Contralateral eye study of refractive, topographic and aberrometric outcomes after femtosecond assisted MyoRing implantation and DALK for management of keratoconus
Mohamed Omar Yousif, Azza Mohamed Ahmed Said
Department of Ophthalmology, Faculty of Medicine, Ain Shams University, Cairo 11736, Egypt
Abstract
●AlM:To evaluate the efficacy of femtosecond laser assisted MyoRing intrastromal corneal implant and deep anterior lamellar keratoplasty (DALK) for management of moderate to advanced keratoconus regarding the degree of changes in visual acuity, refraction, corneal asphericity and aberrations.
●METHODS:A prospective non comparative interventional case study was conducted in Ophthalmology Department,Ain Shams University Hospital in the period from January 2015 to February 2017. The study included 30 eyes of moderate to advanced keratoconus. MyoRing was implanted in one eye (Group l) and DALK operation was performed in the contralateral eye of the same patient (Group ll).Preoperative and 6mo post-operative uncorrected visual acuity(UCVA), corrected distance visual acuity (CDVA), spherical equivalent (SE), corneal and refractive astigmatisms,keratometry and Q-value using topography images were acquired. Quality of vision was assessed in all eyes including total corneal, anterior corneal high order aberrations analysis at 5 mm pupil size and the Strehl ratio of point spread function (PSF) as an objective measure of glare.
●RESULTS:Mean postoperative UCVA, CDVA, SE, refractive astigmatism, keratometry readings and asphericity were statistically improved compared to preoperative parameters in both groups (P<0.05). Significant reduction of all corneal aberrations following both techniques(P<0.05) was achieved except mean trefoil and mean PSF in Group l (P>0.05). Postoperative corneal aberrations were significantly lower in Group ll compared to Group l.A statistically significant negative correlation was found in Group l between the mean change in CDVA (logMAR)and the mean preoperative and mean postoperative total corneal aberrations root mean square (RMS;r=-0.78,P=0.04). Also a statistically significant negative correlation was found between mean preoperative coma RMS and mean post PSF (r=-0.86,P=0.01). ln Group ll, there was a statistically significant positive correlation between mean change in CDVA (logMAR) and mean change in Kmax(r=0.87,P=0.01) and between mean change in refractive cylinder and mean postoperative PSF (r=0.76,P=0.05).
●CONCLUSlON:Femtosecond laser assisted MyoRing and DALK are effective in improving visual acuities, refraction,corneal asphericity and aberrations. MyoRing reduced spherical error more than the corneal cylinder. Post operative homogenous corneal surface and good image quality were achieved following both techniques compared to the preoperative state. However, DALK results in better image quality and lower corneal aberrations.
●KEYWORDS:aberrations; deep anterior lamellar keratoplasty;femtosecond laser; keratoconus; MyoRing
INTRODUCTION
Keratoconus patients require surgery in advanced stages of the disease, because of impaired vision and/or intolerance to spectacles and contact lenses. Altered corneal curvature, consequent irregular astigmatism and central corneal scarring are the causes of poor visual acuity. The goals of corneal transplantation are to provide corneal clarity with minimal irregularity to permit indefinite good vision[1].
Penetrating keratoplasty (PK) had been the standard procedure for the surgical treatment of keratoconus[2]. The drawbacks of this technique were endothelial rejection, ocular surface and suture-related problems. Endothelial cell failure is also a risk of PK in the long-term, as life expectancy of patients keeps on increasing. In addition, steroids are needed for relatively longperiods, adding the risk of secondary glaucoma and cataract formation[3]. Less risk of these complications was achieved with deep anterior lamellar keratoplasty (DALK). It is a surgical procedure that involves removal of corneal stroma down to Descemet membrane (DM) and replacing the stroma with a donor cornea. The presence of a normal endothelium is the absolute requirement for this procedure[4].
The visual outcomes after DALK, although comparable with PK, may be just slightly inferior or less predictable compared with PK, given unpredictable issues regarding residual stromal thickness and DM folds. Nonetheless, elimination of risk of endothelial rejection compensates for this difference[5].Technical difficulty, a steep learning curve and the presence of interface haze are the limitations of this modality of treatment.Most of the innovations in the surgical technique of DALK over the past decade have primarily been focused on avoiding these limitations[4].
Owing to the limitations of corneal transplants, an alternative surgical procedure is developed using a corneal intrastromal implantation system (CISIS). This treatment involves a fullring flexible implant known as a MyoRing implanted into a corneal pocket[6]. Minimizing the spherocylindrical error by modifying the central corneal curvature and reducing the corneal higher-order aberrations by regularizing the corneal surface are the aims of such implantation[7-8]. The advantages of this technology are safety, reversibility, and stability without impairment of the optic axis[6].
Microkeratome pocket creation for implantation of the ring was performed (mechanical dissection) with good visual and refractive results in many studies[6,9-10]. However, the use of femtosecond laser for corneal tunnel creation allows the surgeon to program the tunnel dissection at a predetermined depth with a high degree of precision[11]. This gives better outcomes with fewer complications than a mechanical dissector[12].
For corneal transplant surgery, the laser allows the surgeon to focus the laser energy at a particular depth and then rapidly cut the tissue at that depth without causing any additional injury to the surrounding tissues. This permits doing a smooth lamellar dissection with high precision and allows the surgeon to pattern these cuts into shapes creating a highly precise incision resulting in a perfect match of the donor tissue and the host tissue and a stronger junction and quicker visual recovery[13].
Anterior corneal aberrometric analysis is an important tool in clinical practice for evaluating the ocular optical quality because the first refractive interface (air-cornea) is the most important contributor to the total power of the eye because of the large difference in refractive index existing at this point[11].Significant correlation between optical quality in terms of high order aberrations (HOAs) and visual quality in term of best corrected spectacle visual acuity (BCVA) supporting the value of aberration measurements in predicting visual performance[14].
Assessment of corneal HOAs after DALK for keratoconus was studied in some reports compared with that following PK[15-17], and in two studies[12,18]following MyoRing implantation. However, no studies compared post operative changes between the two techniques.
The aim of the present study was to evaluate the efficacy of two techniques; femtosecond laser assisted MyoRing implantation and DALK for management of moderate to advanced keratoconus, and to compare their postoperative outcomes, regarding degree of changes in visual acuity,refraction, corneal asphericity and aberrations using corneal topography and aberrometry.
SUBJECTS AND METHODS
A prospective non comparative interventional case study included eyes diagnosed as moderate to advanced keratoconus.All participants were non-contact lens wearers. Patients were recruited from a private practice and Ain Shams University Ophthalmic Clinics in the period from January 2015 to February 2017. All possible risks and benefits were explained clearly to the patients before enrollment, written informed consents were taken from all patients after explanation of all procedures to include them in the study. One surgeon (Yousif MO) performed all surgeries and followed up patients at private ophthalmic subspecialty center. The explanation of the procedure to all patients was done and an informed written consent was taken. This study was adhered to the tenets of the Declaration of Helsinki. The approval of Faculty of Medicine,Ain Shams University Research Ethical Committee (FMASU REC) was obtained prior to the start of the study.
PreoperativeIn the same keratoconus patient, one eye was implanted with MyoRing (Study group I) and the contralateral eye had DALK operation (Study group II). Both operations were femtosecond laser assisted. Inclusion criteria were;diagnosis of moderate [steepest K=45-52 diopters (D)]to advanced keratoconus (steepest K≥52 D) according to keratoconus study classification using the steepest K-reading[19]with history of progression over the previous 12mo in the form of change in the steepest K of ≥1 D[20], age between 18 and 45y, maximum K-reading less than 65 D, minimum corneal thickness greater than 400 μm at the thinnest corneal location, and patients able to maintain follow up for 6mo postoperatively. Exclusion criteria were as follows: associated ocular disorders, prior ocular surgeries, previous history of hydrops, evidence of infectious corneal disease in the study eye, unclear visual axis, low endothelial cell count or any endothelial abnormality by specular microscopy, pregnancy or nursing and systemic collagen diseases.
Preoperative evaluation composed of uncorrected visual acuity(UCVA) and best spectacle-corrected distance visual acuity(CDVA) measurement, manifest and cycloplegic refraction, slit lamp examination, fundus examination, corneal topography(Pentacam, Oculus, Wetzlar, Germany) and specular microscopy (SP-1P specular microscope, Topcon, Japan).Evaluation of visual quality in terms of total and anterior corneal aberrometry analysis and, the simulated vision function(point spread function, PSF) were performed preoperatively and postoperatively after complete suture removal and stability of refraction using Sirius Scheimpflug Analyzer (CSO,Costruzione Strumenti Oftalmici, Firenze, Italy).
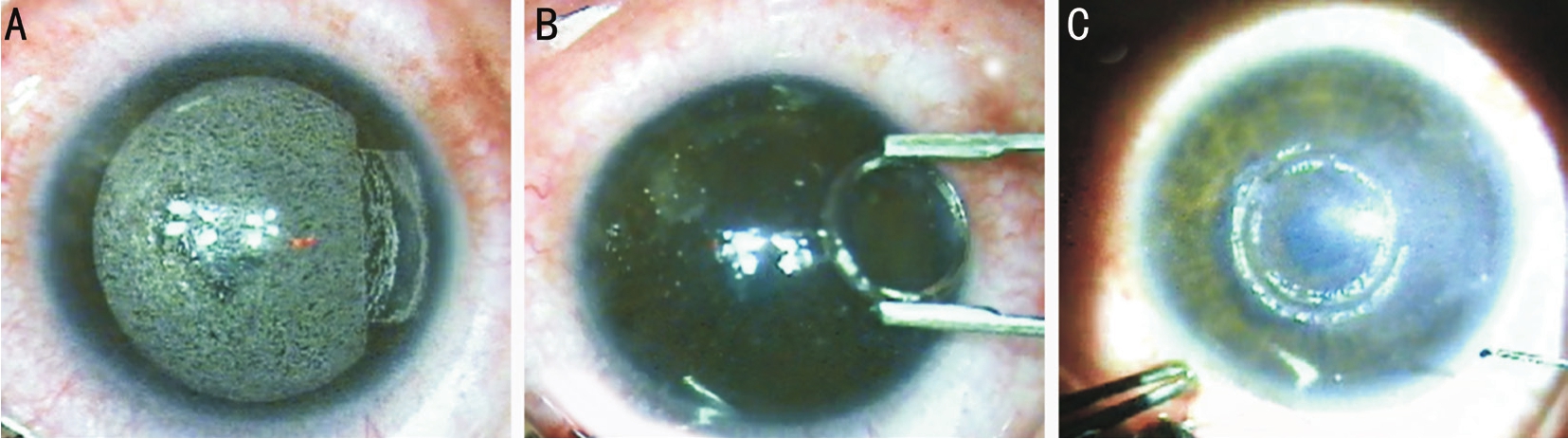
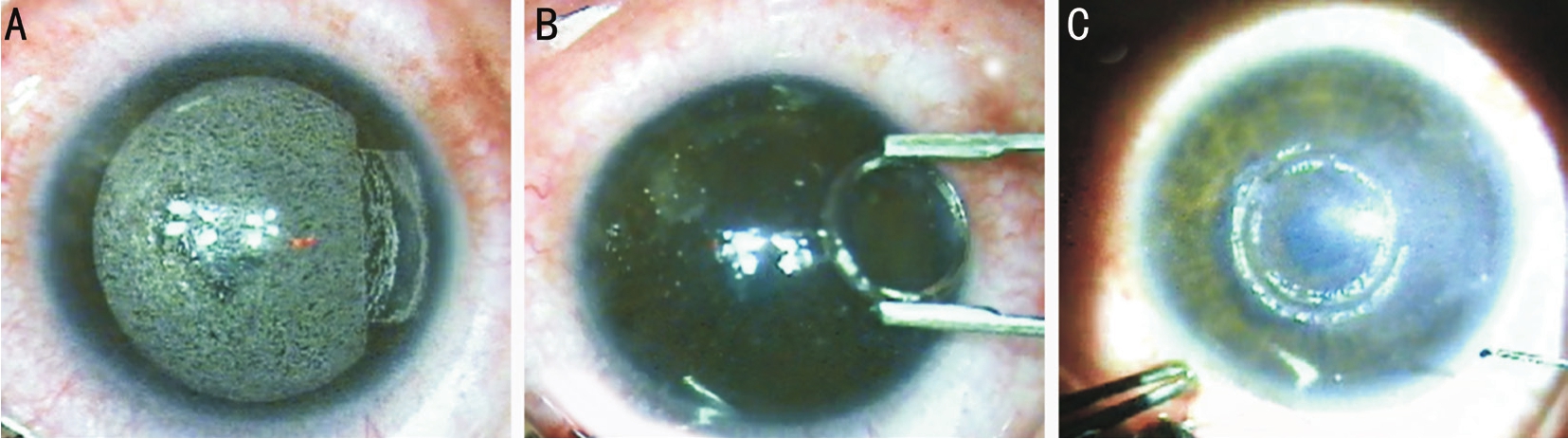
Figure 1 Surgical steps of femtosecond laser assisted MyoRing implantation
A: Corneal pocket creation; B: The deformable ring is hold with a special forceps in order to implant it through 5-mm temporal incision tunnel; C: The complete ring is in its final position inside the corneal pocket with proper centration.
Operative and Postoperative
Group ISurgical procedure for MyoRing implantation was performed under topical anesthesia.
Step 1 (Pocket creation using femtosecond laser)Creation of corneal pocket using femtosecond laser (Wavelight-FS 200, Alcon, USA; Figure 1A). It was designed so as 9 mm in diameter and 300 μm in depth, with a 5-mm small incision tunnel located on the temporal periphery of the cornea.
Step 2 (Ring diameter and thickness selection and insertion)The diameters of the rings were 5 or 6 mm (choice is according to the scotopic pupil and degree of keratoconus),with a thickness of 240, 280, or 320 μm (choice is according to the mean central K reading). The nomogram recommended by the manufacturer (Middle East modified nomogram) was used for ring choice but with some modifications based on surgeon’s experience (Table 1).
An implantation forceps was used to implant the ring. It ovalized the deformable 360° ring in one dimension facilitating its entry in the corneal pocket through the 5-mm temporal incision tunnel (Figure 1B). Once placed into the pocket, the ring inflated to its original preoperative rounded shape. The incision was self-sealed and required no suturing (Figure 1C).No surgical complications were reported in any of the cases.
Postoperatively, gatifloxacin 0.3% and dexamethasone 0.1% eye drops were prescribed for four times daily for one week. Follow up periods were done at 1d, 1wk, 1, 3 and 6mo after surgery for all patients. Figure 1 demonstrated the main surgical steps of femtosecond assisted MyoRing implantation.
Group IIDALK (big bubble technique with complete bearing of DM) operation was performed under local periorbital anesthesia.
Step 1Femtosecond laser (Wavelight-FS 200, Alcon, USA)was used to prepare the recipient and donor tissues as follows:Recipient cornea: A deep complete lamellar cut was created,leaving a residual bed (150 μm) of endothelium, DM and thin part of the corneal stroma. The side cuts were designed to be straight cut or mushroom shaped. The diameter of the side cuts was designed to be 3 mm less than the vertical recipient corneal diameter leaving 1.5-2 mm circumferential recipient tissue. Donor graft: full thickness straight or mushroom shaped side cuts were designed to fit the same dimensions used to cut the recipient cornea. The endothelial layer was left in place till the completion of the bubble dissection of the residual stromal bed from the recipient cornea.
Step 2Under the operating microscope, the remaining surgical procedures were performed as follows: the femtosecond laser cut superficial corneal cap is removed (Figure 2A). A Fogla 27-gauge air injection cannula or bent insulin syringe, attached to a 3 mL air-filled syringe was inserted deep into the corneal stroma and was advanced for 2 to 4 mm, aiming posteriorly toward DM in a paracentral position at an angle almost parallel to the cornea (Figure 2B). Air then was injected forcefully into the deep stroma, reaching a plane and causing a separation of the DM from the overlying stroma up to 0.5 to 1 mm away from the trephination edge (Figure 2C).
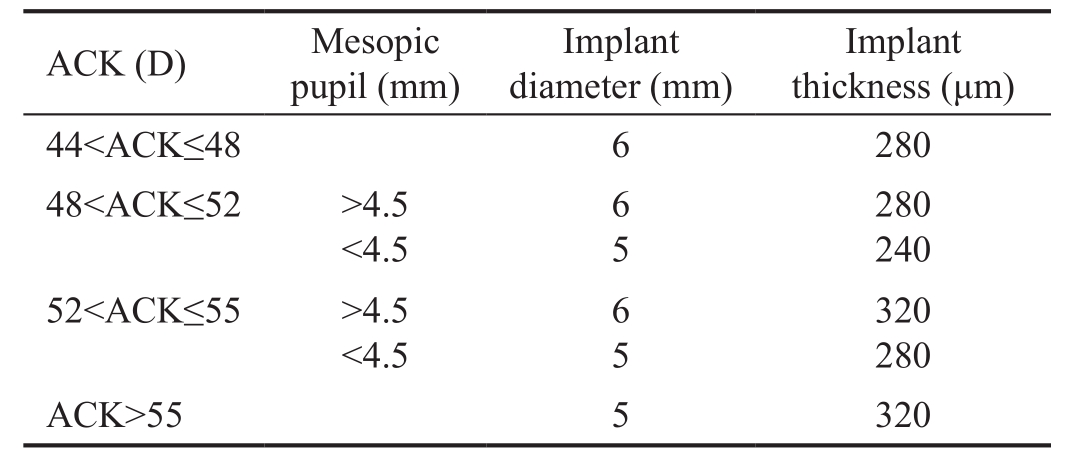
Table 1 Surgeon modified nomogram for MyoRing diameter and thickness choice
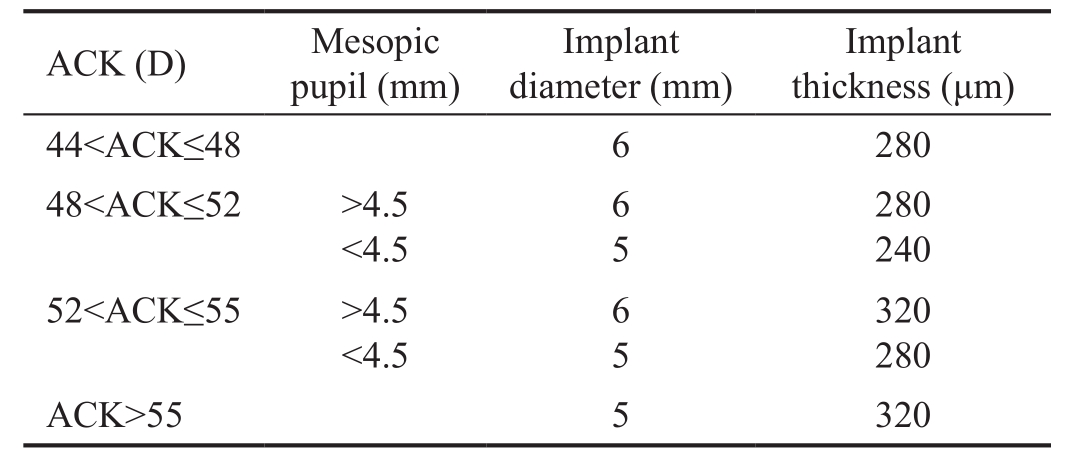
ACK: Average central keratometry.
ACK (D) Mesopic pupil (mm)Implant diameter (mm)Implant thickness (μm)44<ACK≤48 6 280 48<ACK≤52 >4.5<4.5 65 280 240 52<ACK≤55 >4.5<4.5 65 320 280 ACK>55 5 320
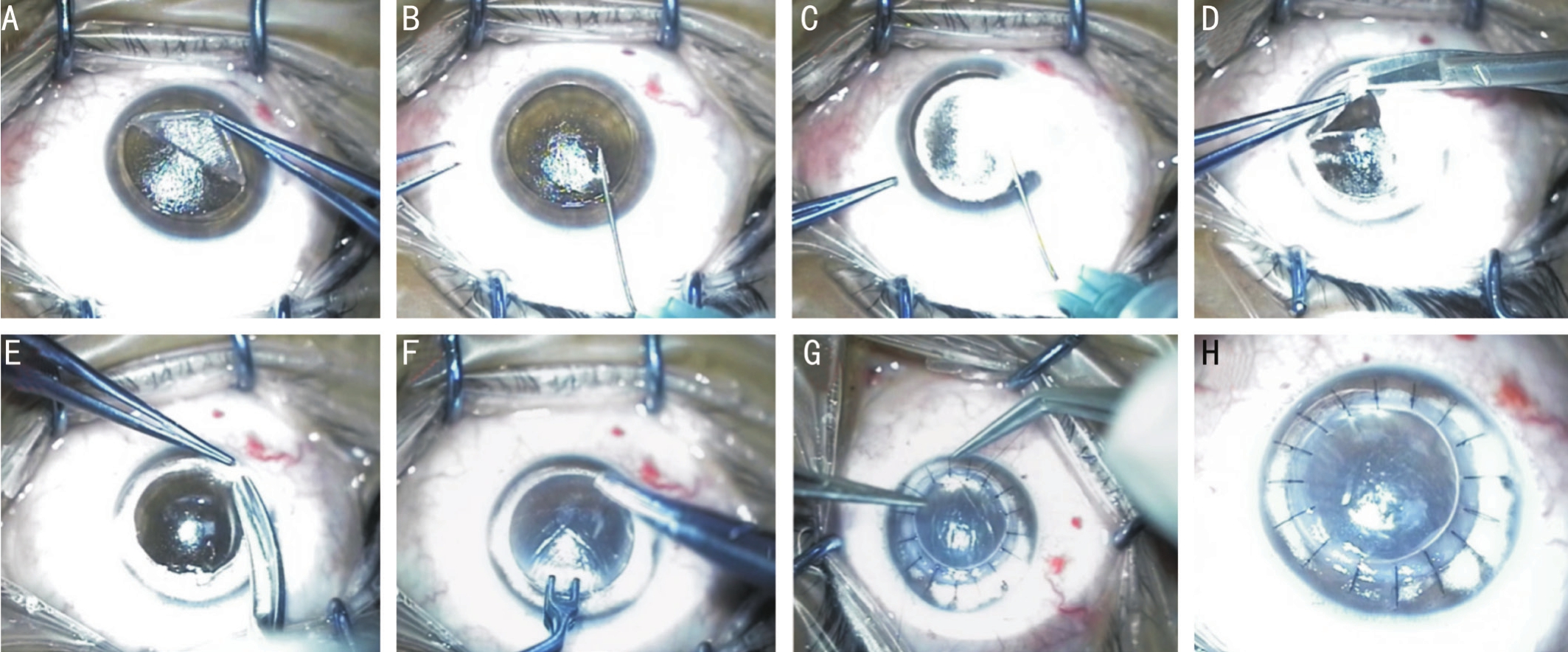
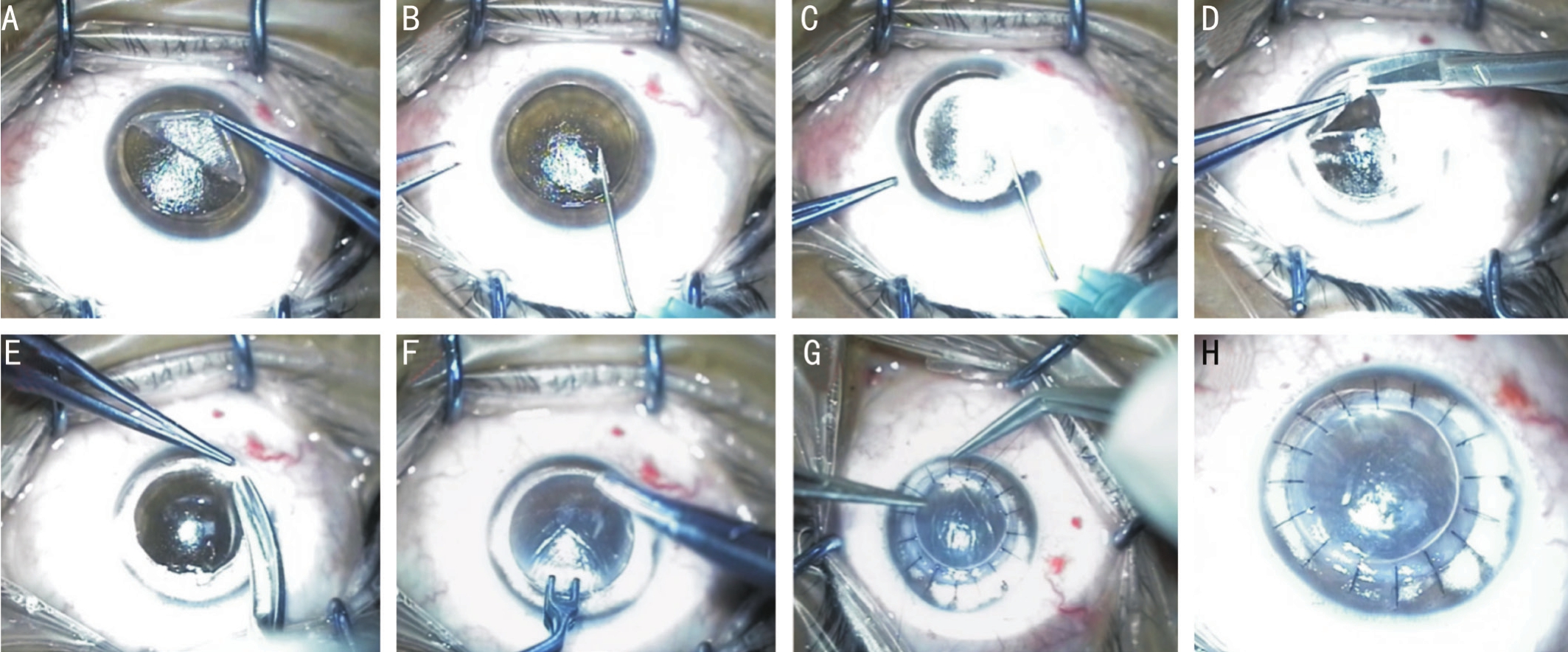
Figure 2 Surgical steps of femtosecond laser assisted DALK
A: A deep complete lamellar cut was created, leaving a residual bed; B:Bent insulin syringe, attached to a 3 mL air-filled syringe was inserted deep into the corneal stroma and was advanced for 2 to 4 mm, aiming posteriorly toward DM in a paracentral position at an angle almost parallel to the cornea; C: Air then was injected forcefully into the deep stroma; D, E: The stromal layers were divided in four quadrants and were excised with blunt-tipped microscissors; F: Corneal donor button was placed over the recipient’s bed following preparation; G, H: The graft is secured using 16 interrupted 10-0 nylon sutures.
After putting some viscoelastic on the center of the cornea,a 15-degree knife was used to make an incision in the most elevated anterior wall of the big bubble. Viscoelastic then was injected in the collapsed space. A blunt spatula was introduced in the space to make sure that the cleavage plane was complete.The stromal layers were divided in four quadrants and were excised with blunt-tipped microscissors (Figure 2D, 2E).
DM and endothelium of the femtosecond laser cut donor corneal button were stained with trypan blue to enable identification and then were removed with a dry swab or forceps. The graft is secured using 16 interrupted 10-0 nylon sutures (Figure 2F-2H). Figure 2 illustrated the surgical steps of femtosecond assisted DALK operation.
Patients received topical gatifloxacin 0.3% and prednisolone acetate 0.1% eye drops. The antibiotic was discontinued after complete epithelialization, whereas the steroid was tapered gradually over 2mo. Patients were followed at postoperative days 1, 3, 7, 14, and 28; then biweekly until 3mo; then monthly until 6mo. Post-operative selective suture removal was based on the amount of corneal astigmatism, guided by topographic pattern starting from the 4thpostoperative month.
Postoperative evaluation and data collection from both groups were done 6mo postoperative and composed of UCVA and best spectacle-CDVA measurement, manifest and cycloplegic refraction, slit lamp examination, corneal topography(Pentacam, Oculus, Wetzlar, Germany). Lines of improvement in acuity were calculated in logarithmic scales according to logMAR notation.
To assess the quality of vision pre- and postoperatively in all eyes and to compare between the topographic and aberrometric changes induced by the two techniques, a 3D Sirius Scheimpflug system (CSO, Costruzione Strumenti Oftalmici, Firenze,Italy) was used to measure and analyze the corneal high order aberrations (HOAs) and glare. This was performed at least 2mo following complete suture removal in study group II and stabilization of refraction in both groups. The root mean square(RMS) values (μm) were evaluated for corneal HOAs at 5 mm pupil size, total and anterior corneal aberrations, coma, trefoil,tetrafoil, spherical type. The Strehl ratio of PSF was used as an objective measure of glare. The higher RMS values, the lesser the homogeneity of the corneal surface with no uniform refraction while the higher Strehl ratio of PSF indicating the better image quality.
Statistical AnalysisData were collected, tabulated, coded and analyzed using SPSS 13 software (SPSS Inc., Chicago,Illinois, USA). Normality of data was assessed by Kolmogorov Smirnov test. Non-parametric quantitative data was expressed as median and interquartile range (IQR), 95% confidence interval for mean. Comparison between variables of dependent samples was performed using Wilcoxon test. Mann-Whitney test was used to compare between variables of two independent samples.
Parametric continuous variables were expressed as mean and standard deviation. Description of qualitative variables was in the form of numbers and percentages. Chi-square test was used to compare between qualitative data. Paired sample Student’st-test was used to compare between quantitative variables of one group before and after surgery and independent sample Student’st-test was used to compare between quantitative variables of the two groups. Spearman’s correlation coefficientwas used to assess the correlation between different variables.The level of significance was set atP-value <0.05.
RESULTS
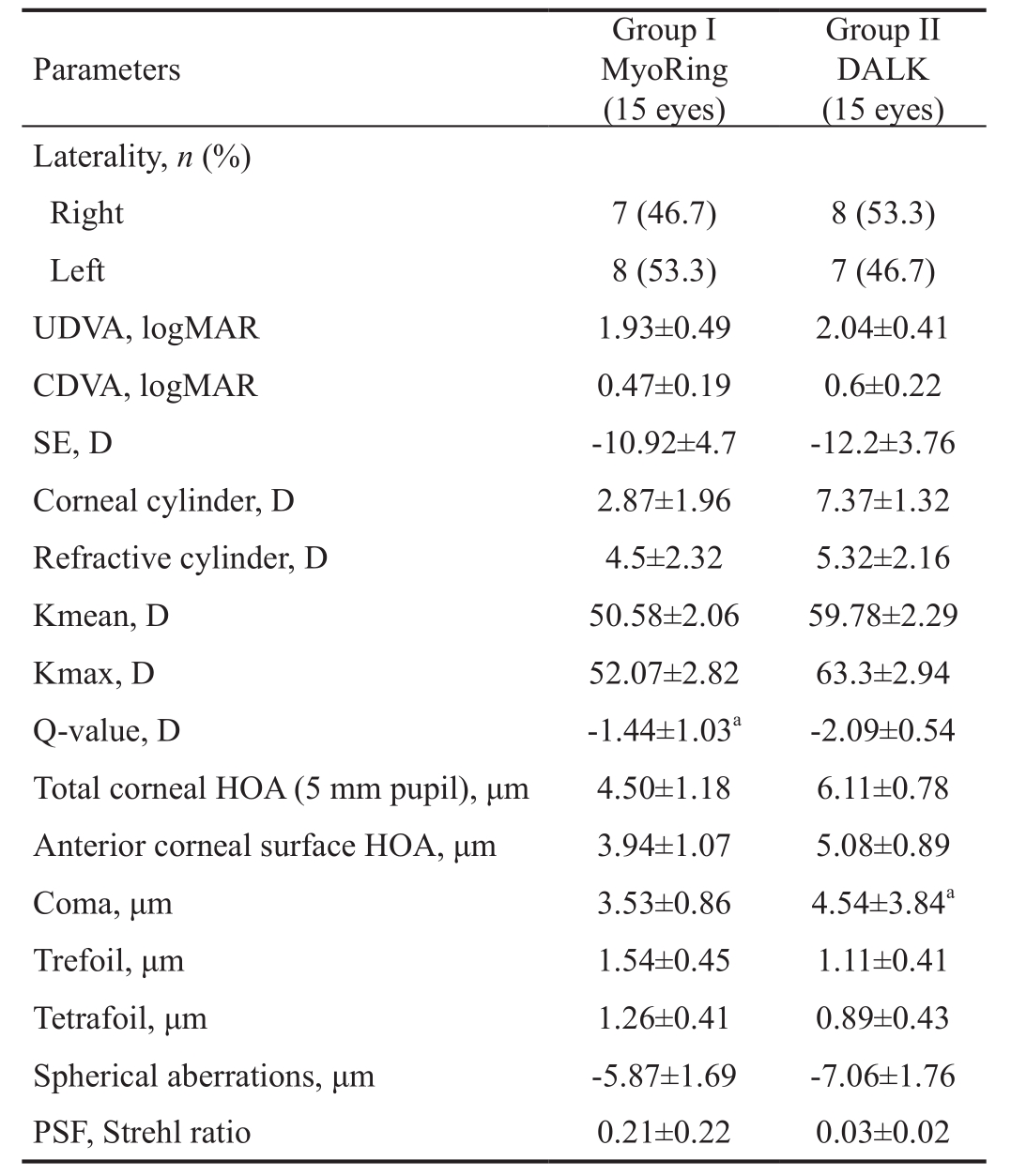
The study included 15 patients (30 eyes); four males (26.7%)and eleven females (73.3%). The median age of the study group was 25.0y (IQR: 8.0 at 95.0% confidence interval)ranging from 24.0 to 35.0y. The patients were bilaterally operated; one eye had MyoRing implantation (Group I)and the contralateral eye had DALK operation (Group II).The preoperative descriptive data of the two groups were demonstrated in Table 2.
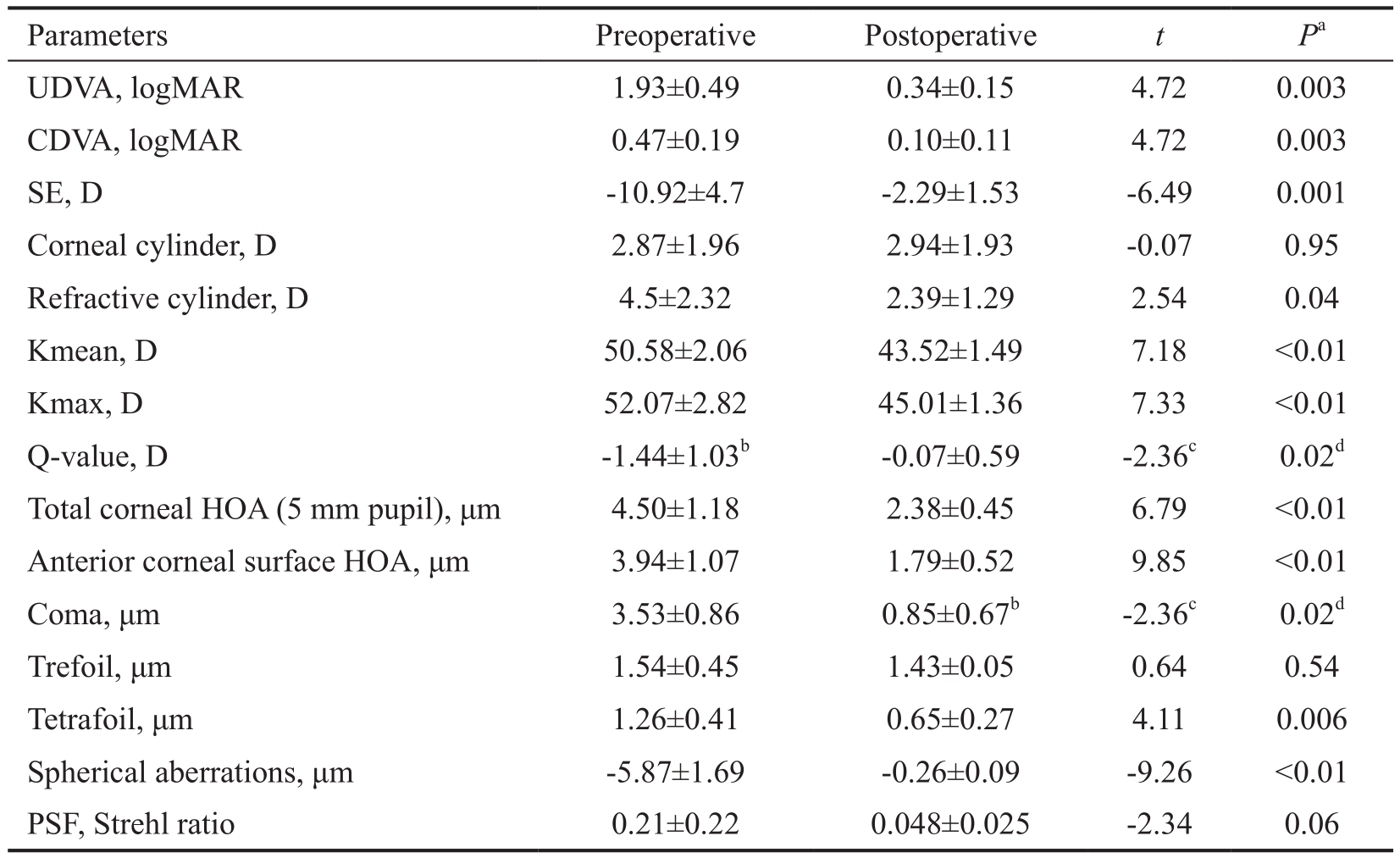
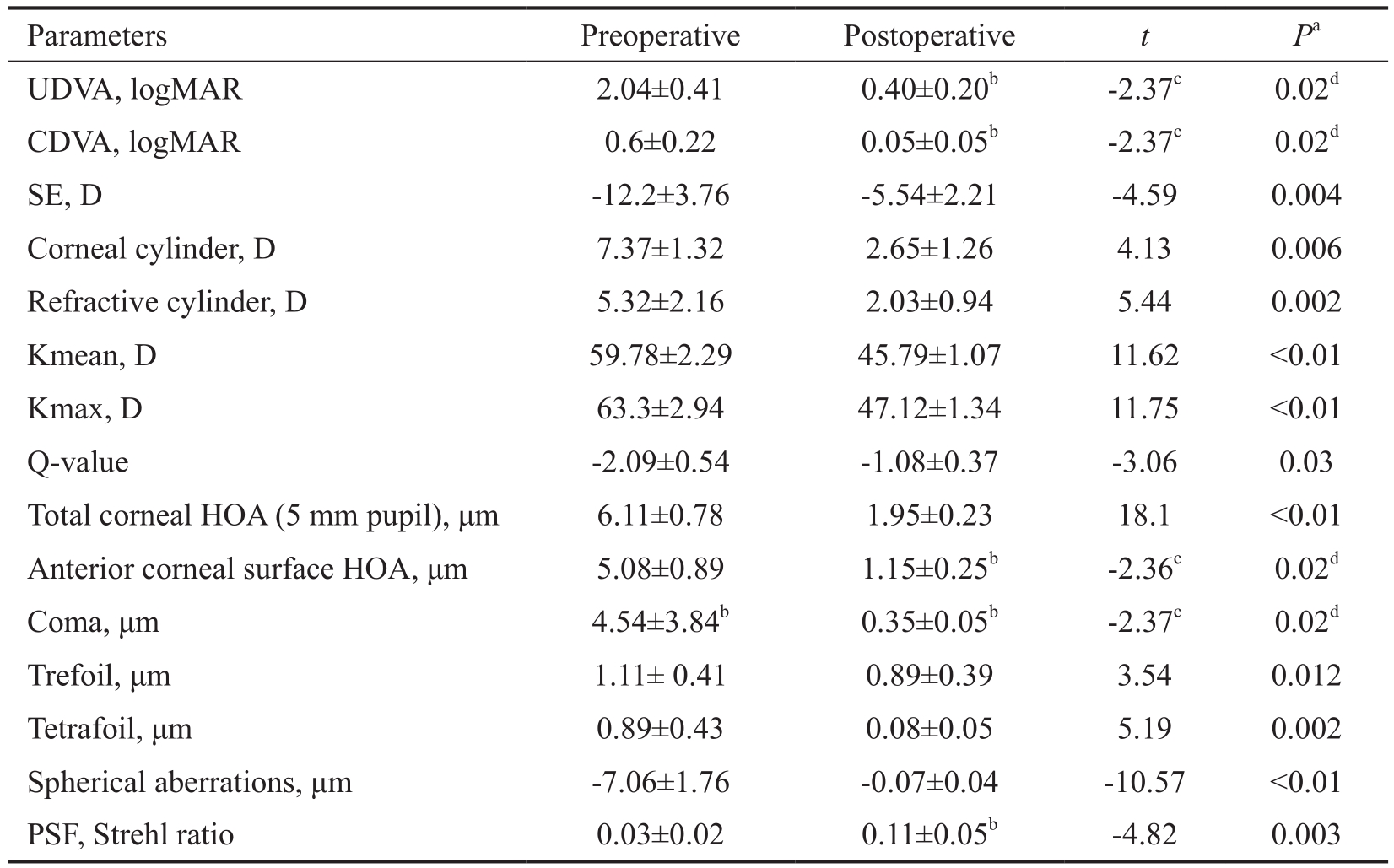
A statistically significant postoperative improvement in visual acuities, corneal astigmatism, refractive cylinders and corneal asphericity in both groups except the mean corneal cylinder, Trefoil RMS and PSF in Group I where there was no statistically significant difference between the preoperative and postoperative values (Tables 3, 4).
Results of Group IAll eyes were implanted with 6 mm MyoRing. Six months following surgery, mean UCVA was significantly improved (P=0.003) with a mean change of 1.59±0.48 D. Postoperative UCVA was better than 1.0 logMAR(20/200) in all eyes at the end of follow up. Mean CDVA was significantly improved (P=0.003) with a mean change of 0.37 logMAR ±0.21 SD. Postoperative CDVA was equal to or better than 0.2 logMAR (20/30) in all eyes at the end of follow up.Mean SE value was reduced significantly with a mean change of 8.64±3.52 D at the end of follow up (P=0.001). Mean corneal astigmatism show no statistically significant change(P=0.95) with a mean change of 1.77±1.75 D while mean refractive cylinder was significantly reduced (P=0.04) with a mean change of 2.39±1.82 D.
Mean Kmean was reduced significantly (P<0.01) with mean change of 7.2±2.32 D. Mean Kmax was reduced significantly from (P<0.01) with a mean change of 6.98±2.52 D. Corneal asphericity (Q-value) was changed significantly (P=0.02) with mean change of 0.59±0.86 SD. Significant improvement in corneal HOAs was observed following MyoRing implantation except in mean trefoil RMS and mean PSF (Strehl ratio)despite reduction of its value postoperatively (P>0.05; Table 3).
Results of Group IISix months following surgery, mean UCVA was significantly improved (P=0.02) with a mean change of 1.53±0.33 D. Postoperative UCVA was better than 1.0 logMAR (20/200) in 10 eyes (91%) at the end of follow up. Mean CDVA was significantly improved (P=0.02) with a mean change of 0.57±0.22 logMAR. Postoperative CDVA was equal to or better than 0.2 logMAR (20/30) in all eyes at the end of follow up.
Mean SE value was reduced significantly with a mean change of 6.67±3.84 D at the end of follow up (P=0.004). Mean corneal astigmatism show statistically significantly decreased(P=0.006) with a mean change of 4.71±3.01 D while mean refractive cylinder was significantly reduced (P=0.002) with a mean change of 3.29±1.59 D.
Mean Kmean was reduced significantly (P<0.01) with mean change of 13.9±3.19 D. Mean Kmax was reduced significantly from (P<0.01) with a mean change of 16.48±3.71 D. Corneal asphericity (Q-value) was changed significantly (P=0.03) with mean change of 0.97±0.87 D. Table 4 demonstrated significant reduction of all corneal aberrations postoperatively compared to preoperative values (P<0.05).
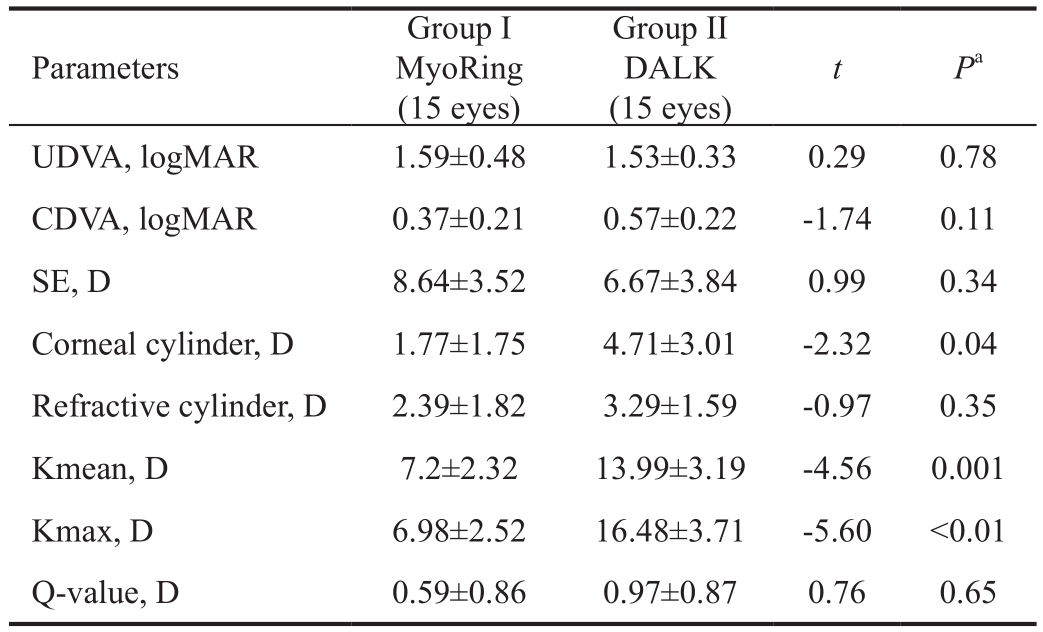
Comparison Between the Two GroupsTable 5 represented comparison between the two study groups regarding the mean postoperative data. There was no statistically significant difference between them (P>0.05) except in mean SE(P=0.008), Kmean (P=0.007) and mean Q-value (corneal asphericity,P=0.004). More significant improvement was found in Group I as regards these postoperative values compared to Group II.
Regarding the mean changes in the preoperative parameters following surgeries; there was no significant difference between both groups except in mean corneal cylinder, mean Kmax and, mean K where more significant reduction was obtained in Group II (P<0.05; Table 6).
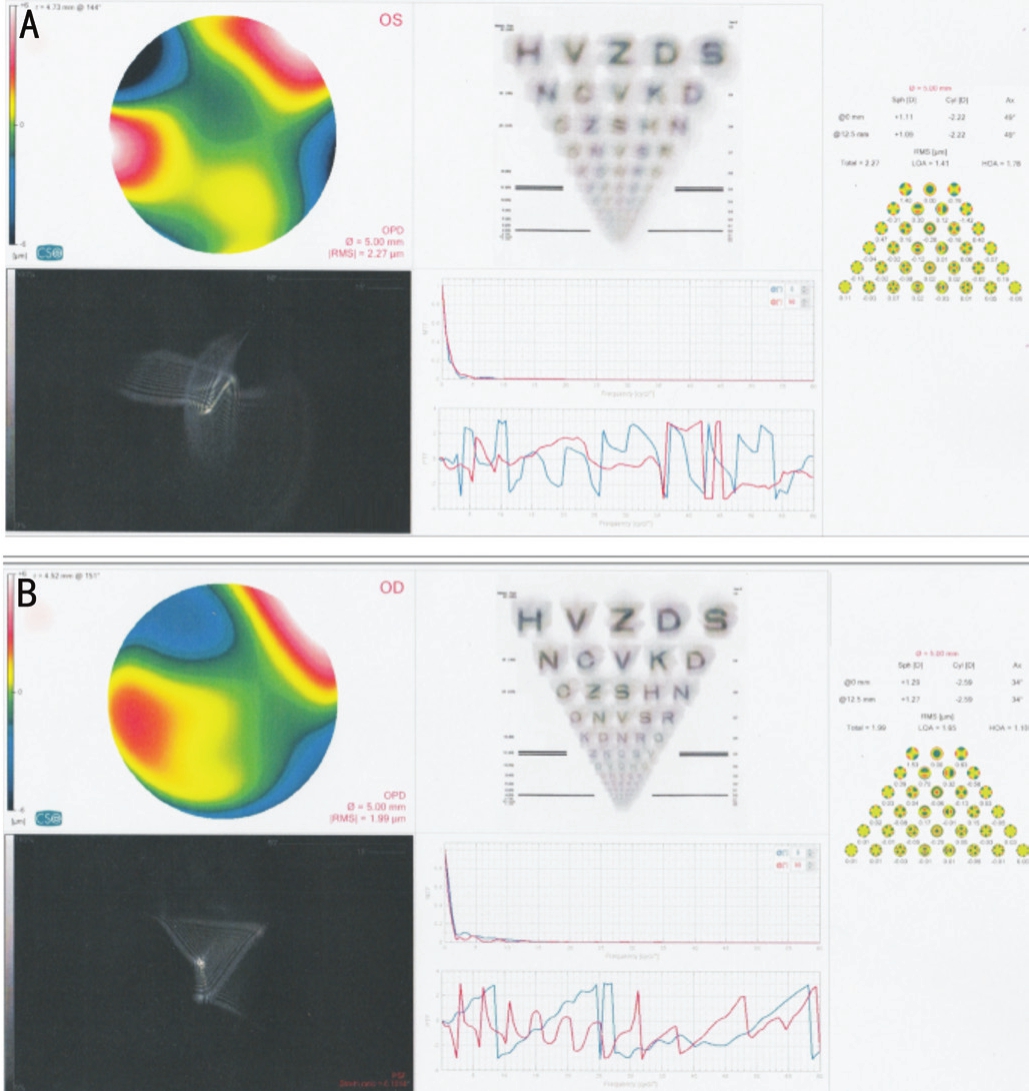
Assessment of corneal high order aberrations postoperatively revealed a statistically significant difference between Group Iand Group II in all aberrations with more homogenous anterior corneal surface following DALK operation as detected by statistically significant lower mean RMS in Group II (P=0.038)for anterior corneal surface and for total cornea compared to Group I (P=0.045). Mean PSF (Strehl ratio) was statistically higher in Group II compared to Group I (P=0.001) which indicated better quality of image and less glare following surgery in the DALK group (Table 5).
Table 2 Preoperative parameters in Group I and Group II mean±SD
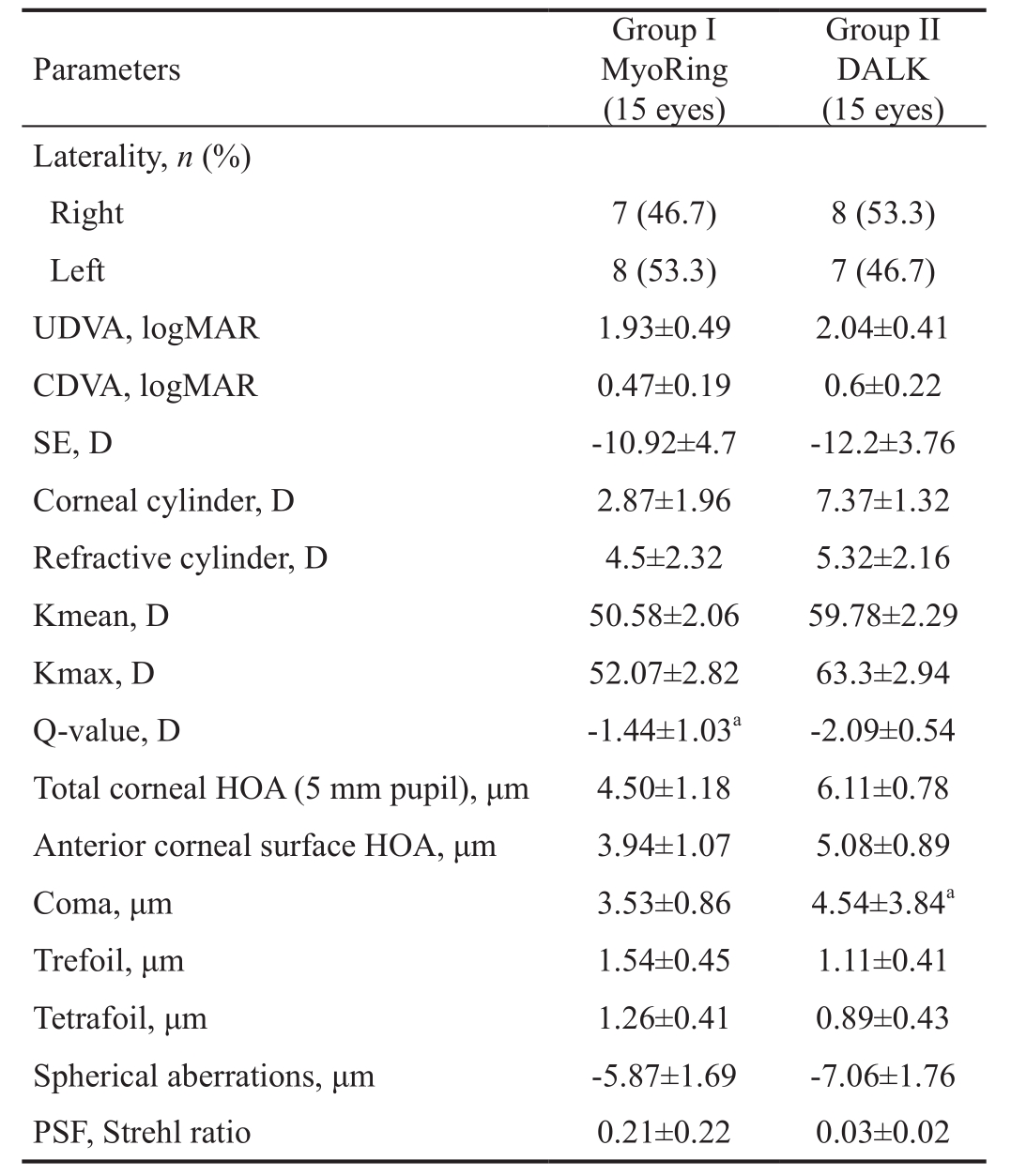
DALK: Deep anterior lamellar keratoplasty; UDVA: Uncorrected distance visual acuity; CDVA: Corrected distance visual acuity; SE:Spherical equivalent; HOA: High order aberration; PSF: Point spread function.aMedian±interquartile range.
Parameters Group I MyoRing(15 eyes)Group II DALK(15 eyes)Laterality,n(%)Right 7 (46.7) 8 (53.3)Left 8 (53.3) 7 (46.7)UDVA, logMAR 1.93±0.49 2.04±0.41 CDVA, logMAR 0.47±0.19 0.6±0.22 SE, D -10.92±4.7 -12.2±3.76 Corneal cylinder, D 2.87±1.96 7.37±1.32 Refractive cylinder, D 4.5±2.32 5.32±2.16 Kmean, D 50.58±2.06 59.78±2.29 Kmax, D 52.07±2.82 63.3±2.94 Q-value, D -1.44±1.03a-2.09±0.54 Total corneal HOA (5 mm pupil), μm 4.50±1.18 6.11±0.78 Anterior corneal surface HOA, μm 3.94±1.07 5.08±0.89 Coma, μm 3.53±0.86 4.54±3.84aTrefoil, μm 1.54±0.45 1.11±0.41 Tetrafoil, μm 1.26±0.41 0.89±0.43 Spherical aberrations, μm -5.87±1.69 -7.06±1.76 PSF, Strehl ratio 0.21±0.22 0.03±0.02
Figure 3A, 3B represented postoperative values of RMS and PSF at (5 mm pupil size) following MyoRing implantation(Group I) and DALK operation (Group II).
In Group I, a statistically significant negative correlation was found between the mean change in CDVA (logMAR) and the mean preoperative and mean postoperative total corneal aberrations RMS (r=-0.78,P=0.04). A statistically significant negative correlation was found between mean preoperativecoma RMS and mean post PSF (r=-0.86,P=0.01) and also between mean preoperative spherical aberrations RMS and mean change in mean K (r=-0.82,P=0.02). A statistically significant positive correlation was found between mean preoperative total corneal HOAs RMS and mean postoperative refractive cylinder (r=0.9,P=0.006).
Table 3 Comparison between preoperative and postoperative parameters in Group I mean±SD
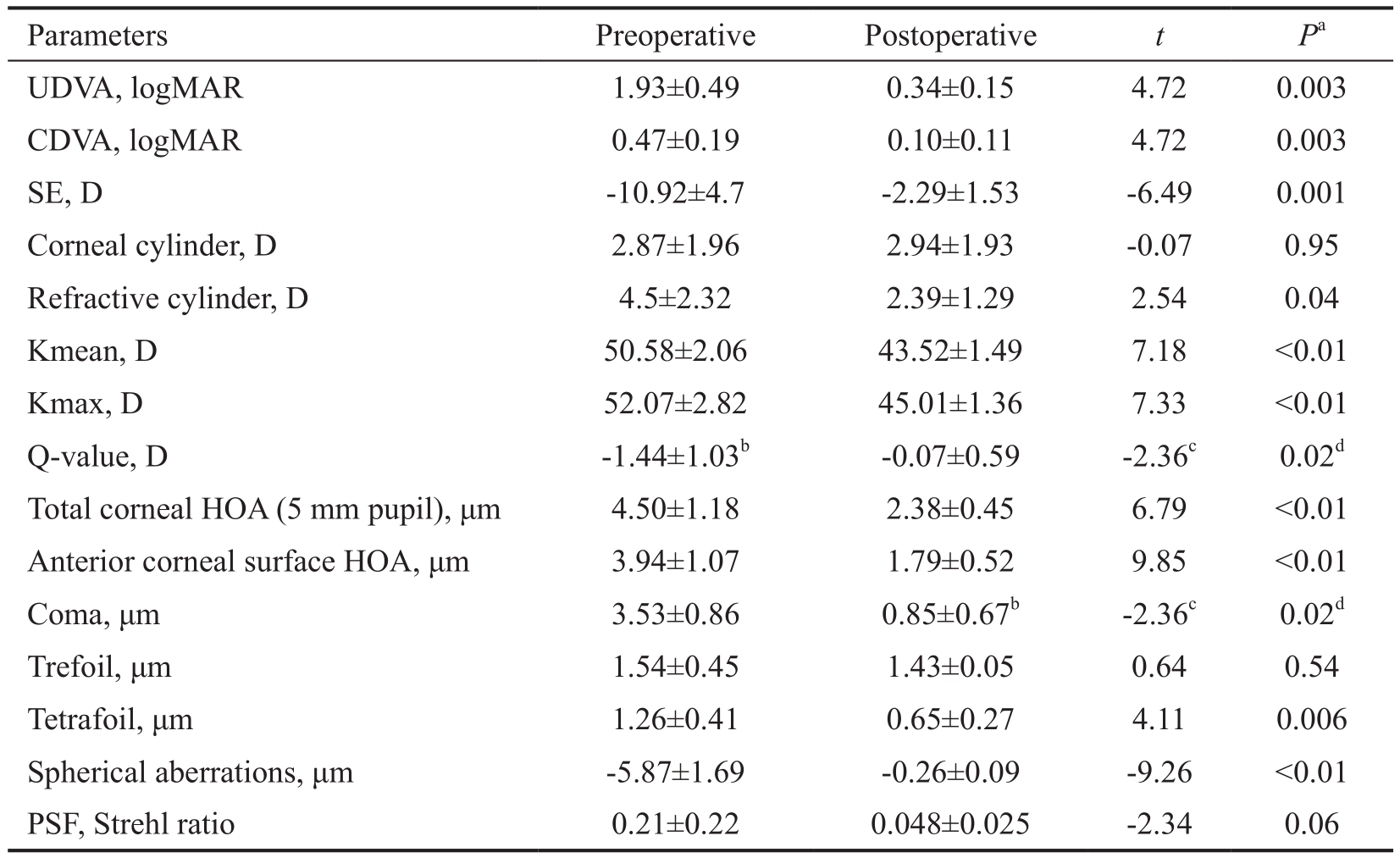
UDVA: Uncorrected distance visual acuity; CDVA: Corrected distance visual acuity; SE: Spherical equivalent;PSF: Point spread function.aComparison using paired sample Student’st-test;bMedian and interquartile range;cZ-value;dComparison using Wilcoxon test;P<0.05 was statistically significant.
Parameters Preoperative PostoperativetPaUDVA, logMAR 1.93±0.49 0.34±0.15 4.72 0.003 CDVA, logMAR 0.47±0.19 0.10±0.11 4.72 0.003 SE, D -10.92±4.7 -2.29±1.53 -6.49 0.001 Corneal cylinder, D 2.87±1.96 2.94±1.93 -0.07 0.95 Refractive cylinder, D 4.5±2.32 2.39±1.29 2.54 0.04 Kmean, D 50.58±2.06 43.52±1.49 7.18 <0.01 Kmax, D 52.07±2.82 45.01±1.36 7.33 <0.01 Q-value, D -1.44±1.03b-0.07±0.59 -2.36c0.02dTotal corneal HOA (5 mm pupil), μm 4.50±1.18 2.38±0.45 6.79 <0.01 Anterior corneal surface HOA, μm 3.94±1.07 1.79±0.52 9.85 <0.01 Coma, μm 3.53±0.86 0.85±0.67b-2.36c0.02dTrefoil, μm 1.54±0.45 1.43±0.05 0.64 0.54 Tetrafoil, μm 1.26±0.41 0.65±0.27 4.11 0.006 Spherical aberrations, μm -5.87±1.69 -0.26±0.09 -9.26 <0.01 PSF, Strehl ratio 0.21±0.22 0.048±0.025 -2.34 0.06
Table 4 Comparison between preoperative and postoperative parameters in Group II mean±SD
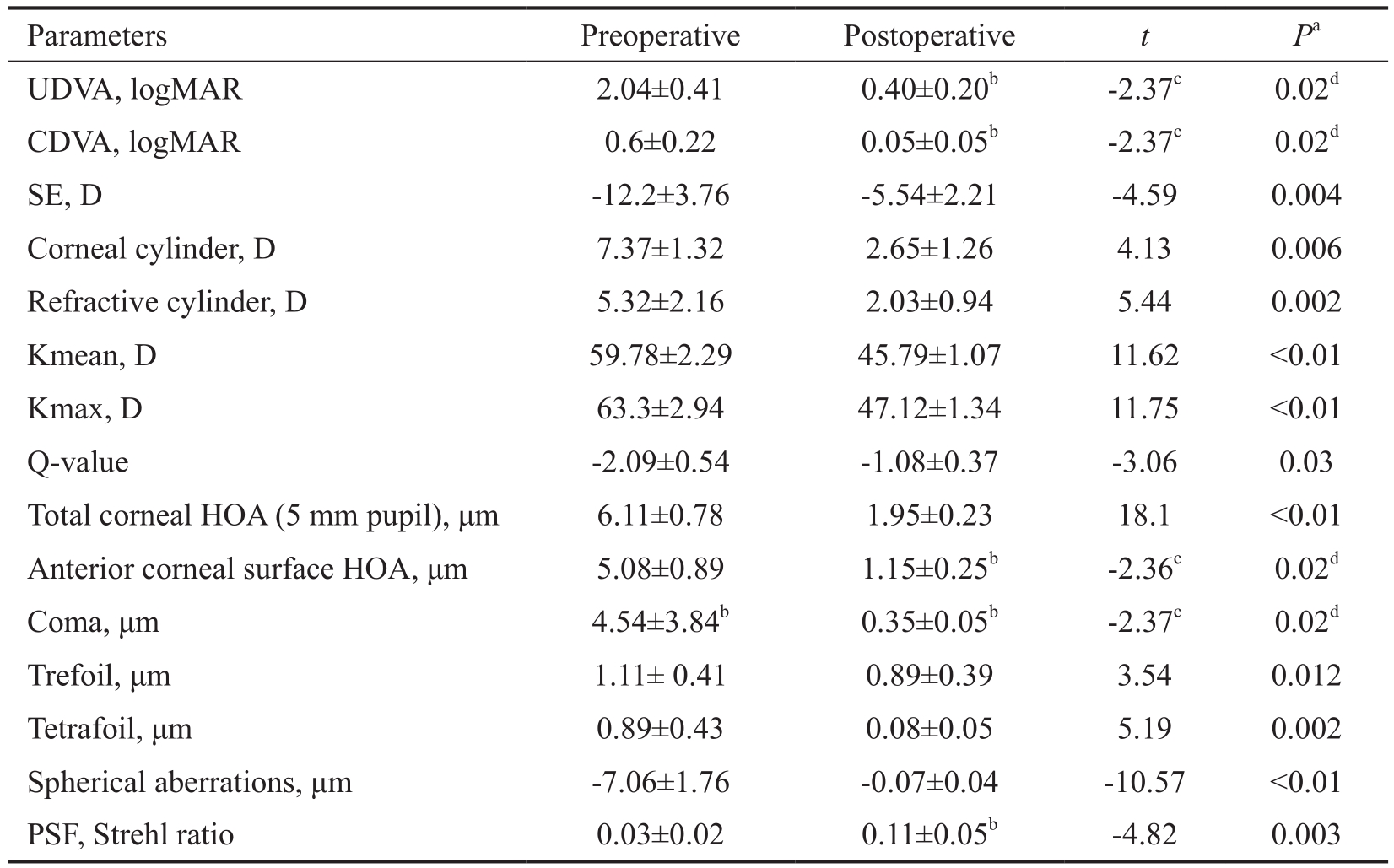
UDVA: Uncorrected distance visual acuity; CDVA: Corrected distance visual acuity; SE: Spherical equivalent;PSF: Point spread function.aComparison using paired sample Student’st-test;bMedian and interquartile range;cZ-value;dComparison using Wilcoxon test;P<0.05 was statistically significant.
Parameters Preoperative PostoperativetPaUDVA, logMAR 2.04±0.41 0.40±0.20b-2.37c0.02dCDVA, logMAR 0.6±0.22 0.05±0.05b-2.37c0.02dSE, D -12.2±3.76 -5.54±2.21 -4.59 0.004 Corneal cylinder, D 7.37±1.32 2.65±1.26 4.13 0.006 Refractive cylinder, D 5.32±2.16 2.03±0.94 5.44 0.002 Kmean, D 59.78±2.29 45.79±1.07 11.62 <0.01 Kmax, D 63.3±2.94 47.12±1.34 11.75 <0.01 Q-value -2.09±0.54 -1.08±0.37 -3.06 0.03 Total corneal HOA (5 mm pupil), μm 6.11±0.78 1.95±0.23 18.1 <0.01 Anterior corneal surface HOA, μm 5.08±0.89 1.15±0.25b-2.36c0.02dComa, μm 4.54±3.84b0.35±0.05b-2.37c0.02dTrefoil, μm 1.11± 0.41 0.89±0.39 3.54 0.012 Tetrafoil, μm 0.89±0.43 0.08±0.05 5.19 0.002 Spherical aberrations, μm -7.06±1.76 -0.07±0.04 -10.57 <0.01 PSF, Strehl ratio 0.03±0.02 0.11±0.05b-4.82 0.003
Table 5 Comparison between Group I and Group II as regards the mean postoperative parameters mean±SD

UDVA: Uncorrected distance visual acuity; CDVA: Corrected distance visual acuity; SE: Spherical equivalent; HOA: High order aberration; PSF: Point spread function.aComparison using independent sample Student’st-test;bMedian and interquartile range;cZ-value;dComparison using Mann-WhitneyUtest;P<0.05 was statistically significant.
Parameters Group I MyoRing (15 eyes) Group II DALK (15 eyes)tPaUDVA, logMAR 0.34±0.15 0.40±0.20b-0.98c0.38dCDVA, logMAR 0.1±0.11 0.05±0.05b-1.43c0.15dSE, D -2.29±1.53 -5.54±2.21 3.19 0.008 Corneal cylinder, D 2.94±1.93 2.65±1.26 0.32 0.75 Refractive cylinder, D 2.39±1.29 2.03±0.94 0.59 0.56 Kmean, D 43.52±1.49 45.79±1.07 -3.26 0.007 Kmax, D 45.01±1.36 47.12±1.34 -2.82 0.15 Q-value, D -0.07±0.59 -1.08±0.37 3.57 0.004 Total corneal HOA (5 mm pupil), μm 2.38±0.45 1.95±0.23 2.24 0.045 Anterior corneal surface HOA, μm 1.79±0.52 1.15±0.25b-2.11c0.038dComa, μm 0.85±0.67b0.35±0.05b-1.59c0.013dTrefoil, μm 1.43±0.05 0.89±0.39 3.67 0.003 Tetrafoil, μm 0.65±0.27 0.08±0.05 5.45 <0.01 Spherical aberrations (μm) -0.26 ±0.09 -0.07±0.04 -5.03 <0.01 PSF (Strehl ratio) 0.048±0.025 0.11±0.05b-3.07c0.001d
Table 6 Changes in visual acuities, refraction, topography and asphericity in each study group mean±SD
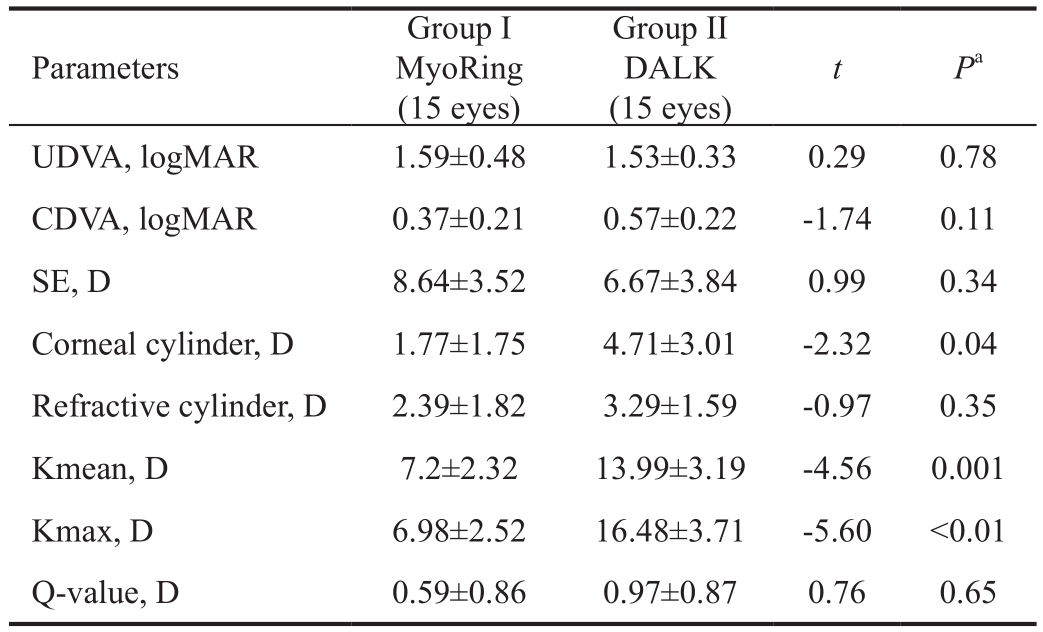
DALK: Deep anterior lamellar keratoplasty; UDVA: Uncorrected distance visual acuity; CDVA: Corrected distance visual acuity;SE: Spherical equivalent.aComparison using independent sample Student’st-test;P<0.05 was statistically significant.
Parameters Group I MyoRing(15 eyes)Group II DALK(15 eyes)tPaUDVA, logMAR 1.59±0.48 1.53±0.33 0.29 0.78 CDVA, logMAR 0.37±0.21 0.57±0.22 -1.74 0.11 SE, D 8.64±3.52 6.67±3.84 0.99 0.34 Corneal cylinder, D 1.77±1.75 4.71±3.01 -2.32 0.04 Refractive cylinder, D 2.39±1.82 3.29±1.59 -0.97 0.35 Kmean, D 7.2±2.32 13.99±3.19 -4.56 0.001 Kmax, D 6.98±2.52 16.48±3.71 -5.60 <0.01 Q-value, D 0.59±0.86 0.97±0.87 0.76 0.65
In Group II, there was a statistically significant positive correlation between mean postoperative CDVA (logMAR)and each of mean postoperative corneal cylinder, refractive cylinder and total corneal aberrations RMS (r=0.95,P=0.001,r=0.93,P=0.002,r=0.81,P=0.03) respectively and significant negative correlation between postoperative mean CDVA(logMAR) and mean spherical aberrations RMS (r=0.81,P=0.03). Also in Group II, there was a statistically significant positive correlation between mean change in CDVA (logMAR)and mean change in Kmax (r=0.87,P=0.01) and between mean change in refractive cylinder and mean postoperative PSF(r=0.76,P=0.05) and significant negative correlation between mean change in refractive cylinder and mean postoperative spherical aberration RMS (r=-0.82,P=0.03).
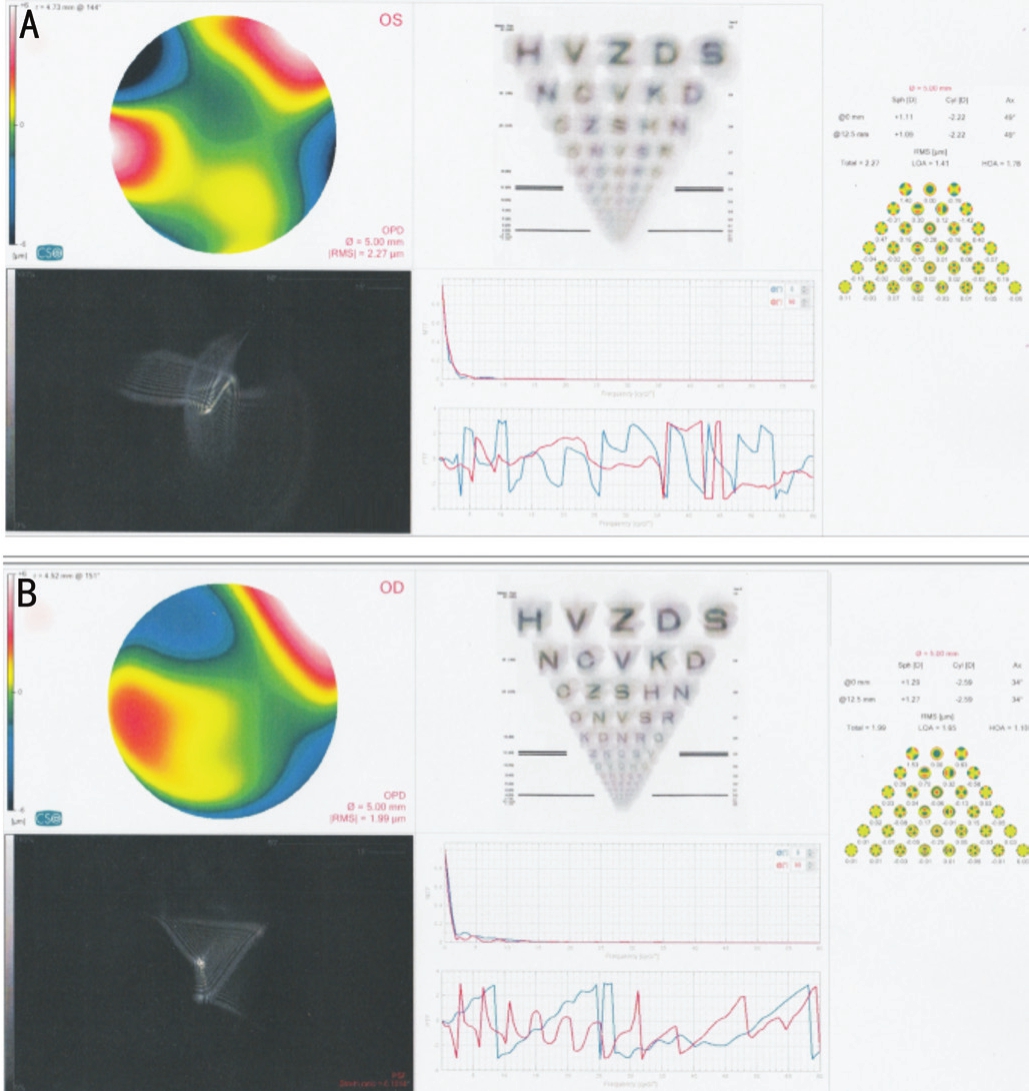
Figure 3 Postoperative values of RMS and PSF at (5 mm pupil size) of one of our patients
A: Left eye after MyoRing implantation,the corneal RMS was 2.27 μm and PSF was 0.072; B: Right eye after DALK, the corneal RMS was 1.99 μm and PSF was 0.10.
DISCUSSION
Keratoplasty is still regarded as a definitive approach in the treatment of keratoconus so it might be interesting to compare the results of MyoRing with data acquired from lamellar keratoplasty.
In the present study, 6mo following femtosecond assisted MyoRing implantation, significant improvement in mean UCVA, CDVA, refractive cylinder, SE, keratometry readings and, corneal asphericity (Q-value) was demonstrated.However, no significant change in corneal astigmatism was obtained for moderate to advanced cases of keratoconus.Satisfactory improvements in visual acuities, refraction and keratometry readings following femtosecond assisted MyoRing implantation were similar to previous studies[9,18,21].The status of preoperative visual acuity, refraction and the severity of keratoconus can affect the results of the operation[18].Jabbarvandet al[8]and Nasrollahiet al[22]concluded that MyoRing implantation in keratoconus improved both UDVA and CDVA significantly. It also reduced spherical power of the cornea and keratometry significantly, especially in advanced cases. Furthermore, it reduced corneal astigmatism, but not as much as spherical errors[8]. The reason for the apparent changes in the refraction and visual acuity of keratoconus patients could be the changes in the corneal surface due to the arcshortening effect of MyoRing implantation, especially during the early weeks after the operation[9,12,18]. Alioet al[12]reported a non-significant increase in CDVA after 5 mm MyoRing implantation. It was believed that poor results in their study may have been caused by small ring size in proportion to the patient’s pupil[8]. Cone position seems to affect the impact of the MyoRing on the corneal curvature. The maximum diameter of the MyoRing is 6 mm and protrusions beyond this point cannot be corrected. It was found that 5 mm rings and max K in the central 8 mm zone in the non central cone group increased. This was while max K in the central 3 mm zone showed a similar decrease in both cone groups[18].
Significant improvement in mean UCVA, CDVA, corneal and refractive cylinders, SE, and keratometry readings after femtosecond assisted DALK operation was documented.More oblate corneal surface was achieved postoperatively.This approach is a safe and effective surgical choice in the treatment of keratoconus and post-LASIK keratectasia[23].It could improve UCVA and BCVA in patients with anterior corneal pathology[24]and provides stable long-term visual and refractive outcomes with minimal complications compared to standard PK[25]. Faster wound healing is related to a better donor-recipient fit with the increased surface area of contacts with subsequent acceleration of suture removal[26].
Comparing the postoperative outcomes, no statistically significant difference between both groups in all measured parameters except in mean SE, K and mean corneal asphericity.
The postoperative values were lower in Group I. This might be due to inclusion of more advanced keratoconus cases in Group II compared to Group I. Despite that, the changes (between preoperative and postoperative values) in mean corneal astigmatism and keratometry readings obtained by DALK operation were significantly higher (64% improvement in corneal cylinder and 23.4 % reduction in mean K respectively)compared to MyoRing group (61.6% and 14.2%). Mean RMSs for corneal HOAs were significantly lower in DALK group postoperatively compared to MyoRing group indicating that the former group had more homogenous surface, also the mean PSF (Strehl ratio) was statistically significant higher in DALK group indicating better image quality compared to MyoRing group.
Postoperative visual quality following DALK is affected by presence of the residual stromal bed. A smoother optical interface resulted in less optical aberration[15]. Considerable light scatter at the interface may be the cause of poor optical quality of the eye[27]. In contrary, it was postulated that the thinnest layer left is expected to be optically negligible and at the same time leaves a protection to DM, lowering the rate of perforation. It is expected that this level is just above the recently described Dua’s layer[17]. Previous studies reported reduction of coma and HOAs after ring segment implantation in keratoconus[8,11,28]. In contrary, a study[12]found no significant changes were present in both after MyoRing implantation and considered these results due to the following reasons;small sample size, pupil was not considered as an inclusion criterion and small optical zone of MyoRing implanted in their study and the different methods for assessment of aberrations and the measurement of total aberrations. The same study[12]and another one[8]reported increased postoperative spherical aberrations after MyoRing implantation (changed from a mean preoperative negative value to a large mean postoperative positive value). They expected this occurred due to flattening of the central part of the cornea and changing the shape of the cornea from prolate to oblate and small size or ring used with significant impact on corneal asphericity[9]. This was not comparable to the present result (preoperative mean negative value became less negative postoperatively) which might be attributed to larger ring diameter used in all eyes. It was believed that larger diameters have the least impact on corneal asphericity and, selecting cases with small pupil size was important to minimize glare induced by MyoRing[12].
The present result found no statistically significant change in mean trefoil RMS following MyoRing implantation with significant decrease in coma. This was comparable to the results of Jabbarvandet al[9]. Inter-subject variability in the optical response to intracorneal ring segments may be due to differences in the corneal biomechanical properties across patients, and from the difficulty to control at the same timethe topographic and refractive outcomes[14]. Significant correlations between mean change in CDVA and each of mean HOAs and mean PSF were found in both study groups. This supports the value of aberration measurements in predicting visual performance. This was comparable to previous studies on normal subjects[29]and following intracorneal ring segments implantation[14]. The current work represents our experience in management of moderate and severe keratoconus using femtosecond assisted MyoRing implantation and femtosecond assisted DALK reporting the efficacy of the two techniques in improvement of corneal parameters and visual outcomes.The study shows that both techniques were effective with more improvement of corneal asphericity and aberrations after DALK. Thus we recommend the idea of use of DALK even for moderate cases of keratoconus for which intracorneal rings are still an option. Relatively small number of cases and lack of randomization were the limitations of our study. Further studies on higher number of cases are needed to compare the efficacy of both techniques in moderate cases.
In conclusion, MyoRing implantation in keratoconus is an acceptable substitute for PK in advanced cases. DALK is another good alternative treatment option, both techniques providing comparable results to PK in terms of visual acuity, refraction and HOAs. Femtosecond assisted MyoRing implantation and DALK (big bubble technique with DM bearing)are effective in improving UCVA and CDVA. MyoRing reduced spherical error more than the corneal cylinder. Post operative homogenous corneal surface and good image quality were achieved following both techniques compared to the preoperative state. However, DALK results in better image quality and less corneal aberrations.
ACKNOWLEDGEMENTS
Conflicts of Interest:Yousif MO, None; Said AMA, None.
REFERENCES
1 Pajic B, Ljubic J, Muller J. Lamellar keratoplasty for keratoconus. In:Garg A, Alio JL, eds,Surgical techniques in Ophthalmology (corneal surgery), 1stedition, Ch. (8), New Delhi, India, Jaypee Brothers Medical Publishers, 2010:45-48.
2 Fukuoka S, Honda N, Ono K, Mimura T, Usui T, Amano S. Extended long-term results of penetrating keratoplasty for keratoconus.Cornea2010;29(5):528-530.
3 Athanasiadis I, Busin M. Anterior lamellar keratoplasty for Keratoconus in: Barbara A, edt, Textbook on Keratoconus New Insights, 1stedition, Ch.(18), New Delhi, India, Jaypee Brothers Medical Publishers, 2012:187-201.
4 Reinhart WJ, Musch DC, Jacobs DS, Lee WB, Kaufman SC, Shtein RM. Deep anterior lamellar keratoplasty as an alternative to penetrating keratoplasty a report by the American Academy of Ophthalmology.Ophthalmology2011;118(1):209-218.
5 Maharana PK, Agarwal K, Jhanji V, Vajpayee RB. Deep anterior lamellar keratoplasty for keratoconus: a review.Eye Contact Lens2014;40(6):382-389.
6 Jadidi K, Nejat F, Mosavi SA, Naderi M, Katiraee A, Janani l,Aghamollaei H. Full-ring intrastromal corneal implantation for correcting high myopia in patients with severe keratoconus.Med Hypothesis Discov Innov Ophthalmol2016;5(3):89-95.
7 Patel S, Marshall J, Fitzke FW 3rd. Model for deriving the optical performance of the myopic eye corrected with an intracorneal ring.J Refract Surg1995;11(4):248-252.
8 Jabbarvand M, Salamatrad A, Hashemian H, Khodaparast M.Continuous corneal intrastromal ring implantation for treatment of keratoconus in an Iranian population.Am J Ophthalmol2013;155(5):837-842.
9 Jabbarvand M, Salamatrad A, Hashemian H, Mazloumi M, Khodaparast M. Continuous intracorneal ring implantation for keratoconus using a femtosecond laser.J Cataract Refract Surg2013;39(7):1081-1087.
10 Janani L, Jadidi K, Mosavi SA, Nejat F, Naderi M, Nourijelyani K.MyoRing implantation in keratoconic patients: 3 years follow-up data.J Ophthalmic Vis Res2016;11(1):26-31.
11 Piñero DP, Alio JL, El Kady B, Coskunseven E, Morbelli H, Uceda-Montanes A, Maldonado MJ, Cuevas D, Pascual I. Refractive and aberrometric outcomes of intracorneal ring segments for keratoconus:mechanical versus femtosecond-assisted procedures.Ophthalmology2009;116(9):1675-1687.
12 Alio JL, Piñero DP, Daxer A. Clinical outcomes after complete ring implantation in corneal ectasia using the femtosecond technology: a pilot study.Ophthalmology2011;118(7):1282-1290.
13 Shehadeh-Mashor R, Chan CC, Bahar I, Lichtinger A, Yeung SN,Rootman DS. Comparison between femtosecond laser mushroom configuration and manual trephine straight-edge configuration deep anterior lamellar keratoplasty.Br J Ophthalmol2014;98(1):35-39.
14 Pérez-Merino P, Ortiz S, Alejandre N, de Castro A, Jiménez-Alfaro I, Marcos S. Ocular and optical coherence tomography-based corneal aberrometry in keratoconic eyes treated by intracorneal ring segments.Am J Ophthalmol2014;157(1):116-127.el.
15 Javadi MA, Feizi S, Yazdani S, Mirbabaee F. Deep anterior lamellar keratoplasty versus penetrating keratoplasty for keratoconus: a clinical trial.Cornea2010;29(4):365-371.
16 Mashor RS, Rootman DB, Bahar I, Singal N, Slomovic AR, Rootman DS. Outcomes of deep anterior lamellar keratoplasty versus intralase enabled penetrating keratoplasty in keratoconus.Can J Ophthalmol2011;46(5):403-407.
17 Hamdi IM, Hamdi MM. Quality of vision after deep anterior lamellar keratoplasty (fluid dissection) compared to penetrating keratoplasty for the treatment of keratoconus.J Ophthalmol2017;2017:4507989.
18 Mohebbi M, Hashemi H, Asgari S, Bigdeli S, Zamani KA. Visual outcomes after femtosecond-assisted intracorneal MyoRing implantation:18 months of follow-up.Graefes Arch Clin Exp Ophthalmol2016;254(5):917-922.
19 Zadnik K, Barr JT, Edrington TB, Everett DF, Jameson M, McMahon TT, Shin JA, Sterling JL, Wagner H, Gordon MO. Baseline findings in collaborative longitudinal evaluation of keratoconus (CLEK) study.Invest Ophthalmol Vis Sci1998;39(13):2537-2546.
20 Chatzis N, Hafezi F. Progression of keratoconus and efficacy of pediatric [corrected] corneal collagen cross-linking in children and adolescents.J Refract Surg2012;28(11):753-758.
21 Daxer A, Mahmoud H, Venkateswaran RS. Intracorneal continuous ring implantation for keratoconus: one-year follow-up.J Cataract Refract Surg2010;36(8):1296-1302.
22 Nasrollahi K, Rezaei L, Ghoreishi M, Kashfi A, Mahboubi M. Clinical outcomes of MyoRing implantation in keratoconic eyes by using the Femtosecond laser technology.J Med Life2015;8(Spec Iss 3):66-71.
23 Lu Y, Shi YH, Yang LP, Ge YR, Chen XF, Wu Y, Huang ZP.Femtosecond laser-assisted deep anterior lamellar keratoplasty for keratoconus and keratectasia.Int J Ophthalmol2014;7(4):638-643.
24 Lu Y, Chen X, Yang L, Xue C, Huang Z. Femtosecond laser-assisted deep anterior lamellar keratoplasty with big-bubble technique for keratoconus.Indian J Ophthalmol2016;64(9):639-642.
25 Romano V, Iovieno A, Parente G, Soldani AM, Fontana L. Long-term clinical outcomes of deep anterior lamellar keratoplasty in patients with keratoconus.Am J Ophthalmol2015;159(3):505-511.
26 Alio JL, Abdelghany AA, Barraquer R, Hammouda LM, Sabry AM.Femtosecond laser assisted deep anterior lamellar keratoplasty outcomes and healing patterns compared to manual technique.BioMed Res Int2015;2015:1-6.
27 Chamberlain W, Omid N, Lin A, Farid M, Gaster RN, Steinert RF.Comparison of corneal surface higher-order aberrations after endothelial keratoplasty, femtosecond laser-assisted keratoplasty, and conventional penetrating keratoplasty.Cornea2012;31(1):6-13.
28 Shabayek MH, Alió JL. Intrastromal corneal ring segment implantation by femtosecond laser for keratoconus correction.Ophthalmology2007;114(9):1643-1652.
29 Cheng X, Bradley A, Thibos LN. Predicting subjective judgment of best focus with objective image quality metrics.J Vis2004;4(4):310-321.
Citation:Yousif MO, Said AMA. Contralateral eye study of refractive, topographic and aberrometric outcomes after femtosecond assisted MyoRing implantation and DALK for management of keratoconus.Int J Ophthalmol2018;11(10):1621-1630
DOl:10.18240/ijo.2018.10.08
Accepted:2018-07-12
Received:2018-03-09
Correspondence to:Azza Mohamed Ahmed Said. Department of Ophthalmology, Faculty of Medicine, Ain Shams University,10thFawzy Elmoteay street, Heliopolis, Cairo 11736, Egypt.dr_azza_22@hotmail.com