkey
2Department of Ophthalmology, Faculty of Medicine,Hacettepe Univerisity, Ankara 06100, Turkey
3Department of Otolarhinoaryngology, Faculty of Medicine,Afyon Kocatepe University, Afyonkarahisar 03200, Turkey
4Medlife Hospital, İstanbul 34500, Turkey
Abstract
●AlM:To evaluate the long-term sucess rate of laserassisted dacryocystorhinostomy (L-DCR) in patients with nasolacrimal duct obstruction (NDO).
●METHODS:Forty-one eyes of forty patients aged between 21-85y (mean 56.7y) who underwent L-DCR for the treatment of NDO were included in this retrospective,non-randomized study. The follow-up time was 72mo.Functional sucess was defined as the disappearance of epiphora under normal conditions and the presence of a patent ostium on lacrimal irrigation. Anatomical success was defined as a patent lacrimal passage on syringing besides continuing epiphora. Surgical failure was defined as persistent epiphora and closed ostium.
●RESULTS:Twenty-seven of 40 patients (67.5%) were female and 13 of 40 patients (32.5%) were male. The NDO was right-sided in 17 (42.5%) patients and left-sided in 22(55%) patients whereas 1 (2.5%) patient had undergone bilateral surgery. ln 11 (27.5%) patients there were additional nasal abnormalities requiring simultaneous surgical approach. The average time for L-DCR was 26.50±4.9min(16-39min) and the average total amount of laser energy used was 287±27.9 J (239-367 J). At the 5y follow-up, anatomical sucess rate was 75.0% (30 patients) and functional success rate was 65.0% (26 patients), whereas surgical failure was seen in 25% (10 patients). Revision of surgery was performed in 10 cases (25.0%); failure of revision surgery was seen in 2 cases (5.0%).
●CONCLUSlON:Transcanalicular L-DCR is a reliable and fast procedure in the treatment of NDO. lt can be alternative to external DCR which is accepted as the gold standard currently. The functional and anatomical success rate is higher in the first months and years, but still satisfactory at fifth year.
●KEYWORDS:nasolacrimal duct obstruction; laser-assisted dacryocystorhinostomy; 5-year follow-up
Dacryocystorhinostomy (DCR), first described by Toti[1]in 1904. In 1921, Dupuy-Dutemps and Bourget[2], and later Falk[3]in 1961, improved rates of successful fistulization by directly suturing the edges of nasal and lacrimal sac mucosal flaps[4]. In 1982, silicone tube intubation has been improved by Older[5]. It gained popularity and became the standart surgical procedure for the treatment of nasolacrimal duct obstruction (NDO). Nowadays, it is the golden standart surgical procedure for NDO.
Due to pre- and postoperative bleeding and longer procedure and recovery times and leaving facial scar of external dacryocystorhinostomy (EX-DCR), researchers and surgeons tried to find alternative techniques. The first endonasal DCR was performed by Caldwell[6]in 1893, and first laser assisted approach was described in 1990 by Massaroet al[7].
Different laser types have been used in DCR procedures:Holmium:Yttrium-Aluminum-Garnet (Ho:YAG) laser;Potassium-Tytanyl-Phosphate (PTP) laser; Neodymium:YAG(Nd:YAG) laser; Erbium:YAG (Er:YAG) and diode laser[4].
Diode laser-assisted DCR (L-DCR) was first reporterd by Eloyet al[8]in 2000. It used more and more because L-DCR had less tissue damage and sufficient osteotomy can be created using diode laser. The advantages of diode laser are; no external facial skin scar, local anesthesia possibility, less hemorrhage,fast procedure and minimal intra- and postoperative complications[4].
Although, L-DCR has several advantages, long term anatomical and functional success rate is remain unclear. The goal of this study is to evaluate the long term (5y) success rate of L-DCR in a selected patient group with acquired NDO.
This is a retrospective nonrandomized, noncomparative,nonrandomized, interventional study conducted by working on the data of 41 eyes of 40 consecutive patients with epiphora referred to the Department of Ophthalmology, Afyon Kocatepe University Hospital, Afyonkarahisar, Turkey. From September 2008 to March 2012, L-DCR was performed to all subjects using multidiode laser. The study was conducted in compliance with the principles of Declaration of Helsinki and approved by Afyonkarahisar Ethics Committee.
All patients with a history of epiphora underwent preoperative full clinical ophtalmic examination (visual acuity, anterior segment examination, intraocular pressure, fundus examination).Lacrimal drainage system irrigation was performed with 26-gauge needle to determine any obstruction. The Ear,Nose and Throat (ENT) consultant examined the nasal cavity routinely. Dacryocystography was performed to all patients by applying approximately 0.5 mL contrast agent (Lipoidol Ultra fluide 480 mg/10 mL, Guerbet, France).
Surgical TechniqueAll surgeries were performed by the same surgeons (Güliz Fatma Yavaş, Tuncay Küsbeci). Nasal endoscopy was assisted during surgery by the same ENT specialist (Kahveci OK). Seven patients who had additional nasal abnormalities underwent surgery under general anestesia. The remaining 33 patients received local anesthesia.Preoperatively nasal decongestant spray (Iliadin, Santa Farma,Turkey) and lidocaine (Vemcaine Pump Sprey 10%, VEM Medicine, Turkey) was applied into the nasal cavity. Local anesthetic lidocaine hydrochloride 20 mg/mL+epinephrine 0.15 mg/mL (Jetokain, Adeka, Turkey) was administered using 30-gauge needle at three poits to achieve infraorbital,ethmoidal and medial canthal nerve blocks.
After operative site antisepsis using povidone iodine 10%, the upper and lower canaliculi were dilated using Bowman probes.A rigid nasal endoscope with a 0-degree angle was inserted into the nose. Multidiode laser (Intermedical Multidiode S-30 OFT; Figure 1) was used. The settings were adjusted for each patient being at 10 W energy, 400ms pulse, 400ms pause and contact mode. The radius of the diode laser fiberoptic probe used was 600 µm. This probe was introduced into the lacrimal sac through the upper and lower canaliculi, until the transillumination of the aiming beam could be seenviathe nasal endoscope just lateral and superior to the middle turbinate. Of 980 nm diode laser was applied until the largest possible osteotomy was achieved. The area of ostetomy was expanded to approximately 8-10 mm in diameter, and coagulated using diod-laser, carbonized tissue was removed under endoscopic guidance. Nasolacrimal passage was irrigated using 0.9% NaCl from both upper and lower punctums. In all subjects, bicanalicular intubation was performed. Totally 23-gauge silicone tube was then passed through the inferior and superior canaluculi, retreived from the nose, tied as a double knot and the knot was left inside the nose (Figure 2).
Postoperative medication consisted of nasal oximetasoline hydrochloride 0.05% sprey (Iliadin, Santa Farma, Turkey) 3 times a day for the first 2d followed by nasal triamcinolone 0.025% sprey (Nasacort AQ, Aventis, Turkey) 4 times a day for 1mo and topical tobramycin/dexametasone eye drops(Tobradex, Alcon Inc., USA) 4 times a day for 1mo.
Follow-up time was 5y. Each patient examined at day 1, week 1,month 1, month 3 and then every 3mo for the first year. After the first year, follow-up was done 12 monthly till 5y. Lacrimal irrigation performed at every visit. The silicon tube removed at 3mo postoperatively.
Functional success was defined as the disappearance of epiphora under normal conditions and the presence of patent ostium on lacrimal irrigation. Anatomical sucess was defined as a patent ostium on lacrimal irrigation besides continuing epiphora. Patients with persistent epiphora and closed ostium on lacrimal irrigation were defined as surgical failure.Statistical analysis was performed using IBM SPSS Version 22.0 (IBM Corp., Armok, NY, USA).
Forty-one eyes of forty patients were included in this study.Of 67.5% of patients (27 out of 40) were female and 32.5% of patients (13 out of 40) were male. Patients age ranged between21-85y (mean 56.7y; Table 1). The NDO was right-sided in 17(42.5%) patients and left-sided in 22 (55%) patients whereas 1(2.5%) patient had undergone bilateral surgery.

Figure 1 Multi-diod laser TM S30-OFT device.
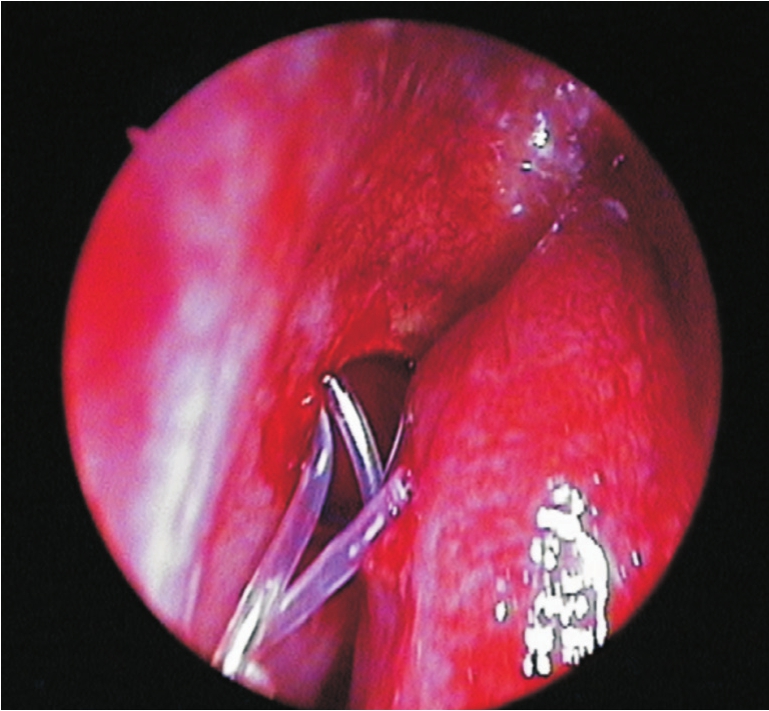
Figure 2 Endoscopic apperance when free ends tied after bicanalicular silicone tube intubation during DCR operation.
The surgery performed under general anestesia in 7 (17.5%)patients whereas 33 patients (83.5%) with local anesthesia. The mean power of used laser energy was 287±27.9 J (239-367 J). The mean procedure time was 26.50±4.9min (16-39min). Silicone tubes removed at postoperative month 3.
At postoperative month 6, functional success was seen in 90%of subjects whereas at postoperative month 12 it was seen in 84% of subjects. At postoperative 60mo (5y), functional sucess was seen in 26 patients (65%), anatomical success was seen in 30 patients (75%). Surgical failure was seen in 10 (25%)subjects (Figure 3).
There were no complications seen intraoperatively.Postoperatively, 1 (2.5%) patient had epistaxis, 1 (2.5%) patient had punctal slitting. Revision of surgery was performed in 10 cases (25%), failure after the revision surgery was seen in 2 cases (5%). There were additional nasal abnormalities in 11 (27.5%) patients. Three patients (7.5%) had concha hypertrophy, 6 patients (15%) had septum deviation, 1 patient(2.5%) had synechia and 1 patient (2.5%) had synechia with septum deviation. Among these patients, 8 of them had septoplasty and 2 of them underwent polip excision together with L-DCR. Three patients who had concha hypertropy were women, 2 of the patients who had septum deviation were women, and 2 patients who had synechy were women .When we analyzed all 27 women patients who underwent L-DCR,3 (11.11%) had concha hypertrophy, 2 (7.4%) had septum deviation, and 2 (7.4%) had synechia. In men, 4 patients(30.77%) had septum deviation (Table 2).
Eloyet al[8]described the use of diode laser for endocanalicular laser DCR surgery in 2000 and reported a success rate of 58.6% (17 out of 29 patients) at postoperative month 6.Alañón Fernándezet al[9]observed 43 patients undergoing transcanalicular DCR for 4-38mo, and reported a sucess rate of 90.7%. Failure was seen in 4 subjects where 2 patients (4.65%)had epiphora and permeable tract, 1 patient (2.2%) presented with lower canaliculi obstruction, and 1 patient showed total closing of osteotomy. In our study 1 (2.5%) patient had an epistaxis after surgery and 1 (2.5%) patient had punctal slitting after surgery which was compatible with the literature.

Figure 3 Anatomical and functional success rate of L-DCR within 5y.
Caversaccioet al[10]used erbium laser in transcanalicular DCR and reported 75% success in 2001. Gulatiet al[11]evaluated the role of endoscopic endonasal DCR in pediatric population aged between 2-12y and reported a success rate of 85% at 6 months.Similarly, Marfatiaet al[12]described 95.65% sucess rate in 21 pediatric patients. Nuhogluet al[4]followed 42 patients undergoing L-DCR for 42mo and reported a long term sucess rate of 95.2%. Denget al[13]reported a sucess rate of 96.0%in subjects undergoing endoscopic DCR at 1-year follow-up.Coumouet al[14]evaluated subjects undergoing endoscopic DCR over a 14-year period from 1999 to 2014 retrospectively and found that adult DCR had an anatomical sucess of 90.1%whereas in children, anatomical success was 91.5%. In our study anatomical success at 6-month follow-up was 90%, at 12-month follow-up was 80%, at 36-month follow-up was 77% and at 60-month follow-up was was 75% of rate. Of 60-month rates in our study was not compatible to the studies was described before; it may cause of selection of age range in our study.
The study of Linet al[15]consisted of 53 consecutive patients who underwent revision endoscopic DCR between 2002 and 2013 for lacrimal duct obstruction. The aim of this study was to identify causes of previous DCR failure, and the authors compared patients whose initial surgery was performed through an external versus an endoscopic approach. They detected in this study that, surgical sucess rates for revision DCR surgery were comparable between the groups, with a mean follow-up of 12.7mo (75% external versus 73.3%endoscopic;P=0.90). Deryaet al[16]compared the success rates of L-DCR and external DCR, and found a sucess rate of 68%in 25 cases undergoing L-DCR after a mean follow-up time of 7.12mo whereas the success rate in 29 patients undergoing external DCR was 86% with a mean follow-up time of 8.82mo.Though the success rate was higher in the EX-DCR group,it was reported to be statistically not significant (P=0.202).Mourya and Rijal[17]compared the efficacy of L-DCR with conventional EX-DCR; and found an overal sucess rate was 90.12% in patients who underwent L-DCR and 95.40% in patients who underwent conventional EX-DCR. Leeet al[18]reported in their retrospective study that the overall sucess rate of endoscopic endonasal DCR was 86.3% for at least 6mo observation. The study of Feijóet al[19]consisted of modified L-DCR where nasal mucosa was removed prior to laser osteotomy versus conventional L-DCR. In the case of modified DCR, the anatomical and functional sucess rates after 12mo were 90 and 86% respectively; whereas after conventional L-DCR, these rates were 77% and 72%, respectively. As the difference of success rates between these 2 methods was statistically not significant, they reported both procedures to be safe and fast with low morbidity.
Table 1 Demographic parameters of patients

Table 2 Additional nasal abnormalities of patients with NDOn(%)
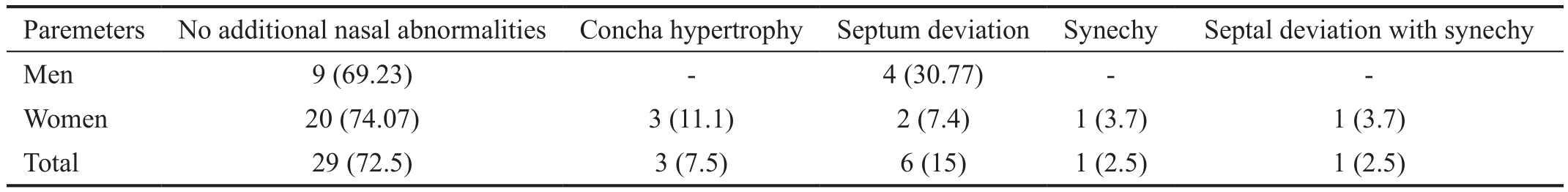
NDO: Nasolacrimal duct obstruction.
In our study rate of anatomical success was 75%, functional success was 65% and surgical failure was 25%. These rates were lower than the success rates reported in the literature. We think that this can be related with the long follow-up time in our study. In the literature there are a few studies that observed patients for a long time period such as ours. The results of the study performed by Kaynaket al[20]are similar to our study. In this study they reported a functional sucess rate of 85.4% at postoperative month 3 that decreased to 67.7% at postoperative month 6, 63.3% at first year and 60.3% second year, while the patency of the lacrimal drainage was restored in 93.1%,74.6%, 69.5%, and 68.2% of the cases, respectively. Also in the study of Plazaet al[21]there was no significant difference between 12mo and 36mo. Ajaloolineet al[22]compared external transcanalicular DCR with L-DCR with amean follow-up of 18mo, and reported a success rate of 94.3% in the L-DCR group versus 92.7% in the EX-DCR group.
In our study, the mean procedure time was 26.5min which was found to be compatible with the literature. Ajaloolineet al[22]reported that the mean operation time was 19min for L-DCR whereas it was 61min for EX-DCR. Mouryaet al[17]reported mean total surgical time to be 17.41min in L-DCR group and 49.49min in conventional EX-DCR group.
Mean laser energy we used was 287 J (239 -367 J), which was consistent with the studies in the literature. Drnovsek-Olupet al[23]reported an average of 245 J (195 to 685 J) of laser energy; Cintraet al[24]used 289 to 532 J (mean 392 J) of laser energy to create an ostium. Basmaket al[25]achieved an increase in surgical sucess (66%-86%) when the mean laser energy that was used during surgery was decreased from 300 to 165 J.
In our study the silicone tubes was removed at 3thmonth. This interval is consistent with the studies in the literature. Rebeizet al[26]recommends the silicone tubes to be removed after at least 6wk. The suggestion of Häuseet al[27]is 6mo, because it creates the risk of fibrosis.
The strength of our study is follow-up time. We followed patients up to 5y. Due to our best of knowledge, there is no other study that has 5y or more follow-up time.
The limitations of our study are, small sample size and lack of control group (no cases of endonasal endoscopic or EX-DCR).Due to our clinic’s limited capacity, we could not operate and followed-up more patients.
In conclusion, transcanalicular L-DCR is known to have a shorter operative time and a relative lower complication rate.It has been increasingly utilized due to the advantages of faster rehabilitation, preservation of the lacrimal pump function,decreased invasiveness, and the absence of an external scar.The functional and anatomical success rate is higher in the first months and years, but still satisfactory at fifth year. But,further long term comparative studies are required to clarify the effectiveness of multidiode L-DCR in patients with NDO.
Conflicts of Interest:Doğan M, None; Alizada A, None;Yavaş GF, None; Kahveci OK, None; Bakan O, None.
REFERENCES
1 Toti A. New conservative method of radical cure of chronic suppurations of the lacrimal sac (dacryocystorhinostomy).Clin Mod Firenze1904;10:385-394.
2 Dupuy-Dutemps L, Bourguet M. Procede plastique de dacryocystorhinosyomieet ses resultants.Ann Ocul1921;158:241-261.
3 Falk P. Communication of the lacrimal caniculi with the nasal cavity by complete exposure and implantation of the lacrimal sac mucosa.Z Laryngol Rhinol1961;40:265-276.
4 Nuhoglu F, Gurbuz B, Eltutar K. Long-term outcomes after transcanalicular laser dacryocystorhinostomy.Acta Otorhinolaryngol Ital2012;32:258-262.
5 Older JJ. Routine use of a silicone stent in a dacryocystorhinostomy.Ophthalmic Surg1982;13(11):911-915.
6 Caldwell GW. Two new operations for obstruction of the nasal duct,with preservation of the canaliculi.Am J Ophthalmol1893;10:189-192.
7 Massaro BM, Gonnering RS, Harris GJ. Endonasal laser dacryocystorhinostomy. A new approach to nasolacrimal duct obstruction.Arch Ophthalmol1990;108(8):1172-1176.
8 Eloy P, Trussart C, Jouzdani E, Collet S, Rombaux P, Bertrand B.Transcanalicular diode laser assisted dacryocystorhinostomy.Acta Otorhinolaryngol Belg2000;54(2):157-163.
9 Alañón Fernández FJ, Alañón Fernández MA, Martínez Fernández A,Cárdenas Lara M. Transcanalicular dacryocystorhinostomy technique using diode laser.Arch Soc Esp Oftalmol2004;79:325-330.
10 Caversaccio M, Frenz M, Schär P, Häusler R. Endonasal and transcanalicular Er:YAG laser dacryocystorhinostomy.Rhinology2001;39(1):28-32.
11 Gulati SP, Wadhera R, Khurana AK, Singh N, Kalra V, Ghai A. Results of endonasal dacryocystorhinostomy in pediatric patients.Ear Nose Throat J2017;96(6):E41-E45.
12 Marfatia H, Shah K, Patil S, Parmar Y. Endonasal dacryocystorhinostomy in children: Our experience.Int J Surg2017;47:91-95.
13 Deng HY, Wang T, Huang XK, Yang QT, Ling SQ, Wang WH, Li MJ,Ning FQ, Zhang GH. Comparative study of recessive spherical headed silicone intubation and endonasal dacryocystorhinostomy under nasal endoscopy for nasolacrimal duct obstruction.Sci Rep2017;7(1):7734.
14 Coumou AD, Genders SW, Smid TM, Saeed P. Endoscopic dacryocystorhinostomy: long-term experience and outcomes.Acta Ophthalmol2017;95(1):74-78.
15 Lin GC, Brook CD, Hatton MP, Metson R. Causes of dacryocystorhinostomy failure: external versus endoscopic approach.Am J Rhinol Allergy2017;31(3):181-185.
16 Derya K, Demirel S, Doganay S,et al. Endoscopic transcanalicular diode laser dacryocystorhinostomy: is it an alternative method to conventional external dacryocystorhinostomy?Ophtal Plast Reconstr Surg2013;29(1):15-17.
17 Mourya D, Rijal RK. Transcanalicular laser-assisted dacryocystorhinostomy with diode laser.Orbit2017;36(6):370-374.
18 Lee JJ, Lee HM, Lim HB, Seo SW, Ahn HB, Lee SB. Learning curve for endoscopic endonasal dacryocystorhinostomy.Korean J Ophthalmol2017;31(4):299-305.
19 Feijó ED, Caixeta JA, de Souza Nery AC, Limongi RM, Matayoshi S. A comparative study of modified transcanalicular diode laser dacryocystorhinostomy versus conventional transcanalicular diode laser dacryocystorhinostomy.Eur Arch Otorhinolaryngol2017;274(8):3129-3134.
20 Kaynak P, Ozturker C, Yazgan S, Karabulut GO, Akar S, Demirok A,Yilmaz OF. Transcanalicular diode laser assisted dacryocystorhinostomy in primary acquired nasolacrimal duct obstruction: 2-year follow up.Ophthalmic Plast Reconstr Surg2014;30(1):28-33.
21 Plaza G, Beteré F, Nogueira A. Transcanalicular dacryocystorhinostomy with diode laser: long-term results.Ophthalmic Plast Reconstr Surg2007;23(3):179-182.
22 Ajalloueyan M, Fartookzadeh M, Parhizgar H. Use of laser for dacrocystorhinostomy.Arch Otolaryngol Head Neck Surg2007;133(4):340-343.
23 Drnovse-Olup B, Beltram M. Transcanalicular diode laser assisted dacryocystorhinostomy.Indian J Ophthalmol2010;58:213-217
24 Cintra PP, Anselma-Lima WT. Endocanalicular diode laser assisted dacryocystorhinostomy.Otolaryngol Head Neck Surg2008;139:159-161.
25 Basmak H, Caklı H, Sahin A, Gursoy H, Ozer A, Altun E, Yildirim N. Comparison of endocanalicular laser dacryocystorhinostomy with and without endonasal procedures.Graefes Arch Clin Exp Ophthalmol2011;249(5):737-743.
26 Rebeiz EE, Shapshay SM, Bowlds JH, Pankratov MM. Anatomic guidelines for dacryocystorhinostomy.Laryngoscope1992;102(10):1181-1184.
27 Häusler R, Caversaccio M. Microsurgical endonasal dacryocystorhinostomy with long-term insertion of bicanalicular silicone tubes.Arch Otolaryngol Head Neck Surg1998;124(2):188-191.
Citation:Doğan M, Alizada A, Yavaş GF, Kahveci OK, Bakan O.Laser-assisted dacryocystorhinostomy in nasolacrimal duct obstruction:5-year follow-up.Int J Ophthalmol2018;11(10):1616-1620
DOl:10.18240/ijo.2018.10.07
Accepted:2018-06-28
Received:2018-03-05
Correspondence to:Mustafa Doğan. Department of Ophthalmology, Faculty of Medicine, Afyon Kocatepe University,Ali Cetinkaya Kampüsü, Afyonkarahisar 03200,Turkey.mustafadogan@yahoo.com