
Figure 1 Different macular status preoperatively A: Macula partly detached RRD (Group A1, foveola-on); B: Macula partly detached RRD (Group A1, foveola-off); C: Macula totally detached RRD(Group A2, foveola-off); D: Macula-on RRD (Group B).
Jian-Bo Mao, Jing-Jing Lin, Xue-Ting Yu, Dan Cheng, Yi-Qi Chen, Ji-Wei Tao, Han-Fei Wu, Lu Jiang,Yun Zhang, Li-Jun Shen
The Affiliated Eye Hospital, Wenzhou Medical University,Hangzhou 310000, Zhejiang Province, China
Abstract
● AlM:To compare the incidence of persistent submacular fuid (SMF) and visual outcome after pars plana vitrectomy(PPV) for rhegmatogenous retinal detachment (RRD) in different preoperative macular status according to optical coherence tomography (OCT).
● METHODS:A non-randomized, retrospective review was performed for patients who underwent successful PPV for RRD.OCT exams were taken preoperatively and 1mo after surgery, until SMF disappeared.According to the preoperative macular status on OCT, patients were divided into two groups: macula-off RRD (Group A) and maculaon RRD (Group B).ln Group A, there were two subgroups:macula partly detached (Group A1) and macula totally detached (Group A2).The main outcome measures were the presence of SMF on OCT 1mo after surgery,and the preoperative and postoperative best corrected visual acuities (BCVA), among the different groups and depending on the presence or absence of persistent SMF.
● RESULTS:A total of 139 eyes of 139 patients were included in the study.Persistent SMF at 1mo after surgery was 15.8% (22/139), all occurring in Group A (22/101); Group B had no SMF at 1mo after surgery (0/38,P=0.002).The incidence of persistent SMF at 1mo after surgery in Group A1 was 50% (14/28), and in Group A2 was 11.0% (8/73,P<0.001).Significant differences were shown between the presence and absence of persistent SMF on foveolaoff RRD, the preoperative BCVA, the 1mo postoperative BCVA, and the degree of the BCVA improvement from 1mo postoperatively to the final follow-up (P<0.05).However,there were no significant differences in the final BCVA(P>0.05).
● CONCLUSlON:Persistent SMF after PPV for retinal detachment is associated with preoperative macular status.Macula-uninvolving RRD shows no persistent SMF after PPV.Macular partly detached RRD has a higher incidence of SMF than macula totally detached RRD after PPV.The persistence of SMF may be responsible for the delayed visual recovery, whereas there were no signifcant differences in the fnal visual acuity.
● KEYWORDS:submacular fluid; rhegmatogenous retinal detachment; optical coherence tomography; vitrectomy;macula
Optical coherence tomography (OCT) is a useful noninvasive tool for detecting macular pathologic features, many of which cannot be seen on clinical examination[1].Subclinical submacular fuid (SMF) has often been identifed on OCT and was shown to persist for months (up to 18mo) after successful retinal detachment (RD) surgery, without being recognized by ophthalmoscopy or fluorescein angiography[2-8].Previous reports mainly studied patients undergoing scleral buckling(SB) procedures, with few about vitrectomy for RD[2,5,7].
The causes of the persistent SMF are still unclear.The incidence of the persistent SMF varies after pars plana vitrectomy(PPV).Wolfensberger and Gonvers[2]reported 24 patients who underwent PPV with no persistent SMF on OCT for 1mo after PPV.Bensonet al[3]reported that in 100 patients who underwent PPV, 15 were found to have persistent subretinal fluid (SRF) on OCT at 6wk after surgery, and there were no signifcant differences in the persistence of SRF between the macula-on RD group and macula-off RD group after PPV.However, in Bensonet al’s study[3], the preoperative macular status was defined by clinical examination alone, rather than by OCT scan.And, no studies showed the relationship between macular status preoperatively and persistent SMF postoperatively.
The influence of persistent SMF on visual outcomes is still controversial.Recent studies[8-10]have showed that persistent SMF may delay the visual recovery, did not injury the final visual outcomes.
This study was undertaken to compare by OCT imaging the incidence of persistent SMF after primary PPV for rhegmatogenous retinal detachment (RRD) in different preoperative macular conditions, and to investigate the relationship between SMF and visual outcome.
A non-randomized, retrospective review was performed for patients who underwent successful PPV surgery for RRD in the Affiliated Eye Hospital of Wenzhou Medical College from June, 2012 to June, 2016.All investigations followed the tenets of the Declaration of Helsinki.Informed consents were obtained from the patients and subjects after explanation of the nature and possible consequences of the study.
Inclusions for analysis were restricted to: 1) patients who completed a follow-up examination at least six months postoperatively;2) patients who completed OCT exam preoperative and 1mo postoperative.Exclusion criteria were: 1) patients with proliferative vitreoretinopathy (above C1); 2) patients with primary surgical failure; 3) patients with a history of ocular surgery, other than an uncomplicated cataract operation; 4) patients with a trauma history; 5) patients with a preexisting macular pathology, such as age-related macular degeneration, macular hole; 6) patients with a condition likely to infuence retinal fattening after RRD surgery, such as epiretinal membrane, and combined traction detachment attributable to diabetes.
Patients underwent best corrected visual acuity (BCVA, the Snellen VA chart) assessment, anterior segment examination,and retinal examination with indirect and slit-lamp biomicroscopy using a Volk super field NC lens and OCT scan preoperative and 1mo after surgery.The 6×6-mm2radial line scan protocol was performed using Spectralis OCT(Heidelberg Engineering, Heidelberg, Germany).Those patients who had an abnormality on OCT scan would undergo follow-up repeated check-up until the SMF disappeared.All the patients completed a follow-up examination at least six months postoperatively.
All surgeries were performed by an experienced retinal surgeon(Shen LJ).Perfuorocarbon was used or not after vitrectomy to fatten the detached retina.C3F8 or silicon was selected based on the surgeon’s decision.All patients were required to be face down for 2wk at least postoperatively.If a visually signifcant cataract developed during the follow-up, cataract surgery would be performed.And the visual acuity (VA) at that point was adopted from the VA at 1mo after cataract surgery.

Figure 1 Different macular status preoperatively A: Macula partly detached RRD (Group A1, foveola-on); B: Macula partly detached RRD (Group A1, foveola-off); C: Macula totally detached RRD(Group A2, foveola-off); D: Macula-on RRD (Group B).
The definition of macula was a round area at the posterior pole measuring appropriately 5.5 mm in diameter[11].SMF was defned as the fuid between the sensory retina and retinal pigment epithelium (RPE) in macula area.
Patients were classifed into two groups showing in the OCT fndings preoperatively.Those who showed macula-involving RRD by OCT were assigned to Group A (Figure 1A-1C), and those who showed macula-uninvolving RRD were assigned to Group B (Figure 1D).Relying on the different range of detachment in macula, we further subdivided Group A into subgroups A1 and A2.Group A1 (Figure 1A, 1B), macula was partly detached; Group A2 (Figure 1C), macula was totally detached.Those who showed SMF on OCT 1mo after surgery were assigned to group SMF (+), while the others were assigned to group SMF (-).We continued follow-up examination until SMF disappeared.Final VA was defned as BCVA at least 6mo after surgery.
For statistical comparison, VA was expressed as a logarithm of the minimum angle of resolution (logMAR) equivalents.The Mann-WhitneyUtest,ttest, Chi-square test, and Fisher’s exact test were used to assess the significance of observed associations.APvalue <0.05 was considered signifcant.All analyses were conducted using SPSS 20.
A total of 139 patients (139 eyes) were recruited in this study.The mean follow-up time was 10.74mo (range 6-56mo).Table 1 showed the patients’ demographic data.Group A consisted of 101 (72.7%) patients, and Group B consisted of 38 (27.3%)patients.Twenty-two (15.8%) patients had persistent SMF on OCT at 1mo after surgery.As shown in Table 1, no patient had persistent SMF on OCT at 1mo after surgery in Group B,whereas 22 (21.8%) patients in Group A had persistent SMF on OCT at 1mo after surgery (χ2=9.83,P=0.002).Maculauninvolved RRD patients had better VA (Z=-7.02,P<0.001)and fewer clock hours of detachment than macula-involvedRRD patients preoperatively (Z=-3.31,P=0.001).There was no difference in age, gender, duration of symptoms, number of high myopia eyes, the use of perfluorocarbon, different tamponades, or follow-up time between the two groups.
Table 1 Demographic and clinical characteristics of Group A and Group B

BCVA: Best corrected visual acuity.
Table 2 Demographic and clinical characteristics of Group A1 and Group A2

BCVA: Best corrected visual acuity; SMF: Submacular fuid.
Table 3 Comparison of preoperative and postoperative BCVA between SMF (+) group and SMF (-) group for foveola-on RRD
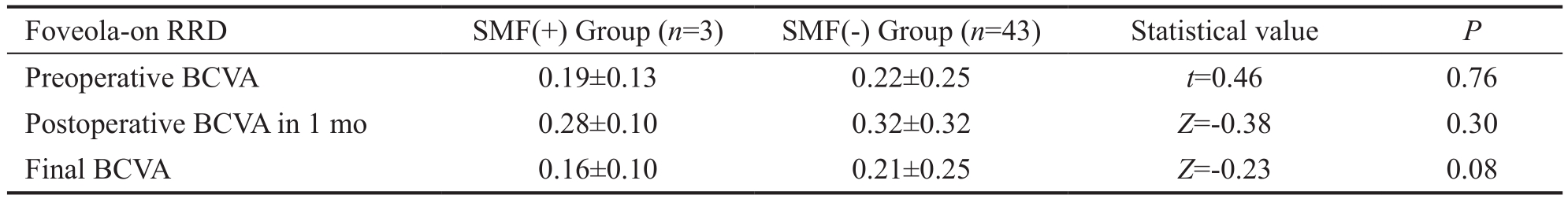
RRD: Rhegmatogenous retinal detachment; SMF: Submacular fuid; BCVA: Best corrected visual acuity.
Table 4 Comparison of preoperative and postoperative BCVA and degree of change in BCVA between SMF (+) group and SMF (-) group for foveola-off RRD

RRD: Rhegmatogenous retinal detachment; SMF: Submacular fuid; BCVA: Best corrected visual acuity.
In Group A (macula-off group), persistent SMF 1mo after surgery was more frequent in the macula partly detached group(Group A1, 14/28, 50%) than in the macula totally detached group (Group A2, 8/73, 11.0%,χ2=18.105,P<0.001).And, the macula partly detached group had better preoperative BCVA than did the macula totally detached group (Z=-5.32,P<0.001).But, there were no significant differences between the two groups in age or duration of detachment, nor was it associated with the use of C3F8 or silicon (Table 2).
There were two foveola statuses in the macular partly detached RRD group before surgery: foveola-on RRD and foveola-off RRD.Figure 1A, 1D were included in foveola-on RRD whereas Figure 1B, 1C were foveola-off RRD.The visual outcomes were compared between the SMF (+) and SMF (-) groups in foveola-on and foveola-off RRD, respectively (Tables 3, 4).There were no signifcant preoperative or postoperative BCVA difference between the SMF (+) and SMF (-) groups in the foveola-on RRD during the follow-up times.However, in the foveola-off RRD, the SMF (+) group had signifcantly higher preoperative BCVA (Z=-2.40,P=0.017), postoperative BCVA at 1mo(Z=-2.49,P=0.013), and improvement from 1mo BCVA to the final BCVA than did the SMF (-) group (Z=-2.71,P=0.007;Figure 2).The final VA outcomes, along with the change in BCVA at other time points, showed no significant difference between the two groups.

Figure 2 Comparison of preoperative and postoperative BCVA between SMF (+) group and SMF (-) group for foveola-off RRD.
OCT is widely used in detecting SMF after surgery.The OCT images are able to show shallow SRF, even when all retinal breaks are closed and the retina appears fully attached on ophthalmoscopy.
Quintyn and Brasseur[12]reported that the SRF of the RRD contained hyaluronic acid, various proteins (globulin, plasmin,apoprotein, fibronectin), lipids, and glucides, and assumed that the osmotic pressure (which was linked to the protein content) would be the main cause of SRF accumulation.Veckeneeret al[13]further hypothesized that the persistent SRF after surgery may be mostly related with the conditions of high cellularity and viscosity in the subretinal space.Then,in PPV, after water is largely excluded, the residual SRF is left much more concentrated in hyaluronic acid, protein, and other components.The osmotic pressure would increase and be reabsorbed through the outer blood-retinal barrier, which would explain the persistent SMF after the surgery.Chenet al[14]recently used a prospective study showing that completely exchanging SRF with balanced salt solution would diminish the SMF after the surgery, if there was no RPE damage.Kimet al[15]also showed evidence that delayed absorption of SMF after surgery was associated with high choroidal permeation.Nonetheless, Kimet al[16]studied the periphery SRF blebs and proposed that there was a horizontal power parallel with the interface of PRE-photoreceptor cells,and this power resulted in the changes of the blebs features.
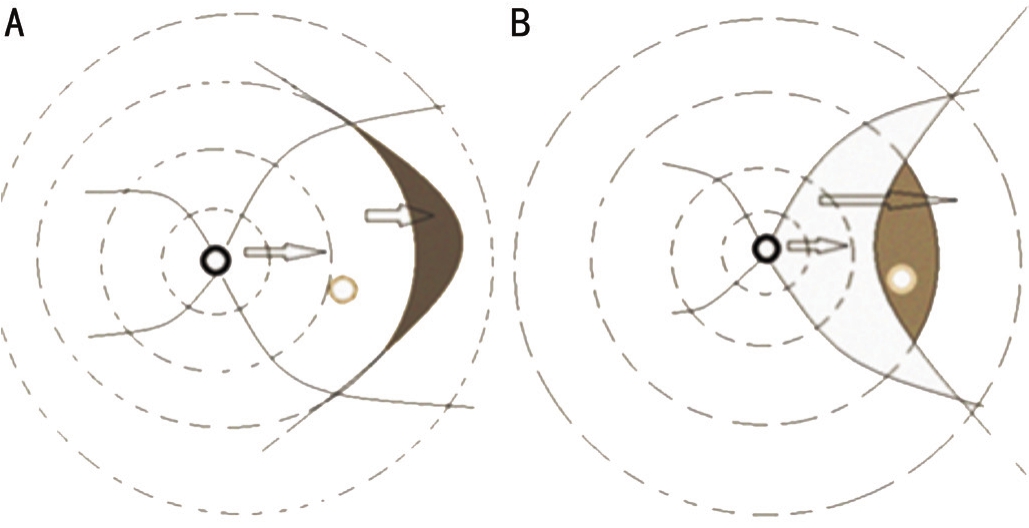
Figure 3 Edge effect Two statuses of the edge of the detached retina.A: Macula totally detached; B: Macula partly detached.
In our study, 22 of 139 eyes had SMF detected by OCT at 1mo after surgery.The incidence (15.8%) of SMF at 1mo after PPV was almost the same as that in Bensonet al’s study[17](15.0%), who described 100 RD patients who underwent PPV; SRF was seen in 15 of 100 patients at 6wk.However,Kimet al[18]described only 1 of 16 (6.3%) RD patients who underwent PPV showed persistent SMF 1mo after surgery,and Wolfensberger and Gonvers[2]described no one in 24 RD patients who underwent PPV showed persistent SMF 1mo after surgery.The small sample in these studies and short duration of the symtoms[5,18]may contribute to the lower incidence of persistent SMF.Both Bensonet al[17]and Theodossiadiset al[5]had reported that macular-uninvolving RRD patients had a higher prevalence of persistent SMF after the surgery,which conflicted with our result (0/28).Thus, we speculated three reasons for the difference, as follows: 1) low-resolution OCT missed the shallow SMF preoperatively; 2) the OCT was performed earlier than just before the surgery, which did not take the progress of RRD into account; and 3) the supine position during the surgery contributed to the SMF.
Our study was the first to discover the relationship between the preoperative macular status and the incidence of persistent SMF after PPV.According to the preoperative macular status,patients were divided into three groups.And, we surprisingly found that the incidence of persistent SMF after PPV for RD was 50% in the macula partly detached RRD patients, which was higher than that in macula-on RRD patients (0,P<0.001),or the macula totally detached RRD patients (11%,P<0.001).Taking the the former results into account, we considered that the residual SMF may be the most important source of persistent SMF after RRD surgery.And, the residual SMF was highly associated with the preoperative macular status.
We hypothesized there was an edge effect.Figure 3 shows two statuses of the edge of detached retina: the arc face to the discus opticus or the arc back to the discus opticus.In the frst status, SRF is enclosed by perfuorocarbon or air.The edge of the detached retina is unable to be excluded (the left picture).In the second status, the SRF on the edge is pushed forward and begins to accelerate from zero speed.The speed of the SRF on the edge may be slower than perfuorocarbon or tamponade.Then, the perfluorocarbon or tamponade will stop the SRF from moving forward under gravity.Furthermore, the position of the edge may be the reason that the macular partly detached RRD group had a higher rate of SMF after surgery: as none of our patients’ hole was located on the posterior pole, the edge effect would more frequently happen in macular partly RRD,especially with the temporal holes, than in the macula area in macular totally detached RRD or macula-on RRD.We infer that there will be SRF on the edge in patients with macular totally detached RRD or macula-on RRD.Figure 4 shows the SRF that was 3.82 mm away from the center of the macula 1mo after surgery in a macular-on RRD patient.Kanget al[19]showed OCT and fundus photograph findings of SRF away from the macula area as well.

Figure 4 A macular-on RRD patient postoperative OCT image in 1mo The SRF (double right arrow) was 3.82 mm away from the foveola.
For the VA, previous studies had produced contrary conclusions.Most of the studies concluded that the persistent SMF after surgery did not correlate with final VA[20].Some studies that concluded differently were limited by the small sample sizes or the short follow-up period.Whereas Bensonet al[3]reported that RD patients with SRF 6wk after PPV had worse VA.However, 50 in 157 were macula-on whereas 107 in 157 were macula-off RD patients.When visual outcomes were compared between the presence or the absence of persistent SRF groups, they calculated the VA of macula-on and maculaoff patients together.It is well known that VA in foveolaon RD patients is better than that in foveola-off RD patients preoperatively or postoperatively.And, almost all maculaon patients did not have SRF after PPV.It turned out that the more macular-on patients there were, the better the visual outcome of the absence of persistent SRF group.Thus, in our study, when comparing VA among SMF (+) and SMF (-)groups, we divided all patients into foveola-on and foveolaoff RRD groups.Futhermore, there were 46 foveola-on RRD patients, and only 3 had persistent SMF.Considering such a small number of patients in the SMF (+) group, we excluded the foveola-on RRD patients.
In the foveola-off RRD group (Table 4), just as we presumed,the largest portion of the SMF (+) group were macular partly detached patients (A1), whereas the SMF (-) group was derived from nearly all the macular detached patients (A2).So, it explained why the SMF (+) group had significantly higher preoperative VA and postoperative VA along a short time-period (P<0.05).In our study, there was no significant evidence that SMF influences the final visual outcomes.All the patients had gradually recovered VA (Figure 2).But, when comparing the speed or the extent of the improvement of VA between the two groups, obviously the SMF (+) group was slower and smaller during the follow-up period.There was a signifcant difference in the change of BCVA from 1 to 6mo.We concluded that, among the foveola-off RRD patients, the persistence of SMF after the surgery may be responsible for the delayed visual recovery.
In conclusion, persistent SMF after PPV for RD was associated with preoperative macular status.The grouup of patients with macula partly detached RRD had a higher incidence of SMF than did the patients with macula totally detached or those with macula-on RRD after PPV surgery.The edge effect may be an explanation for this phenomenon.The persistence of SMF may disturb the recovery of the VA in the short term, whereas it has no infuence on the fnal visual outcome.
Foundation:Supported by the Platform Key Project of Medical Scientifc Research Foundation of Zhejiang Province(No.2016ZDA016).
Conflicts of Interest:Mao JB, None; Lin JJ, None; Yu XT,None; Cheng D, None; Chen YQ, None; Tao JW, None; Wu HF, None; Jiang L, None; Zhang Y, None; Shen LJ, None.
REFERENCES
1 Puliafto CA, Hee MR, Lin CP, Reichel E, Schuman JS, Duker JS, Izatt JA, Swanson EA, Fujimoto JG.Imaging of macular diseases with optical coherence tomography.Ophthalmology1995;102(2):217-229.
2 Wolfensberger TJ, Gonvers M.Optical coherence tomography in the evaluation of incomplete visual acuity recovery after maculaoff retinal detachments.Graefes Arch Clin Exp Ophthalmol2002;240(2):85-89.
3 Benson SE, Schlottmann PG, Bunce C, Xing W, Charteris DG.Optical coherence tomography analysis of the macula after vitrectomy surgery for retinal detachment.Ophthalmology2006;113(7):1179-1183.
4 Meng ZJ, Gao YF, Wang YT.Clinical survey and analysis of persistent submacular fluid on optical coherence tomography after surgery for rhegmatogenous retinal detachment.Zhonghua Yan Ke Za Zhi2013;49(12):1075-1080.
5 Theodossiadis PG, Georgalas IG, Emfetzoglou J, Kyriaki TE, Pantelia E, Gogas PS, Moschos MN, Theodossiadis GP.Optical coherence tomography findings in the macula after treatment of rhegmatogenous retinal detachments with spared macula preoperatively.Retina2003;23(1):69-75.
6 Ge LN, Shen LJ, Zhao ZQ, Fang HZ, Zheng JW.Study of macular feature and visual acuity after successful rhegmatogenous retinal detachment surgery.Chin J Praet Ophthalmol2012;30(9):1045-1048.
7 Seo JH, Woo SJ, Park KH, Yu YS, Chung H.Influence of persistent submacular fuid on visual outcome after successful scleral buckle surgery for macula-off retinal detachment.Am J Ophthalmol2008;145(5):915-922.
8 Baba T, Hirose A, Moriyama M, Mochizuki M.Tomographic image and visual recovery of acute macula-off rhegmatogenous retinal detachment.Graefes Arch Clin Exp Ophthalmol2004;242(7):576-581.
9 Yu H, Gao MH, Li Y, Wang Y.Relationship between morphologic macular changes and visual outcome in eyes with persistent submacular fuid after surgery for macula-off rhegmatogenous retinal detachment and relevant factors of persistent submacular fuid.Chin J Ocul Fundus Dis2013;29(2):136-141.
10 Kim YK, Kim YW, Woo SJ, Ahn J, Hwang DJ, Park KH.Persistent submacular fluid and structural and functional recovery of retina.Ophthalmology2014;121(12):2501-2502.
11 Ge J, Zhao JL, Li XX.Ophthalmology.2th Edition.Beijing.PA:People’s Medical Publishing House;2011:62.
12 Quintyn JC, Brasseur G.Subretinal fuid in primary rhegmatogenous retinal detachment: physiopathology and composition.Surv Ophthalmol2004;49(1):96-108.
13 Veckeneer M, Derycke L, Lindstedt EW, van Meurs J, Cornelissen M, Bracke M, Van Aken E.Persistent subretinal fluid after surgery for rhegmatogenous retinal detachment: hypothesis and review.Graefes Arch Clin Exp Ophthalmol2012;250(6):795-802.
14 Chen X, Zhang Y, Yan Y, Hong L, Zhu L, Deng J, Din Q, Huang Z, Zhou H.Complete subretinal fluid drainage is not necessary during vitrectomy surgery for macular off rhegmatogenous retinal detachment with peripheral breaks: a prospective, nonrandomized comparative interventional study.Retina2017;37(3):487-493.
15 Kim JM, Lee EJ, Cho GE, Bae K, Lee JY, Han G, Kang SW.Delayed absorption of subretinal fluid after retinal reattachment surgery and associated choroidal features.Korean J Ophthalmol2017;31(5):402-411.
16 Kim YK, Ahn J, Woo SJ, Hwang DJ, Park KH.Multiple subretinal fuid blebs after successful retinal detachment surgery: incidence, risk factors,and presumed pathophysiology.Am J Ophthalmol2014;157(4): 834-841.
17 Benson SE, Schlottmann PG, Bunce C, Xing W, Charteris DG.Optical coherence tomography analysis of the macula after scleral buckle surgery for retinal detachment.Ophthalmology2007;114(1):108-112.
18 Kim YK, Woo SJ, Park KH, Yu YS, Chung H.Comparison of persistent submacular fuid in vitrectomy and scleral buckle surgery for macula-involving retinal detachment.Am J Ophthalmol2010;149(4):623-629.e1.
19 Kang SW, Kim JH, Shin WJ, Kim JI.Subretinal fluid bleb after successful scleral buckl in gand cryotherapy for retinal detachment.Am J Ophthalmol2008;146(2):205-210.
20 Gharbiya M, Malagola R, Mariotti C, Parisi F, De Vico U, Ganino C,Grandinetti F.Spectral-domain optical coherence tomography analysis of persistent subretinal fuid after scleral buckling surgery for macula-off retinal detachment.Eye(Lond)2015;29(9):1186-1193.
Citation:Mao JB, Lin JJ, Yu XT, Cheng D, Chen YQ, Tao JW, Wu HF,Jiang L, Zhang Y, Shen LJ.Comparison of persistent submacular fluid in different preoperative macular status after vitrectomy for rhegmatogenous retinal detachment.Int J Ophthalmol2018;11(11):1796-1801
DOl:10.18240/ijo.2018.11.10
Accepted:2018-08-14
Received:2018-06-10
Correspondence to:Li-Jun Shen.Department of Retina Center, the Affiliated Eye Hospital of Wenzhou Medical University, 618 Fengqi East Road, Hangzhou 310000,Zhejiang Province, China.slj@mail.eye.ac.cn