·Investigation·
Validation of the Glaucoma Quality of Life-15 Questionnaire in Serbian language
Ivan Sencanic1, Tatjana Gazibara2, Jelena Dotlic3, Miroslav Stamenkovic1,4, Vesna Jaksic1,3, Marija Bozic3,5,Anita Grgurevic2
1Clinic for Eye Disease “Prof. dr Ivan Stankovic”, University Medical Center “Zvezdara”, Belgrade 11050, Serbia
2Institute of Epidemiology, Faculty of Medicine, University of Belgrade, Belgrade 11129, Serbia
3Faculty of Medicine, University of Belgrade, Belgrade 11129,Serbia
4Faculty of Special Education and Rehabilitation, University of Belgrade, Belgrade 11000, Serbia
5Clinic for Eye Disease “Prof. dr Djordje Nesic”, Clinical Center of Serbia, Belgrade 11129, Serbia
Abstract
●AlM:To translate the Glaucoma Quality of Life-15(GQL-15) to Serbian language and asses its validity and reliability in the population of Serbian patients.
●METHODS:The study included 177 glaucoma patients.Clinical parameters (visual acuity, mean defect and square root of loss variance of visual field) and socio-demographic data were collected. Patients were stratified according to the Nelson’s glaucoma staging system as mild, moderate and advanced glaucoma. All patients filled out the GQL-15 and National Eye lnstitute Visual Function Questionnaire(NEl-VFQ 25). The GQL-15 was translated following the internationally-accepted methodology, and its psychometric properties were assessed by using classical test theory and Rasch analysis.
●RESULTS:The mean total score for the GQL-15 was 20.68±7.31. The Cronbach’s alpha coefficient for the whole scale was 0.89 (central and near vision, α=0.24; peripheral vision, α=0.85; glare and dark adaptation, α=0.83). Factor analysis established 4 factors (70.3% of variance): two corresponding to the original factors and two new factors specific for the Serbian population. The GQL-15 score correlated positively with almost all clinical parameters and NEl-VFQ 25 proving good criterion validity. Correlation of the GQL-15 total score on test-retest confirmed appropriate scale reproducibility (ρ=0.96,P<0.001). The GQL-15 discriminated well advanced from mild and moderate glaucoma. ln Rasch analysis we obtained adequate item(0.95) reliability index. Almost all items had infit and outfit mean squares in the accepted range.
●CONCLUSlON:Serbian version of the GQL-15 demonstrates adequate reliability and validity. This version of the GQL-15 is a valid instrument for evaluation of quality of life among Serbian speaking patients with glaucoma and can be applied in daily clinical work.
●KEYWORDS:glaucoma; GQL-15; scale validation; Serbian
INTRODUCTION
Glaucoma is a chronic optic neuropathy, resulting in irreversible loss of the visual field and it is the second leading cause of irreversible blindness worldwide[1-2].
Progressive loss of peripheral vision in glaucoma is associated with difficulties in day-to-day activities that include independent navigation, reading, drivingetc[3]. While clinical measurements fail to fully describe activity limitations of glaucoma patents, self-reported visual disability questionnaires tend to assess the actual impact of the disease on patients’functioning and their quality of life (QOL)[4-7].
The Glaucoma Quality of Life-15 (GQL-15) is a glaucomaspecific questionnaire designed in the early 2000s that is brief, concise and easy to administer. Available literature data confirmed good validity and reliability, showing that GQL-15 correlates strongly with visual field loss and other psychophysical measures of visual function (contrast sensitivity, glare disability, dark adaptation, stereopsis)[8]. Thus far, the GQL-15 has been translated to German[9-10]and Chinese[11]languages and it was also applied in English language in Nigerian[12], Indian[13],Singaporean[14]and Australian[15]populations.
Currently, there is a lack of information on the impact of glaucoma on QOL in Serbian population. Therefore, translation of the GQL-15 to Serbian language would provide important information related to the most important factors associated with QOL of glaucoma patients in this population. The aim of this study was to translate the Glaucoma Quality of Life-15 to Serbian language and asses its validity and reliability in the population of Serbian glaucoma patients.
SUBJECTS AND METHODS
PatientsAll consecutive glaucoma patients who came for regular check-up between August 2015 and September 2016 at the Clinic for Eye Disease University Medical Center“Zvezdara” in Belgrade, the capital of the Republic of Serbia,were recruited for the study.
Eligible participants for the study were 18 years or older Serbian speaking patients with glaucoma diagnosed more than one year prior to enrollment. Glaucoma was defined as presence of glaucomatous disc cupping associated with reproducible visual field loss in one or both eyes. Consequently,patients with primary open angle glaucoma (POAG), primary angle-closure glaucoma (PACG), normal tension glaucoma(NTG), pseudo-exfoliative (PEX) and pigmentary glaucoma(PG) were included in this study.
As the exclusion criteria we considered severe vision-impaired eye diseases: age-related macular degeneration, clinically significant cataract (grade 2 or more by Lens Opacities Classification System III) and significant corneal opacities.We also excluded patients with high refractive errors (greater than 5 dioptres sphere and/or cylindrical errors greater than 2 dioptres cylinder) and patients with history of previous intraocular surgery within the last 3mo. In addition, exclusion criteria were major neurological, psychiatric, cognitive or orthopedic disturbances that could affect patients’ vision and QOL.
Demographic information (age, sex, marital and employment status, level of education) were collected through detailed interviews. All patients underwent a complete ophthalmological examination, including anterior and posterior segment evaluation and a comprehensive clinical assessment of glaucoma. To correlate QOL as measured by the GQL-15 with clinical parameters, we conducted visual acuity and visual field measurements. Snellen visual acuity was recorded and converted to the logarithm of the minimal angle of resolution(logMAR) for data analysis. A central 30° visual field evaluation using automated static perimetry (OCTOPUS 600,Haag-Streit Eye Suite, Switzerland) was performed. Patients who had unreliable visual fields (e.g.fixation loss, reliability factor exceeding 15%) were not included in the study. Visual field mean defect (MD) and square root of loss variance (sLV)were noted.
In order to correlate self-perceived QOL with the disease severity, we performed a stratification of our patients using the Nelson’s Glaucoma Staging System[8]. This system is based on the central visual field deficit and classifies the patients into these three groups: mild (loss of less than one half of the visual field only in one eye), moderate (loss of more than one half of the visual field in one eye, or loss of less than one half of the visual field in both eyes) and severe (deficit of more than one half of visual field lost in both eyes). This staging system has been shown to strongly correlate with the perimetric MD[8].The eye with better overall visual sensitivity, as determined by the perimetric MD, was marked as the better eye and the contralateral eye as the worse eye.
The study was approved by the Ethics Committee of the Faculty of Medicine (approval No. 2650/VI-20), University of Belgrade and all participants provided signed informed consent before enrolment.
Glaucoma Quality of Life-15 QuestionnaireThe GQL-15 questionnaire was developed by Nelsonet al[8]and was comprised of 15 vision-related items. The item-level responses for each factor are coded on a five-point scale (1 meaning no difficulty and 5 meaning severe difficulty), while 0 is marked if the participant does not perform the activity as a result of non-visual cause. These items are grouped into four subscales:1) “Central and near vision” (two items); 2) “Peripheral vision” (six items); 3) “Dark adaptation and glare” (six items);and 4) “Outdoor mobility” (one item). Total score is derived by summing all item-level response scores. Higher GQL-15 scores are revealing lower QOL. Subscale scores are derived by coding the item-level responses on a numerical interval scale ranging from 0 (no difficulty) to 100 (severe difficulty).Subscale scores are average of the sum of scores generated for the item-level subscale responses. Higher subscale scores are indicating lower QOL and greater difficulty with subscale specific tasks[3,6,8].
Translation of the Glaucoma Quality of Life-15The permission from the scale’s author for translation and application of the GQL-15 was received and the standard procedure for translation of a questionnaire was applied in order to generate the Serbian version of the GQL-15[16-17]. Translation of the original GQL-15 questionnaire to Serbian language was performed by two independent translators who were native Serbian speakers, one from the medical field who was involved with the study design and other with no medical background(“forward translation”). The translators were aiming at creating a version that would be equivalent to the original one and each of them independently produced a translated version with a written report highlighting ambiguous or demanding phrases.Subsequently, the two translators worked together to synthesize a consensus version of the questionnaire with a following written report. Then two new translators, who were blinded to the original questionnaire and who were not working in a medical field, performed “backward translation”, creating two back translated versions of the questionnaire in English language. In order to reach a final version of the questionnaire,an expert committee was formed that included researchers and all the aforementioned translators. Their goal was to reviewall the translations with the corresponding written reports and to reach a consensus on any controversial items. Semantic,idiomatic, experiential and conceptual equivalence between the original and the final version of a questionnaire were priority of the committee’s work and an accompanying written report was also made[16-17]. To check the interpretation of the translated items, clarity, simplicity and relevance of the questions by the Serbian population, the new version of GQL-15 was pre-tested on 15 glaucoma patients.
Since there were no comments related to understanding and clarity of items, the final version was established and applied in this study. In our study the GQL-15 questionnaire was completed by the patients in the presence of a physician.
National Eye Institute Visual Function QuestionnaireNational Eye Institute Visual Function Questionnaire (NEIVFQ 25) is a vision-specific instrument that is most commonly used worldwide for vision related QOL assessments for patients with visual impairment[18]. It is comprised of 25 items that are grouped into 12 domains (general health, general vision, ocular pain, difficulty with near-vision activities,distance-vision activities, limitation of social functioning because of vision, mental health problems because of vision,role limitations because of vision, dependency on others because of vision, driving difficulties, difficulty with color vision and difficulty with peripheral vision). A composite score of NEI-VFQ 25 is generated by averaging the scores of all subscales except general health. A higher score indicates better vision-related QOL. The NEI-VFQ 25 has recently been translated and validated in Serbian language and it was shown that this version is a good and reliable tool for vision related QOL evaluations[19].
Statistical AnalysesDescriptive statistical analyses were performed to characterize the participants’ socio-demographic and clinical data using SPSS statistical software (Version 21.0 SPSS Science). To describe the GQL-15 scale, we analyzed minimal and maximal scores for each item and for all GQL-15 subscales. After stratification of glaucoma patients, Kruskal-Wallis analysis of variance was used to examine the effect of glaucoma severity on clinical characteristics (better and worse eye visual acuity, better and worse eye MD, better and worse eye sLV), GQL-15 summary score and subscale scores.
To evaluate reproducibility, 133 of 177 glaucoma patients repeated the GQL-15 questionnaire after 2wk period had elapsed. Reproducibilityi.e.test-retest assessment of the Serbian GQL-15 was assessed using the Spearman’s correlation coefficient.
Internal consistencyCronbach’s alpha coefficient was used to evaluate internal consistency of the Serbian version of the GQL-15 for each subscale. Values above 0.7 were recognized as statistically adequate[17]. Hotelling T-square test (HT2) test was used to evaluate the significance of differences between acquired mean score values of all GQL-15 items together and a hypothetic case where all items have an identical score.Corrected Item-Total Correlation (CI-TC) analysis was performed to test discriminating characteristics of the scale items. The CI-TC analysis demonstrates the relationship of one item with the score of remaining scale items. If CI-TC score is higher or equal to 0.4, an item can be regarded as an appropriate part of the scale[17].
Construct validityIn order to asses construct validity, an exploratory factor analysis-EFA (principal component analysis-PCA with Varimax rotation) was performed, which identifies complex interrelationships among items[17]. If resulting eigenvalue is over 1.0 a factor is regarded as significant. Factor loadings of the PCA are correlation coefficients between the scale items and factors that are identified. It is calculated as a total of square factor loadings (i.e.percent of variance) for all factors included in the given scale item. Higher communality index values are preferable, while as an index lower than 0.4 implies that an item should be withdrawn from the scale[17].
Criterion validityCriterion validity was assessed by correlating (Spearman’s correlation) the mean GQL-15 score with demographic (age, sex, marital and employment status,level of education) and clinical characteristics (visual acuity,MD, sLV and glaucoma severity) as well as with the NEI-VFQ 25 scores[17].
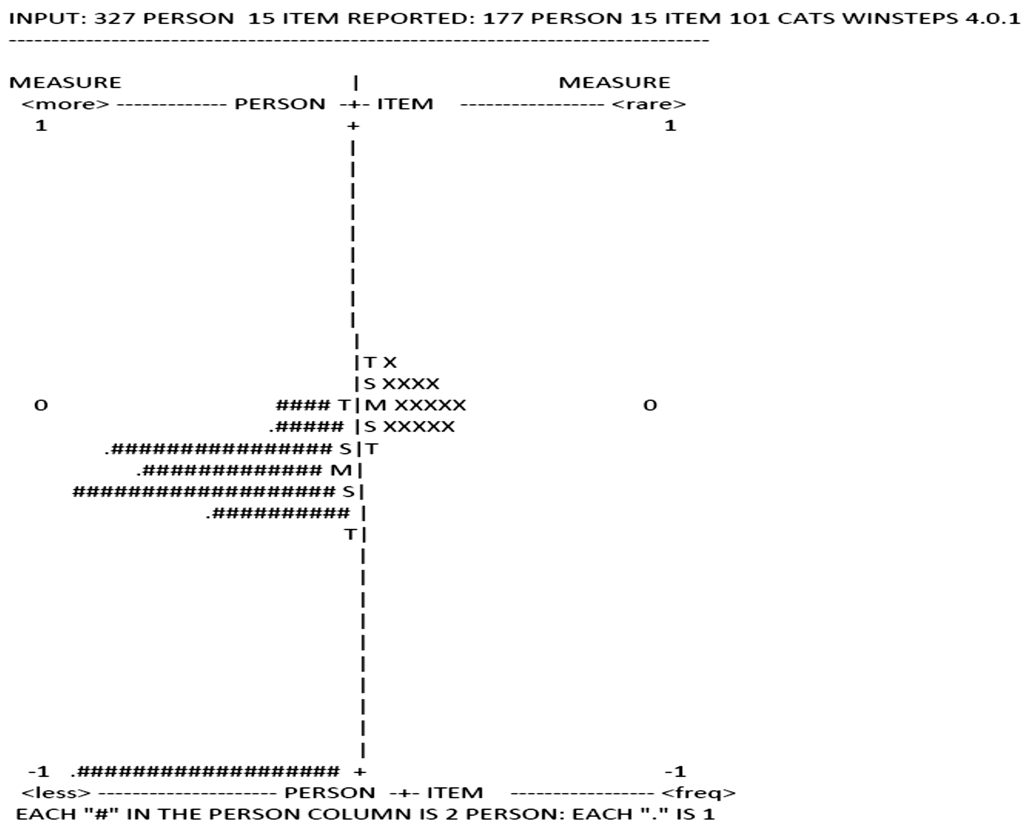
Psychometric properties in Rasch analysisIn addition to the traditional concept of validating a questionnaire, the Serbian GQL-15 also underwent a Rasch analysis, which is a contemporary method (probability based mathematical model)of testing psychometric characteristics of an instrument[20-21]. It evaluates person’s ability with regard to an item difficulty and the results are being defined in log-odds units (logits). Item difficulty and person ability are presented on an interval scale(chart) with logits representing measurement units. Positive(upper) part of the scale depicts items with greater difficulty and a person with higher ability, while negative (lower) side represents a person with lower ability and less difficulty items[20-21]. Winsteps software (version 4.0.1) was used to perform the Rasch analysis.
Person separation denotes instrument measurement precision and it reveals how many strata of person ability a questionnaire can differentiate. Item separation shows the reproducibility of the instrument and the number of item groups based on their difficulty level. A reliability coefficient of 0.8 for these two separation indices is regarded as suitable[9,13,22-24].Unidimensionality is an element that describes questionnaire’s ability to measure a single construct and it is best determined by fit statistics (infit and outfit). Both infit and outfit statistics define how well each item conforms to the underlying construct, with the infit statistics being more revealing indicator since it is less sensitive to effect of the outliers. Mean squarestandardized residuals (MNSQ) are being used to represent fit statistics and values between 0.5 and 1.5 are considered to be acceptable[9,13,22-24].
Table 1 Demographic and clinical characteristics of Serbian patients with glaucoma

GL: Glaucoma; POAG: Primary open angle glaucoma; PACG: Primary angle-closure glaucoma; NTG: Normal tension glaucoma; PEX: Pseudoexfoliative; PG: Pigmentary glaucoma; logMAR: Logarithm of the minimal angle of resolution; MD: Mean defect; sLV: Square root of loss variance;aProbability valueP<0.05 between mild and moderate glaucoma, moderate and advanced glaucoma and mild and advanced glaucoma;
bprobability valueP<0.05 between mild and moderate glaucoma and mild and advanced glaucoma.
Patients characteristics Overall group (n=177) Mild GL (n=101) Moderate GL (n=38) Advanced GL (n=38)Age, mean±SD (y) 62.83±13.60 60.78±13.39 63.66±13.07 67.45±13.80 Sex,n(%)Female 113 (63.8) 67 (66.3) 23 (60.5) 23 (60.5)Male 64 (36.2) 34 (33.7) 15 (39.5) 15 (39.5)Education level,n(%)Primary school 12 (6.8) 4 (4.0) 1 (2.6) 7 (18.4)Secondary school 60 (33.9) 30 (29.7) 16 (42.1) 14 (36.8)University 105 (59.3) 67 (66.3) 21 (55.3) 17 (44.7)Marital status,n(%)Married/cohabitated 119 (67.2) 68 (67.3) 26 (68.4) 25 (65.8)Other (divorced, widowed, single) 58 (32.8) 43 (42.6) 12 (31.6) 13 (34.2)Employment status,n(%)Employed 52 (29.4) 38 (37.6) 7 (18.4) 7 (18.4)Unemployed 11 (6.2) 7 (6.9) 2 (5.3) 2 (5.3)Retired 114 (64.4) 56 (55.4) 29 (76.3) 29 (76.3)Type of glaucoma,n(%)POAG 80 (45.2) 57 (56.4) 10 (26.3) 13 (34.2)PACG 28 (15.8) 16 (15.8) 3 (7.9) 9 (23.7)PEX 28 (15.8) 7 (6.9) 9 (2.4) 12 (31.6)PG 15 (8.5) 9 (8.9) 4 (10.5) 2 (5.3)NTG 26 (14.7) 12 (11.9) 12 (31.6) 2 (5.3)Better eye visual acuity (logMAR)a0.08±0.11 0.06±0.08 0.11±0.11 0.13±0.15 Worse eye visual acuity (logMAR)a0.68±1.58 0.08±0.13 0.36±0.91 2.61±2.47 Better eye visual field (db)MDa2.38±5.04 -0.39±1.53 3.27±3.36 8.72±6.21 sLVb4.01±3.05 2.60±1.28 5.63±4.60 6.18±2.59 Worse eye visual field (db)MDa7.65±9.37 1.40±2.74 9.66±5.55 22.56±5.26 sLVa4.71±3.08 3.50±1.89 7.91±3.08 4.89±3.48
RESULTS
Description of the Study SampleOne hundred seventy seven patients with glaucoma meeting the eligibility criteria were enrolled. The mean age of the patients was 62.83±13.60y.The majority of patients were women (63.8%), married or cohabitating (67.2%), with higher education level (59.3%)and retired (64.4%). Nearly half of our patients (45.2%) had POAG, while PACG and PEX patients were equally distributed(15.8%). Moreover, NTG was registered in 14.7% and PG in 8.5% of patients. Stratification by disease severity showed that 101 patients (57.1%) belonged to the mild, 38 patients (21.5%)to the moderate and 38 (21.5%) to the advanced glaucoma group. With the disease severity visual acuity of both better and worse eye was significantly reduced, while MD and sLV significantly increased. There was no significant difference in sLV of the better eye between moderate and advanced glaucoma group. The overall socio-demographic and clinical characteristics of patients are presented in Table 1.
Glaucoma Quality of Life-15 ScoresThere were no major changes in the description of items during the process of translation and validation. The simple literal translation was adequate for almost all GQL-15 items.
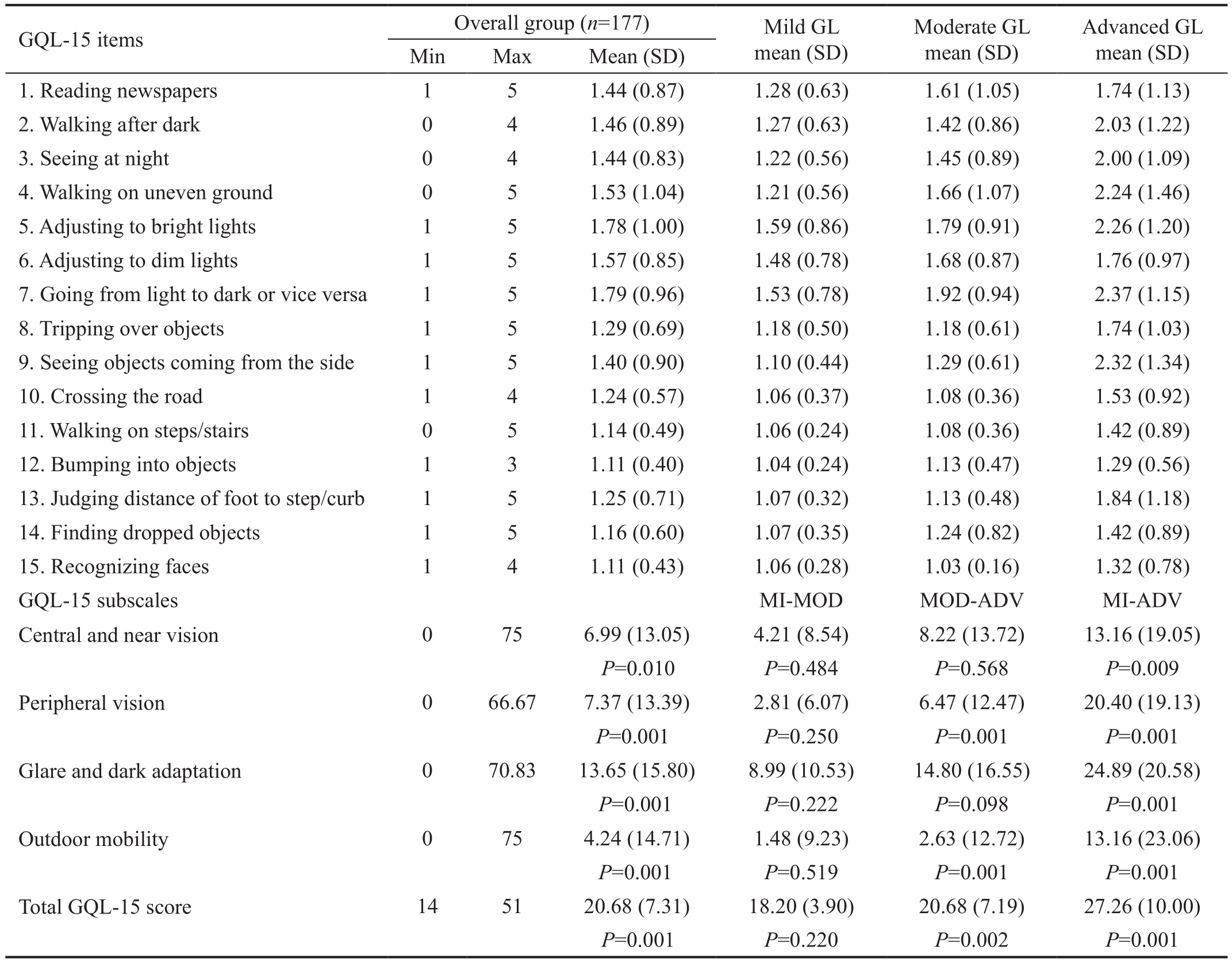
The mean total score for the Serbian GQL-15 was 20.68±7.31 indicating that QOL of Serbian glaucoma patients was rather good. The values of item and domain scores of the Serbian GQL-15 in the overall population as well as regarding the glaucoma stages are shown in Table 2. The differences in the total score and all subscales scores of GQL-15 were statistically significant between mild and advanced group.Significant differences in the total score, “Peripheral vision”and “Outdoor mobility” subscales were also registered between moderate and advanced glaucoma group. There were no significant differences between mild and moderate glaucoma patients regarding summary and subscale scores of the GQL-15(Table 2).
Table 2 Average scores on GQL-15 in Serbian language according to items and subscales as well as according to glaucoma stages(subscale score comparison between the glaucoma stages)
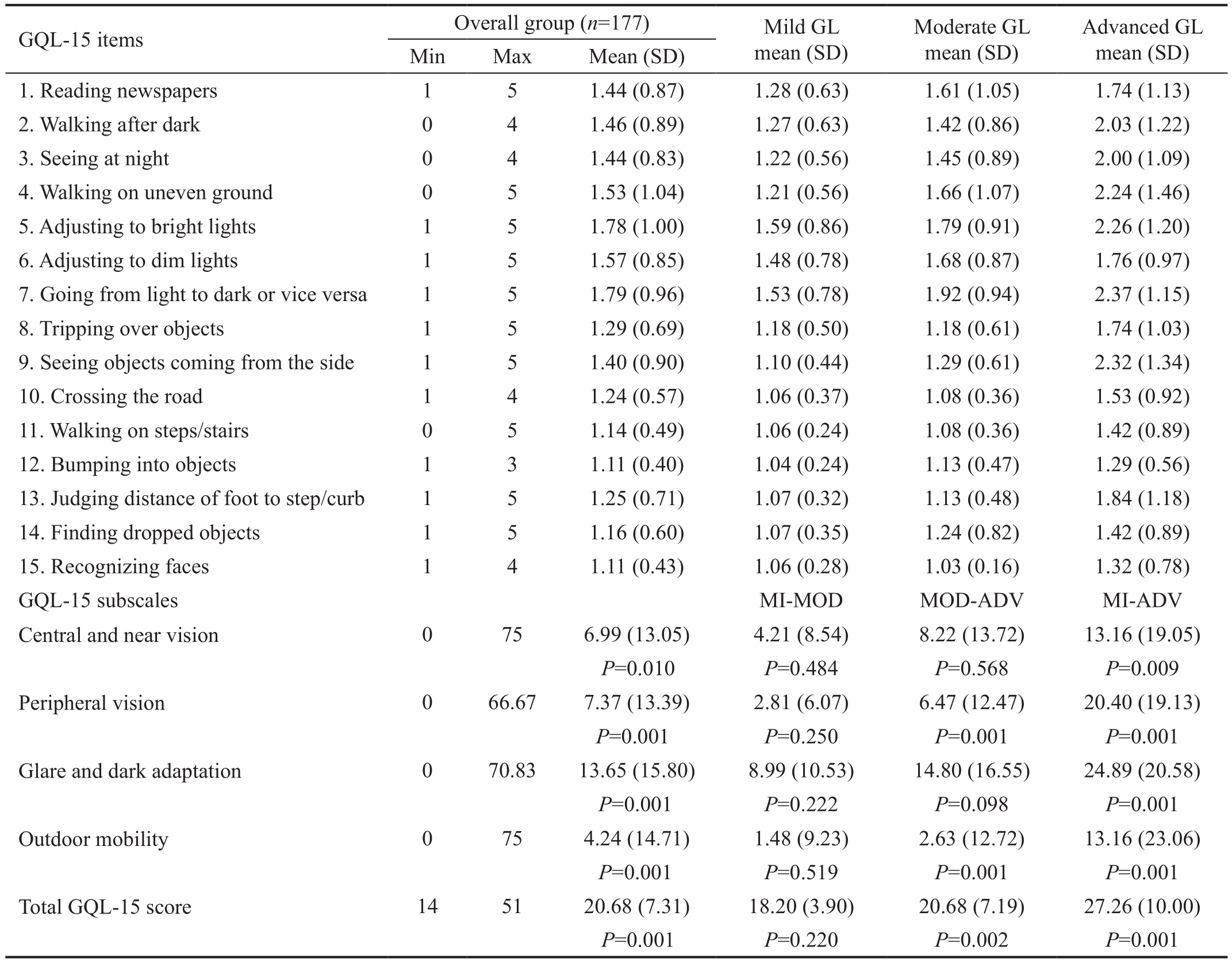
GL: Glaucoma; SD: Standard deviation; MI: Mild glaucoma; MOD: Moderate glaucoma; ADV: Advanced glaucoma;P: Probability value.
1. Reading newspapers 1 5 1.44 (0.87) 1.28 (0.63) 1.61 (1.05) 1.74 (1.13)2. Walking after dark 0 4 1.46 (0.89) 1.27 (0.63) 1.42 (0.86) 2.03 (1.22)3. Seeing at night 0 4 1.44 (0.83) 1.22 (0.56) 1.45 (0.89) 2.00 (1.09)4. Walking on uneven ground 0 5 1.53 (1.04) 1.21 (0.56) 1.66 (1.07) 2.24 (1.46)5. Adjusting to bright lights 1 5 1.78 (1.00) 1.59 (0.86) 1.79 (0.91) 2.26 (1.20)6. Adjusting to dim lights 1 5 1.57 (0.85) 1.48 (0.78) 1.68 (0.87) 1.76 (0.97)7. Going from light to dark or vice versa 1 5 1.79 (0.96) 1.53 (0.78) 1.92 (0.94) 2.37 (1.15)8. Tripping over objects 1 5 1.29 (0.69) 1.18 (0.50) 1.18 (0.61) 1.74 (1.03)9. Seeing objects coming from the side 1 5 1.40 (0.90) 1.10 (0.44) 1.29 (0.61) 2.32 (1.34)10. Crossing the road 1 4 1.24 (0.57) 1.06 (0.37) 1.08 (0.36) 1.53 (0.92)11. Walking on steps/stairs 0 5 1.14 (0.49) 1.06 (0.24) 1.08 (0.36) 1.42 (0.89)12. Bumping into objects 1 3 1.11 (0.40) 1.04 (0.24) 1.13 (0.47) 1.29 (0.56)13. Judging distance of foot to step/curb 1 5 1.25 (0.71) 1.07 (0.32) 1.13 (0.48) 1.84 (1.18)14. Finding dropped objects 1 5 1.16 (0.60) 1.07 (0.35) 1.24 (0.82) 1.42 (0.89)15. Recognizing faces 1 4 1.11 (0.43) 1.06 (0.28) 1.03 (0.16) 1.32 (0.78)GQL-15 subscales MI-MOD MOD-ADV MI-ADV Central and near vision 0 75 6.99 (13.05) 4.21 (8.54) 8.22 (13.72) 13.16 (19.05)P=0.010P=0.484P=0.568P=0.009 Peripheral vision 0 66.67 7.37 (13.39) 2.81 (6.07) 6.47 (12.47) 20.40 (19.13)P=0.001P=0.250P=0.001P=0.001 Glare and dark adaptation 0 70.83 13.65 (15.80) 8.99 (10.53) 14.80 (16.55) 24.89 (20.58)P=0.001P=0.222P=0.098P=0.001 Outdoor mobility 0 75 4.24 (14.71) 1.48 (9.23) 2.63 (12.72) 13.16 (23.06)P=0.001P=0.519P=0.001P=0.001 Total GQL-15 score 14 51 20.68 (7.31) 18.20 (3.90) 20.68 (7.19) 27.26 (10.00)P=0.001P=0.220P=0.002P=0.001 GQL-15 items Overall group (n=177) Mild GL mean (SD)Moderate GL mean (SD)Advanced GL mean (SD)Min Max Mean (SD)
Reproducibility of the Serbian version of the GQL-15 as measured by the Spearman’s correlation coefficient was very good (ρ=0.96,P<0.001).
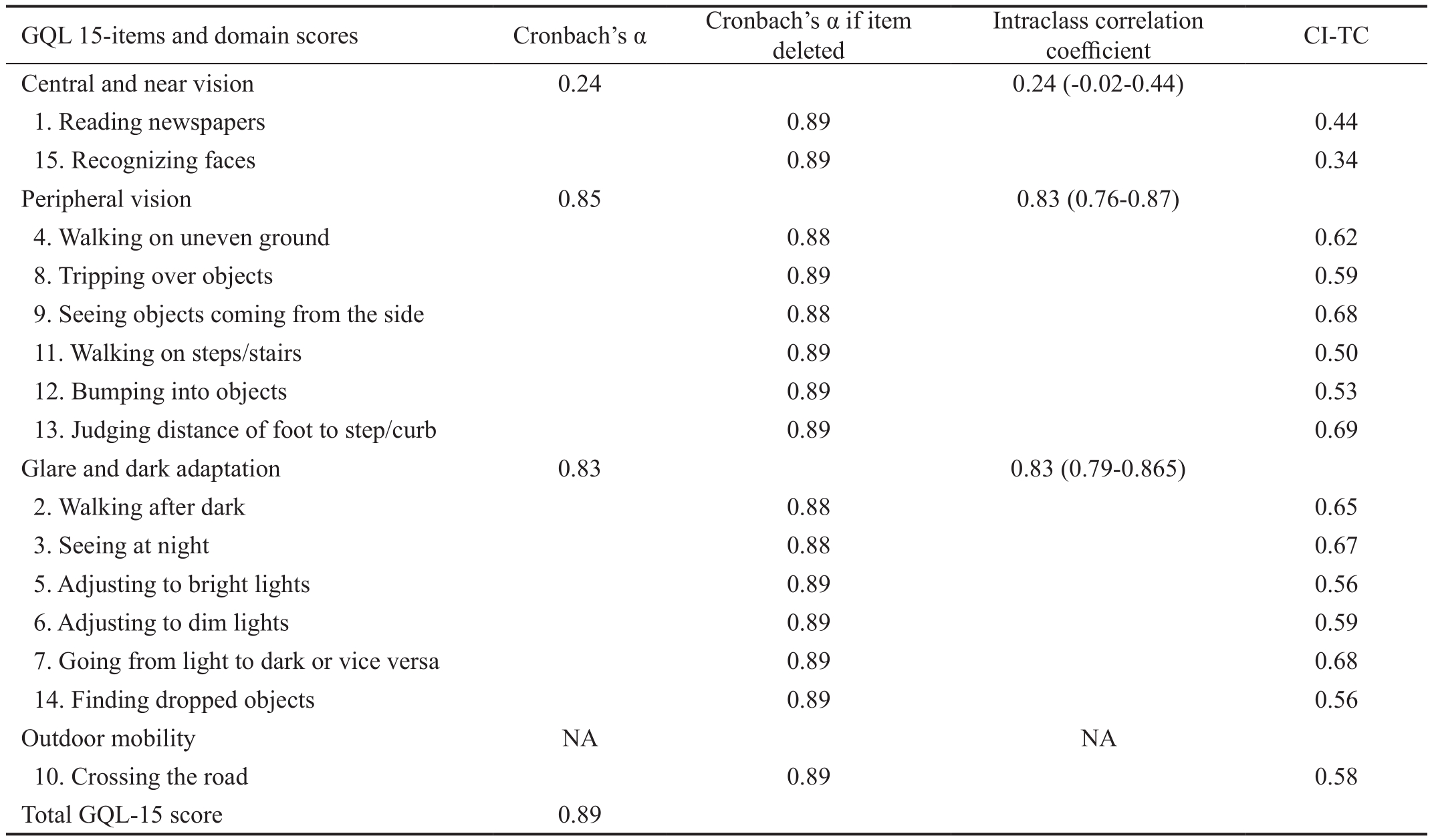
Internal ConsistencyThe internal consistency (Cronbach’s alpha coefficient) of the Serbian version of the GQL-15 was 0.89. Cronbach’s alpha for GQL-15 subscales “Peripheral vision” and “Glare and dark adaptation” were also adequate,while for subscale “Central and near vision” the coefficient was low (Table 3). Outdoor mobility subscale was composed of only one item, thus the internal consistency was not evaluated. Value of Cronbach’s alpha coefficient if item deleted was above 0.80 for all items. The values of the CI-TC coefficient for the GQL-15 in Serbian population were higher than 0.40 for almost all items. Item 15 “Recognizing faces”had the CI-TC coefficient of 0.34, somewhat lower than the adequate value of 0.4 (Table 3). Hotelling’s T-Squared test was highly significant (HT2=157.37;F=10.40;P<0.001).
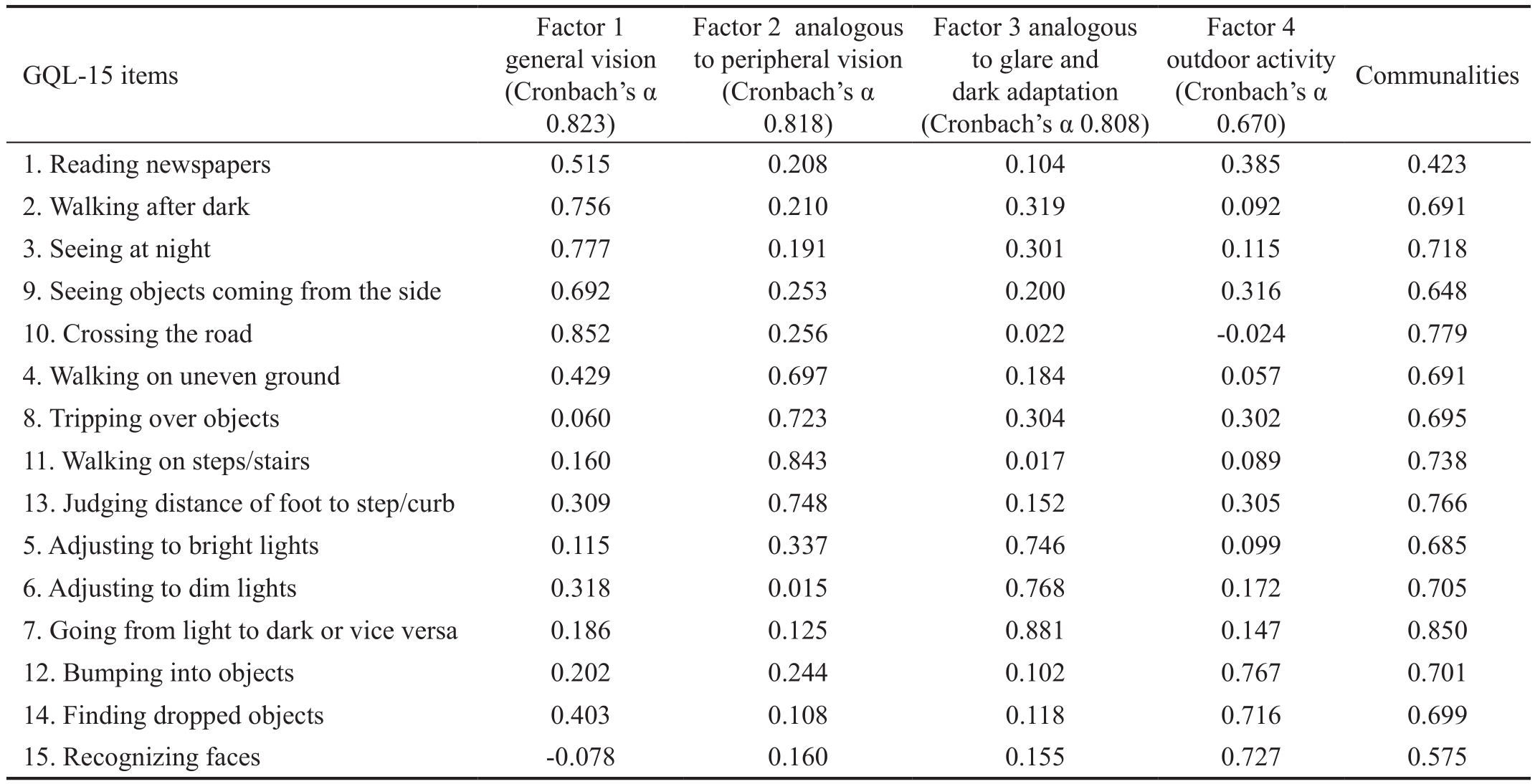
Construct ValidityOn factor analysis of the Serbian GQL-15 we obtained 4 factors just like in the original scale (Table 4).Total variance defined by the four extracted factors was 70.3%.However, item distribution did not conform to the original GQL-15 version. The first factor (42.70% of total variance)contained 5 items, item 1 of the “Central and near vision“subscale, two items (2 and 3) from “Dark adaptation and glare“subscale, item 9 from the original peripheral vision subscale and item 10 from the outdoor mobility subscale. The second factor (9.92% of variance) included 4 items (4, 8, 11 and 13)from the original “Peripheral vision“ subscale. Factor 3 (9.37%of variance) contained 3 items (5, 6 and 7) from the “Dark and glare adaptation“ subscale. Item 12 from “Peripheral vision“subscale, item 14 from the original “Glare and dark adaptation“subscale and item 15 from “Central vision“ subscale were clustered in Factor 4 (8.31% of variance). Therefore, our factor 2 corresponds to the original factor “Peripheral vision“and factor 3 with “Glare and dark adaptation“. Conversely,two novel factors (factor 1 General vision; factor 4 Outdoor activity) were obtained in the Serbian population (Table 4).All items had an adequate communality index of more than 0.4. Furthermore, internal consistency was tested among our new four factors. Cronbach’s alpha coefficients demonstrated excellent internal consistency for “General vision”, “Peripheral vision” and “Glare and dark adaptation” (0.823, 0.818 and 0.808 respectively). Slightly lower value of the coefficient was observed in the new factor “Outdoor activity” and it equaled 0.670, somewhat below the acceptable cut-off of 0.7.
Table 3 Cronbach’s alpha coefficients, interclass correlation coefficients and CI-TC coefficients for the Serbian version of the GQL-15 scale
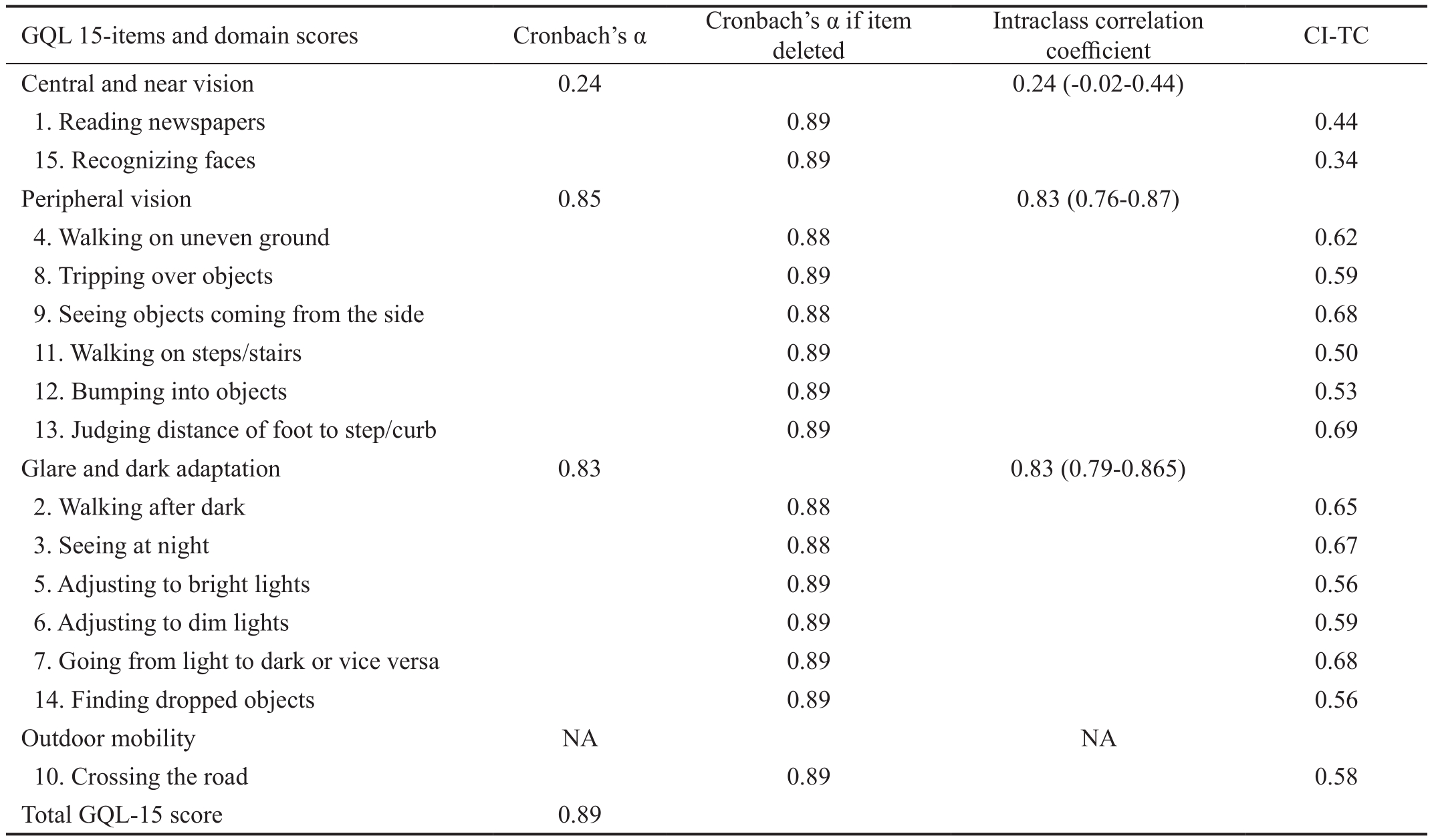
GQL-15: Glaucoma Quality of Life-15; CI-TC: Corrected item-total correlation coefficient; NA: Not applicable.
0.44 15. Recognizing faces 0.89 0.34 Peripheral vision 0.85 0.83 (0.76-0.87)4. Walking on uneven ground 0.88 0.62 8. Tripping over objects 0.89 0.59 9. Seeing objects coming from the side 0.88 0.68 11. Walking on steps/stairs 0.89 0.50 12. Bumping into objects 0.89 0.53 13. Judging distance of foot to step/curb 0.89 0.69 Glare and dark adaptation 0.83 0.83 (0.79-0.865)2. Walking after dark 0.88 0.65 3. Seeing at night 0.88 0.67 5. Adjusting to bright lights 0.89 0.56 6. Adjusting to dim lights 0.89 0.59 7. Going from light to dark or vice versa 0.89 0.68 14. Finding dropped objects 0.89 0.56 Outdoor mobility NA NA 10. Crossing the road 0.89 0.58 Total GQL-15 score 0.89 GQL 15-items and domain scores Cronbach’s α Cronbach’s α if item deleted Intraclass correlation coefficient CI-TC Central and near vision 0.24 0.24 (-0.02-0.44)1. Reading newspapers 0.89
Table 4 Exploratory factor analysis of Serbian version of GQL-15 with communalities and Cronbach’s coefficients for each factor
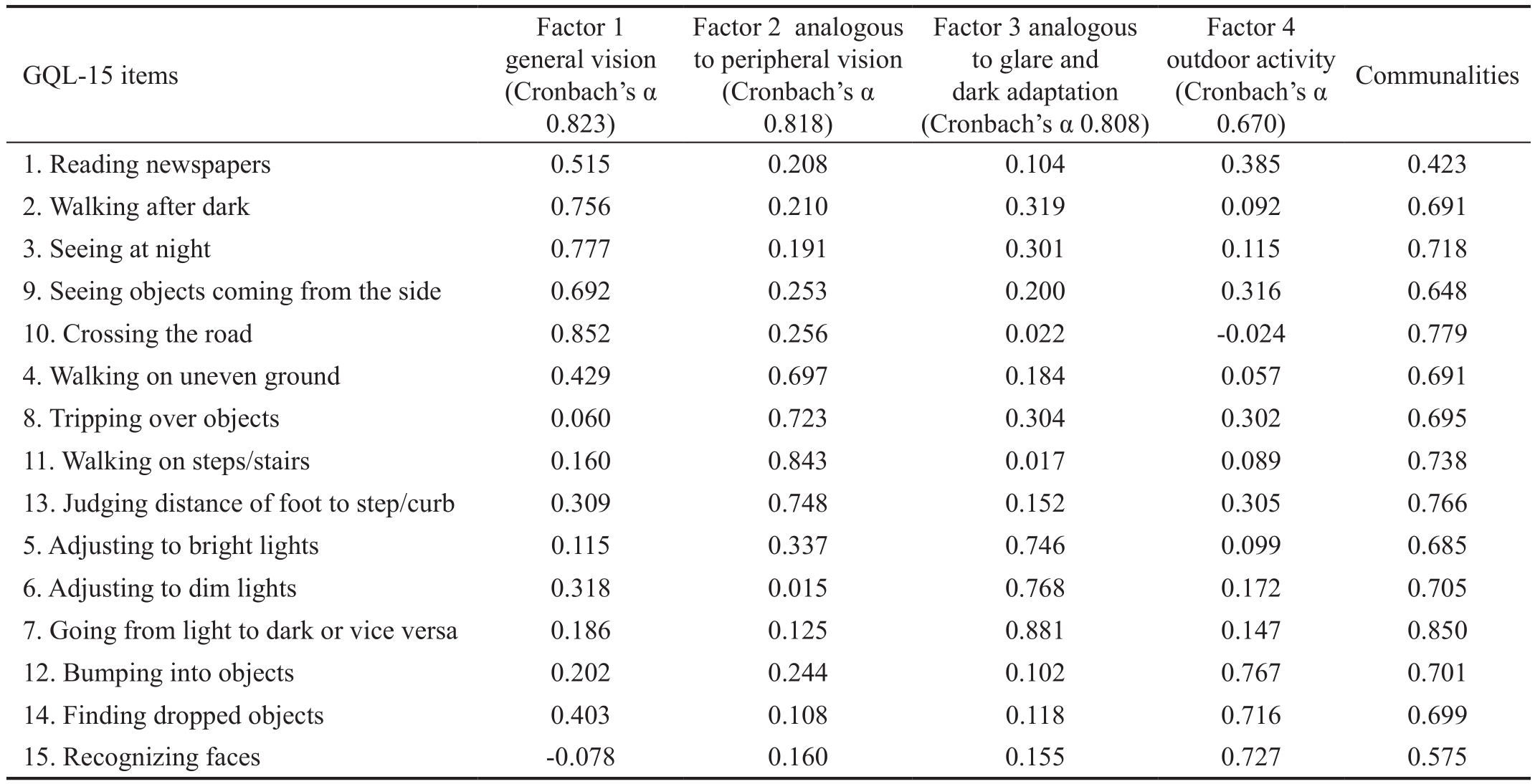
GQL-15: Glaucoma Quality of Life-15.
GQL-15 items Factor 1 general vision(Cronbach’s α 0.823)Factor 2 analogous to peripheral vision(Cronbach’s α 0.818)Factor 3 analogous to glare and dark adaptation(Cronbach’s α 0.808)Factor 4 outdoor activity(Cronbach’s α 0.670)Communalities 1. Reading newspapers 0.515 0.208 0.104 0.385 0.423 2. Walking after dark 0.756 0.210 0.319 0.092 0.691 3. Seeing at night 0.777 0.191 0.301 0.115 0.718 9. Seeing objects coming from the side 0.692 0.253 0.200 0.316 0.648 10. Crossing the road 0.852 0.256 0.022 -0.024 0.779 4. Walking on uneven ground 0.429 0.697 0.184 0.057 0.691 8. Tripping over objects 0.060 0.723 0.304 0.302 0.695 11. Walking on steps/stairs 0.160 0.843 0.017 0.089 0.738 13. Judging distance of foot to step/curb 0.309 0.748 0.152 0.305 0.766 5. Adjusting to bright lights 0.115 0.337 0.746 0.099 0.685 6. Adjusting to dim lights 0.318 0.015 0.768 0.172 0.705 7. Going from light to dark or vice versa 0.186 0.125 0.881 0.147 0.850 12. Bumping into objects 0.202 0.244 0.102 0.767 0.701 14. Finding dropped objects 0.403 0.108 0.118 0.716 0.699 15. Recognizing faces -0.078 0.160 0.155 0.727 0.575
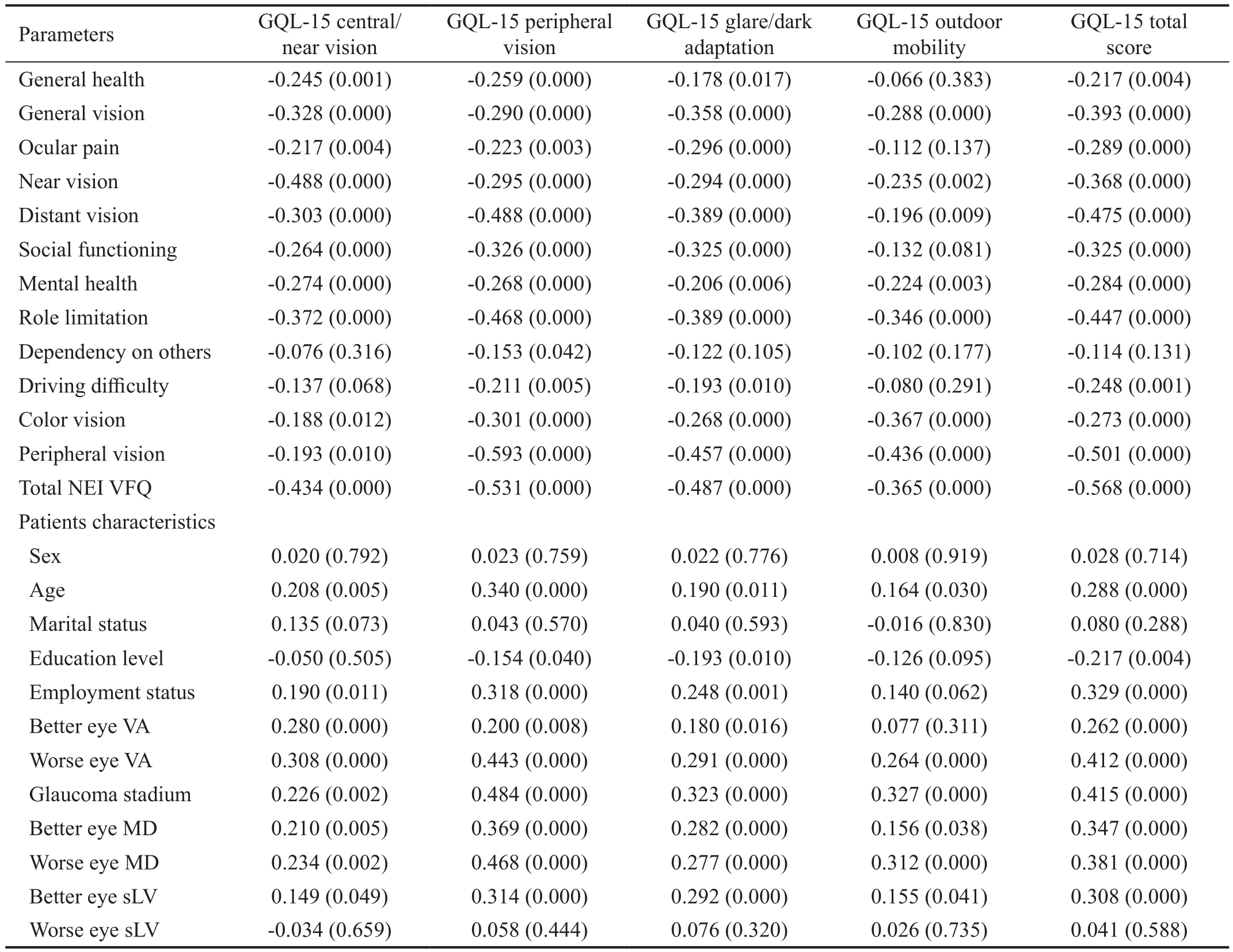
Citerion ValidityThe GQL-15 total score in Serbian population correlated significantly negatively with the NEIVFQ 25 composite score as well as with all NEI-VFQ 25domains except “Dependency on others” because of vision(Table 5). Also, significant negative correlations were observed when GQL-15 subscales were correlated with NEI-VFQ 25 domains. However, except for the “Peripheral vision”subscale none of the other GQL-15 subscales correlated with the “Dependency on others because of vision” NEI-VFQ 25 domain. Furthermore, Spearman’s correlation coefficients were not significant when GQL-15 “Central vision” and“Outdoor mobility” were compared with NEI-VFQ 25 “Driving difficulty” and when “Outdoor mobility” was compared with“General health” and “Ocular pain” of the NEI-VFQ 25 (Table 5).The GQL-15 total score and almost all subscale scores correlated significantly positively with better eye and worse eye VA, better eye and worse eye MD and better eye sLV (Table 5).Only mobility subscale score did not correlate significantly with better eye visual acuity. Among the demographic variables, age and professional status were significantly positively correlated with GQL-15 summary score and subscale scores (except mobility subscale score with professional status). In contrast,patients’ education level was correlated significantly negatively with the GQL-15 summary score as well as with glare and dark adaptation subscale scores (Table 5).
Table 5 Correlation of GQL-15 subscales and total score with NEI-VFQ 25 and patient demographic and clinical characteristics
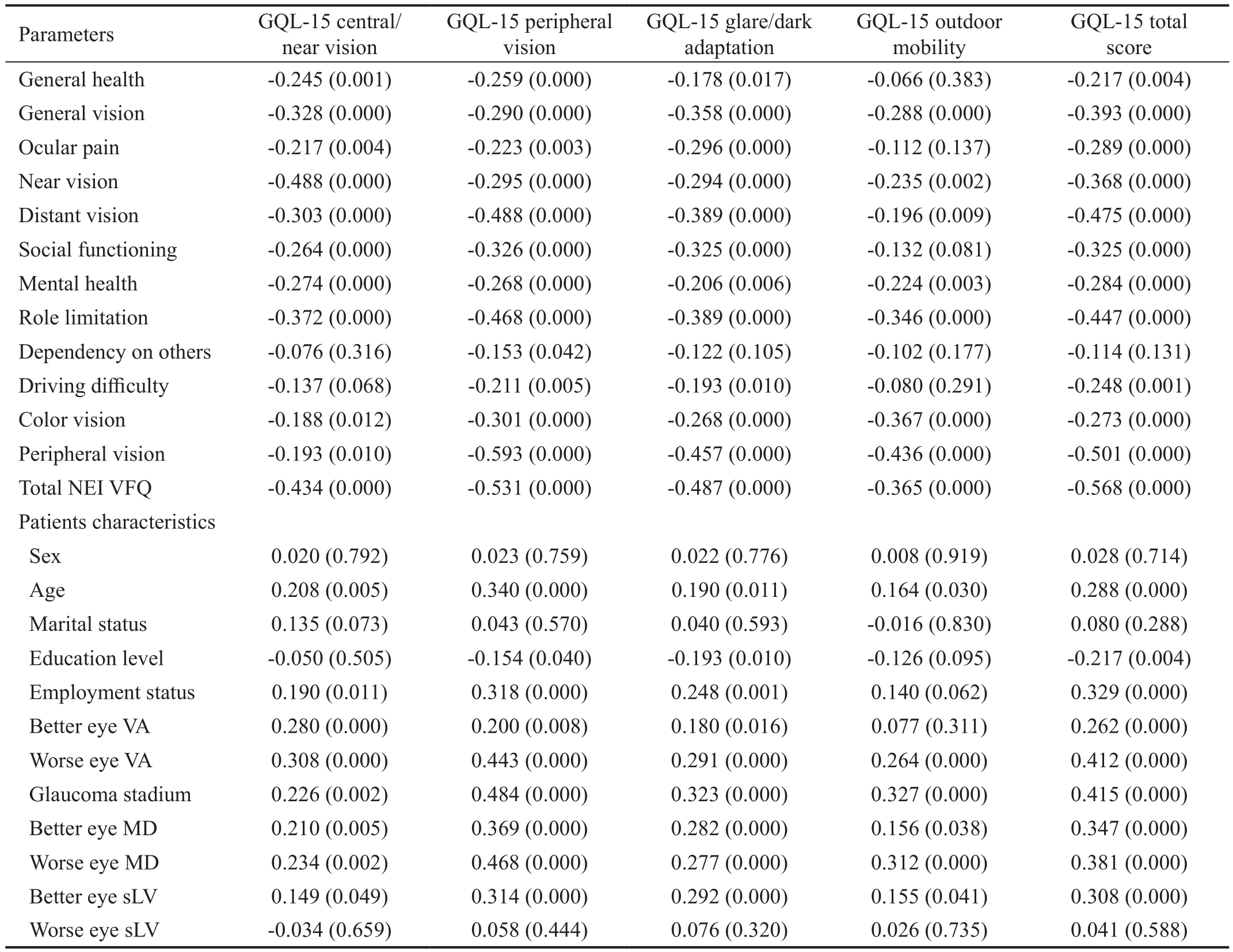
Spearman’s correlation coefficient (ρ) and probability values; GQL-15: Glaucoma Quality of Life-15; VA: Visual acuity; MD: Mean defect; Slv:Square root of loss variance.
GQL-15 total score General health -0.245 (0.001) -0.259 (0.000) -0.178 (0.017) -0.066 (0.383) -0.217 (0.004)General vision -0.328 (0.000) -0.290 (0.000) -0.358 (0.000) -0.288 (0.000) -0.393 (0.000)Ocular pain -0.217 (0.004) -0.223 (0.003) -0.296 (0.000) -0.112 (0.137) -0.289 (0.000)Near vision -0.488 (0.000) -0.295 (0.000) -0.294 (0.000) -0.235 (0.002) -0.368 (0.000)Distant vision -0.303 (0.000) -0.488 (0.000) -0.389 (0.000) -0.196 (0.009) -0.475 (0.000)Social functioning -0.264 (0.000) -0.326 (0.000) -0.325 (0.000) -0.132 (0.081) -0.325 (0.000)Mental health -0.274 (0.000) -0.268 (0.000) -0.206 (0.006) -0.224 (0.003) -0.284 (0.000)Role limitation -0.372 (0.000) -0.468 (0.000) -0.389 (0.000) -0.346 (0.000) -0.447 (0.000)Dependency on others -0.076 (0.316) -0.153 (0.042) -0.122 (0.105) -0.102 (0.177) -0.114 (0.131)Driving difficulty -0.137 (0.068) -0.211 (0.005) -0.193 (0.010) -0.080 (0.291) -0.248 (0.001)Color vision -0.188 (0.012) -0.301 (0.000) -0.268 (0.000) -0.367 (0.000) -0.273 (0.000)Peripheral vision -0.193 (0.010) -0.593 (0.000) -0.457 (0.000) -0.436 (0.000) -0.501 (0.000)Total NEI VFQ -0.434 (0.000) -0.531 (0.000) -0.487 (0.000) -0.365 (0.000) -0.568 (0.000)Patients characteristics Sex 0.020 (0.792) 0.023 (0.759) 0.022 (0.776) 0.008 (0.919) 0.028 (0.714)Age 0.208 (0.005) 0.340 (0.000) 0.190 (0.011) 0.164 (0.030) 0.288 (0.000)Marital status 0.135 (0.073) 0.043 (0.570) 0.040 (0.593) -0.016 (0.830) 0.080 (0.288)Education level -0.050 (0.505) -0.154 (0.040) -0.193 (0.010) -0.126 (0.095) -0.217 (0.004)Employment status 0.190 (0.011) 0.318 (0.000) 0.248 (0.001) 0.140 (0.062) 0.329 (0.000)Better eye VA 0.280 (0.000) 0.200 (0.008) 0.180 (0.016) 0.077 (0.311) 0.262 (0.000)Worse eye VA 0.308 (0.000) 0.443 (0.000) 0.291 (0.000) 0.264 (0.000) 0.412 (0.000)Glaucoma stadium 0.226 (0.002) 0.484 (0.000) 0.323 (0.000) 0.327 (0.000) 0.415 (0.000)Better eye MD 0.210 (0.005) 0.369 (0.000) 0.282 (0.000) 0.156 (0.038) 0.347 (0.000)Worse eye MD 0.234 (0.002) 0.468 (0.000) 0.277 (0.000) 0.312 (0.000) 0.381 (0.000)Better eye sLV 0.149 (0.049) 0.314 (0.000) 0.292 (0.000) 0.155 (0.041) 0.308 (0.000)Worse eye sLV -0.034 (0.659) 0.058 (0.444) 0.076 (0.320) 0.026 (0.735) 0.041 (0.588)Parameters GQL-15 central/near vision GQL-15 peripheral vision GQL-15 glare/dark adaptation GQL-15 outdoor mobility
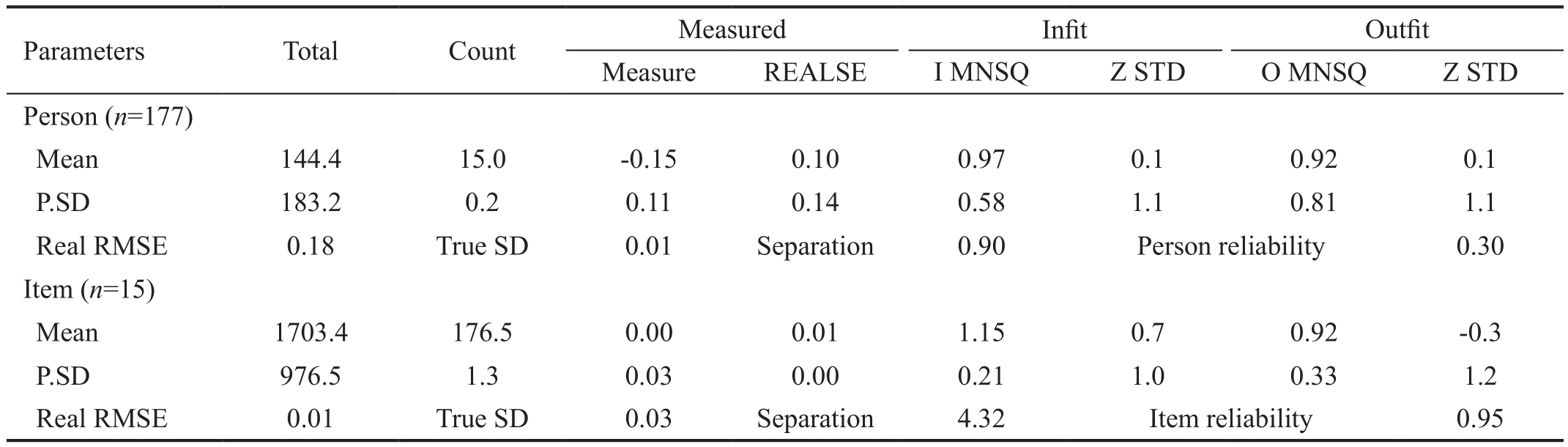
Psychometric Properties in Rasch AnalysisAccording to the performed Rasch analysis we observed that GQL-15 reliability index for items is quite high, indicating its adequate reproducibility. Moreover, obtained separation index (4.32)shows that the GQL-15 has four groups of items in terms of their difficulty level (Table 6). This was desired, as the GQL-15 can consequently be used for glaucoma patients with different abilities and stages.
Contrary, person reliability index as well as separation was rather low. However, as the GQL-15 questionnaire is an instrument for measuring quality of life, which is entirely individual and subjective, feelings cannot be graded nor compared between people, this part of the analysis is less important in our case and any finding is satisfactory.
The very low standard error of measurement (Model SE)presented on the Table 7 proves the reliability of the GQL-15 items. Only two items (1 and 14) have infit and only one (1)outfit mean squares above the standard accepted range (0.5 to1.5). This means that some average glaucoma patients would have a problem to answer these questions and that these questions are better for presenting the two extremes of QOL(very bad or very good). Still, as all correlation coefficients are very close to expected, our analysis is proven to be successful.In the Figure 1 we observed that the majority of glaucoma patients we tested were similar and around the mean level of ability and consequent QOL, although we had a distinct group of patients with very low abilities, probably due to advanced disease stage. Moreover, the graphic shows that although there were four groups of item difficulty, the difference in item levels was not significant. There were ten (2/3) of GQL-15 questionnaire that corresponded adequately with patients abilities, symptoms and/or feelings. Still, a lot of patients had no items in GQL-15 that would appropriately represent their condition and QOL. This
finding once again stresses the subjectivity and individuality of the feeling of QOL and indicates that more questionnaires should always be used together when assessing QOL.
Table 6 Rasch analysis GQL-15 fit statistics
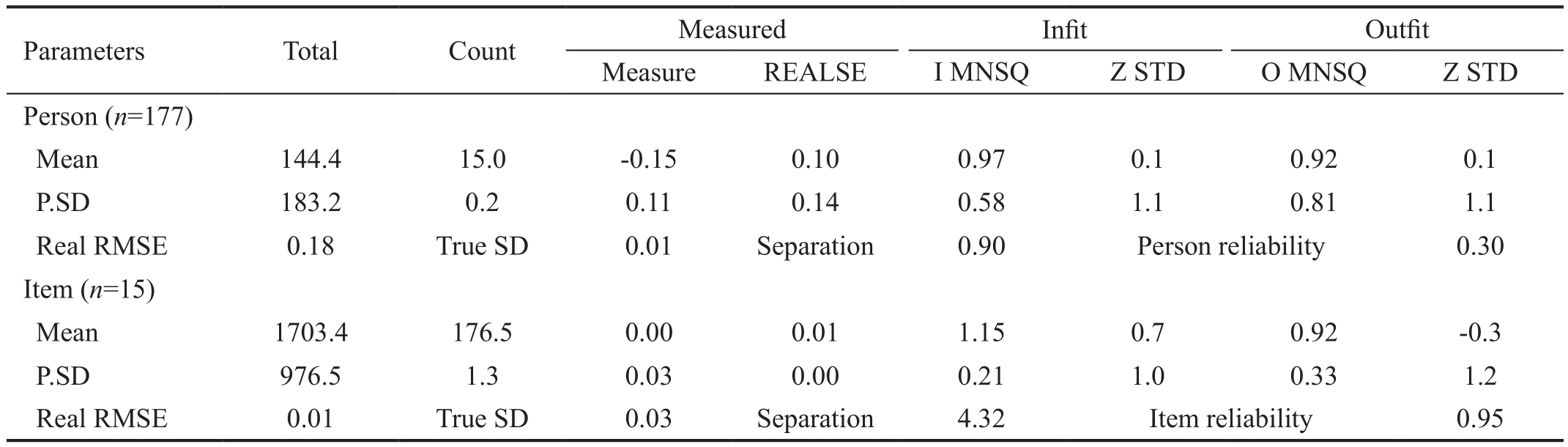
P.SD: Population standard deviation; REALSE: Standard errors of measure estimates; Z: Z standardized scores; STD: Standard deviation; I: Infit;O: Outfit; MNSQ: Mean square standardized residuals.
Parameters Total Count Measured Infit Outfit Measure REALSE I MNSQ Z STD O MNSQ Z STD Person (n=177)Mean 144.4 15.0 -0.15 0.10 0.97 0.1 0.92 0.1 P.SD 183.2 0.2 0.11 0.14 0.58 1.1 0.81 1.1 Real RMSE 0.18 True SD 0.01 Separation 0.90 Person reliability 0.30 Item (n=15)Mean 1703.4 176.5 0.00 0.01 1.15 0.7 0.92 -0.3 P.SD 976.5 1.3 0.03 0.00 0.21 1.0 0.33 1.2 Real RMSE 0.01 True SD 0.03 Separation 4.32 Item reliability 0.95
Table 7 Rasch analysis GQL-15 item statistics

P.SD: Population standard deviation; SE: Standard error; MNSQ: Mean square standardized residuals; Z: Z standardized scores; STD: Standard deviation; Correl.: Correlation; Expect.: Expected.
Entry number Total score Total count Measure Model SE Infit Outfit Ptmeasure MNSQ Z STD MNSQ Z STD Correl. Expect.1 2000 177 -0.01 0.01 1.52 2.9 1.88 3.4 0.40 0.47 2 2175 177 -0.02 0.00 0.87 -0.9 0.89 -0.5 0.51 0.49 3 2000 177 -0.02 0.01 0.88 -0.7 0.88 -0.5 0.49 0.48 4 2450 177 -0.03 0.00 1.17 1.2 1.02 0.2 0.50 0.52 5 3425 177 -0.04 0.00 1.11 0.9 1.10 0.7 0.58 0.57 6 2575 177 -0.03 0.00 1.03 0.2 0.89 -0.6 0.54 0.52 7 3525 177 -0.05 0.00 0.89 -0.8 0.86 -0.9 0.62 0.58 8 1325 177 0.00 0.01 1.13 0.8 0.75 -1.0 0.41 0.41 9 1800 177 -0.01 0.01 1.10 0.6 0.82 -0.8 0.44 0.46 10 750 177 0.03 0.01 1.29 1.3 0.55 -1.5 0.33 0.33 11 650 177 0.04 0.01 1.17 0.8 0.89 -0.2 0.31 0.31 12 500 177 0.05 0.01 0.98 0.0 0.65 -0.8 0.30 0.28 13 1100 177 0.01 0.01 1.05 0.3 0.58 -1.7 0.39 0.38 14 800 177 0.03 0.01 1.52 2.1 0.66 -1.1 0.32 0.34 15 476 177 0.05 0.01 1.49 1.6 1.45 1.1 0.23 0.28 Mean 1703.4 177 0.00 0.01 1.15 0.7 0.92 -0.3 / /P.SD 976.5 177 0.03 0.00 0.21 1.0 0.33 1.2 / /
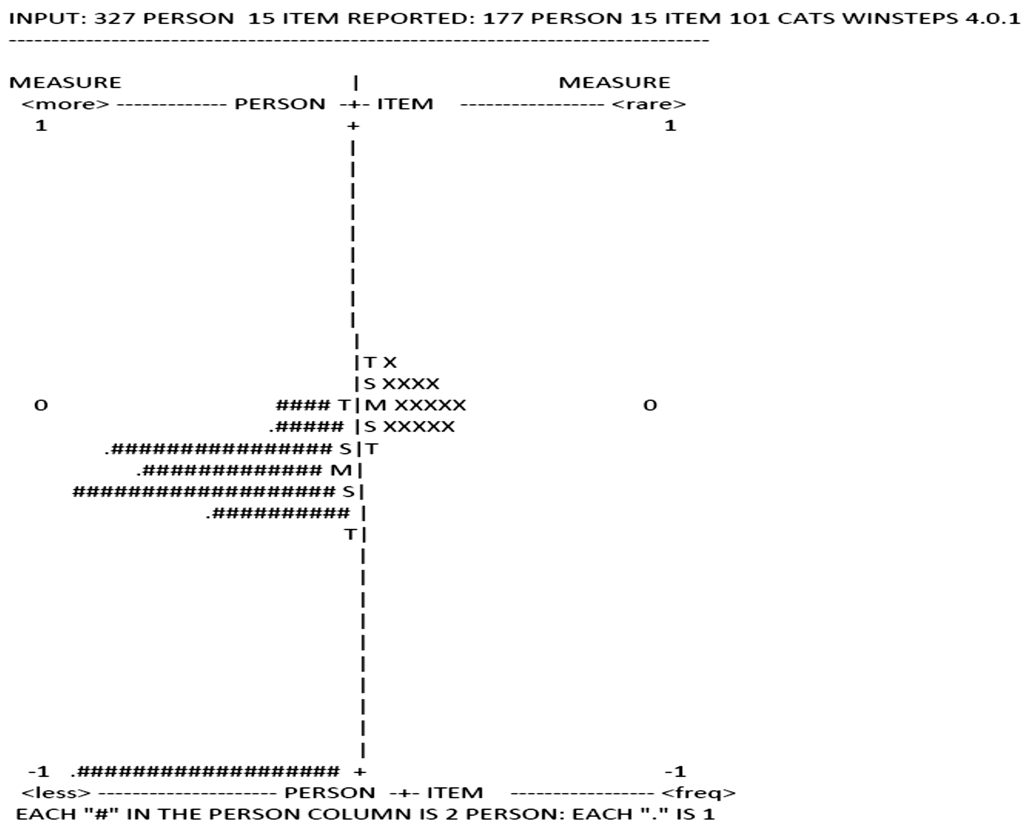
Figure 1 Rasch analysis GQL-15 person item chart.
DISCUSSION
This is the first study to evaluate psychometric properties of the questionnaire examining QOL among persons with glaucoma in Serbian language. Our goal was to validate the GQL-15 questionnaire and establish the scale for further use in clinical setting in Serbian language. Previous studies focusing on validation of the GQL-15 in other languages confirmed that psychometric properties of this scale were appropriate[10-11].
GQL-15 ScoresCompared to previous studies that aimed at validating the GQL-15 questionnaire, the mean overall summary score and the mean scores in different glaucoma stages were lower in Serbian population than the average values in the other reports[8,11,15]. Nevertheless, all studies agree that the glaucoma-related QOL deteriorate with the glaucoma severity[8,11,14-15]. Our result were comparable to the original GQL-15 study population, except for the mean summary score in advanced glaucoma group, which was somewhat higher than in Nelson’s sample[8]. Possible explanation for such results could be that, contrary to Nelson’s original population,we included patients with progressive visual field loss, which could explain the higher QOL values of advanced glaucoma group than in the original GQL-15 study[8]. In accordance with the previous studies, we have observed that “Glare and dark adaptation” was the subscale that yielded the highest average score, indicating that glaucoma patients have the greatest difficulties in glare and dark-related tasks[8,12,15,25].
Internal ConsistencyThe Cronbach’s alpha coefficient of the Serbian GQL-15 for the whole scale was 0.89, demonstrating an excellent internal consistency. A similar coefficient was obtained for the original scale[8]as well as in other cultural settings[11]. In terms of GQL-15 subscales, Cronbach’s alpha coefficients for “Peripheral vision” and “Glare and dark adaptation” subscales were both greater than 0.7, meaning that our patients responded consistently to the questions within these two subscales. Only “Central and near vision”subscale demonstrated low coefficient value of 0.24. Possible explanation for such a value could be related to the fact that this subscale is comprised of only two items (1 and 15) and reduction in number of items in the subscale could have also reduced the Cronbach’s alpha coefficient. Secondly, decreased Cronbach’s alpha coefficient could be attributed to the low value of the CI-TC coefficient for item 15 (i.e.“recognizing faces”) that was 0.34, suggesting that this item may not be entirely appropriate for the “Central and near vision” subscale at least in Serbian GQL-15 version.
Additionally, test-retest reliability of the scale, evaluated by the Spearman’s correlation coefficient of 0.96 showed that the total score of the Serbian GQL-15 remained stable over the twoweek period, suggesting a high level of scale reproducibility.
Construct ValidityAccording to exploratory factor analysis,Serbian version of the GQL-15 also exhibited 4 dimensions as the original version[8]and Chinese validation[11]. All factor loadings in our questionnaire were above the arbitrary cutoff of 0.4. However, all items did not conform to the item distribution of the original version, as it was the case with the Chinese validation[9]. Items 1, 2, 3, 9 and 10 formed a new subscale entitled “General Vision”, whereas items 12, 14,15 were clustered in the novel subscale “Outdoor activity”.Furthermore, internal consistency was tested for the novel four subscales and Cronbach’s alpha coefficients ranged from 0.823 to 0.670, demonstrating good correlation between items of these new subscales.
Despite the differences, metric evidence of the entire GQL-15 questionnaire compelled us to keep all the original items in the Serbian version of the GQL-15. We could explain this discrepancy in item distribution as a result of social and cultural differences. Items such as bumping into objects,finding dropped objects and recognizing faces, originally all coming from different subscales, were perceived by Serbian patients as “Outdoor activities”. Our patients seem to struggle during socializing and activities outside of their homes, while they have no problems with recognizing family members and household objects. The second novel subscale observed in our analysis included reading newspapers, walking after dark, seeing at night, seeing objects coming from the side and crossing the road. In order to exert these actions, a person needs to use both central and peripheral vision jointly in light and dark conditions. This finding suggests that in Serbian population all vision-related activities are considered to be in one similar domain, that we entitled “General vision”.
Criterion ValidityStrong correlations were demonstrated between GQL-15 outcomes and glaucoma clinical indices such as better and worse eye visual acuity, better and worse eye MD, better eye sLV and stage of glaucoma. However,correlation was not statistically significant when worse eye sLV was compared with the questionnaire summary and subscale scores. This result was expected, given the fact that sLV is a parameter that reflects the local non-uniformity of visual field defects. In cases of advance glaucoma, sLV can be paradoxically low, reflecting diffuse and uniformly deep areas of a visual deficit[26-27].
Our results indicate that GQL-15 has a good discriminatory capacity to differentiate advanced glaucoma from mild and moderate stage of the disease. Similar to our results, the original GQL-15 study as well as many other studies[8,11-12,15]found a marked difference in the summary score between mild and advanced glaucoma, while few studies reportedthat GQL-15 also discriminates advanced from the moderate glaucoma group[11-12,15]. Unlike some studies of Zhouet al[11]and of Goldberget al[15]we did not find significant difference in GQL-15 score between mild and moderate group. The outcome of the Serbian GQL-15 is more in favor of the traditional concept of glaucoma being an insidious disease,with the symptoms that appear until the late stage and that QOL is not affected in mild and moderate stages until there is some degree of visual impairment[26]. Serbian version of the GQL-15 was found to discriminate well the moderate from the advanced glaucoma in the terms of peripheral vision and outdoor mobility activities. In addition, total and subscales scores of the GQL-15 were correlated with NEIVFQ 25 composite and domain scores in order to analyze the validity of the Serbian GQL-15. The highest correlations were observed between total GQL-15 and NEI-VFQ 25 scores and also between analogous domains of these two instruments.For example central vision and peripheral vision subscales of the GQL-15 and corresponding domains of the NEI-VFQ 25 showed remarkable association. Likewise, the NEI-VFQ 25“Driving difficulty” correlated with “Peripheral vision” and“Glare and dark adaptation” subscales of the GQL-15, but not with “Central/near vision” or “Outdoor mobility”, which is in concordance with the appropriate aspects of vision that are crucial to perform driving. Furthermore, out of all the GQL-15 subscales only “Peripheral vision” was associated with NEIVFQ 25 “Dependency on others because of vision”, which could imply that our patients need assistance for performing activities that include side vision, and not for other visionrelated activities.
Psychometric Properties in Rasch AnalysisAdequate psychometric characteristics (reproducibility and reliability)of GQL-15 were proven with the performed Rasch analysis.The GQL-15 can be used for glaucoma patients with different abilities and stages. Rasch analysis, just like the factor analysis,extracted four groups of items. The difference in item difficulty was not significant. Most items corresponded adequately with patients’ condition and QOL. Still, patients with low functional abilities had no items in GQL-15 that would appropriately represent their condition and QOL. Moreover, items 1 and 14 are better for presenting extremes of QOL (very bad or very good). These findings correspond with other available GQL validations[10-11,15].
Misfit ItemsDifferent analyses that were performed in this study have shown that some of the items might be excluded from the Serbian version of the GQL-15 (item 15 according to internal consistency measurements; items 1 and 14 according to Rasch analysis). However, we decided to keep the scale structure with all items for a couple of reasons. Mainly, as the GQL-15 assesses QOL which is entirely subjective and individual feeling, all items can be important only, perhaps,for different people according to their personality type.Moreover, in terms of clinical relevance, study authors found all the GQL-15 items interesting and relevant in daily work with glaucoma patients. Furthermore, different statistical analyses pointed out to different items, indicating that other aspects and not just mathematical parameters need to be considered. Nevertheless, there were no significant changes in Cronbach’s α if any of the items were deleted, indicating no need for item omission. Additionally, in order to easily and adequately compare different populations the same structure of questionnaire should be applied. Therefore, as in the original and other translations GQL had 15 items, study authors decided that this concept should remain in Serbian version as well. Finally, Rasch analysis showed that not only that no items should be omitted, but in order to cover the symptoms and feeling and accurately describe self-perceived disability of all glaucoma patients, an instrument with even more items should be applied. Finally, the study aim was not to redesign the GQL-15, but to validate the existing instrument for use in Serbian population.
In conclusion, Serbian version of the GQL-15 is a simple and brief assessment tool with good internal consistency and reproducibility. This translated version demonstrates a remarkable internal consistency (Cronbach’s alpha 0.89) and strong relationship with clinical parameters of glaucoma.The Serbian GQL-15 exhibited four dimensions, just like the original, although some items were distributed into two novel subscales, which could be attributed to the local socio-cultural context. The Serbian version of GQL-15 is a valid instrument for evaluation of QOL among persons with glaucoma and can be applied in everyday clinical settings. This questionnaire can be used for further investigations of glaucoma-associated issues in the Serbian population.
ACKNOWLEDGEMENTS
Authors’ contributions:Sencanic I: study design, data collection, drafting of the manuscript, literature review;Gazibara T: statistical analyses, drafting of the manuscript;Dotlic J: statistical analyses, drafting of the manuscript;Stamenkovic M: patient selection and patient exam, results interpretation; Jaksic V: data collection, patient interview,literature review; Bozic M: patient selection and patient exam and interview, literature review; Grgurevic A: study design, results interpretation. All authors critically revised the manuscript for its intellectual content.
Conflicts of Interest:Sencanic I, None; Gazibara T, None;Dotlic J, None; Stamenkovic M, None; Jaksic V, None;Bozic M, None; Grgurevic A, None.
REFERENCES
1 Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: a review.JAMA2014;311(18):1901-1911.
2 Bourne RR, Taylor HR, Flaxman SR, Keeffe J, Leasher J, Naidoo K,Pesudovs K, White RA, Wong TY, Resnikoff S, Jonas JB; Vision Loss Expert Group of the Global Burden of Disease Study. Number of people blind or visually impaired by glaucoma worldwide and in world regions 1990-2010: a meta-analysis.PLoS One2016;11(10):e0162229.
3 Quaranta L, Riva I, Gerardi C, Oddone F, Floriani I, Konstas AG. Quality of life in glaucoma: a review of the literature.Adv Ther2016;33(6):959-981.
4 Zhang S, Liang Y, Chen Y, Musch DC, Zhang C, Wang N. Utility analysis of vision-related quality of life in patients with glaucoma and different perceptions from ophthalmologists.J Glaucoma2015;24(7):508-514.
5 Zhou C, Qian S, Wu P, Qiu C. Quality of life of glaucoma patients in China: sociodemographic, clinical and psychological correlates-a crosssectional study.Qual Life Res2014;23(3):999-1008.
6 Khadka J, McAlinden C, Pesudovs K. Quality assessment of ophthalmic questionnaires: review and recommendations.Optom Vis Sci2013;90(8):720-744.
7 Khadka J, McAlinden C, Gothwal VK, Lamoureux EL, Pesudovs K.The importance of rating scale design in the measurement of patientreported outcomes using questionnaires or item banks.Invest Ophthalmol Vis Sci2012;53(7):4042-4054.
8 Nelson P, Aspinall P, Papasouliotis O, Worton B, O’Brien C. Quality of life in glaucoma and its relationship with visual function.J Glaucoma2003;12(2):139-150
9 Khadka J, Pesudovs K, McAlinden C, Vogel M, Kernt M, Hirneiss C.Reengineering the glaucoma quality of life-15 questionnaire with rasch analysis.Invest Ophthalmol Vis Sci2011;52(9);6971-6977.
10 Lappas A, Foerster AM, Schild AM, Rosentreter A, Dietlein TS.Quantification of subjective visual quality of life in glaucoma patients:first results of a German version of the GQL-15 questionnaire.Ophthalmologe2011;108(8):745-752.
11 Zhou C, Yao J, Qian S, Wu P. Linguistic and psychometric validation of the Chinese version of the Glaucoma Quality of Life-15 (GQL-15-CHI): a cross-sectional study.Health Qual Life Outcomes2013;11:188.
12 Onakoya AO, Mbadugha CA, Aribaba OT, Ibidapo OO. Quality of life of primary open angle glaucoma patients in Lagos, Nigeria: clinical and sociodemographic correlates.J Glaucoma2012;21(5):287-295.
13 Gothwal VK, Reddy SP, Bharani S, Bagga DK, Sumalini R,Garudadri CS, Rao HL, Senthil S, Pathak-Ray V, Mandal AK. Impact of glaucoma on visual functioning in Indians.Invest Ophthalmol Vis Sci2012;53(10):6081-6092.
14 Wang B, Aung T, Marella M, Zheng Y, Wong TY, Perera S, Wong TT, Ho CL, Lamoureux EL. Impact of bilateral open and closed-angle glaucoma on glaucoma-specific functioning in Asians.J Glaucoma2013;22(4):330-335.
15 Goldberg I, Clement CI, Chiang TH, Walt JG, Lee LJ, Graham S,Healey PR. Assessing quality of life in patients with glaucoma using the Glaucoma Quality of Life-15 (GQL-15) questionnaire.J Glaucoma2009;18(1):6-12.
16 Stevens GA, Alkema L, Black RE, Boerma JT, Collins GS, Ezzati M, Grove JT, Hogan DR, Hogan MC, Horton R, Lawn JE, Marušić A, Mathers CD, Murray CJ, Rudan I, Salomon JA, Simpson PJ, Vos T, Welch V; GATHER Working Group. Guidelines for Accurate and Transparent Health Estimates Reporting: the GATHER statement.PLoS Med2016;13(6):e1002056.
17 Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures.Spine (Phila Pa 1976)2000;25(24):3186-3191.
18 Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD; National Eye Institute Visual Function Questionnaire Field Test Investigators. Development of the 25-item National Eye Institute Visual Function Questionnaire.Arch Ophthalmol2001;119(7):1050-1058.
19 Kovac B, Vukosavljevic M, Djokic Kovac J, Resan M, Trajkovic G, Jankovic J, Smiljanic M, Grgurevic A. Validation and cross-cultural adaptation of the National Eye Institute Visual Function Questionnaire(NEI VFQ-25) in Serbian patients.Health Qual Life Outcomes2015;13:142.
20 Mallinson T. Why measurement matters for measuring patient vision outcomes.Optom Vis Sci2007;84(8):675-682.
21 van Alphen A, Halfens R, Hasman A, Imbos T. Likert or Rasch?Nothing is more applicable than good theory.J Adv Nurs1994;20(1):196-201.
22 Lamoureux EL, Pallant JF, Pseudovs K, Hassell JB, Keeffe JE.The Impact of Vision Impairement Questionnaire: an evaluation of its measurement properties using Rasch analysis.Invest Ophthalmol Vis Sci2006;47:4732-4741.
23 Pseudovs K, Garamendi E, Keeves JP, Elliot DB. The Activities of Daily Vision Scale for cataract surgery outcomes: reevaluating validity with Rasch analysis.Invest Ophthalmol Vis Sci2003;44:2892-2899.
24 Mollazadegan K, Huang J, Khadka J, Wang Q, Yang F, Gao R,Pesudovs K. Cross-cultural validation of the National Eye Institute Visual Function Questionnaire.J Cataract Refract Surg2014;40(5):774-784.
25 Mbadugha CA, Onakoya AO, Aribaba OT, Akinsola FB. A comparison of the NEIVFQ25 and GQL-15 questionnaires in Nigerian glaucoma patients.Clin Ophthalmol2012;6:1411-1419.
26 Qiu M, Wang SY, Singh K, Lin SC. Association between visual field defects and quality of life in the United States.Ophthalmology2014;121(3):733-740.
27 Blumenthal EZ, Sapir-Pichhadze R. Misleading statistical calculations in far-advanced glaucomatous visual field loss.Ophthalmology2003;110(1):196-200.
Citation:Sencanic I, Gazibara T, Dotlic J, Stamenkovic M, Jaksic V,Bozic M, Grgurevic A. Validation of the Glaucoma Quality of Life-15 Questionnaire in Serbian language.Int J Ophthalmol2018;11(10):1674-1684
DOl:10.18240/ijo.2018.10.16
Accepted:2018-08-25
Received:2018-04-18
Correspondence to:Anita Grgurevic. Institute of Epidemiology,Faculty of Medicine, University of Belgrade, Visegradska 26a,PO Box 20, 11129 Belgrade 102, Serbia. anita.grgurevic@gmail.com