Relation between preoperative hyperopia and surgical outcome in infantile esotropia
Haeng Jin Lee1, Jeong-Ah Kim1, Seong-Joon Kim1,2, Young Suk Yu1,2
1Department of Ophthalmology, Seoul National University College of Medicine, Seoul 110-744, South Korea
2Seoul Arti ficial Eye Center, Seoul National University Hospital Clinical Research Institute, Seoul 110-744, South Korea
Abstract● AlM: To evaluate the relation between preoperative hyperopia and surgical outcomes of infantile esotropia in patients younger than 24 months of age.● METHODS: Medical records of patients who underwent bilateral medial rectus muscle recession for infantile esotropia between November 1, 2002 and December 1,2011 were retrospectively reviewed. Patients were divided into two groups according to the degree of preoperative hyperopia. Group l had less than +3.0 diopter (D) of hyperopia and group ll had between +3.0 and +5.0 D of hyperopia. Postoperative alignments were evaluated 1wk, 3, 6mo, and 1y after surgery. Following the 1-year postoperative visit, patients were monitored yearly.Relationships between preoperative factors including hyperopia and postoperative outcomes were evaluated.● RESULTS: Forty-six patients were included, with 33 patients in group l and 13 patients in group ll. The preoperative mean refractive error was +0.88 D in group l and +3.45 D in group ll. Surgical outcomes were not signi ficantly different between groups at any postoperative time point examined. Cumulative probability of surgical success, prevalence of inferior oblique overaction,dissociated vertical deviation, and re-operation rate were not signi ficantly different between groups.● CONCLUSlON: Preoperative moderate hyperopia (less than +5.0 D) did not affect the surgical outcome of infantile esotropia. Therefore, the surgical correction of esotropia should be considered when the angle of esodeviation is unchanged following hyperopia correction, even in children with moderate hyperopia.
INTRODUCTION
Infantile esotropia develops before 6 months of age and is defined as a non-accommodative concomitant esotropia without neurological deficits[1-2]. Patients with infantile esotropia have an angle of esodeviation of 30 prism diopters(PD) or more and a refractive error is similar to that of normal infants[1,3-4]. Most of infantile esotropia patients with large and constant esodeviation require surgical intervention to restore binocular vision and improve stereoacuity[5-13]. However,pediatric ophthalmologists should consider the effect of refractive error on esotropia because esodeviations can be accommodative.
Prior studies have shown that esodeviation could spontaneously decrease in infantile esotropia patients with hyperopia[14-15].However, few studies have examined the effect of hyperopia on the surgical outcome of infantile esotropia, with even fewer studies on moderate hyperopia. Therefore, we evaluated the relation between preoperative hyperopia and surgical outcomes following bilateral medial rectus muscle recession in infantile esotropia patients younger than 24 months of age.
SUBJECTS AND METHODS
SubjectsThis nonrandomized, retrospective case series was ethically approved by the Institutional Review Board of Seoul National University Hospital. All study conduct adhered to the tenets of the Declaration of Helsinki.
Patients who underwent standard bilateral medial rectus muscle recession for infantile esotropia between November 1,2002 and December 1, 2011, and followed for more than 6mo were included. All surgeries were performed by one surgeon(Kim SJ). Written informed consent for all surgical procedures was obtained from the patients’ parents or guardians. Patients with an underlying neurological defect or paralytic condition(e.g.cerebral palsy, hydrocephalus, prior strabismus surgery, or other comorbid ocular disease) were excluded. Patients were examined at least two times following 4wk of spectacle use.Patients with a >10 PD change in the angle of esotropia after hyperopic correction were assumed to have an accommodative component and were excluded from analyses. Patients with amblyopia, defined as presenting strong fixation preference after occlusion therapy provided before surgery, were also excluded.
Factors including age, sex, preoperative refractive errors,presence of anisometropia, preoperative and postoperative angle of deviation, and prevalence of dissociated vertical deviation(DVD) or inferior oblique overaction (IOOA) were retrospectively reviewed. Postoperative follow-up examinations were performed 1wk, 3, 6mo, and 1y after surgery. All patients were reexamined yearly beginning 2y after surgery.
Ophthalmologic Examination and Procedure of SurgeryAll patients underwent a comprehensive ophthalmologic examination before surgery, including a cycloplegic refraction with 1% cyclopentolate hydrochloride. Prescription glasses to correct hyperopia were made and refractive error was fully corrected in patients with +3.0 or more diopters (D) of hyperopia. Preoperative angle of esodeviation was measured on at least three occasions in all patients by one experienced examiner using the alternate prism cover test at near (0.33 m) and distance (6 m) fixation in the primary gaze, with appropriate spectacle correction if required. A modi fied Krimsky method was used to examine uncooperative patients. If the angle of esodeviation was more than 50 PD, the angle of deviation was measured using two loose plastic prisms (Luneau, France) held in one hand. Prisms were held over each eye separately (not stacked), with the apex facing the nose.
In patients with IOOA, surgical correction was determined according to the severity of IOOA (grades ranged from 0 to+4.0). An IOOA was considered to be clinically signi ficant if it was more severe than a grade +1. Patients with an IOOA grade of +1 underwent inferior oblique (IO) myotomy. Patients with an IOOA grade between +1.5 and +2 underwent IO myectomy.Patients with an IOOA grade greater than or equal to +2 underwent IO anterior transposition.
All surgeries were performed after esodeviation was stable and remained greater than 30 PD (as con firmed by more than two consecutive examinations). Surgeries were performed under general anesthesia, and surgical dosages were applied using Parks’ surgical protocol for graded bilateral medial rectus muscle recession[16].
Evaluation of Surgical OutcomesPatients were divided into two groups according to the degree of preoperative hyperopia(mean spherical equivalent of both eyes). Group I had less than +3.0 D of esotropia and group II had between +3.0 and +5.0 D of esotropia. Surgical outcomes were categorized into four groups using a modified version of von Noorden’s criteria[4,17], which are based on postoperative angle of deviation: orthotropia/mini-microtropia, microtropia (5-10 PD),small-angle deviation (11-20 PD), and large-angle deviation(>20 PD). In addition, each subgroup was further divided into the following three subgroups based on the postoperative angle of deviation at distance: overcorrection (exophoria/tropia >10 PD),success (esophoria/tropia or exophoria/tropia ≤10 PD), and undercorrection/recurrence (esophoria/tropia >10 PD).
Surgical outcome was determined using the deviation at the last follow-up visit. However, in cases of reoperation, the final angle of deviation was de fined as the angle measured during the last visit before reoperation. The time between surgery and recurrence was calculated. Reoperations were performed for recurrent esotropia or consecutive exotropia when the maximal angle of deviation was ≥15 PD and patients had poor fusional control, in which an increase in the manifest phase of esotropia was frequently noticed by parents and/or clinicians.
Statistical AnalysisThe Mann-WhitneyUtest, Fisher’s exact test, and Kruskal-Wallis test were used for comparing factors.Kaplan-Meier survival analysis and a log-rank test were used for comparing the recurrence rates. Statistical signi ficance was de fined asP<0.05. Statistical analyses were conducted using SPSS software for Windows version 18.0 (SPSS Inc., Chicago,Illinois, USA).
RESULTS
Patient DemographicsForty-six patients were ultimately included in this study. Mean age at the time of the initial surgery was 12.3±4.0mo (range 6-22mo). The preoperative angle of esodeviation was 59.5±17.5 PD (range 30-85 PD) and the preoperative refractive error was +1.61±1.47 D. Patients were followed after surgery for 38.3±31.3mo.
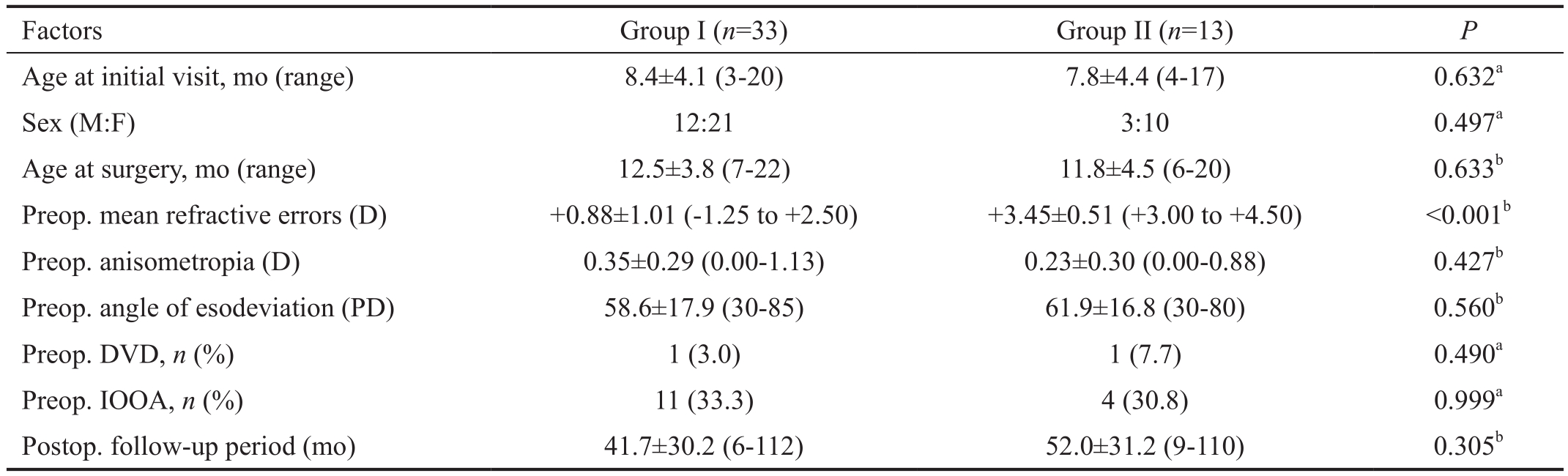
Patient Clinical Characteristics in Each Preoperative Refractive Error GroupThirty-three patients were in group I and 13 patients were in group II. Mean preoperative refractive error was +0.88±1.01 D in group I and +3.45±0.51 D in group II (P<0.001). Significant anisometropia was not observed in either group (group I: 0.35±0.29 D, group II:0.23±0.30 D;P=0.427). Mean subject age at the time of surgery was 12.5±3.8mo in group I and 11.8±4.5mo in group II and mean preoperative angle of esodeviation was 58.6±17.9 PD in group I and 61.9±16.8 PD in group II (P=0.633 and 0.560,respectively). Patients were followed for 41.7±30.2mo and 52.0±31.2mo after the initial surgery in groups I and II,respectively (P=0.305; Table 1).
The prevalence of IOOA and DVD was not significantly different between groups before or after surgery. After the surgery, DVD was observed in 10 patients (30.3%) in group I and 4 patients (30.8%) in group II (P=0.999) and IOOA was observed in 16 patients (48.5%) in group I and 5 patients(38.5%) in group II (P=0.744).
Surgical Outcomes in Patients Grouped by Preoperative Mean Refractive ErrorTable 2 summarizes surgical outcomes,as determined using a modified version of von Noorden’s criteria. Both groups were evaluated at 1wk and 3, 6, 12, 24,and 36mo after surgery.
Table 1 Demographic and clinical characteristics of patients with infantile esotropia who underwent bilateral medial rectus muscle recession before 24mo of age
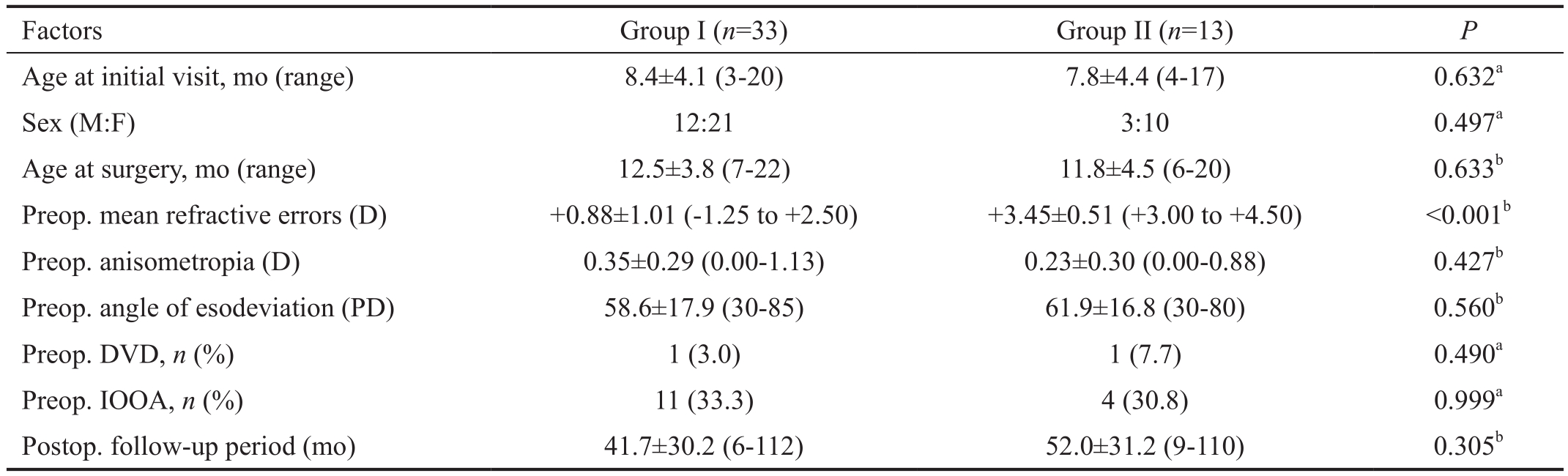
Group I: Patients with preoperative mean refractive errors <+3.0 D; Group II: Patients with preoperative mean refractive errors ≥+3.0 D and <+5.0 D;PD: Prism diopters; DVD: Dissociated vertical deviation; IOOA: Inferior oblique overaction.aFisher’s exact test,bMann-WhitneyUtest.
 Age at initial visit, mo (range) 8.4±4.1 (3-20) 7.8±4.4 (4-17) 0.632aSex (M:F) 12:21 3:10 0.497aAge at surgery, mo (range) 12.5±3.8 (7-22) 11.8±4.5 (6-20) 0.633bPreop. mean refractive errors (D) +0.88±1.01 (-1.25 to +2.50) +3.45±0.51 (+3.00 to +4.50) <0.001bPreop. anisometropia (D) 0.35±0.29 (0.00-1.13) 0.23±0.30 (0.00-0.88) 0.427bPreop. angle of esodeviation (PD) 58.6±17.9 (30-85) 61.9±16.8 (30-80) 0.560bPreop. DVD,n(%) 1 (3.0) 1 (7.7) 0.490aPreop. IOOA,n(%) 11 (33.3) 4 (30.8) 0.999aPostop. follow-up period (mo) 41.7±30.2 (6-112) 52.0±31.2 (9-110) 0.305b
Age at initial visit, mo (range) 8.4±4.1 (3-20) 7.8±4.4 (4-17) 0.632aSex (M:F) 12:21 3:10 0.497aAge at surgery, mo (range) 12.5±3.8 (7-22) 11.8±4.5 (6-20) 0.633bPreop. mean refractive errors (D) +0.88±1.01 (-1.25 to +2.50) +3.45±0.51 (+3.00 to +4.50) <0.001bPreop. anisometropia (D) 0.35±0.29 (0.00-1.13) 0.23±0.30 (0.00-0.88) 0.427bPreop. angle of esodeviation (PD) 58.6±17.9 (30-85) 61.9±16.8 (30-80) 0.560bPreop. DVD,n(%) 1 (3.0) 1 (7.7) 0.490aPreop. IOOA,n(%) 11 (33.3) 4 (30.8) 0.999aPostop. follow-up period (mo) 41.7±30.2 (6-112) 52.0±31.2 (9-110) 0.305b
Table 2 Surgical outcomes in patients with infantile esotropia who underwent bilateral medial rectus muscle recession before 24mo of age using a modi fied version of von Noorden’s criterian(%)
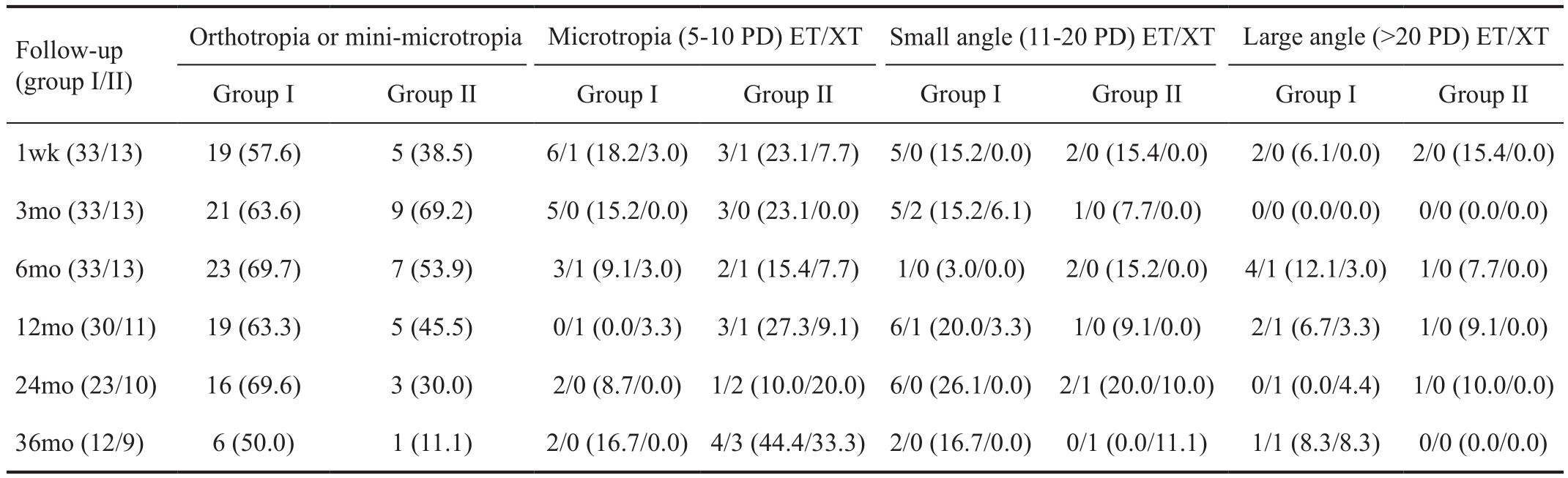
Group I: Patients with preoperative refractive errors <+3.0 D; Group II: Patients with preoperative refractive errors ≥+3.0 D and <+5.0 D. PD: Prism diopter; ET: Esotropia; XT: Exotropia.
Orthotropia or mini-microtropia Microtropia (5-10 PD) ET/XT Small angle (11-20 PD) ET/XT Large angle (>20 PD) ET/XT Group I Group II Group I Group II Group I Group II Group I Group II 1wk (33/13) 19 (57.6) 5 (38.5) 6/1 (18.2/3.0) 3/1 (23.1/7.7) 5/0 (15.2/0.0) 2/0 (15.4/0.0) 2/0 (6.1/0.0) 2/0 (15.4/0.0)3mo (33/13) 21 (63.6) 9 (69.2) 5/0 (15.2/0.0) 3/0 (23.1/0.0) 5/2 (15.2/6.1) 1/0 (7.7/0.0) 0/0 (0.0/0.0) 0/0 (0.0/0.0)6mo (33/13) 23 (69.7) 7 (53.9) 3/1 (9.1/3.0) 2/1 (15.4/7.7) 1/0 (3.0/0.0) 2/0 (15.2/0.0) 4/1 (12.1/3.0) 1/0 (7.7/0.0)12mo (30/11) 19 (63.3) 5 (45.5) 0/1 (0.0/3.3) 3/1 (27.3/9.1) 6/1 (20.0/3.3) 1/0 (9.1/0.0) 2/1 (6.7/3.3) 1/0 (9.1/0.0)24mo (23/10) 16 (69.6) 3 (30.0) 2/0 (8.7/0.0) 1/2 (10.0/20.0) 6/0 (26.1/0.0) 2/1 (20.0/10.0) 0/1 (0.0/4.4) 1/0 (10.0/0.0)36mo (12/9) 6 (50.0) 1 (11.1) 2/0 (16.7/0.0)4/3 (44.4/33.3)2/0 (16.7/0.0) 0/1 (0.0/11.1) 1/1 (8.3/8.3) 0/0 (0.0/0.0)Follow-up(group I/II)
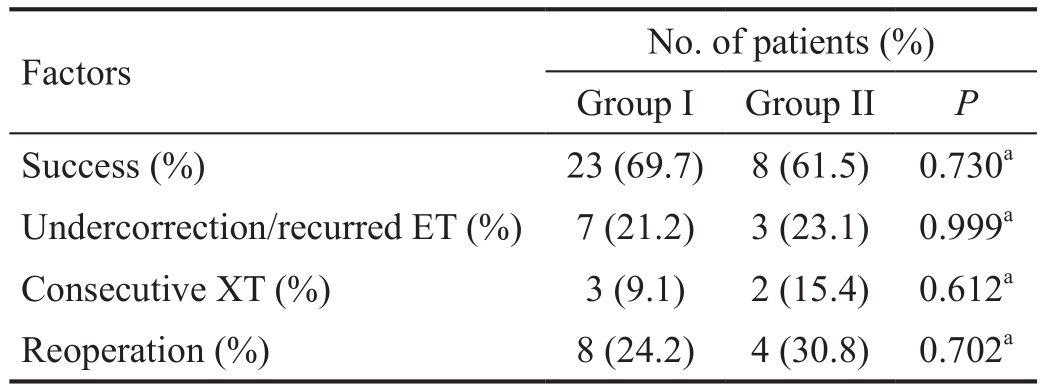
Group I had a 69.7% success rate and group II had a 61.5%success rate (P=0.730). Group I had 7 patients (21.2%) with undercorrection or recurrence and group II had 3 patients(23.1%) with undercorrection or recurrence (P=0.999). Group I had 3 patients (9.1%) with overcorrection and group II had 2 patients (15.4%) with overcorrection (P=0.612; Table 3).
Survival Analysis and Preoperative Mean Refractive Error According to The Surgical OutcomesThe Kaplan-Meier survival analysis revealed that recurrence of of >10 PD of esophoria/tropia or consecutive exophoria/tropia (based on cumulative probability of success) was not significantly different between groups at 6, 12, 24, 36, 48, 60, 72, and 84mo after surgery (allP>0.05; Figure 1).
The preoperative mean refractive error was not significantly different between groups divided according to the surgical outcome: +1.59±1.51 (range -1.13 to +4.50) D in the success group, +1.31±1.54 (range -1.25 to +3.56) D in the undercorrection/recurrent esotropia group, and +2.34±1.02(range +0.94 to +3.50) D in the overcorrection group (Kruskal-Wallis test,P=0.431).
Table 3 Surgical outcomes of patients with infantile esotropia who underwent bilateral medial rectus muscle recession before 24mo of age according to the preoperative mean refractive errors
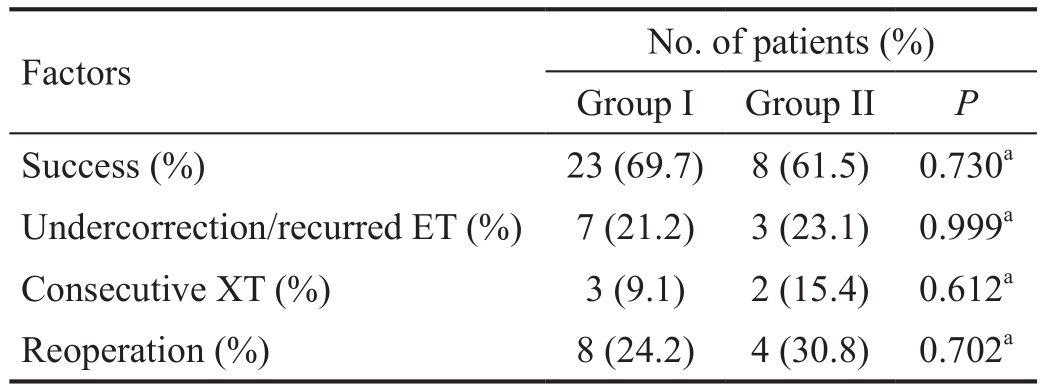
Group I: Patients with preoperative refractive errors <+3.0 D; Group II: Patients with preoperative refractive errors ≥+3.0 D and <+5.0 D.ET: Esotropia; XT: Exotropia.aFisher’s exact test.
 Success (%) 23 (69.7) 8 (61.5) 0.730aUndercorrection/recurred ET (%) 7 (21.2) 3 (23.1) 0.999aConsecutive XT (%) 3 (9.1) 2 (15.4) 0.612aReoperation (%) 8 (24.2) 4 (30.8) 0.702a
Success (%) 23 (69.7) 8 (61.5) 0.730aUndercorrection/recurred ET (%) 7 (21.2) 3 (23.1) 0.999aConsecutive XT (%) 3 (9.1) 2 (15.4) 0.612aReoperation (%) 8 (24.2) 4 (30.8) 0.702a
DISCUSSION
Visual accommodation in infants fully develops to the adult level by 4 months of age[18]. Therefore, accommodative factors may confound infantile esotropia, making it important to evaluate the degree of hyperopia in these patients. Hyperopia should be fully corrected prior to measuring the amount of surgical correction[19-20].Several ophthalmologists have studied the association between refractive errors and the natural course or surgical outcome of infantile esotropia. Costenbader[3]found that the distribution was similar between patients with and without infantile esotropia and that refractive error and degree of deviation were not correlated. In that study, 5.6%, 46.4%, 41.8%, and 6.4% of patients with infantile esotropia had myopia, mild hyperopia,moderate hyperopia, and severe hyperopia (more than +5.25 D).Burian[14]found that pediatric patients with a refractive error of +4.00 D or greater tended to have a decrease in the angle of esodeviation over time. Although this information is important for clinically managing infantile esotropia, it cannot be used to determine whether surgical management should be suggested in cases of infantile esotropia with hypertropia, because of the wide range in the degree of esodeviation (from 6 PD to >50 PD) and lack of results regarding the change in esodeviation after correction of hyperopic refractive error, which distinguishes accommodative esotropia from true infantile esotropia. In contrast, the Congenital Esotropia Observational Study reported that only 46 patients (27%) showed spontaneous resolution with hyperopic correction. Patients with a constant deviation ≥40 PD presenting after 10 weeks of age had a low likelihood of spontaneous resolution, suggesting the need for early surgical correction in these patients. In addition, there was no correlation between refractive errors and spontaneous resolution of esodeviation[21]. Stageret al[22]also did not find a correlation between refractive error and postoperative alignment in patients who underwent surgery for infantile esotropia before 1 year of age.
The current study examined surgical outcomes in 46 patients who underwent bilateral medial rectus muscle recession for infantile esotropia before 24 months of age, according to the degree of preoperative hyperopia.
We excluded patients with early-onset accommodative esotropia by evaluating hyperopia prior to surgery. Only patients that did not have a change in the angle of esodeviation after wearing glasses were included in analyses. We found that patients with concomitant moderate hyperopia from+3.0 D to +5.0 D did not have signi ficantly different clinical characteristics (e.g.age at the time of surgery, preoperative angle of esodeviation, concomitant IOOA or DVD, amount of bilateral medial rectus muscle recession, and postoperative deviation angle) or long-term success rates than patients with no or mild hyperopia. In addition, when patients were grouped according to the surgical outcome (orthotropia, consecutive exotropia, and undercorrection or recurrent esotropia groups),the degrees of preoperative refractive error were not found to be correlated with surgical outcomes for infantile esotropia among the groups. This finding is in agreement with that of Stageret al[22]and supports the notion that preoperative moderate hyperopia does not affect the surgical outcomes.Therefore, our study suggests that surgical correction can be considered for correcting infantile esotropia with moderate hyperopia.
This study had several strengths. Our study population was relatively homogeneous and all subjects underwent bilateral medial rectus muscle recession at a very young age (<24 months of age). Hileset al[23]reported no correlation between the refractive error and the development of an exodeviation or anatomic outcomes in patients with infantile esotropia who underwent bilateral medial rectus muscle recession before 1 year of age. However, in their study, only 8 of 54 patients had hyperopia greater than +3.00 D, which poses a limitation in determining the effect of hyperopia on postoperative alignment. Baeet al[24]also reported no apparent correlation between the refractive error and anatomical outcomes in patients with infantile esotropia who underwent bilateral medial rectus muscle recession. However, patient age at the time of surgery was 67mo and was highly variable (range 6mo-55y). Moreover, 64.3% of their patients were over 24 months of age at the time of surgery. Our study also had some limitations, mainly related to its retrospective design and relatively small sample size (particularly group II, as in the study by Hileset al[23]). Furthermore, we did not have access to stereoacuity testing results before or after surgery. Prospective,systematic studies that include a larger number of patients are needed.
In conclusion, preexisting moderate hyperopia prior to bilateral medial rectus muscle recession for infantile esotropia has no effect on the surgical outcome. Therefore, surgical correction of esotropia could be helpful for patients with preoperative refractive errors between +3.0 and +5.0 D when the angle of esodeviation is unchanged following hyperopic correction.
ACKNOWLEDGEMENTS
Conflicts of Interest: Lee HJ,None;Kim JA,None;Kim SJ,None;Yu YS,None.
REFERENCES
1 Helveston EM. 19th annual Frank Costenbader Lecture-the origins of congenital esotropia.J Pediatr Ophthalmol Strabismus1993;30(4):215-232.
2 Ing M, Costenbader FD, Parks MM, Albert DG. Early surgery for congenital esotropia.Am J Ophthalmol1966;61(6):1419-1427.
3 Costenbader FD. Infantile esotropia.Trans Am Ophthalmol Soc1961;59:397-429.
4 von Noorden GK. A reassessment of infantile esotropia. XLIV Edward Jackson memorial lecture.Am J Ophthalmol1988;105(1):1-10.
5 Wagner RS. Preservation of the monofixation syndrome following surgery for infantile esotropia.J Pediatr Ophthalmol Strabismus2015;52(6):334.
6 Park KA, Oh SY. Long-term surgical outcomes of infantile-onset esotropia in preterm patients compared with full-term patients.Br J Ophthalmol2015;99(5):685-690.
7 Magli A, Carelli R, Esposito F, Bruzzese D. Essential infantile esotropia:Postoperative sensory outcomes of strabismus surgery.Semin Ophthalmol2017;32(6):663-671.
8 Hug D. Management of infantile esotropia.Curr Opin Ophthalmol2015;26(5):371-374.
9 Chatzistefanou KI, Ladas ID, Droutsas KD, Koutsandrea C,Chimonidou E. Three horizontal muscle surgery for large-angle infantile or presumed infantile esotropia: long-term motor outcomes.JAMA Ophthalmol2013;131(8):1041-1048.
10 Birch E, Stager D, Wright K, Beck R. The natural history of infantile esotropia during the first six months of life. Pediatric Eye Disease Investigator Group.J AAPOS1998;2(6):325-328.
11 Cerman E, Eraslan M, Ogut MS. The relationship of age when motor alignment is achieved and the subsequent development of stereopsis in infantile esotropia.J AAPOS2014;18(3):222-225.
12 Bayramlar H, Karadag R, Yildirim A, Ocai A, Sari U, Dag Y. Mediumterm outcomes of three horizontal muscle surgery in large-angle infantile esotropia.J Pediatr Ophthalmol Strabismus2014;51(3):160-164.
13 Ing MR. Outcome study of surgical alignment before six months of age for congenital esotropia.Ophthalmology1995;102(12):2041-2045.
14 Burian HM. Hypermetropia and esotropia.J Pediatr Ophthalmol Strabismus1972;9:135-143.
15 Moore S. The natural course of esotropia.Am Orthopt J1970;21:80-83.
16 Ansons AM, Davis H. Diagnosis and management of ocular motility disorders. Fourth edition. New York: Wiley; 2014:706.
17 von Noorden GK. Infantile esotropia: a continuing riddle.Am Orthopt J1984;34(1):52-62.
18 Haynes H, White BL, Held R. Visual accommodation in human infants.Science1965;148(3669):528-530.
19 von Noorden GK, Campos EC. Binocular vision and ocular motility:theory and management of strabismus. Sixth edition. St. Louis: Mosby Inc, 2002.
20 Hwang JM, Min BM, Park SC, Oh SY, Sung NK. A randomized comparison of prism adaptation and augmented surgery in the surgical management of esotropia associated with hypermetropia: one-year surgical outcomes.J AAPOS2001;5(1):31-34.
21 Pediatric Eye Disease Investigator Group. Spontaneous resolution of early-onset esotropia: experience of the Congenital Esotropia Observational Study.Am J Ophthalmol2002;133:109-118.
22 Stager DR, Weakley DR Jr, Everett M, Birch EE. Delayed consecutive exotropia following 7-millimeter bilateral medial rectus recession for congenital esotropia.J Pediatr Ophthalmol Strabismus1994;31(3):147-150.
23 Hiles DA, Watson BA, Biglan AW. Characteristics of infantile esotropia following early bimedial rectus recession.Arch Ophthalmol1980;98(4):697-703.
24 Bae SH, Choi DG. Clinical features and surgical outcomes of infantile esotropia according to the age at surgery.J Korean Ophthalmol Soc2008;49(12):1961-1967.
Citation:Lee HJ, Kim JA, Kim SJ, Yu YS. Relation between preoperative hyperopia and surgical outcome in infantile esotropia.Int J Ophthalmol2018;11(12):1963-1967
DOl:10.18240/ijo.2018.12.15
● KEYWORDS:infantile esotropia; hyperopia; medial rectus muscle recession
Received:2017-07-08 Accepted: 2018-02-07
Correspondence to:Seong-Joon Kim. Department of Ophthalmology, Seoul National University College of Medicine, 101 Daehak-Ro, Jongno-Gu, Seoul 110-744, South Korea. ophjun@snu.ac.kr
 Age at initial visit, mo (range) 8.4±4.1 (3-20) 7.8±4.4 (4-17) 0.632aSex (M:F) 12:21 3:10 0.497aAge at surgery, mo (range) 12.5±3.8 (7-22) 11.8±4.5 (6-20) 0.633bPreop. mean refractive errors (D) +0.88±1.01 (-1.25 to +2.50) +3.45±0.51 (+3.00 to +4.50) <0.001bPreop. anisometropia (D) 0.35±0.29 (0.00-1.13) 0.23±0.30 (0.00-0.88) 0.427bPreop. angle of esodeviation (PD) 58.6±17.9 (30-85) 61.9±16.8 (30-80) 0.560bPreop. DVD,n(%) 1 (3.0) 1 (7.7) 0.490aPreop. IOOA,n(%) 11 (33.3) 4 (30.8) 0.999aPostop. follow-up period (mo) 41.7±30.2 (6-112) 52.0±31.2 (9-110) 0.305b
Age at initial visit, mo (range) 8.4±4.1 (3-20) 7.8±4.4 (4-17) 0.632aSex (M:F) 12:21 3:10 0.497aAge at surgery, mo (range) 12.5±3.8 (7-22) 11.8±4.5 (6-20) 0.633bPreop. mean refractive errors (D) +0.88±1.01 (-1.25 to +2.50) +3.45±0.51 (+3.00 to +4.50) <0.001bPreop. anisometropia (D) 0.35±0.29 (0.00-1.13) 0.23±0.30 (0.00-0.88) 0.427bPreop. angle of esodeviation (PD) 58.6±17.9 (30-85) 61.9±16.8 (30-80) 0.560bPreop. DVD,n(%) 1 (3.0) 1 (7.7) 0.490aPreop. IOOA,n(%) 11 (33.3) 4 (30.8) 0.999aPostop. follow-up period (mo) 41.7±30.2 (6-112) 52.0±31.2 (9-110) 0.305b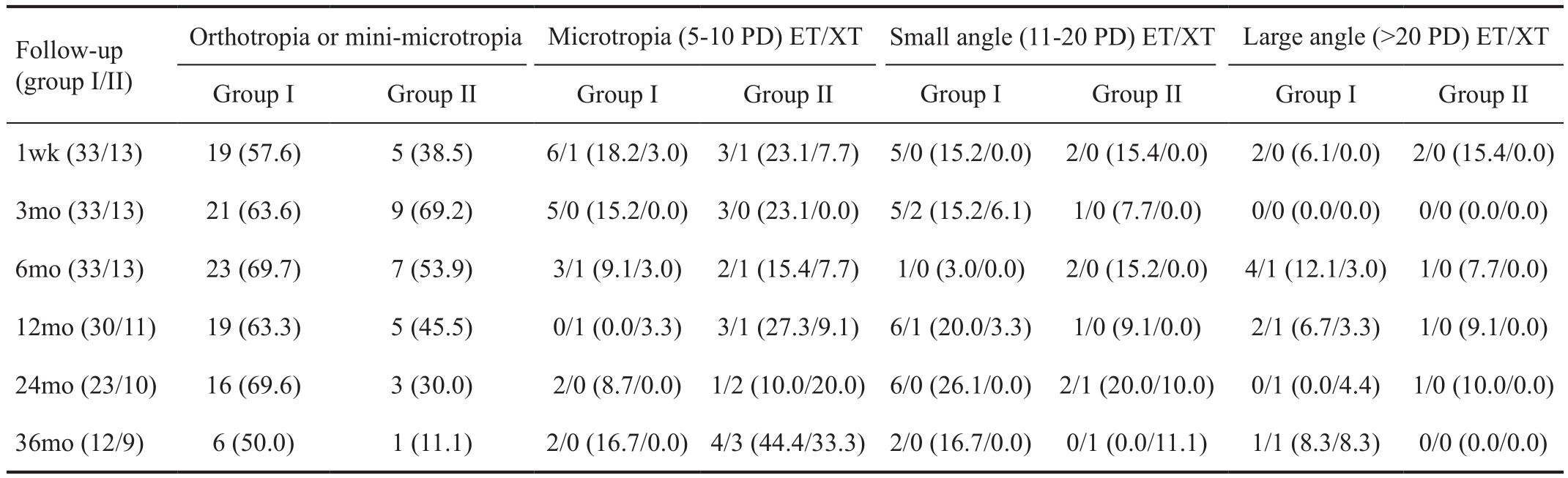
 Success (%) 23 (69.7) 8 (61.5) 0.730
Success (%) 23 (69.7) 8 (61.5) 0.730