
Figure 1 Rate of post-cataract surgery endophthalmitis by type of surgery
Phaco converted to ECCE was defined as phaco surgery which is converted to a larger incision surgery (ECCE) to extract the nucleus.
Yong Zheng Wai1, Fiona Lee Min Chew2, Mohamad Aziz Salowi2,3, Chai Liang Ang4, Yong Yuin Chong5,Tassha Hilda Adnan6, Pik-Pin Goh6
1Department of Ophthalmology, Hospital Tuanku Jaafar Seremban, Seremban 70300, Malaysia
2Department of Ophthalmology, Hospital Selayang, Batu Caves 68100, Malaysia
3Department of Ophthalmology, Faculty of Medicine,University Sultan Zainal Abidin, Kuala Terengganu 21300,Malaysia
4Department of Emergency Medicine, Hospital Teluk Intan,Teluk Intan 36000, Malaysia
5Faculty of Medicine, MAHSA University, Kuala Lumpur 50603, Malaysia
6Clinical Research Centre, Hospital Kuala Lumpur, Kuala Lumpur 53000, Malaysia
Abstract
●AlM:To report the incidence, risk factors and visual outcomes for postoperative endophthalmitis (POE) based on 7-year data from the Malaysian Ministry of Health Cataract Surgery Registry (MOH CSR).
●METHODS:Data was collected from the web-based MOH CSR. All consecutive cataract surgery patients from 1stJune 2008 to 31stDecember 2014 were identified.Exclusion criteria were traumatic cataract or previous ocular surgery. Demographic data, ocular co-morbidities,intraoperative details and postoperative visual acuity (VA)at final ophthalmological follow-up were noted. All eyes were taken for analysis. Subjects with POE were compared against subjects with no POE for risk factor assessment using multiple logistic regressions.
●RESULTS:A total of 163 503 subjects were screened. The incidence of POE was 0.08% (131/163 503). Demographic POE risk factors included male gender (OR: 2.121, 95%Cl:1.464-3.015) and renal disease (OR: 2.867, 95%Cl: 1.503-5.467). POE risk increased with secondary causes of cataract (OR: 3.562, 95%Cl: 1.740-7.288), uveitis (OR:11.663, 95%Cl: 4.292-31.693) and diabetic retinopathy (OR:1.720, 95%Cl: 1.078-2.744). lntraoperative factors reducing POE were shorter surgical time (OR: 2.114, 95%Cl: 1.473-3.032), topical or intracameral anaesthesia (OR: 1.823,95%Cl: 1.278-2.602), posterior chamber intraocular lens(PClOL; OR: 4.992, 95%Cl: 2.689-9.266) and foldable lOL (OR: 2.276, 95%Cl: 1.498-3.457). POE risk increased with posterior capsule rupture (OR: 3.773, 95%Cl: 1.915-7.432) and vitreous loss (OR: 3.907, 95%Cl: 1.720-8.873).Postoperative VA of 6/12 or better was achieved in 15.27%(20/131) subjects with POE.
●CONCLUSlON:This study concurs with other studies regarding POE risk factors. Further strengthening of MOH CSR data collection process will enable deeper analysis and optimization of POE treatment.
●KEYWORDS:cataract; endophthalmitis; eye; infection;surgery
A cute postoperative infectious endophthalmitis (POE)is a dreaded complication of cataract surgery. It occurs within 6wk post surgery, with a mean presentation of 6 to 8d after surgery[1]. The incidence of POE is documented to range from 0.023% to 0.43%[2-3]. Bacterial causes represent the most common causes, namely coagulase negative staphylococci(70%) and gram-positive cocci (25%)[4-5]. Precautions for POE prevention include prophylactic preoperative antibiotics,aseptic techniques and postoperative ocular and systemic antibiotics. Treatment of POE includes intravitreal antibiotics and early vitrectomy[6-7]. Ocular sequelae range from transient anterior chamber inflammation to necrotic retinitis and retinal detachment. Early detection may lead to salvageable vision.
Cataract surgery is on the rise in Malaysia with a documented increase from 12 798 cases performed in 2002 to 44 534 cases performed in 2015[8]. The average rate for POE in Malaysiawas estimated to range from 0.04% to 0.2%[8-10]. Based on this estimate, the Malaysian Ministry of Health set the national standard for POE at less than 0.2%[9]. Limited information however exists regarding updated epidemiological and surgical factors for POE in Malaysia. Therefore, this paper aims to report the incidence, prevalence, risk factors and visual outcomes for POE based on 7-year data from the Malaysian Ministry of Health Cataract Surgery Registry (MOH CSR).
This is a retrospective cross-sectional study. The study was registered with the National Medical Research Registry and obtained ethical approval from the Medical Research and Ethics Committee of the Ministry of Health of Malaysia.The study conformed to the guidelines of the Declaration of Helsinki and was compliant to all local laws. Data was collected from the web-based MOH CSR. The MOH CSR is a division of the National Eye Database (NED), which collects information from 43 participating cataract centers in Malaysia[11]. These centers performed systematic data entry for consecutive cataract surgery according to predefined sets of preoperative, operative and outcome forms. The case report or data collection forms (CRFs), were developed by a team of ophthalmologists, optometrists, data managers and statisticians. The variables included in the CRFs were agreed upon at the national level before being tested in pilot studies.Data entry in each participating center was performed by the ophthalmology trained doctors under the supervision of on-site coordinators and optometrists to ensure complete, updated and standard method of data collection and entry.
All consecutive patients who underwent cataract extraction from 1stJune 2008 to 31stDecember 2014 were identified as potential study subjects. Patients were excluded if they had traumatic cataract or had previous ocular surgery. Data were collected using the standardized CRF forms and entered directly into the web system. For demography, information of interest included age, gender, ethnicity and medical illnesses such as diabetes, hypertension and renal disease. Ocular comorbidities included preoperative visual acuity (VA), cause of cataract (except traumatic cataract), glaucoma, uveitis,pseudoexfoliation and diabetic retinopathy. Intraoperative details comprised of surgeon status, type of admission,duration and type of surgery, anaesthesia used, intraocular lens(IOL) information, posterior capsular rupture (PCR), vitreous loss and zonular dehiscence. Postoperative details were subjects’ VA at final ophthalmological follow-up. All eyes were taken for analysis. Subjects with POE were compared against subjects with no POE (control group) for risk factor assessment. The subjects were further divided into 2 agecategories which were less than and more than 75 years of age. The mean duration of presentation of POE was compared against subjects’ preoperative and postoperative VA.

Figure 1 Rate of post-cataract surgery endophthalmitis by type of surgery
Phaco converted to ECCE was defined as phaco surgery which is converted to a larger incision surgery (ECCE) to extract the nucleus.
Statistical MethodsIBM SPSS Statistics 20 (IBM SPSS Statistics for Windows, IBM) was used to for data analysis.Continuous variables were presented by mean and standard deviation for normally distributed data. Skewed data were presented by median and IQR. Categorical variables were described in frequency and percentage. Multiple logistic regressions were used to estimate odds ratio (OR) and 95%confidence intervals (CI).P-values less than 0.05 were considered statistically significant
A total of 163 503 subjects were screened and the incidence of POE was 0.08% (131/163 503). When analyzed by year, POE was noted to decrease from 0.11% (18/16 790) in the year 2008 to 0.06% (19/29 840) in the year 2014. Phacoemulsification had the lowest percentage of POE (0.07%, 88/131 180),followed by extra-capsular cataract extraction (ECCE; 0.10%,26/26 267) and other cataract surgery (phaco convert ECCE and intracapsular cataract extraction (ICCE; 0.29%, 17/5925;Figure 1).
The patients with POE had a median age of 64y [mean age 62.18y, standard deviation (SD): 13.44]. The mean presentation of POE was 26.1d. Age and ethnicity did not influence POE.Males represented 65.65% (86/131) of the study population and were noted to have a higher risk of POE compared to female subjects (OR: 2.121, 95%CI: 1.464-3.015,P=0.001).Renal disease was a significant risk factor for POE (OR: 2.867,95%CI: 1.503-5.467,P=0.001; Table 1). The mean POE for the group with preoperative VA 6/12 or better was 27.6d (SD:21.08), while the mean POE for the group with preoperative VA worse than 6/12 was 25.84d (SD: 34.74). The difference between the 2 groups was not statistically significant with theP-value of 0.42.
Pre-operative vision did not influence POE. Secondary causes of cataract were noted to be associated with a higher risk of POE (OR: 3.562, 95%CI: 1.740-7.288,P=0.001). Subjectswith uveitis (OR: 11.663, 95%CI: 4.292-31.693,P=0.001)and diabetic retinopathy (OR: 1.720, 95%CI: 1.078-2.744,P=0.023) had significantly higher incidence of POE (Table 2).Surgeon status (P=0.417) and type of admission (P=0.716)did not affect the incidence of POE. Surgical time of 45min or longer was associated with a 2-fold increased risk of POE (OR:2.114, 95%CI: 1.473-3.032,P=0.001). Topical or intracameral anaesthesia appeared to be protective from POE (OR: 1.823,95%CI: 1.278-2.602,P=0.027). Placement of posterior chamber intraocular lens (PCIOL; OR: 4.992, 95%CI: 2.689-9.266,P=0.001) and foldable IOL (OR: 2.276, 95%CI: 1.498-3.457,P=0.04) had reduced POE. PCR (OR: 3.773, 95%CI:1.915-7.432,P=0.001) and vitreous loss (OR: 3.907, 95%CI:1.720-8.873,P=0.001) significantly increased the risk of POE(Table 3).
Table 1 Patient demographics with POE
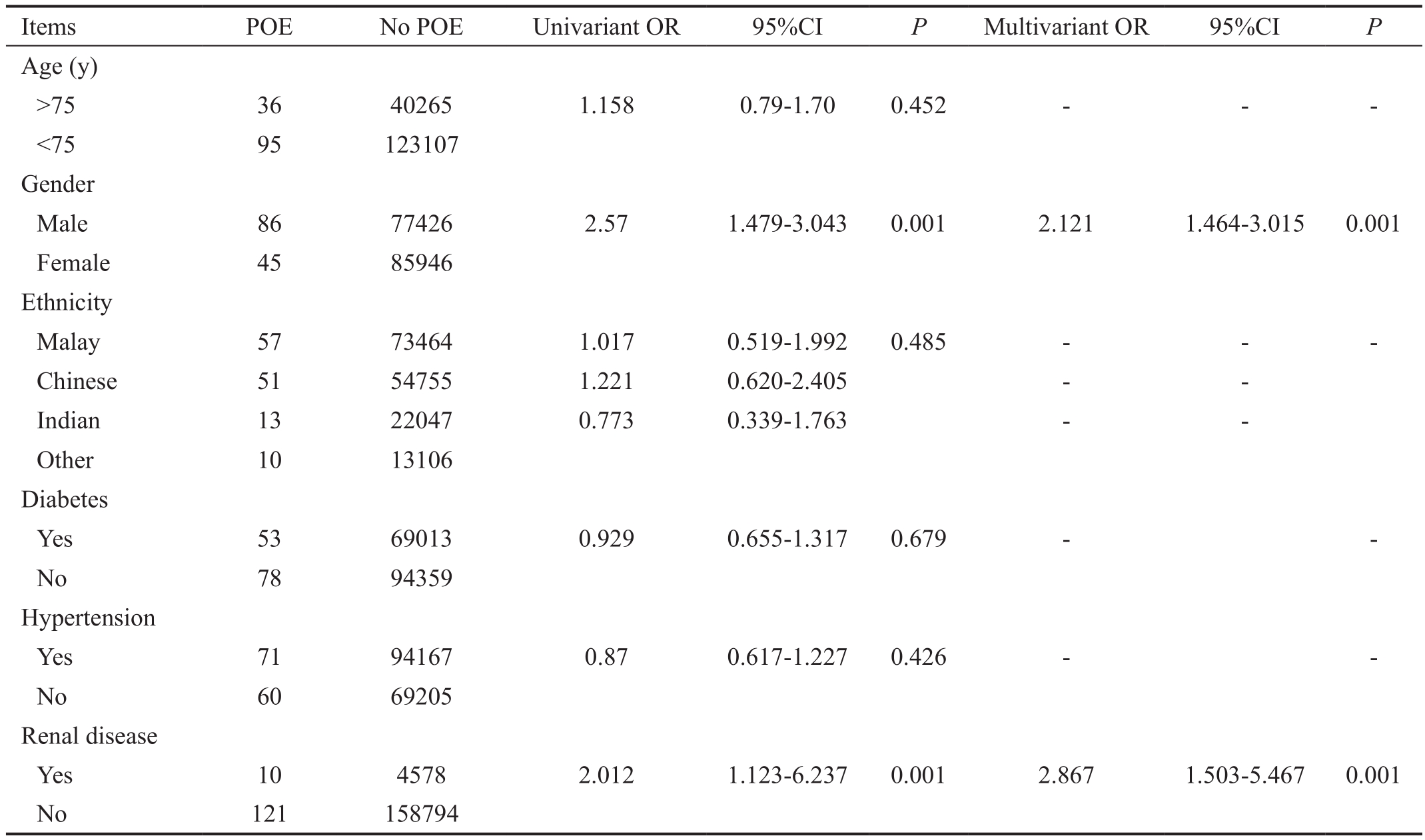
POE: Postoperative endophthalmitis.
Table 2 Preoperative ocular co-morbidities with POE
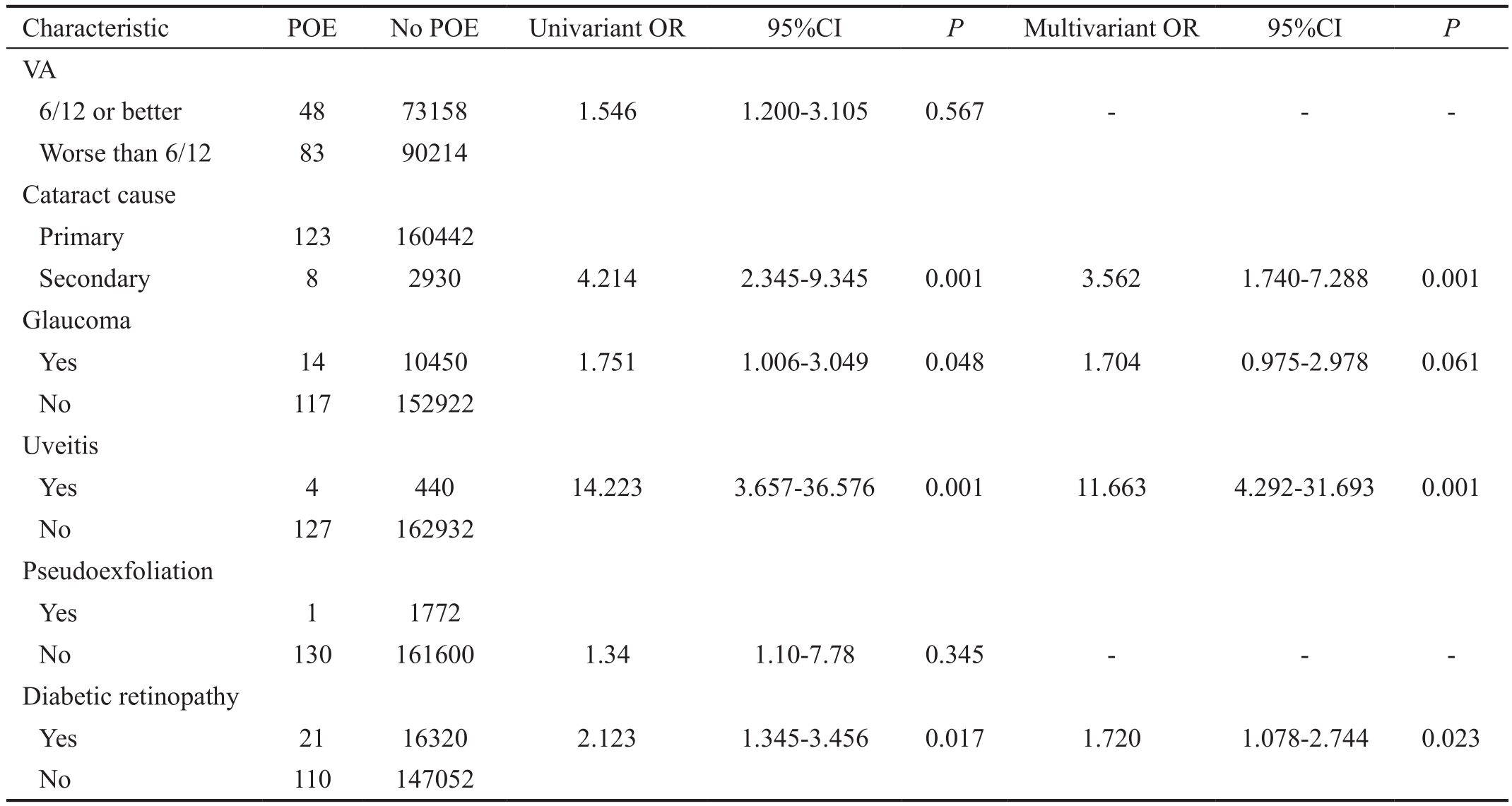
VA: Visual acuity; POE: Postoperative endophthalmitis.
Table 3 Intraoperative complication, postoperative VA with POE

POE: Postoperative endophthalmitis; Phaco: Phacoemulsification; ECCE: Extracapsular cataract extraction; IOL: Intraocular lens; ACIOL:Anterior chamber intraocular lens; PCIOL: Posterior chamber intraocular lens.
Postoperative VA of 6/12 or better was achieved in 15.27%(20/131) subjects with POE. POE was associated with a 4.534 risk of subjects achieving a final VA or worse than 6/12(95%CI: 2.816-7.300,P=0.001; Figure 2). The mean POE for the group with postoperative VA 6/12 or better was 27.9d (SD:40.59), while the mean POE for group postoperative VA worse than 6/12 was 24.53d (SD: 24.14). However, there was no statistical difference between the 2 groups with theP-value of 0.071.
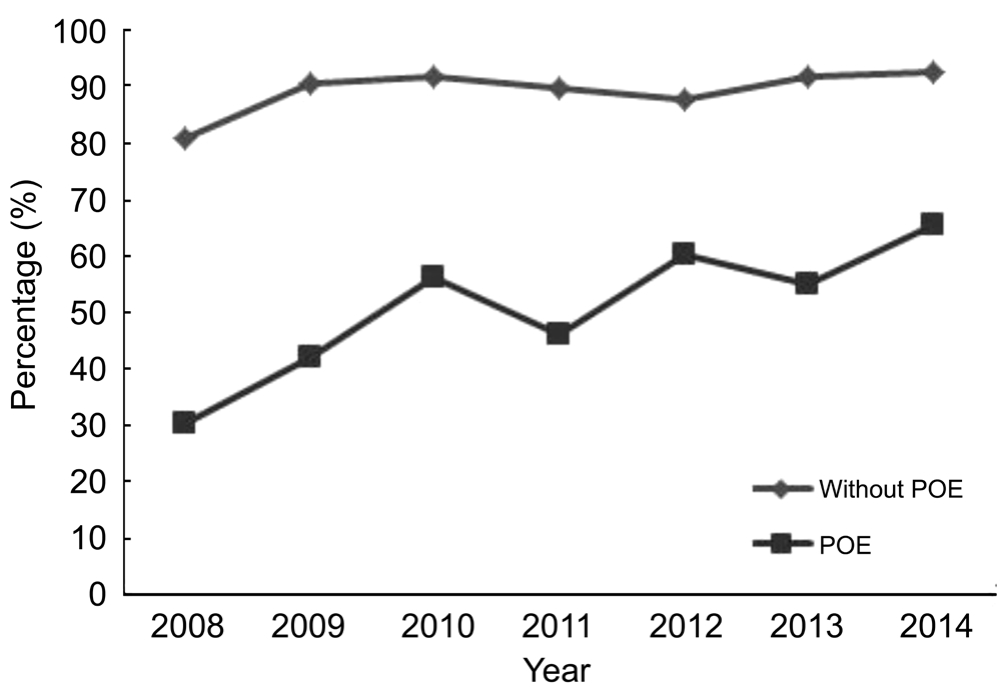
Figure 2 Percentage of post-operative VA 6/12 or better by eyes without POE and POE.
Our study incidence POE of 0.08% was consistent with local and international published studies[2-3,9-10]. The yearly incidence of POE showed a decreasing trend. This could be due to the introduction of newer POE prevention techniques,better surgical techniques and improved acceptance of phacoemulsification[8,12-13]. Phacoemulsification was shown to be superior to other techniques of cataract extraction for prevention of POE. This was due to smaller surgical incision and reduced surgical operating time[14]. Our findings of male gender being a risk factor for POE was similar to other reported studies[15]. It has been reported that male subjects may have different ocular flora, varying compliance to medication and possibly be on alpha antagonists which may lead to floppy iris syndrome which may complicate cataract surgery[16]. We noted renal disease significantly increased the risk of POE. This maybe a result of renal patients, especially those on dialysis having reduced innate immunity and increased risk of vascular accessrelated infections[17]. Secondary cataract was a risk factor for POE. This could be related to the cause of cataract as steroidinduced cataract patients would have reduced immunity and uveitic cataract patients may have complicated cataract with excessive inflammation postoperatively. Interestingly, we noted that although diabetes was not associated with POE,patients with diabetic retinopathy had a slightly increased risk of POE. Though we were unable to analyse the extent of diabetic retinopathy, it was reported that diabetic retinopathy is an indicator of poor diabetic control[18]. This may explain why these patients had increased risk of POE as they would have impaired innate immunity secondary to poor diabetic control.We also noted increased surgical duration was associated with POE. This would be secondary to increased exposure of intraocular contents to the external environment and may indicate complexity of surgery and possible complications intraoperatively. Though topical or intracameral anaesthesia appeared to be protective of POE, this data may be skewed as surgeons tend to give stronger anaesthesia such as subtenon or peribulbar anaesthesia for anticipated difficult cases and if complications occur intraoperatively. Placement of IOL and foldable IOL would be an indicator of uneventful surgery rather than a protective factor for POE. We noted that disruption of the vitreous phase was consistent with increased risk of POE. This was supported by reported literature[19]. Our study subjects with POE had worse final VA for POE compared to reported literature who reported that 43% achieved VA of 20/40 or better[4,20]. This may be due to different organisms,delayed presentation or varying follow-up as the data collected was only up to 3mo postoperatively. More research however needs to be done in this.
Preventive measures suggested for endophthalmitis include hand disinfection with povidone-iodine (PVI) 10% or chlorhexidine gluconate, instillation of PVI 5% into the conjunctiva sac, meticulous draping of eyelashes and intracameral antibiotics[21-22]. In view all our patients had routine intracameral antibiotics as per Malaysian Ministry of health protocol since 2007, it may be variations of other preventive measures, which led to endophthalmitis.Variation in preventive measures however was not included in the NED data collected. Suturing of corneal wounds post phacoemulsification has been documented to reduce the risk of endophthalmitis[23]. This was because wound closure from the oedema induced by stromal hydration has been reported to last from 20min to one week[24-25]. It may be beneficial for surgeons to suture the wounds as a preventive measure in patients with risk factors for endophthalmitis though this requires further research.Limitations of this study were that it was retrospective and data analysed was based on secondary data collected, which may be vulnerable to reporting errors. We were also unable to analyze the causative organisms for endophthalmitis and the follow up period after POE due to limitations of the CSR data entry.
Our study however is still valid as it gives an updated analysis of POE in Malaysia with good representation of all ethnicities.This study concurs with other studies regarding the risk factors for POE though our subjects final VA is worse than reported literature. We believe the study findings will pave the way for upgrading of data collection by the MOH CSR to allow deeper analysis and optimization of POE treatment in the future.
We acknowledge all the health care providers who contributed data to Malaysian Ministry of Health Cataract Surgery Registry(MOH CSR).
Conflicts of Interest:Wai YZ, None; Fiona Chew LM,None; Mohamad AS, None; Ang CL, None; Chong YY,None; Tassha HA, None; Goh PP, None.
REFERENCES
1 Yannuzzi NA, Si N, Relhan N, Kuriyan AE, Albini TA, Berrocal AM, Davis JL, Smiddy WE, Townsend J, Miller D, Flynn HW Jr. Endophthalmitis after clear corneal cataract surgery: outcomes over two decades.AM J Ophthalmol2017;174:155-159.
2 Jabbarvand M, Hashemian H, Khodaparast M, Jouhari M, Tabatabaei A, Rezaei S. Endophthalmitis occurring after cataract surgery. Outcomes of more than 480 000 cataract surgeries, epidemiologic features, and risk factors.Ophthalmology2016;123(2):295-301.
3 Lundström M, Friling E, Montan P. Risk factors for endophthalmitis after cataract surgery: predictors for causative organisms and visual outcomes.J Cataract Refract Surg2015;41(11):2410-2416.
4 Cunningham C, Widder J, Raiji V. Endophthalmitis.Dis Mon2017;63(2):45-48.
5 Durand ML. Endophthalmitis.Clin Microbiol Infect2013;19(3):227-234.
6 Altan T, Acar N, Kapran Z, Unver YB, Yurttaser S, Küçüksümer Y, Eser I. Acute-onset endophthalmitis after cataract surgery. Success of initial therapy, visual outcomes, and related factors.Retina2009;29(5):606-612.
7 Thomas BJ, Mehta N, Yonekawa Y,et al. Pars plana vitrectomy for late vitreoretinal sequelae of infectious endophthalmitis surgical management and outcomes.Retina2017;37(4):651-656.
8 Mohamad Aziz Salowi, Goh PP (Eds).The Ninth Report of the National Eye Database 2015. National Eye Database: Kuala Lumpur, Malaysia, 2016.
9 Goh PP, Hussein E, Mustari Z, Ismail M. The First Annual Report of the National Eye Database 2007. Page 26. Available at http://www.crc.gov.my/wp-content/uploads/documents/report/1stnedReport.pdf.
10 Salowi MA, Goh PP, Yusof NS, Adlina AR, Ruqqayah AK.The 7thReport of the National Eye Database 2013. National Eye Database: Kuala Lumpur, Malaysia, 2014.
11 Goh PP, Elias H, Norfariza N, Mariam I. National Eye Database-a web based surveillance system.Med J Malaysia2008;63(Suppl C):20-23.
12 Salowi MA, Chew FLM, Adnan TH, King C, Ismail M, Goh PP. The Malaysian Cataract Surgery Registry: risk indicators for posterior capsular rupture.Br J Ophthalmol2017;101(11):1466-1470.
13 Garg P, Roy A, Sharma S. Endophthalmitis after cataract surgery:epidemiology, risk factors, and evidence on protection.Curr Opin Ophthalmol2017;28(1):67-72.
14 Relhan N, Forster RK, Flynn Jr HW. Endophthalmitis: then and Now.Am J Ophthalmol2018;e-pub ahead of print 4 December 2017.
15 Hashemian H, Mirshahi R, Khodaparast M, Jabbarvand M. Postcataract surgery endophthalmitis: Brief literature review.J Curr ophthalmol2016;28:101-105.
16 Cao H, Zhang Lu, Li L, Lo SK. Risk factors for acute endophthalmitis following cataract surgery: a systematic review and Meta-analysis.PLoS One2013;8(8):e71731.
17 Kuo G, Lu YA, Sun WC, Chen CY, Kao HK, Lin Y, Lee CH, Hung CC, Tian YC, Hsu HH. Epidemiology and outcomes of endophthalmitis in chronic dialysis patients: a 13-year experience in a tertiary referral center in Taiwan.BMC Nephrol2017;18(1):270.
18 Fenwick EK, Xie J, Man REK, Sabanayagam C, Lim L, Rees G, Wong TY, Lamoureux EL. Combined poor diabetes control indicators are associated with higher risks of diabetic retinopathy and macular edema than poor glycemic control alone.PLoS One2017;12(6):e0180252.
19 Zhu Y, Chen X, Chen P, Wu J, Hua H, Yao K. The occurrence rate of acute-onset postoperative endophthalmitis after cataract surgery in Chinese small- and medium-scale departments of ophthalmology. Sci Rep2017;7(1):40776.
20 Gower EW, Keay LJ, Stare DE, Arora P, Cassard SD, Behrens A,Tielsch JM, Schein OD. Characteristics of endophthalmitis after cataract surgery in the United States medicare population. Ophthalmology2015;122(8):1625-1632.
21 Packer M, Chang DF, Dewey SH, Little BC, Mamalis N, Oetting TA,Talley-Rostov A, Yoo SH. Prevention, diagnosis, and management of acute postoperative bacterial endophthalmitis.J Cataract Refract Surg2011;37(9):1699-1714.
22 Nguyen CL, Oh LJ, Wong E, Francis IC. Povidone-iodine 3-minute exposure time is viable in preparation for cataract surgery.Eur J Ophthalmol2017;27(5):573-576.
23 Thoms SS, Musch DC, Soong HK. Postoperative endophthalmitis associated with sutured versus unsutured clear corneal cataract incision.Br J Ophthalmol2007;91:728-730.
24 Ku JJ, Wei MC, Amjadi S, Montfort JM, Singh R, Francis IC. Role of adequate wound closure in preventing acute postoperative bacterial endophthalmitis.J Cataract Refract Surg2012;38(7):1301-1302.
25 Fukuda S, Kawana K, Yasuno Y, Oshika T. Wound architecture of clear corneal incision with or without stromal hydration observed with 3-dimensional optical coherence tomography.Am J Ophthalmol2011;151(3):413-419.
Citation:Wai YZ, Fiona Chew LM, Mohamad AS, Ang CL, Chong YY, Tassha HA, Goh PP. The Malaysian cataract surgery registry:incidence and risk factors of postoperative infectious endophthalmitis over a 7-year period.Int J Ophthalmol2018;11(10):1685-1690
DOl:10.18240/ijo.2018.10.17
Accepted:2018-04-23
Received:2018-01-24
Correspondence to:Yong Zheng Wai. Department of Ophthalmology, Hospital Tuanku Jaafar Seremban, Seremban 70300, Malaysia. yong_zheng92@hotmail.com