Table 1 Description of patients in groups 1 and 2
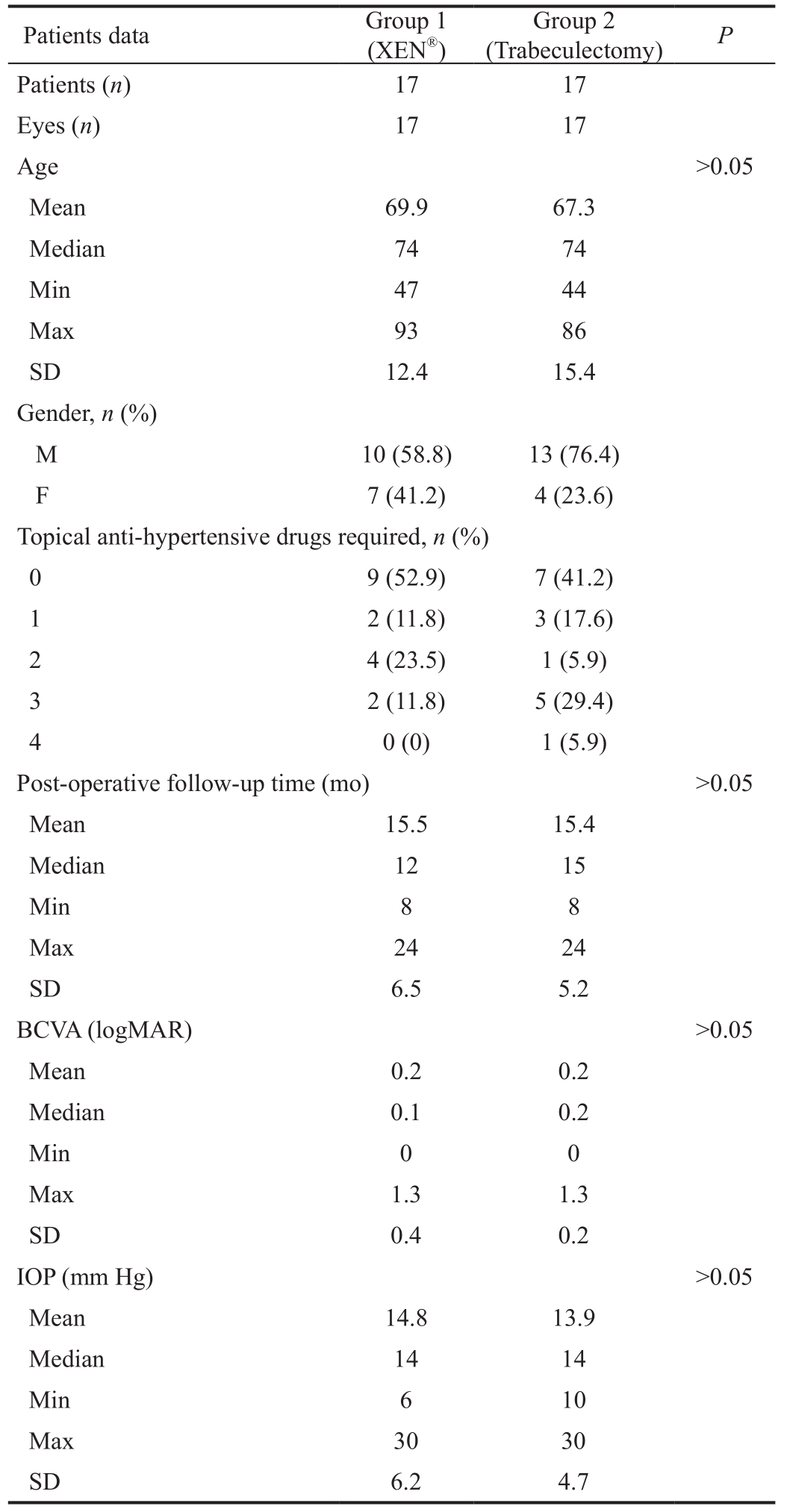
Min: Minimum; Max: Maximum; SD: Standard deviation; BCVA:Best-corrected visual acuity; IOP: Intraocular pressure.
?
The ophthalmologist must always bear in mind the in fluence that both diagnosis and treatment of glaucoma have on the patient’s quality of life[1]. There are several studies on the impact of glaucoma on quality of life, however the effect of treatment on the routine of these patients has been poorly studied[2-4]. Most clinical trials have evaluated the success of treatments with objective clinical measures[5-8],and only one randomized multicenter clinical trial has been conducted so far to assess the impact of glaucoma treatment in quality of life[9].
The Glaucoma Symptom Scale (GSS) questionnaire is a modified version of the “Ocular Hypertension Treatment Study 10-item Symptom Checklist”. It is specific for patients with glaucoma and it quantifies common symptoms present in patients with this condition. It is a simple, short,comprehensive test consisting of ten questions that include two dimensions: non-visual ocular symptoms (burning/smarting/stinging, tearing, soreness/tiredness, itching, foreign body sensation, dryness) and visual symptoms (blurry/dim vision,hard to see in daylight, hard to see in darkness, halos around lights). Allows to apply the test to each individual eye (result of 0-50) or bilaterally (result of 0-100). It has been validated for use in clinical practice and in research to quantify symptoms in patients with glaucoma, namely to assess the effect of the disease and its treatments on the populations[10].
Trabeculectomy is considered the gold standard approach concerning the surgical treatment of glaucoma, since it allows an effective reduction of intraocular pressure (IOP) in most cases. However, the postoperative period of this surgery may be associated with complications, sometimes compromising the patient’s vision[11-12].
The implant of the XEN45®Gel Stent Glaucoma Treatment System (Allergan, Irvine, CA) is considered a minimally invasive surgical procedure and it was introduced in 2014 in Europe for treatment of open angle glaucoma refractory to medical therapy[13]. It is inserted by a microincision into the cornea and creates a drainage fistula for aqueous humor to the subconjunctival space[8,14]. It is a less traumatic procedure than trabeculectomy and associated with a lower incidence of serious complications, which could mean a faster recovery and a lower impact on quality of life[15-16].
The primary aim of this study was to compare the mediumterm quality of life of patients with advanced open angle glaucoma who underwent XEN®implantation or trabeculectomy and to secondarily investigate the relationship with potentially involved variables.
The authors conducted a comparative cross-sectional study in agreement with the Declaration of Helsinki for research involving humans. At our tertiary institution of ophthalmology,a sample of patients with open angle glaucoma who underwent XEN®implantation and trabeculectomy, between October 2015 and February 2017, were recruited. All patients to whom the XEN®implant was placed in the specified period were chosen for group 1. For group 2, a random selection of patients submitted to trabeculectomy in the same period was performed, in order to match the number of patients in group 1. All patients (groups 1 and 2) had advanced open angle glaucoma, uncontrolled with anti-hypertensive therapy, and the conjunctiva was satisfactorily preserved in both groups.
Patients submitted to combined surgery, prior ipsilateral eye surgery, diagnosed with ocular surface disease, cognitive or auditory impairment were excluded from the study. The following data were analyzed as: age, gender, postoperative follow-up time, topical anti-hypertensive therapy in the postoperative period, last record of best-corrected visual acuity(BCVA) and IOP. Patients were contactedviatelephone and,after their verbal consent to participate in the study, answered the GSS questionnaire in relation to the operated eye. The patient was asked, for each of the 10 symptoms addressed in the questionnaire, whether this was a problem or not in the last 4wk and, if so, what was the degree of discomfort. The answers were converted into numerical values, according to the questionnaire [absent -4, present 0 to -3 (very uncomfortable 0, some discomfort -1, little inconvenience -2, did not cause discomfort -3)]. At the sum of the individual values, 10 values were always added and the final GSS score between 0 and 50 was obtained.
Statistical analysis was performed using SPSS software version 23.0 (SPSS, Chicago, USA). Comparison of the GSS results between groups was performed using the Mann-Whitney test and Spearman’s correlation was used for the correlation analysis of the variables. ThePvalue less than 0.05 was considered statistically signi ficant.
The study included 34 eyes from 34 patients, 17 eyes in each group. All patients selected to participate in the study accepted to respond to the survey. Regarding mean age, group 1 presented 69.9±12.4y and group 2 presented 67.3±15.4y(P>0.05). The characterization of patients in both groups is shown in Table 1.
The mean GSS score for group 1 was 42.6±6.8 (median, 47;p25, 36.5; p75, 48.5) and for group 2 it was 41.6±7.0 (median,43; p25, 36.5; p75, 47;P=0.34). There were no statistically signi ficant differences between groups when symptoms were compared alone or in terms of visual and non-visual symptoms(Table 2).
Table 1 Description of patients in groups 1 and 2
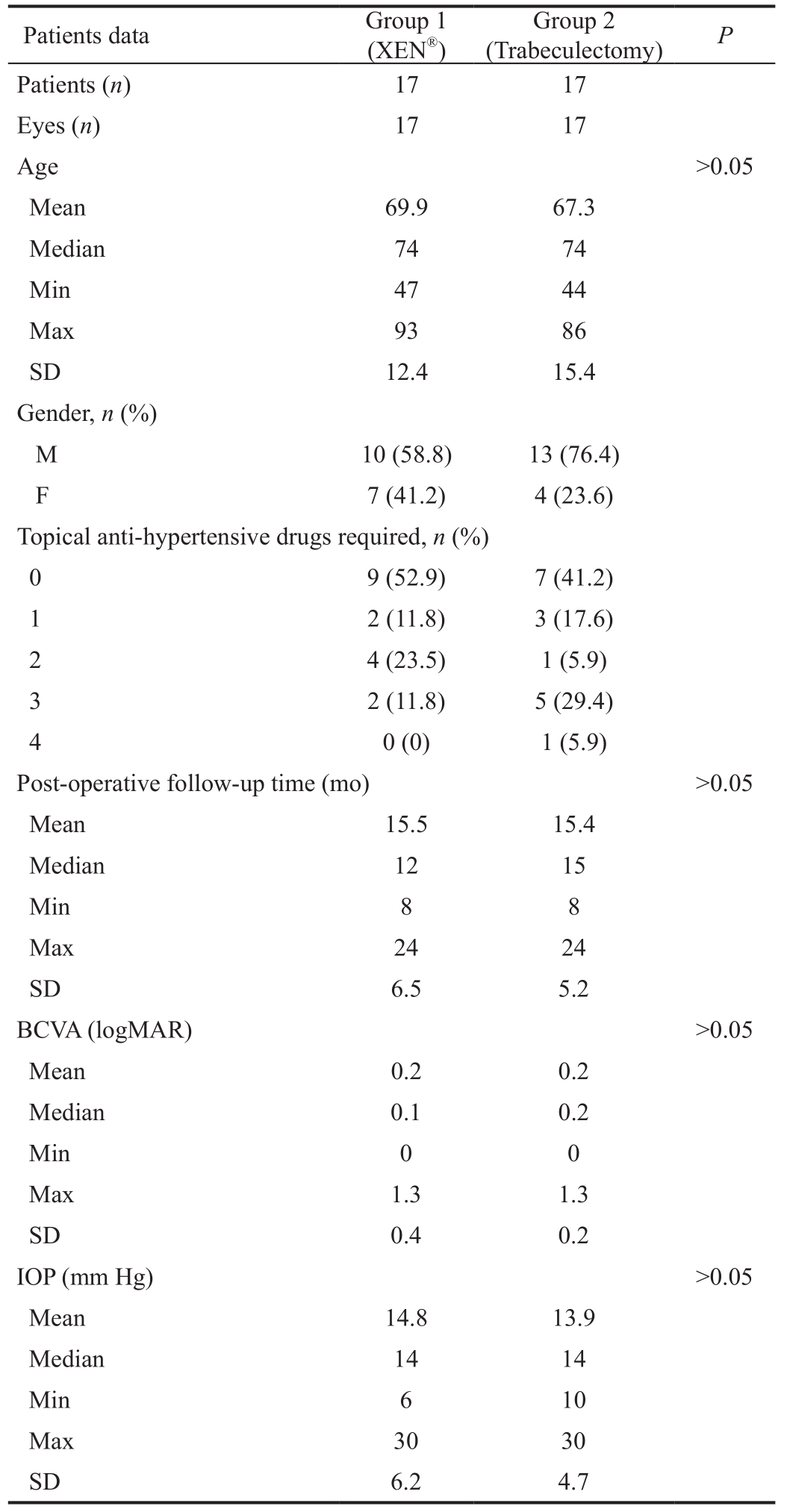
Min: Minimum; Max: Maximum; SD: Standard deviation; BCVA:Best-corrected visual acuity; IOP: Intraocular pressure.
?
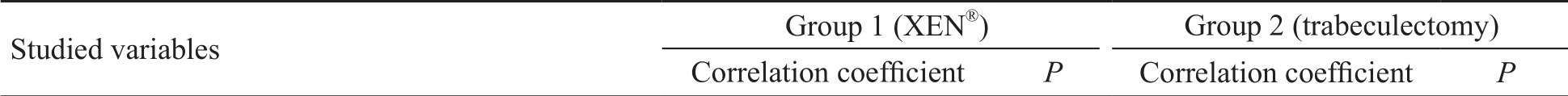
The analysis of the relationship between the results of the GSS questionnaire and the various variables revealed a strongly negative correlation between the administration of topical antihypertensive drug and the GSS result in both study groups(r=-0.88,P<0.01 andr=-0.59,P=0.01, respectively). There was a moderate negative correlation between GSS and IOP in group 1 (r=-0.50,P=0.03). No significant correlations were established with age, postoperative follow-up time and BCVA(Table 3).
Table 2 GSS results (general results, by symptom and by non-visual and visual symptoms) and comparison between the two groups

GSS: Glaucoma Symptom Scale; Min: Minimum; Max: Maximum; SD: Standard deviation.
 GSS score 0.34 Mean 42.6 41.6 Min 30 22 Max 50 49 SD 6.8 7.0 Median 47 43 P25 36.5 36.5 P75 48.5 47.0 Symptom (mean)Burning/smarting/stinging 3.1 2.7 0.20 Tearing 3.0 2.7 0.26 Dryness 3.6 4.0 0.06 Itching 3.5 3.6 0.36 Soreness/tiredness 3.1 3.1 0.45 Foreign body sensation 3.5 3.4 0.44 Blurry/dim vision 3.2 2.8 0.15 Hard to see in daylight 3.1 3.0 0.40 Hard to see in darkness 3.6 3.5 0.30 Halos around lights 3.5 2.9 0.07 Non-visual symptoms (mean) 19.8 19.5 0.43 Visual symptoms (mean) 13.5 12.1 0.16
GSS score 0.34 Mean 42.6 41.6 Min 30 22 Max 50 49 SD 6.8 7.0 Median 47 43 P25 36.5 36.5 P75 48.5 47.0 Symptom (mean)Burning/smarting/stinging 3.1 2.7 0.20 Tearing 3.0 2.7 0.26 Dryness 3.6 4.0 0.06 Itching 3.5 3.6 0.36 Soreness/tiredness 3.1 3.1 0.45 Foreign body sensation 3.5 3.4 0.44 Blurry/dim vision 3.2 2.8 0.15 Hard to see in daylight 3.1 3.0 0.40 Hard to see in darkness 3.6 3.5 0.30 Halos around lights 3.5 2.9 0.07 Non-visual symptoms (mean) 19.8 19.5 0.43 Visual symptoms (mean) 13.5 12.1 0.16
Table 3 Study of the relationship between the variables and the GSS result
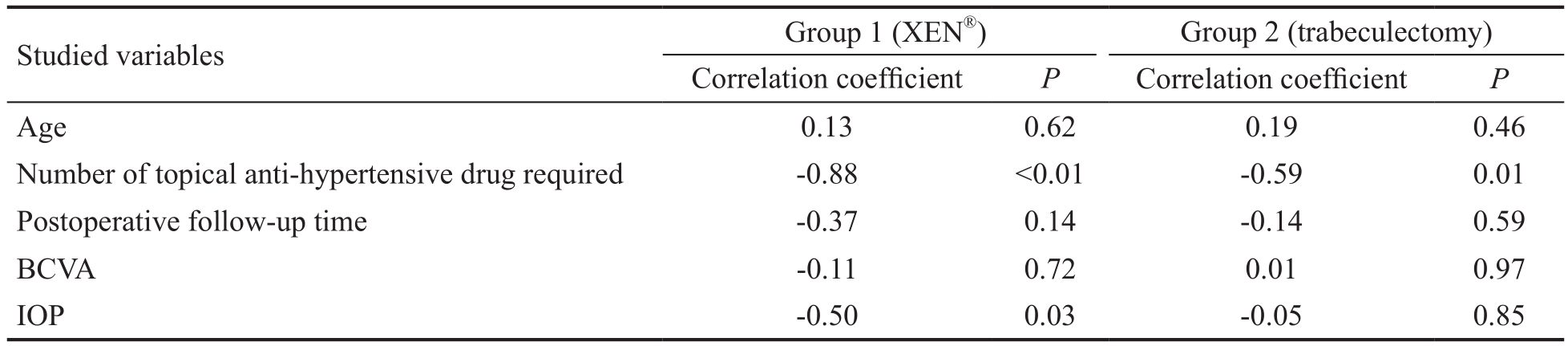
BCVA: Best-corrected visual acuity; IOP: Intraocular pressure.
 Age 0.13 0.62 0.19 0.46 Number of topical anti-hypertensive drug required -0.88 <0.01 -0.59 0.01 Postoperative follow-up time -0.37 0.14 -0.14 0.59 BCVA -0.11 0.72 0.01 0.97 IOP -0.50 0.03 -0.05 0.85
Age 0.13 0.62 0.19 0.46 Number of topical anti-hypertensive drug required -0.88 <0.01 -0.59 0.01 Postoperative follow-up time -0.37 0.14 -0.14 0.59 BCVA -0.11 0.72 0.01 0.97 IOP -0.50 0.03 -0.05 0.85
The impact of glaucoma diagnosis and therapy on the patient’s quality of life still lacks practical objective measures. To the best of our knowledge, this is the first study to evaluate the quality of life in patients submitted to XEN®device implantation. The GSS questionnaire was applied in order to determine whether there were recognized differences in the effect of two different surgical treatments in quality of life of patients with glaucoma.
Although other questionnaires such as the NEI VFQ-25 were more frequently cited[1,17-20], the GSS questionnaire was chosen because it is simpler and shorter to apply, with good patient adherence, and because it includes non-visual symptoms in the comparison of the results of the two types of intervention performed.Likewise, there are no published studies comparing the quality of life of this new procedure with trabeculectomy[11].The analysis demonstrated the non-inferiority of quality of life of one group in relation to the other for the presence and degree of discomfort of non-visual and visual ocular symptoms. The surgical technique underlying XEN®device implantation and trabeculectomy might suggest less impact on ocular symptomatology in the first group, but this was not observed in this study. The advantages of a minimally invasive surgery, such as the XEN®implant, regarding ocular surface symptomatology may be concentrated mainly in the immediate postoperative period and this was not included in this analysis.Similar results were obtained by Pahlitzschet al[20], when comparing the quality of life 6-months post trabeculectomy,iStent®and Trabectome®procedure. In this study, the authors chose to standardize follow-up time between the two groups,and there was no significant difference between the two groups. Further studies may compare results in the immediate postoperative period or different stages in each group according to the clinical presentation, namely with the features of the conjunctiva after trabeculectomy. The number of topical antihypertensive drugs strongly in fluenced the quality of life in both groups, possibly due to the symptomatology of the ocular surface that can develop collaterally[21].
There was also a moderate negative relationship between IOP and the outcome of the score in group 1, which may be related to the need for instillation of anti-hypertensive drops and to manipulation of the filtering bleb. The quality of life analysis performed by Guedeset al[22], who compared groups at different stages of glaucoma and with different therapeutic strategies, found that early glaucoma was associated with poorer quality of life, probably due to the psychological impact of the diagnosis of the disease. In the moderate and advanced phases, the quality of life did not differ signi ficantly between the groups with medical and surgical therapy.
There are some limitations in this study, such as the fact that it is a small sample, but it is important to note that our center was the first at national level to insert the XEN®device and the reported results resemble to those patients. Moreover, the results may be influenced according to the status of patients such as vision or visual field in the fellow eye. This is mainly a pioneering study, comparing the results of a classic surgical technique (trabeculectomy) with the results of a recently marketed device (XEN®), most properly the first cases that matched the criteria for the study. It will be important to undertake further studies with a larger number of patients and applying the survey prior to surgery and regularly thereafter.
The use of this type of questionnaire is important in clinical practice because it allows the monitoring of chronic ocular symptoms objectively. The applicability of GSS in research is validated and may be an important tool in the comparative study of different treatments, medical or surgical.
Conflicts of Interest: Basílio AL,None;Moura-Coelho N,None;Passos I,None;Cardoso MS,None;Domingues I,None;Reina M,None;Flores R,None;Gomes T,None.
1 Quaranta L, Riva I, Gerardi C, Oddone F, Floriano I, Konstas AGP. Quality of life in glaucoma: a review of the literature.Adv Ther2016;33(6):959-981.
2 Black N. Patient reported outcome measures could help transform healthcare.BMJ2013;346:f167-f167.
3 Kotecha A, Feuer WJ, Barton K, Gedde SJ. Quality of life in the tube versus trabeculectomy study.Am J Ophthalmol2017;176:228-235.
4 Hirneiss C, Kortüm K. Quality of life in patients with glaucoma.Klin Monbl Augenheilkd2016;233(2):148-153.
5 Burr J, Azuara-Blanco A, Avenell A, Tuulonen A. Medical versus surgical interventions for open angle glaucoma.Cochrane Database Syst Rev2012;(9):CD004399.
6 Lavia C, Dallorto L, Maule M, Ceccarelli M, Fea AM. Minimallyinvasive glaucoma surgeries (MIGS) for open angle glaucoma: a systematic review and meta-analysis.PLoS One2017;12(8):e0183142.
7 Rulli E, Quaranta L, Riva I, Poli D, Hollander L, Galli F, Katsanos A, Oddone F, Torri V, Weinreb RN. Visual field loss and vision-related quality of life in the Italian primary open angle glaucoma study.Sci Rep2018;8:619.
8 Kerr NM, Wang J, Barton K. Minimally invasive glaucoma surgery as primary stand-alone surgery for glaucoma.Clin Exp Ophthalmol2017;45(4):393-400.
9 Janz NK, Wren PA, Lichter PR, Musch DC, Gillespie BW, Guire KE.Quality of life in newly diagnosed glaucoma patients the collaborative initial glaucoma treatment study.Ophthalmology2001;108(5):887-897.
10 Lee BL, Gutierrez P, Gordon M, Wilson MR, Cioffi GA, Ritch R,Sherwood M, Mangione CM. The Glaucoma Symptom Scale. A brief index of glaucoma-speci fic symptoms.Arch Ophthalmol1998;116(7):861-866.
11 Fernández S, Pardiñas N, Laliena JL, Pablo L, Díaz S, Pérez S,Honrubia FM. Long-term tensional results after trabeculectomy. A comparative study among types of glaucoma and previous medical treatment.Arch Soc Esp Oftalmol2009;84(7):345-352.
12 Ansari E. An update on implants for minimally invasive glaucoma surgery (MIGS).Ophthalmol Ther2017;6(2):233-241.
13 Grover DS, Flynn WJ, Bashford KP, Lewis RA, Duh YJ, Nangia RS,Niksch B. Performance and safety of a new ab interno gelatin stent in refractory glaucoma at 12 months.Am J Ophthalmol2017;183:25-36.
14 Lewis RA. Ab interno approach to the subconjunctival space using a collagen glaucoma stent.J Cataract Refract Surg2014;40(8):1301-1306.
15 SooHoo JR, Seibold LK, Radcliffe NM, Kahook MY. Minimally invasive glaucoma surgery: current implants and future innovations.Can J Ophthalmol2014;49(6):528-533.
16 Brandão LM, Grieshaber MC. Update on minimally invasive glaucoma surgery (MIGS) and new implants.J Ophthalmol2013;2013:1-12.
17 Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S.Development of the 25-item National Eye Institute Visual Function Questionnaire.Arch Ophthalmol2001;119(7):1050.
18 Simão LM, Lana-Peixoto MA, Araújo CR, Moreira MA, Teixeira AL.The brazilian version of the 25-item national eye institute visual function questionnaire: translation, reliability and validity.Arq Bras Oftalmol2008;71(4):540-546.
19 Hirooka K, Nitta E, Ukegawa K, Tsujikawa A. Vision-related quality of life following glaucoma filtration surgery.BMC Ophthalmology2017;17(1):66.
20 Pahlitzsch M, Klamann MK, Pahlitzsch ML, Gonnermann J, Torun N, Bertelmann E. Is there a change in the quality of life comparing the micro-invasive glaucoma surgery (MIGS) and the filtration technique trabeculectomy in glaucoma patients?Graefes Arch Clin Exp Ophthalmol2017;255(2):351-357.
21 Costa VP, Marcon IM, Galvão Filho RP, Malta RF. The prevalence of ocular surface complaints in Brazilian patients with glaucoma or ocular hypertension.Arq Bras Oftalmol2013;76(4):221-225.
22 Guedes RA, Guedes VM, Freitas SM, Chaoubah A. Quality of life of medically versus surgically treated glaucoma patients.J Glaucoma2013;22(5):369-373.