·Brief Report·
Clinical and laboratory features of PCR-confrmed periocular tuberculosis in China
Rui-Qi Ma1,2,3, Lu Gan1,2,3, Ying-Wen Bi1, Yi-Fei Yuan1, Hui Ren1, Jiang Qian1
1Department of Ophthalmology, Eye & ENT Hospital of Fudan University, Shanghai 200031, China
2NHC Key Laboratory of Myopia (Fudan University), Shanghai 200031, China
3Laboratory of Myopia, Chinese Academy of Medical Sciences,Shanghai 200031, China
Abstract
● Experts lack knowledge of periocular tuberculosis (TB)in China.Nested polymerase chain reaction (PCR) shows advantages in diagnosis of extrapulmonary TB.Our study aims to explore the clinical and laboratory features of PCR-confirmed periocular TB.We retrospectively reviewed medical records of presumptive periocular TB and performed nested PCR test to confrm diagnosis.Nine cases were recruited.Clinical symptoms were chronic and insidious.Eight cases achieved favorable visual acuity, while one underwent enucleation due to fungal-TB panophthalmitis.Sensitivity of caseous necrosis, acidfast bacilli (AFB) staining and interferon γ release assay(T-SPOT) test are 33.3%, 44.4% and 85.7% respectively.Low lymphocyte percentage (P=0.019) and high monocytelymphocyte ratio (P=0.042) positively correlate with AFB staining.Male gender (P=0.048) and Langhans giant cell(P=0.048) positively correlate with caseous necrosis.To conclude, traditional TB ancillary tests are not as sensitive as nested PCR technique.Several factors facilitate diagnosis including male gender, decreased lymphocytes,and typical Langhans giant cells.
● KEYWORDS:periocular tuberculosis; nested polymerase chain reaction; acid-fast bacilli staining; caseous necrosis;lymphocyte; Langhans giant cell
INTRODUCTION
Periocular tuberculosis (TB) refers tomycobacterium tuberculosis(MTB) infection around the eye, and on its surface[1].It comprises many subtypes, including TB of eyelid,conjunctiva, cornea, sclera, nasolacrimal system and other intraorbital tissues.Although the prevalence is low, periocular TB can cause devastating outcomes[2].Therefore, experts need to fully investigate the clinical and laboratory features of periocular TB.MTB culture sensitivity in extrapulmonary TB is very low, fuctuating from 11.9% to 34.2% in different studies[3-4].A substantial amount of periocular TB cases was diagnosed presumptively without pathogenic evidences, and these cases may mislead understanding of periocular TB clinical features[5].Recently, nested polymerase chain reaction(nPCR) shows advantages in extrapulmonary TB diagnosis[6].The technique amplifies one gene target with two pairs of primers in two rounds of amplification, resulting in more abundant products and lower mispairing rate[7].More and more studies adopt nPCR as gold standard to diagnose tuberculous infection.We reviewed medical records of presumptive TB cases in our hospital, performed nPCR test to obtain defnitive diagnosis, and carefully analyzed the clinical and laboratory features of polymerase chain reaction (PCR)-confirmed periocular TB.
METHODS
Briefy, we reviewed all medical records of periocular TB in adults(older than 18 years old) without human immunodeficiency virus (HIV) from 2007 to 2017.The study protocol was in accordance with Declaration of Helsinki (2008), and approved by the Institutional Review Board.Informed consent was obtained from all patients.Inclusive criteria were suggestive clinical symptoms/signs and positive response to antituberculous therapy (ATT).The criteria are consistent with WHO diagnostic criteria of extrapulmonary TB[3].Cases with follow-up less than two years were excluded.To confirm diagnosis, we performed nPCR test targeting IS6110 with formalin-fixed paraffin-embedded specimens as Ritiset al[8]reported.Clinical features of confirmed periocular TB cases were then summarized, including demographics, medical history, ophthalmic examination, systemic evaluation, and various imaging results.
To investigate laboratory features, we conducted acid-fast bacilli (AFB) staining and hematoxylin-eosin (HE) staining.AFB staining was performed with Ziehl-Neelsen method in at least ten slides from each paraffn block.Other laboratory tests were reviewed, including blood routine test, tuberculin skin test (TST) and interferon γ release assay (T-SPOT).Correlation analysis was conducted between different variables and three important TB parameters, including caseous necrosis, positive AFB staining and positive T-SPOT result.ATT therapy and follow-up results were summarized, and data analysis was carried out to examine the infuential factors for ATT treatment results.Pvalue less than 0.05 is statistically signifcant.
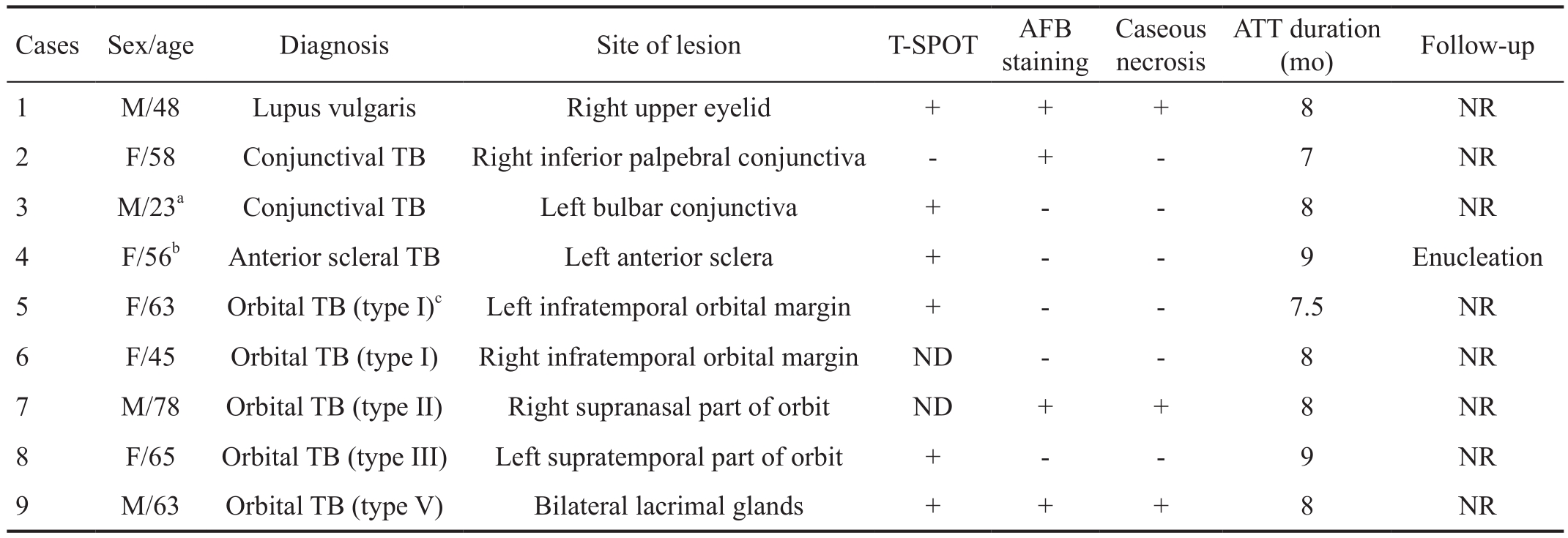
Table 1 Clinical and laboratory features of PCR-confirmed periocular TB
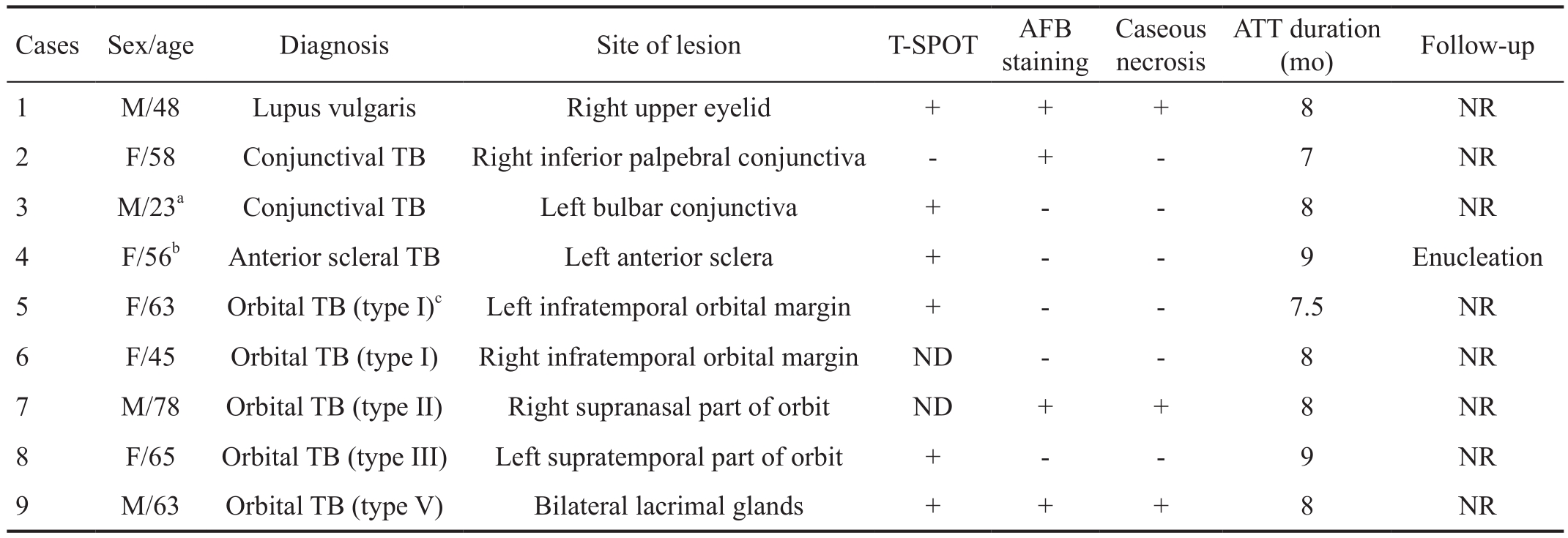
TB: Tuberculosis; ND: Not done; T-SPOT: Interferon γ release assay; AFB: Acid-fast bacilli; ATT: Anti-tuberculous therapy; NR: No recurrence.aThe patient was coinfected with ocular herpes simplex;bThe patient was enucleated due to fungal-tuberculous panophthalmitis (refer to Case Report section);cType I: Classical periostitis; Type II: Orbital soft tissue tuberculoma/cold abscess; Type III: Orbital TB with evidence of bony involvement; Type IV: Orbital TB arising from the paranasal sinuses; Type V: Tuberculous dacryoadenitis.
Cases Sex/age Diagnosis Site of lesion T-SPOT AFB staining Caseous necrosis ATT duration(mo) Follow-up 1 M/48 Lupus vulgaris Right upper eyelid + + + 8 NR 2 F/58 Conjunctival TB Right inferior palpebral conjunctiva - + - 7 NR 3 M/23aConjunctival TB Left bulbar conjunctiva + - - 8 NR 4 F/56bAnterior scleral TB Left anterior sclera + - - 9 Enucleation 5 F/63 Orbital TB (type I)cLeft infratemporal orbital margin + - - 7.5 NR 6 F/45 Orbital TB (type I) Right infratemporal orbital margin ND - - 8 NR 7 M/78 Orbital TB (type II) Right supranasal part of orbit ND + + 8 NR 8 F/65 Orbital TB (type III) Left supratemporal part of orbit + - - 9 NR 9 M/63 Orbital TB (type V) Bilateral lacrimal glands + + + 8 NR
RESULTS AND DISCUSSION
Clinical FeaturesTwelve cases complied with the inclusive criteria of presumptive periocular TB.Nine cases (10 eyes)were confirmed by nPCR test, including one lupus vulgaris of eyelid, two tuberculous conjunctivitis, one tuberculous anterior scleritis, and five orbital TB (Table 1).Age range was 23 to 78 years old (mean 59.75, median 63).Male to female ratio was 4 to 5.All lesions were unilateral except for a bilateral tuberculous dacryoadenitis (case 9).One patient complained of vision loss and ocular pain due to tuberculous anterior scleritis (case 4).Lupus vulgaris (case 1) presented with chronic swelling and painless ulceration of eyelid(Figure 1A).Conjunctival TB manifested as either nodular(Figure 1B) or diffused (Figure 1C) hyperplasia with purulent discharge.Orbital TB was insidious, and presented with cold, nontender soft tissue swelling.On CT scan, the lesions generally presented as medium density mass with moderate enhancement, and sometimes presented with bony erosion and abscess formation (Figure 1D, 1E).On MRI scan, the lesion signals were commonly iso-/hypointense on T1 images (Figure 1F), iso-/hyperintense on T2 images, and heterogeneous on enhanced images (Figure 1G).Other symptoms included progressive proptosis, eye position deviation and ocular movement defects.At the time of presentation, two patients suffered systemic symptoms such as fatigue, weight loss and poor appetite.No patients had chest symptoms including breathless, hemoptysis, or chest pain.All patients were immunocompetent, and five out of nine had diabetes.Chest X-ray was conducted in eight cases, with no active pulmonary lesions discovered.One case underwent chest CT scan, and was detected with fbrotic strips at right lung apex.Regarding to TB related medical histories, all patients had bacille Calmette-Guerin vaccination after birth.Two patients recalled TB contact history during childhood.One patient had a history of tuberculous lymphadenitis.
Laboratory FeaturesT-SPOT test was positive in six out of seven patients (85.7% sensitivity).Four patients were examined with TST test, and all showed positive reaction with induration larger than 10 mm.On HE staining, all cases showed granulomatous inflammation, and three of them presented caseous necrosis (33.3% sensitivity).On AFB staining, four out of nine cases were confrmed with positive results (44.4% sensitivity).Based on blood tests, lymphocyte percentage (in all blood cells) decreased in four out of nine cases (44.4%), erythrocyte sedimentation rate accelerated in two out of three cases (66.7%), C-reactive protein elevated in one out of three cases (33.3%), and mild anemia was discovered in two out of nine cases (22.2%).Other blood tests including angiotensin converting enzyme, auto-antibodies,hepatitis and syphilis infection showed nothing special.CT or MRI scan was performed in orbital TB patients.

Figure 1 Imaging study of periocular TB A: Lupus vulgaris (case 1).Redness and swelling of right upper eyelid, along with purulent discharge and painless ulceration; B: Tuberculous conjunctivitis (case 2).Recurrent redness and purulence on ocular surface, and a nodule formed at lower palpebral conjunctiva; C: Tuberculous conjunctivitis (case 3).Purulent discharge and diffuse papillary hyperplasia of bulbar conjunctiva; D-E: Orbital TB with evidence of bony involvement (case 8).CT scan showed a partially-enhanced lesion with well-defned cyst formed inside, along with orbital bone compression and absorption; F-G: Tuberculous dacryoadenitis (case 9).MRI scan revealed diffuse enlargement of bilateral lacrimal gland with hypo-intense signal on T1 images, iso-intense signal on T2 images, and enhanced heterogeneously on fat-suppression sequence.
Treatment and Follow-upAll patients were prescribed with two-stage ATT: four drugs (isoniazid, rifampin, pyrazinamide,ethambutol) for the frst two months, and two drugs (isoniazid,rifampin) for the next five to seven months.The average treatment duration was 8mo.Five patients suffered delayed diagnosis as a result of underdiagnosis or misdiagnosis.These patients had longer ATT therapy (one tailedttest,P=0.031)than timely diagnosis patients, indicating that delayed diagnosis may be a risk factor for longer ATT duration.After withdrawal of ATT therapy, seven patients recovered completely without vision loss.One patient had slight vision loss due to optic nerve compression (visual acuity from 0.8 to 0.6, International Standard Chart).One patient suffered complete vision loss due to enucleation (refer to case report section).
Data AnalysisCorrelation analysis was conducted between important tuberculous parameters (T-SPOT, AFB staining,caseous necrosis and ATT duration) and potential influence variables (Table 2).Based on data analysis, low lymphocyte percentage (Spearman’s Rank,P=0.019) and high monocytelymphocyte (M/L) ratio (Spearman’s Rank,P=0.042)positively correlate with positive AFB staining.Male gender(Fisher exact probability,P=0.048) and Langhans giant cell(Fisher exact probability,P=0.048) positively correlate with existence of caseous necrosis.AFB staining and caseous necrosis positively correlate with each other (Fisher exact probability,P=0.048).No variables showed correlation with T-SPOT test and ATT duration.The results suggested that male patients with decreased lymphocytes, as well as Langhans giant cells on HE staining, were more prone to be diagnosed with periocular TB.
Case ReportA 56-year-old female farmer came to our hospital.Her chief complaint was blurred vision, recurrent redness, and ocular pain for ten months.Slit-lamp examination showed scleral nodules and anterior chamber inflammation.After ruled out autoimmune diseases, we performed TST and T-SPOT tests.Both tests showed positive results, and highly suggested tuberculous infection.To confirm diagnosis, we conducted scleral biopsy.HE staining showed granulomatous infammation and caseous necrosis (Figure 2A); fungal staining and AFB staining were negative; nPCR test was positive(Figure 2B).We made the diagnosis of anterior tuberculous scleritis, and subscribed ATT treatment for nine months.

Figure 2 Case report of fungal-TB coinfection A 56-year-old female (case 4) complained of blurred vision, recurrent redness and ocular pain for ten months.A: Histological staining of scleral biopsy tissue showed granulomatous infammation without typical caseous necrosis (stain, HE;magnifcation, ×500); B: Existence of MTBwas confrmed by nPCR (lane 1, positive control; lane 2, negative control; lane 3, blank control; lane M, molecular size marker; lane 4 & 5, nPCR products); C: ATT was prescribed, but panophthalmitis developed six months later.Histopathology of enucleated eyeball showed atypical granulomatous infammation surrounded by neovascularization and bleeding (stain, HE; magnifcation,×500); D-E: Special staining confrmed both fungus infection (D: stain, periodic acid-Schiff; magnifcation, ×500) and TB infection (E: stain,Ziehl-Neelsen; magnifcation, ×630).
Table 2 Correlation between tuberculous parameters and continuous variables

AFB: Acid-fast bacilli; T-SPOT: Interferon γ release assay; ATT:Anti-tuberculous therapy.aSignifcant difference.bRefers to symptom duration from onset to fnal diagnosis;cLymphocyte percentage in all blood cells;dDivided into ocular surface lesions (including lacrimal gland) and orbital lesions;eDivided into nodular lesions and diffuse lesions;fDivided into biopsy group and surgical removal group.
Variables T-SPOT AFB staining Caseous necrosis ATT duration Continuous variables Age 0.500 0.213 0.200 0.451 Symptom durationb0.324 0.246 0.406 0.299 Lymphocyte percentagec0.182 0.019a0.063 0.386 Monocyte-lymphocyte ratio 0.330 0.042a0.063 0.428 Neutrophil-lymphocyte ratio 0.182 0.076 0.167 0.384 Dichotomous variables Sex 0.571 0.167 0.048a0.500 Site of lesiond0.714 0.317 0.595 0.452 Shape of lesione0.143 0.167 0.583 0.109 Interventionf0.143 0.167 0.583 0.109 Diabetes 0.571 0.643 0.405 0.500 Langhans giant cell 0.571 0.167 0.048a0.500 T-SPOT - 0.429 0.714 0.060 AFB staining 0.429 - 0.048a0.156 Caseous necrosis 0.714 0.048a- 0.500
Six months later, she came back to our hospital, with complete vision loss, intractable pain and large amounts of purulent discharge.She recalled that her eyes were scratched by plants a month ago.When asked about ATT treatment, she arbitrarily stopped taking drugs three months ago because of symptom relief.On physical examination, the right globe was fixed,with hypopyon and tenderness.B-scan showed complete retinal detachment, thinning sclera and surrounding soft tissue edema.The patient was diagnosed with panophthalmitis, and underwent enucleation.Histopathological analysis showed untypical granulomatous inflammation (Figure 2C), with positive fungal staining (Figure 2D), positive AFB staining(Figure 2E) and positive nPCR result.The final diagnosis was fungal-tuberculous coinfection.Insufficient treatment may be the cause of double infection.We restarted both antituberculous and anti-fungal therapy, and the patient recovered completely after nine months.
Nested PCR technique is a major breakthrough in diagnosis of extrapulmonary TB.The novel technique shows better performance than traditional PCR and other ancillary TB tests,especially in paucibacillary extrapulmonary specimens[9].Many in-house nPCR tests are available based on amplifed targets.The most widely used target is IS6110, a multi-copy sequence randomly distributing throughout MTB genome[10].Diagnostic efficacy of nPCR is still unsure in periocular TB, and we suggest further study to explore the performance of nPCR technique in diagnosis of periocular TB.Based on our study,male gender, decreased lymphocyte count and high M/L ratio are three important parameters to assist TB diagnosis.Similar gender bias was previously reported in other TB studies[11-12],and the gender pattern is probably reversed in Caucasian studies[13-14].M/L ratio was adopted as TB biomarker in many previous TB studies[15], and was used to monitor ATT response during treatment of pediatric osteoarticular TB[16].Coinfection is an important issue in TB patients.According to WHO report in 2017, TB-HIV coinfection has drawn worldwide attention[17].However, few studies focus on TB coinfection in immunocompetent patients.Therefore, coinfection is an unneglectable issue in both immunosuppressive and immunocompetent patients.To conclude, our study helps health workers to grasp more profound comprehension of clinical and laboratory features of periocular TB, and offers insights into the essential role of nested PCR technique for periocular TB diagnosis.
ACKNOWLEDGEMENTS
We gratefully acknowledge Dr.Rui Zhang and Dr.Yan-Qing Zhang (Fudan Eye & ENT Hospital) for providing the orbital tissues.
Foundation:Supported by National Natural Science Foundation of China (No.81800867).
Conflicts of Interest:Ma RQ, None; Gan L, None; Bi YW,None; Yuan YF, None; Ren H, None; Qian J, None.
REFERENCES
1 Shakarchi FI.Ocular tuberculosis: current perspectives.Clin Ophthalmol2015;9:2223-2227.
2 Babu K, Mukhopadhyay M, Bhat SS, Chinmayee J.Orbital and adnexal tuberculosis: a case series from a South Indian population.J Ophthalmic Inflamm Infect2014;4:12.
3 Norbis L, Alagna R, Tortoli E, Codecasa LR, Migliori GB, Cirillo DM.Challenges and perspectives in the diagnosis of extrapulmonary tuberculosis.Expert Rev Anti Infect Ther2014;12(5):633-647.
4 Jia H, Pan L, Qin S, Liu F, Du F, Lan T, Zhang X, Wei R, Du B, Liu Z, Huang H, Zhang Z.Evaluation of interferon-γ release assay in the diagnosis of osteoarticular tuberculosis.Diagn Microbiol Infect Dis2013;76(3):309-313.
5 Urzua CA, Lantigua Y, Abuauad S, Liberman P, Berger O, Sabat P,Velasquez V, Castiglione E, Calonge M.Clinical features and prognostic factors in presumed ocular tuberculosis.Curr Eye Res2017;42(7):1029-1034.
6 Wilson SM, McNerney R, Nye PM, Godfrey-Faussett PD, Stoker NG,Voller A.Progress toward a simplifed polymerase chain reaction and its application to diagnosis of tuberculosis.J Clin Microbiol1993;31(4):776-782.
7 Furini AA, Pedro Hda S, Rodrigues JF, Montenegro LM, Machado RL, Franco C, Schindler HC, Batista IM, Rossit AR.Detection of mycobacterium tuberculosis complex by nested polymerase chain reaction in pulmonary and extrapulmonary specimens.J Bras Pneumol2013;39(6):711-718.
8 Ritis K, Tzoanopoulos D, Speletas M, Papadopoulos E, Arvanitidis K,Kartali S, Sideras P.Amplifcation of IS6110 sequence for detection of mycobacterium tuberculosis complex in HIV-negative patients with fever of unknown origin (FUO) and evidence of extrapulmonary disease.J Intern Med2010;248(5):415-424.
9 Meghdadi H, Khosravi AD, Ghadiri AA, Sina AH, Alami A.Detection of mycobacterium tuberculosis in extrapulmonary biopsy samples using PCR targeting IS6110, rpoB, and nested-rpoB PCR Cloning.Front Microbiol2015;6:675.
10 Sinha P, Gupta A, Prakash P, Anupurba S, Tripathi R, Srivastava GN.Differentiation of mycobacterium tuberculosis complex from nontubercular mycobacteria by nested multiplex PCR targeting IS6110,MTP40 and 32kD alpha antigen encoding gene fragments.BMC Infect Dis2016;16:123.
11 Boum Y 2nd, Atwine D, Orikiriza P, Assimwe J, Page AL, Mwanga-Amumpaire J, Bonnet M.Male gender is independently associated with pulmonary tuberculosis among sputum and non-sputum producers people with presumptive tuberculosis in Southwestern Uganda.BMC Infect Dis2014;14:638.
12 Mason PH, Snow K, Asugeni R, Massey PD, Viney K.Tuberculosis and gender in the Asia-Pacifc region.Aust N Z J Public Health2017;41(3):227-229.
13 Salam T, Uddin JM, Collin JR, Verity DH, Beaconsfeld M, Rose GE.Periocular tuberculous disease: experience from a UK eye hospital.Br J Ophthalmol2015;99(5):582-585.
14 Shoughy SS, Jaroudi MO, Tabbara KF.Clinical manifestations and outcome of tuberculous sclerokeratitis.Br J Ophthalmol2016;100(9):1301-1303.
15 Naranbhai V, Hill AV, Abdool Karim SS, Naidoo K, Abdool Karim Q, Warimwe GM, McShane H, Fletcher H.Ratio of monocytes to lymphocytes in peripheral blood identifies adults at risk of incident tuberculosis among HIV-infected adults initiating antiretroviral therapy.J Infect Dis2014;209(4):500-509.
16 Agarwal A, Bhat MS, Kumar A, Shaharyar A, Mishra M, Yadav R.Lymphocyte/monocyte ratio in osteoarticular tuberculosis in children: a haematological biomarker revisited.Trop Doct2016;46(2):73-77.
17 World Health Organization.Global tuberculosis report 2017.Available at http://www.who.int/tb/publications/global_report/en/.Accessed on October 17, 2018.
Citation:Ma RQ, Gan L, Bi YW, Yuan YF, Ren H, Qian J.Clinical and laboratory features of PCR-confrmed periocular tuberculosis in China.Int J Ophthalmol2018;11(11):1865-1869
DOl:10.18240/ijo.2018.11.20
Accepted:2018-09-04
Correspondence to:Jiang Qian.Department of Ophthalmology, Eye & ENT Hospital of Fudan University, 83 Fen Yang Road, Shanghai 200031, China.qianjiang@fudan.edu.cn Received: 2018-01-03
Co-first authors:: Rui-Qi Ma and Lu Gan