Endothelial parameters in central and peripheral cornea in patients wearing contact lenses
Saulius Galgauskas1, Justina Ignataviciute1, Zivile Vieversyte2, Rimvydas Asoklis1
1Vilnius University, Center of eye diseases, Vilnius 08661,Lithuania
2Faculty of Medicine, Vilnius University, Vilnius 08661,Lithuania
Abstract
● AlM:To measure the parameters of endothelium in the central and peripheral parts of the cornea and evaluate the infuence of wearing the hard and soft contact lenses on the mentioned parameters.
● METHODS:A specular microscope was used to measure the corneal endothelium parameters in both eyes of 139 Caucasians (a total of 278).All participants were divided into three groups: soft lens wearers, hard lens wearers and a control group.Factors, such as age, smoking,types of lens material, duration of lens wear and lens air permeability were assessed to determine their impact on the morphometric parameters of the endothelium.
● RESULTS:A lower percentage of hexagon-like cells and higher cell variation than in other groups were determined in hard contact lens wearers.The difference in density of endotheliocytes between the groups was not observed.The measurements of the morphometric parameters in soft contact lens wearers did not depend neither on the duration of lens wear, nor on air permeability.The relation between the patients’ age and the variation of endothelium parameters was determined in the group of hard contact lens wearers.
● CONCLUSlON:Wearing hard contact lenses provokes pleomorphism and polymegethism of the corneal endothelium, while soft contact lenses do not impact any parameters of the endothelium, most likely due to higher air permeability.
● KEYWORDS:corneal endothelium; morphometry; endothelial changes; contact lenses
INTRODUCTION
Injuries of the corneal endothelium are related to a variety of eye diseases, such as corneal distrophies, critical reduction in the density of endotheliocytes, named as the most common cause of the corneal transplant rejection within fve years after transplantation[1], and recently determined relation between density of endotheliocytes and expression of the symptoms of dry eye syndrome[2].In order to standardize the degree of the corneal endothelial damage, the classification, based on the density of endotheliocytes and corneal changes identifed during ophthalmobiomicroscopy, was suggested in 2014[3].
The studies describing the density of endotheliocytes not only in central but also in the peripheral corneain vivoappeared already in 1977[4].With the possibility of measuring endothelial parameters in the periphery using more and more automated and patient-friendly methods, this was started in order to more accurately predict endothelium changes and their effects after various interventions (e.g.LASIK, lamellar keratoplasty),and to specifcally investigate the potential of endotheliocytes regeneration/proliferation at the corneal periphery which could be used to treat endothelial damage effectively[5-8].
The aim of this research is to measure the corneal endothelium parameters in the central and peripheral corneal areas and to determine the infuence of the wear of soft and hard contact lenses on changes in these parameters in the Lithuanian population.
SUBJECTS AND METHODS
After receipt of an informed consent, 139 Caucasian patients(a total of 278 eyes) were involved to the research.Totally 31 males and 108 females at the age from 18 to 68 (33.12±19.97)y were involved.All participants had no anterior segment diseases,diabetes mellitus, no eye injuries or surgical treatment in anamnesis.All of them were divided into three groups: soft contact lens wearers (SCL), hard contact lens wearers (HCL)and a control group (CG) which included participants who have never worn contact lenses.Patients’ anamnesis was collected on the following: age, sex, smoking, duration of contact lenses wear, type of contact lenses (daily-wear/ monthly-wear/conventional-wear), type of contact lens material [silicone (Si)/hydrogel (Hy)/ silicone-hydrogel (SiHy)/ rigid gas permeable(RGP)/ polymethyl methacrylate (PMMA)].
Central corneal thickness (CCT) and parameters of endothelium were assessed in central and six peripheral points of the cornea using a specular microscope (Topcon SP-1P).Examination of the endothelium included endothelial cell density (ECD),polymegethism (variation of cells size-CV %) and pleomorphism(percentage of hexagon-like cells-HEX %).Only the data obtained after measuring at least 60 endotheliocytes were used in the research.
IBM SPSS®20.0 (IBM Corporation, Armonk, NY, USA) and Microsoft Excel®2007 (Microsoft Corporation, Redmond,WA, USA) were used for the statistical analysis.Student’st-test and Pearson’s correlation coefficient (r) values were calculated.The data were considered statistically signifcant atP<0.05.
This study was approved by the Human Ethics Committee of Vilnius University Faculty of Medicine.
RESULTS
The CG included 67 participants: 20 males and 47 females aged from 21 to 68 (32.64±13.18)y.The group of the SCL consisted of 37 participants [6 males and 31 females aged from 23 to 45 (25±3.05)y] and the group of the HCL had 40 patients:5 males and 35 females at the age from 18 to 64 (42±12.81)y.Distribution of endothelial parameters in the examined points is shown in Table 1 (CG), Table 2 (HCL) and Table 3 (SCL).ECD varied from 1678.5 to 4421 cells/mm2and in superior corneal point was statistically signifcantly higher in all groups(P=0.002; Figure 1).ECD in the central cornea in CG and HCL groups was statistically significantly lower than in the peripheral points (P=0.002; Figure 1).Statistically signifcant ECD difference between all groups was not observed in any of the examined corneal points [center (C)P=0.02, superior(S)P=0.04, inferior (I)P=0.25, nasosuperior (NS)P=0.1,nasoinferior (NI)P=0.09, temporosuperior (TS)P=0.02,temporoinferior (TI)P=0.04].
The lowest CV was measured in the CG (20%), the highest in the group of HCL and the CG (52.50%).CV in HCL group was statistically significantly higher than in SCL and CG (P<0.001; Figure 2).The lowest HEX was measured in HCL group (28.5%), the highest in CG (81%).HEX in HCL group was statistically signifcantly lower than in SCL and CG(P<0.001; Figure 3).
Average measurement of CCT was 528.25±37.01 µm(ranged from 452 to 662 µm).CCT measured in the CG was 526.82±38.73 µm (ranged from 370 to 623 µm).In the SCL group 534.05±35.18 µm (ranged from 468 to 662 µm),HCL group 524.85±35.85 µm (ranged from 452 to 584 µm).Statistically signifcant CCT difference between all groups was not observed (P=0.52).Neither ECD, nor CV or HEX did not depend on CCT (Pvalues, respectively, 0.41, 0.74 and 0.66).There was a weak negative correlation between ECD and HEX with age in the CG (Table 4).
The CG included 9 smokers and 58 non-smokers.The group of SCL had 13 and 24, and the group of HCL had 5 and 30,respectively.In total there were 27 smokers and 112 nonsmokers.In SCL group, longer time of smoking was associated with a reduction in the values of ECD (Table 5).According to the significance value, there was no correlation between the parameters and smoking (Table 6).
Table 1 Corneal endothelium parameters values in control group

SD: Standard deviation.
Parameters Localization Mean SD Endothelial cell density (cell/mm2)Central 2899.22 295.74 Superior 3346.52 420.70 Inferior 2986.15 320.12 Nasosuperior 2980.49 325.87 Nasoinferior 2986.58 316.95 Temporosuperior 3064.08 343.04 Temporoinferior 3029.38 336.61 Polymegethism(%)Central 57.35 6.82 Superior 55.24 7.49 Inferior 59.80 6.69 Nasosuperior 62.45 8.21 Nasoinferior 60.88 7.63 Temporosuperior 59.40 7.62 Temporoinferior 57.35 6.82 Central 29.91 3.34 Superior 33.50 5.00 Inferior 30.05 4.08 Nasosuperior 30.56 4.46 Nasoinferior 30.05 4.48 Temporosuperior 31.05 4.19 Temporoinferior 29.45 3.67 Pleomorphism(%)
Table 2 Corneal endothelium parameters values in hard contact lens wearers

SD: Standard deviation.
Parameters Localization Mean SD Endothelial cell density(cell/mm2)Central 2982.41 365.02 Superior 3249.02 430.16 Inferior 3078.60 401.45 Nasosuperior 3108.00 366.33 Nasoinferior 3089.41 428.86 Temporosuperior 3194.80 407.21 Temporoinferior 3078.14 423.05 Polymegetism(%)Central 48.52 7.27 Superior 48.97 5.99 Inferior 51.04 6.34 Nasosuperior 52.54 7.78 Nasoinferior 54.41 9.32 Temporosuperior 51.62 6.37 Temporoinferior 48.52 7.27 Central 36.04 4.21 Superior 36.32 6.08 Inferior 34.84 5.44 Nasosuperior 35.42 6.46 Nasoinferior 34.10 5.53 Temporosuperior 35.10 4.70 Temporoinferior 33.35 3.61 Pleomorphism(%)

Figure 1 Distribution of the endothelial cell density in various corneal points.

Figure 2 Distribution of megethism in various corneal points.
Table 3 Corneal endothelium parameters values in soft contact lens wearers

SD: Standard deviation.
Parameters Localization Mean SD Endothelial cell density(cell/mm2)Central 3084.66 345.92 Superior 3479.91 313.19 Inferior 3079.31 266.93 Nasosuperior 3103.54 352.63 Nasoinferior 3126.75 267.89 Temporosuperior 3241.44 270.62 Temporoinferior 3206.72 266.24 Polymegetism(%)Central 56.56 6.82 Superior 58.44 7.67 Inferior 60.40 8.01 Nasosuperior 63.79 7.04 Nasoinferior 61.52 8.41 Temporosuperior 60.75 7.40 Temporoinferior 56.56 6.82 Central 29.81 3.09 Superior 32.05 4.81 Inferior 29.08 3.25 Nasosuperior 29.21 3.34 Nasoinferior 29.33 3.17 Temporosuperior 30.04 3.38 Temporoinferior 28.94 2.93 Pleomorphism(%)

Figure 3 Distribution of pleomorphism in various corneal points.
Table 4 Correlation between endothelial parameters and age

Group ParametersPCorrelation(Pearson)Control Endothelial cell density 0.000 -0.490 Polymegethism 0.273 Pleomorphism 0.000 -0.430 Soft contactEndothelial cell density 0.131 lensPolymegethism 0.152 Pleomorphism 0.116 Hard contactEndothelial cell density 0.259 lens (PMMA/Polymegethism 0.033 RGP)Pleomorphism 0.731
Table 5 Correlation between endothelial parameters and duration of smoking

aAll participants-smokers.
GroupaParameters (periphery)P(Pearson)Correlation Control Endothelial cell density 0.878 Polymegethism 0.098 Pleomorphism 0.022 Soft contact lens Endothelial cell density 0.004 -0.742 Polymegethism 0.238 Pleomorphism 0.424 Hard contact lens(PMMA/RGP)Endothelial cell density 0.886 Polymegethism 0.396 Pleomorphism 0.126
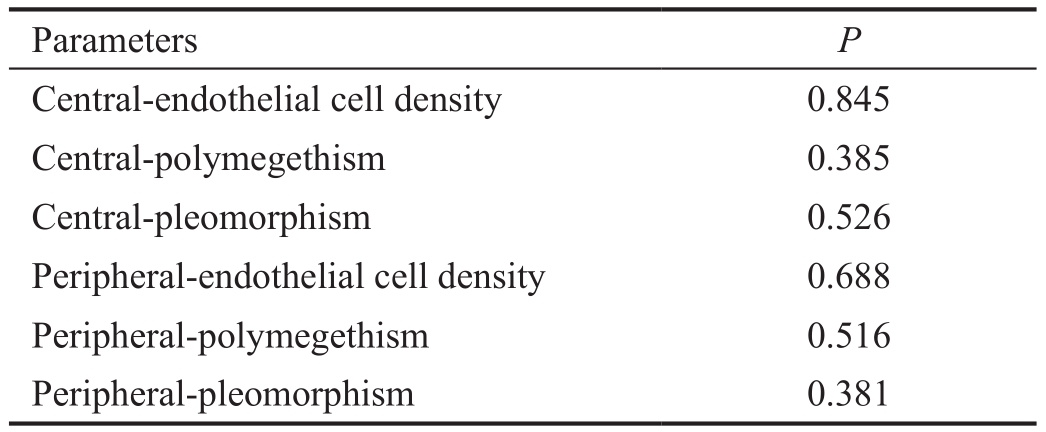
The duration of lenses wear in SCL group varied from 3 to 144mo (62.54±40.63mo).In this group, there was no correlation between duration and other parameters (Table 7).Daily-wear lenses were worn by 1 (2.7%), monthly-wear by 36(97.3%) participants.This is why the impact of lenses wearing mode was not evaluated.Permeability of oxygen in SCL group varied from 19.7 to 175.Permeability of oxygen had no statistically significant impact on the studied parameters(Table 8).Using the linear regression method and measuring infuence of permeability of oxygen, duration of lens wear and mode, on all parameters of endothelium, revealed that none of these factors had more impact than others (Table 9).
Table 6 Correlation between endothelial parameters and smoking

SD: Standard deviation.
Group S+/S- Parameters Mean SDP(Pearson)Control Smokers (S+) Endothelial cell density 2896.73 cell/mm2312.68 0.200 Polymegethism 32.69% 4.99 0.200 Pleomorphism 57.95% 6.29 0.177 Non-smokers (S-) Endothelial cell density 3091.73 cell/mm2312.68 0.200 Polymegethism 30.48% 3.72 0.078 Pleomorphism 59.38% 5.99 0.200 Soft contact lens S+ Endothelial cell density 3197.46 cell/mm2277.35 0.200 Polymegethism 30.23% 3.40 0.200 Pleomorphism 60.39% 6.09 0.200 S- Endothelial cell density 3211.05 cell/mm2247.77 0.200 Polymegethism 29.53% 2.76 0.200 Pleomorphism 60.17% 6.31 0.117 Hard contact lens (PMMA/RGP) S+ Endothelial cell density 2880.63 cell/mm2411.19 0.146 Polymegethism 32.70% 4.18 0.200 Pleomorphism 52.31% 5.69 0.200 S- Endothelial cell density 3175.05 cell/mm2334.40 0.062 Polymegethism 35.21% 4.58 0.200 Pleomorphism 51.00% 5.43 0.200
Table 7 Correlation between endothelial parameters and duration of soft contact lens wear

ParametersPCentral-endothelial cell density 0.068 Central-polymegethism 0.109 Central-pleomorphism 0.160 Peripheral-endothelial cell density 0.508 Peripheral-polymegethism 0.384 Peripheral-pleomorphism 0.630
Table 8 Correlation between endothelial parameters and soft contact lens permeability of oxygen
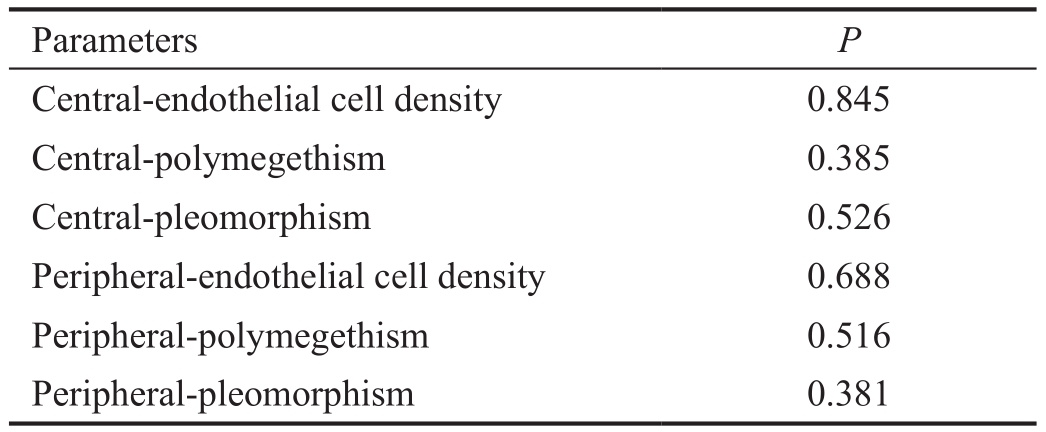
ParametersPCentral-endothelial cell density 0.845 Central-polymegethism 0.385 Central-pleomorphism 0.526 Peripheral-endothelial cell density 0.688 Peripheral-polymegethism 0.516 Peripheral-pleomorphism 0.381
In HCL group PMMA lenses were worn by 11 (31.42%)participants, RGP by 8 (22.85%) participants.Totally 16 (45.71%) patients at frst wore PMMA lenses which later were changed into RGP-these participants were assessed as mixed wearers.The type of contact lens material did not make any statistically signifcant impact on endothelial parameters.Measuring in the central cornea (C) ECDP=0.206, CVP=0.146, HEXP=0.491, in the peripheral cornea (P) ECDP=0.029, CVP=0.070, HEXP=0.048.PMMA lenses were being worn from 12 to 492 (242.33±122.71)mo, BostonXO from 24 to 204 (112.83±53.20)mo.PMMA lenses were being worn statistically significantly longer than Boston XO(P=0.000).Duration of lenses wear did not have any impact on endothelium parameters (C) ECDP=0.903, CVP=0.069, HEXP=0.249, (P) ECDP=0.682, CVP=0.012, HEXP=0.011.Based on the linear regression method, participants’ age had a statistically signifcant impact on ECD in the peripheral cornea(Table 10).
Table 9 Various predictors impact on endothelial parameters in soft contact lens group

Parameters PredictorsPCentral-endothelial cell density Dk/t 0.948 Duration 0.518 Schedule 0.127 Central-polymegethism Dk/t 0.711 Duration 0.194 Schedule 0.252 Central-pleomorphism Dk/t 0.954 Duration 0.031 Schedule 0.200 Peripheral-endothelial cell density Dk/t 0.319 Duration 0.614 Schedule 0.010 Peripheral-polymegethism Dk/t 0.757 Duration 0.540 Schedule 0.303 Peripheral-pleomorphism Dk/t 0.736 Duration 0.119 Schedule 0.275
Table 10 Various predictors impact on endothelial parameters in hard contact lens (PMMA/RGP) group

Parameters PredictorsPCentral-endothelial cell density Material 0.078 Duration of wear 0.040 Age 0.016 Central-polymegethism Material 0.934 Duration of wear 0.734 Age 0.308 Central-pleomorphism Material 0.642 Duration of wear 0.157 Age 0.357 Peripheral-endothelial cell density Material 0.016 Duration of wear 0.010 Age 0.001 Peripheral-polymegethism Material 0.254 Duration of wear 0.617 Age 0.177 Peripheral-pleomorphism Material 0.442 Duration of wear 0.101 Age 0.892
DISCUSSION
HCL group had a higher pleomorphism and polymegethism than other groups.Many of the studies published so far point out both CV and HEX changes in wearing contact lenses[9-10].In 2001, Leeet al[11]wrote about the difference in the variation of cells size between those, who did not wear contact lenses,and those, who had a history of wearing lenses for at least 10y (respectively 22%-29% and 26%-33%).HEX percentage reduction was from 59.4%-71% in those not wearing lenses and up to 47.5%-70% when wearing lenses for a minimum of ten years[11].In wearing contact lenses, a more significant variation of the parameters from the norm correlates with the corneal hypoxia[12].Possibly, analogical changes were not discovered in SCL group because of lenses’ higher oxygen permeability.It is important to note that in HCL group the average of patients’ age was higher than in other groups.Different authors have contradicting opinions about the impact of age on pleomorphism and polymegethism.Some of them state that the age has no infuence on rates, while others claim that they increase with age[12-14].Some authors state that the expression of pleomorphism takes time and it is not such a change of endothelium that can be quickly revealed,yet it is a highly sensitive marker of the endothelial damage and instability[12].Neither change of CV, nor of HEX causes corneal decompensation or clinical expression.Meanwhile,CV increase and HEX decrease are related to the subsequent reduction of ECD and are considered to be its precursors[12].
In HCL group, ECD statistically significantly did not differ from SCL and CG and its mean was not lower in this age group than the one mentioned in literature[15-21].This does not interfere with research describing ECD when wearing contact lenses and it is explained by the fact that reduction of endotheliocytes, unlike pleomorphism and polymegethism,it is not an early reaction to stress (mainly hypoxia and hypercapnia[22-23]), but is a late outcome of wearing lens for a long time[12]or does not appear at all after wearing gas permeable lenses[24].ECD decrease with aging, indicated by many sources[13,19,25], was observed only in HCL and CG when measuring endotheliocytes in the corneal periphery.Although it is claimed that the morphometric endothelial parameters are the most stable at the age of 15-50y[11], ECD decrease in SCL group did not show up possibly due to the group very homogenous in age (standard deviation was only 3.05) while the age of participants was more varied in HCL and CG groups.
In HCL and CG, ECD in the central cornea was lower than in the periphery.This is likely to be associated with homogenous age of participants in SCL group.It is assumed that the cause of higher density in the endothelial periphery can be the lack of space for endotheliocytes growth[26].
The corneal pachymetry performed in our investigation showed thinner corneas than the means presented in the research carried out in 2013 in which the Lithuanian population with equal age was examined[14].Small errors are possible due to different methods of measurement.
Corneal thickness did not have any impact to the endothelial morphometric parameters.There are some studies that find no relation between CCT and ECD[26].Others claim that thinner corneas have lower ECD[20,27].It is found that the cornea decompensates and its oedema develops when critical reduction (400-500 cells/mm2) of ECD is reached[26].
Smoking did not have any influence on the endothelial parameters, though it was observed that longer duration of smoking causes endothelial thinning.It is confrmed in Sayinet al[28]research which was performed in 2014.
In SCL group duration of lenses wear and permeability of oxygen did not influence any of the endothelial parameters.The possible impact of duration of wear was not observed due to short time (average 5y).Most sources state that more stable endothelial changes are observed when lenses are worn for at least 6y[11], although there are those who claim that 25y are required[12].Permeability of oxygen had no impact most likely due to highly oxygen permeable contact lenses.After reaching permeability of oxygen of at least 200, open eye oxygenation is the same as without contact lenses[29].This is why literature states that the contemporary materials of contact lenses solve hypoxia[24,30-31].However, it is admitted that the endothelial changes depend not only on hypoxia, but also on hypercapnia[22-23].Therefore, the future works for the manufacturers of lenses will be targeted not only at increase of Dk/t, but also at reduction of hypercapnia.
The evaluation ofthe impact of HCL materials on the corneal endothelium was impossible in this research because of a small sample of patients.Also, the majority of those who wore not oxygen permeable PMMA lenses at frst, after some time changed them to oxygen permeable lenses.Although there were no significant differences inside this group, there was evident CV increase and HEX decrease in HCL group as compared to SCL and CG.
ACKNOWLEDGEMENTS
The authors would like to thank Idalija Baltruniene MD for referring patients for examination.
Conflicts of Interest:Galgauskas S, None; Ignataviciute J,None; Vieversyte Z, None; Asoklis R, None.
REFERENCES
1 Patel SP, Bourne WM.Corneal endothelial cell proliferation: a function of cell density.Invest Ophtalmol Vis Sci2009;50(6):2742-2746.
2 Kheirkhah A, Saboo US, Abud TB, Dohlman TH, Arnoldner MA,Hamrah P, Dana R.Reduced corneal endothelial cell density in patients with dry eye disease.Am J Ophthalmol2015;159(6):1022-1026.e2.
3 Kinoshita S, Amanao S, Inoue Y, Ohashi Y, Takahashi H, Tsubota K, Nishida K.Grading for corneal endothelial damage.Nippon Ganka Gakkai Zasshi2014;118(2):81-83.
4 Wiffen SJ, Hodge DO, Bourne WN.The effect of contact lens wear on the central and peripheral corneal endothelium.Cornea2000;19(1):47-51.
5 Zheng T, Le Q, Hong J, Xu J.Comparison of human corneal cell density by age and corneal location: an in vivo confocal microscopy study.BMC Ophthalmol2016;16:109.
6 Choi SO, Jeon HS, Hyon JY, Oh YJ, Wee WR, Chung TY, Shin YJ, Kim JW.Recovery of corneal endothelial cells from periphery after injury.PLoS One2015;10(9):e0138076.
7 Mimura T, Joyce NC.Replication completence and senescence in central and peripheral human corneal endothelium.Invest Ophthalmol Vis Sci2006;47(4):1387-1396.
8 Amann J, Holley GP, Lee SB, Edelhauser HF.Increased endothelial cell density in the paracentral and peripheral regions of the human cornea.Am J Ophthalmol2003;135(5):584-590.
9 Chang SW, Hu FR, Lin LL.Effects of contact lenses on corneal endothelium-a morphological and functional study.Ophthalmologica2001;215(3):197-203.
10 Carlson KH, Bourne WM, Brubaker RF.Effect of long-term contact lens wear on corneal endothelial cell morphology and function.Invest Ophthalmol Vis Sci1988;29(2):185-193.
11 Lee JS, Park WS, Lee SH, Oum BS, Cho BM.A comparative study of corneal endothelial changes induced by different durations of soft contact lens wear.Graefes Arch Clin Exp Ophthalmol2001;239(1):1-4.
12 Liesegang TJ.Physiologic changes of the cornea with contact lens wear.CLAO J2002;28(1):12-27.
13 Gambato C, Longhin E, Catania AG, Lazzarini D, Parrozzani R, Midena E.Aging and corneal layers: an in vivo corneal confocal microscopy study.Graefes Arch Clin Exp Ophthalmol2015;253(2):267-275.
14 Galgauskas S, Norvydaitė D, Krasauskaitė D, Stech S, Ašoklis RS.Age-related changes in corneal thickness and endothelial characteristics.Clinical Interventions in Aging2013;8:1445-1450.
15 McCarey BE, Edelhauser HF, Lynn MJ.Review of corneal endothelial specular microscopy for FDA clinical trials of refractive procedures,surgical devices and new intraocular drugs and solutions.Cornea2008;27(1):1-16.
16 Zavala J, López Jaime GR, Rodríguez Barrientos CA, Valdez-Garcia J.Corneal endothelium developmental strategies for regeneration.Eye2013;27(5):579-588.
17 Doughty MJ.A prospective analysis of corneal endothelial polymegethism and cell density in young adult Asian.Clin Exp Optom2014;97(3):256-263.
18 Mohammad-Salih PA.Corneal endothelial cell density and morphology in normal Malay eyes.Med J Malaysia2011;66(4):300-303.
19 Higa A, Sakai H, Sawaguchi S, Iwase A, Tomidokoro A, Amano S,Araie M.Corneal endothelial cell density and associated factors in a population-based study in Japan: the Kumejima study.Am J Ophthalmol2010;149(5):794-799.
20 Patel HY, Patel DV, McGhee CN.Identifying relationships between tomography-derived corneal thickness, curvature, and diameter and in vivo confocal microscopic assessment of the endothelium in healthy corneas of young adults.Eye (Lond)2009; 23(2):270-278.
21 Tanaka H, Okumura N, Koizumi N, Sotozono C, Sumii Y, Kinoshita S.Panoramic view of human corneal endothelial cell layer observed by a prototype slit-scaning wide-field contact specular microscope.Br J Ophthalmol2017;101(5):655-659.
22 Leung BK, Bonanno JA, Radke CJ.Oxygen-defcient metabolism and corneal edema.Prog Retin Eye2011;30(6):471-492.
23 Chhabra M, Prausnitz JM, Radke CJ.Modeling corneal metabolism and oxygen transport during contact lens wear.Optom Vis Sci2009;86(5):454-466.
24 Bourne WM.The effect of long-term contact lens wear on the cells of the cornea.CLAO J2001;27(4):225-230.
25 Niederer RL, Perumal D, Sherwin T, McGhee CN.Age-related differences in the normal human cornea: a laser scanning in vivo confocal microscopy study.Br J Ophthalmol2007;91(9):1165-1169.
26 Wörner CH, Olguín A, Ruíz-García JL, Garzón-Jiménez N.Cell patern in adult human corneal endothelium.PLoS One2011;6(5):e19483.
27 Müller A, Craig JP, Grupcheva CN.The effects of corneal parameters on the assessment of endothelial cell density in the elderly eye.Br J Ophthalmol2004;88(3):325-330.
28 Sayin N, Kara N, Pekel G, Altinkaynak H.Effects of chronic smoking on central corneal thickness, endothelial cell, and dry eye parameters.Cutan Ocul Toxicol2014;33(3):201-205.
29 Papas EB.The significance of oxygen during contact lens wear.Contact Lens Anterior Eye2014;37(6):394-404.
30 Sweeney DF.Have silicone hydrogel lenses eliminated hypoxia?Eye Contact Lens2013;39(1):53-60.
31 Nguyen T, Soni PS, Brizendine E, Bonanno JA.Variability in hypoxiainduced corneal swelling is associated with variability in corneal metabolism and endothelial function.Eye Contact Lens2003;29(2):117-125.
Citation:Galgauskas S, Ignataviciute J, Vieversyte Z, Asoklis R.Endothelial parameters in central and peripheral cornea in patients wearing contact lenses.Int J Ophtahlmal2018;11(11):1768-1773
DOl:10.18240/ijo.2018.11.06
Accepted:2018-09-19
Received:2017-11-19
Correspondence to:Zivile Vieversyte.Universiteto str.2,Vilnius 08661, Lithuania.vieversytezivile@gmail.com