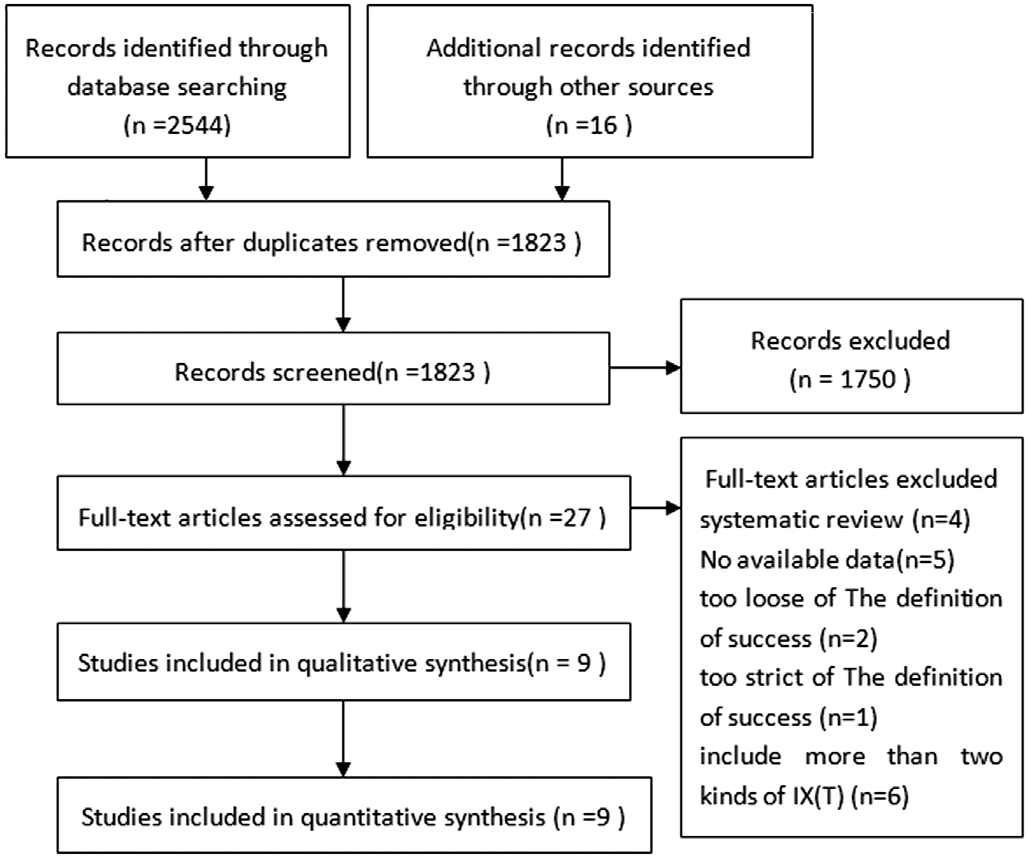
Figure 1 Flow chart of search process [based on Preferred Reporting Items for Systematic Reviews and Meta-Analyses(PRISMA) Guidelines].
Intermittent exotropia [IX(T)] is the most common type of exotropia, accounting for a proportion of up to 50% to 90% of all patients with exodeviation[1]. IX(T) is characterized by intermittent divergence of the optical axis, which is usually present initially on distance fixation or when the child is tired. The ocular misalignment may worsen or deteriorate into constant exotropia, which adversely affects stereo vision and may cause amblyopia; conversely the misalignment may resolve over time[2].
The commonly used surgical methods for IX(T) include bilateral lateral rectus recession (BLR), unilateral lateral rectus recession and medial rectus resection (R&R), of which, the R&R is considered to be more effective than BLR according to most of the clinical studies. However, it is suggested by Yukselet al[3]that BLR and R&R gained similar success rates after surgery. So, the conclusion of which surgical approaches is the best for treating IX(T) is still to be argued, given the divergent as above. Moreover, the evidence for the comparative effectiveness of both two kinds of surgeries is limited by the few randomized controlled trials (RCT; the comparison of efficacy of the two approaches is practically found in only one RCT). Although there are several observational studies have been conducted with strict experimental design and a relative long follow-up time, all of them are restrained by the insufficient sample size. To overcome the limitation of this,the very Meta-analysis was conducted to integrate all available data from the observational studies to finally draw a relatively reliable conclusion. In accordance with the difference of the deviation angle at distance fixation and near fixation, IX(T)can be classified as basic, true divergence excess, pseudodivergence excess and convergence insuf ficiency[4]. Since too many subtypes being involved in a Meta-analysis may lead to a tough job of the results interpretation and unconvinced conclusion, the surgical outcomes in patients with only basic IX(T) was evaluated in the Meta-analysis.
Unilateral lateral rectus recession (ULR) is often used to treat small-angle exotropia, and it is also an option for moderateangle exotropia. A large number of studies have compared the efficacy between BLR and R&R[5-9], but few articles directly compare the efficacy between ULR and R&R. So, a comprehensive literature search has been conducted regarding the articles in associated with such comparison on the ef ficacy between ULR and R&R, and then a review was performed to integrate the evidence with regard to the effectiveness of these two kinds of surgeries.
Literature SearchThree major databases (PubMed, EMBASE,and the Cochrane Library) were applied with suitable keywords irrespective of the language and date published,for relevant articles. The keywords for disease are exotropia,divergent strabismus, ocular misalignment, ocular deviation,intermittent exotropia; and for intervention, the keywords are surgery, operation, surgical operation. Furthermore, every relevant reference included in the articles was manually researched. In addition, other search routes, such as Google Scholar search engine and relevant organizational websites,were also appropriately applied.
Trials SelectionOnly literatures meeting the selection criteria established in advance were incorporated in this Meta-analysis.Selection criteria: 1) Basic type of IX(T) [the difference of deviation angle between distance fixation and near fixation less than 10 prism diopter (PD)] with patients younger than 18y; 2) Surgical intervention includes BLR and R&R and/or include ULR and R&R; 3) At least one of the primary outcome measures (success rate, overcorrection rate and undercorrection rate) can be extracted or calculated with data provided by the literature; 4) At least with a six-months follow-up; 5) The change of deviation angle was selected as one of the criteria to assess the success of surgery; 6) The de finition of a success is de finite.
Data ExtractionAfter discussion of two independent reviewers and referring to many literatures in this regard, some of the more important data were extracted, including location,age, number of patients, the duration of follow-up, types of IX(T), preoperative deviation, outcome variables, de finition of surgical success.
Quality AssessmentWith reference to the quality evaluation criteria of three representative retrospective cohort studies,in conjunction with the characteristics of the articles themselves, a quality appraisal standard consisting of eight items was built. If an article satis fied more than five of eight items (robust inclusion/exclusion criteria or consecutive recruitment, prospective study, guidelines/protocol applied for surgery, outcome appropriately measured, identify important confounding factors, adjust for confounding factors,followed-up for at least twelve months, authors’ conclusions substantiated by the reported data), it was then considered to be a high-quality retrospective cohort study.
The quality of RCT was assessed with Cochrane Handbook for Systematic Reviews of Interventions in terms of parameters of sequence generation, allocation concealment, masking(blinding), incomplete outcome data, selective outcome reporting, and other sources of bias.
Statistical AnalysisThis Meta-analysis was performed using RevMan 5.3 (Cochrane Community, UK). In which,mean differences (MDs) with 95%CIs and odd risks (ORs)with 95%CIs were used for continuous data and dichotomous data, respectively. While for heterogeneity, it was quantified using theI2statistic, andI2>50% indicates the presence of heterogeneity[10]. Then, the outcome data were integrated with a random-effects model that accounts for clinical heterogeneity,and aP<0.05 was considered statistically significant, except otherwise specified. In addition, publication bias was also assessed by visually inspecting a funnel plot.
Study CharacteristicsThe database searching identified 2544 trials, and another 16 trials were also found through other methods (including 9 trials by manual search on reference list of incorporated studies and 7 by Google Scholar engine).After removal of duplicates and suitable screening, only 27 of 2560 trials that was found to be preliminarily satis fied with the inclusion criteria; then an assessment of eligibility covering full text of all 27 articles was performed, which found that 3 of them have unreasonable de finition of success rate, and 5 of them were found without available data, and another 6 of them include more than two kinds of IX(T). Consequently,only 9 trials were eventually selected (Figure 1)[11-19].
Of these studies, six of nine compared BLR and R&R, and other three studies examined the surgical results of BLR and R&R. Only one of the eleven trials involved in the studies is RCT, and all of rest are observational studies with comparative group. Seven research literatures were conducted in Asia (two in China, four in Korea, one in Singapore). Two studies were in the United States. In all incorporated studies, parameters of success rate, recurrence rate and overcorrection rate were indicated.
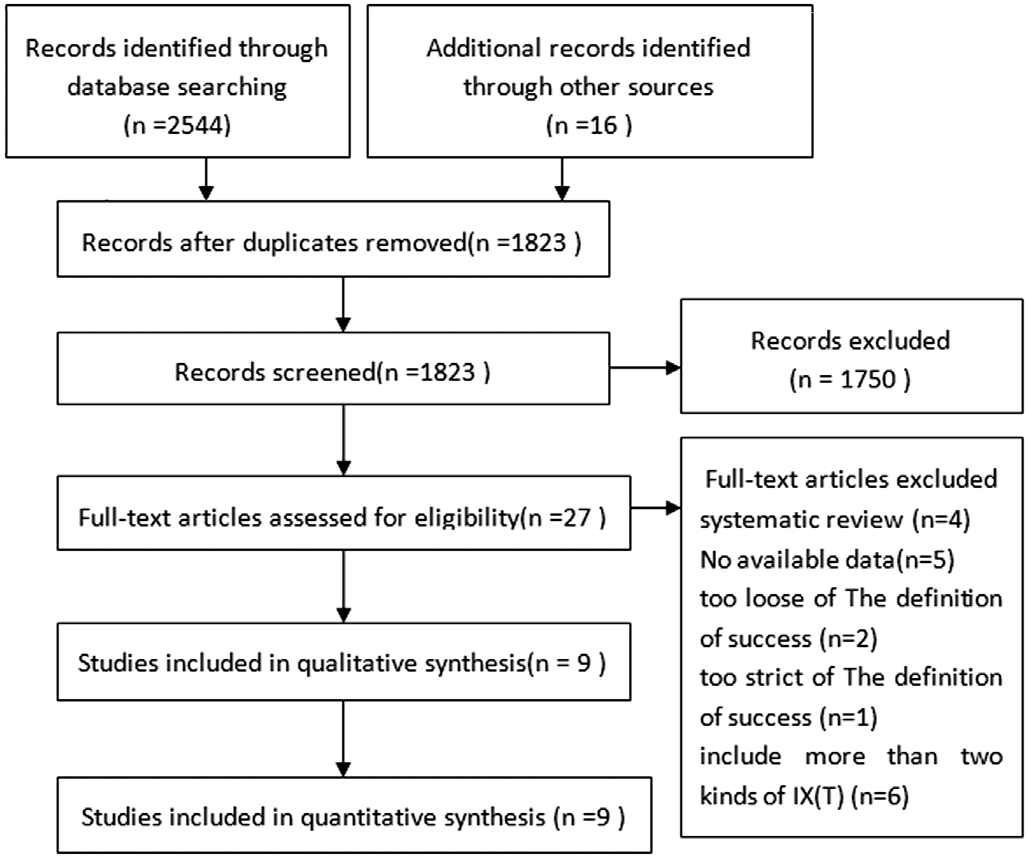
Figure 1 Flow chart of search process [based on Preferred Reporting Items for Systematic Reviews and Meta-Analyses(PRISMA) Guidelines].
In Wanget al’s[11]study, the definition of success was an esodeviation of ≤5 PD and exodeviation ≤8 PD at distance and near in primary position, respectively. After contacting the author, it is suggested that none patients’ postsurgery exodeviation angle was within 8 PD and 10 PD. Therefore,esodeviation of ≤5 PD and exodeviation ≤10 PD at distance and near in primary position was reasonably considered as the standard of surgery success in this article to eventually unify the conditions.
Similarity, in Chiaet al’s study[14], success was de fined as an IX(T) ≤10 PD, however the number of postoperative esotropic children and esodeviation angle of each esotropic children for both BLR and R&R group at final follow-up was given in the article, which enabled the possibility to calculate success rate,overcorrection rate, and recurrence rate, with the prerequisite of that an esodeviation of ≤5 PD and exodeviation of ≤10 PD at distance in primary position was thought to be success of surgery.So far, the definition of success was unified in all 6 studies.Table 1 shows the main characteristics of the included trials.
Risk of Bias in Included Studies
Randomized controlled trialsOnly one RCT was incorporated in this Meta-analysis[16]. The study has an unclear risk of bias in some areas according to the Cochrane Handbook, since the two procedures of randomization and allocation concealment were not described very clearly. In addition, the detection bias concerned for the blinding is not used in the evaluation of outcome.
Cohort studiesEight studies with comparison groups were included in this Meta-analysis. In seven of all studies[11-14,17-19],patients were recruited continuously, and the cases were selected in accordance with defined inclusion and exclusion criteria. And in the rest one study, details of patient recruitment were poorly selective[15]. There is a possibility of selection bias in at least five studies as the absence of standard protocol for the choice of IX(T) surgical procedure[12,14-15,17,19]. In most cases, intervention was made by the surgeon based on their experience, and sometimes, the decision was made after discussion between the surgeon and patient(s). Six articles were referred to guidelines and/or a standardized protocol to determine the surgical formula[11,13,15-16,18-19].
There are so many outcome indicators could be used to evaluated the effect of surgery, like postoperative angle of deviation, sensory function, control or the combination of above. In this Meta-analysis, all incorporated studies provide motor alignment and/or improvement and/or success rates.But as regard to the issue of how to determine the success of the operation, it is still divergent. Most authors de fine surgical success as esodeviation of ≤5 PD to exodeviation of ≤10 PD at distance in primary position on each follow-up visit. However,both a stricter and a looser de finition of success [e.g.IX(T)<10 PD,or orthophoria <10 PD esotropia/exotropia, 8 PD of exophoria and 8 PD of esophoria, 10 PD of exophoria and 10 PD of esophoria] are employed by others. In order to minimise clinical heterogeneity, only studies with a definition of the success as an esodeviation of ≤5 PD to exodeviation of ≤10 PD at distance in primary position or the success rate of which can be calculated through the data provided, were incorporated in the Meta-analysis.
Two studies[13-14]did not report the patients’ age and angle of deviation at baseline, both of which are important in fluential confounding factors. The difference of age and motor alignment at baseline was not statistically signi ficant between two compared groups in other studies (Table 2).
Quantitative Synthesis
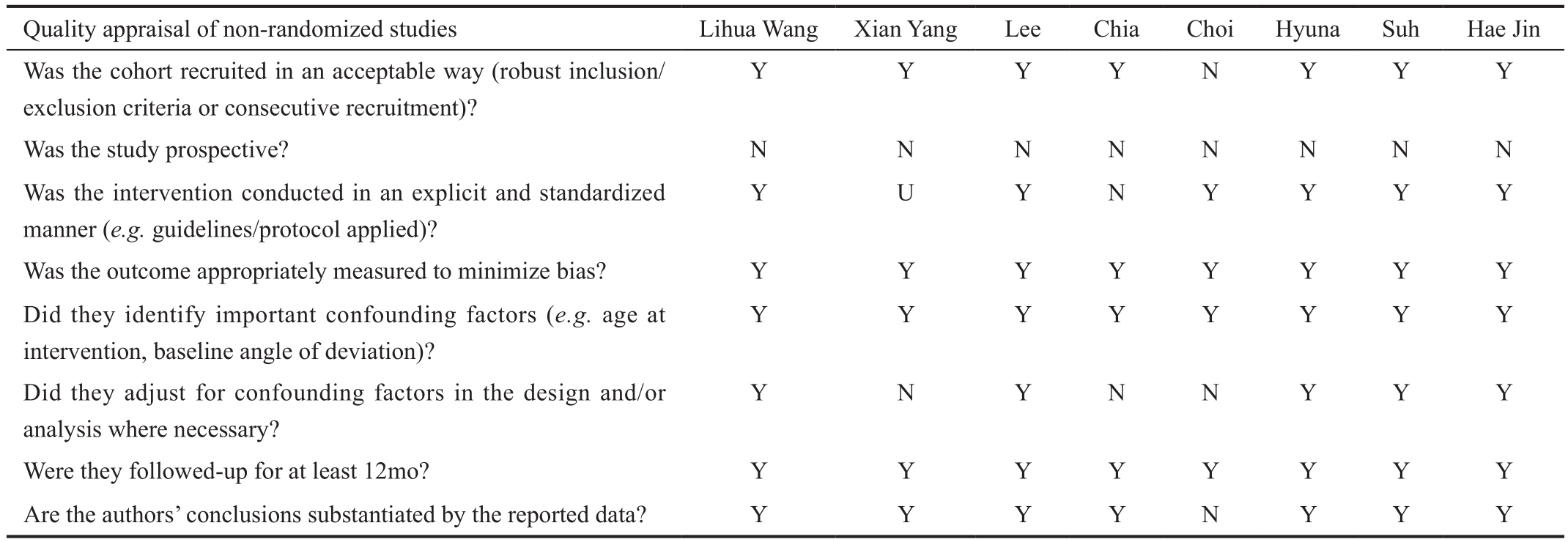
BLR versus R&RThe success rate of two kinds of surgeries:Seven studies compared the success rate of BLR versus R&R,and found that the difference was not statistically significant between two groups (pooled OR=0.96, 95%CI 0.43, 2.10),while the heterogeneity of the outcome was evident (I2=78%,P<0.001; Figure 2).
Age of surgery onset, preoperative angle of deviation and follow-up time are important factors that in fluence the outcome of surgery. After a subgroup analysis in aspects of the age and the preoperative deviation angle, an evident heterogeneity was also observed. However, a stratify analysis in term of the length of follow-up time indicated that BLR achieved higher success rate (pooled OR=2.49, 95%CI 1.61, 3.86) with little heterogeneity identi fied (I2=39%,P=0.20) for a mean duration of follow-up of more than 2y. While, for a mean duration of follow-up of less than 2y, R&R group was superior to the BLR group, given that patients from R&R group acquired a much higher success rate (OR=0.56, 95%CI 0.33, 0.94) without identi fied heterogeneity (I2=9%,P=0.35; Figure 3).
Table 1 Description of studies

RCT: Random control trial; BLR: Bilateral lateral rectus recession; R&R: Unilateral lateral rectus recession combined with medial rectus resection; ULR:Unilateral lateral rectus recession; D: Distance; N: Near; NN: Not note; PD: Prism diopter; O: Overcorrection; S: Success; U: Undercorrection.
First author,year, country Study design/follow-up Type /Age Final sample size Preoperative deviation,PD Postoperative outcomes De finition of surgical success Wang LH,2013, China Esodeviation of ≤5 PD to exodeviation of ≤8 PD at distance and near in primary position Yang X,2014, China Retrospective study/BLR: 16.4±9.7mo;R&R: 13.5±9.2m Basic type IX(T)/BLR: 7.39±3.14y;R&R: 8.15±2.47y BLR: 38; R&R: 47 BLR, D:33.5±7.1;N: 34.3±8.3; R&R,D: 32.9±9.2;N: 36.4±6.7 BLR, O:4,S:25,U:9;R&R, O:4,S:40,U:3 Retrospective study/BLR: Mean:3.7y;R&R: Mean:3.7y Basic type IX(T)/BLR: 13.81±7.81y;R&R: 14.25±7.81y BLR: 107; RR:106 BLR, D: 41.68±17.03;N: 44.39±15.26; R&R,D: 58.82±27.60;N: 68.21±23.04 BLR, O:3,S:65,U:39;R&R, O:4,S:46,U:56 Esodeviation of ≤5 PD to exodeviation of ≤10 PD at distance in primary position Lee S,2001, Korea Esodeviation of ≤5 PD to exodeviation of ≤10 PD at distance in primary position on each follow-up visit.Chia A,2005, Singapore Retrospective study/1y Basic type IX(T)/mean age of 7.1y BLR: 46; R&R: 57 NN BLR, O:3,S:26,U:17;R&R, O:6,S:34,U:17 Esodeviation of ≤5 PD to exodeviation of ≤10 PD at distance in primary position Choi J,2012, Korea Retrospective study/1y Basic type IX(T)/under 16y BLR: 26; R&R: 11 BLR, D: 38.7±6.9;N: 18.5±17.6; R&R,D: 38.4±6.5; N: 7.7±14.5 BLR, O:0,S:8,U:18;R&R, O:0,S:7,U:4 Retrospective study/BLR: 44.2±15.8mo;R&R: 47.8±16.9mo,24mo minimum follow-up Basic type IX(T)/BLR: 6.8±3.4 y;R&R: 7.2±2.3 y BLR: 55; R&R: 73 BLR, D: 40.5±5.8;N: 40.0±8.0; R&R,D: 29.4±3.8;N:30.5±6.4 BLR, O:2,S:32,U:21;R&R, O:3,S:20,U:50 Success was de fined as esophoria/tropia ≤5 PD to exophoria/tropia ≤10 PD Burton J.Kushner,1998, America Success was de fined as esophoria/tropia ≤5 PD to exophoria/tropia ≤10 PD Kim H,2016, Korea RCT/1y follow-up(range 12-15mo)Basic type IX(T)/BLR: 5.3±2.7y,R&R: 5.5±2.9y R&R: 17; BLR: 87 BLR, D: 29.8±6.3;R&R, D: 28.1±4.7 BLR, O:5,S:65,U:17;R&R, O:1,S:14,U:2 esodeviation of ≤5 PD to exodeviation of ≤10 PD at distance in primary position Suh SY,2015, America Retrospective study/ULR: 3.6±1.6y;R&R: 3.1±1.0y Basic and true divergence excess IX(T)/ULR:7.0±2.5; R&R: 7.0±2.3 ULR: 69; R&R: 61 ULR, D: 19.2 ±1.4;N: 17.7±2.7; R&R,D: 18.7±2.5; N: 18.3±2.3 ULR, O:2,S:26,U:41;R&R, O:5,S:38,U:18 Retrospective study/ULR: 37.1±16.5mo(range, 24-78mo);R&R: 44.6±18.5mo(range, 24-84mo)Basic and true divergence excess IX(T)/ULR: 78.5±22.2mo;BLR: 77.5±24.2mo ULR: 37; R&R: 33 ULR, D: 22.2±2.1; N:22.3±3.3; R&R,D: 24.5±1.4;N: 26.4±3.6 ULR, O:0,S:17,U:20;R&R, O:3,S:13,U:17 Esodeviation of ≤5 PD to exodeviation of ≤10 PD at distance in primary position Kim HJ,2014, Korea Retrospective study/ULR: 53.8±26.4mo;R&R: 52.5±27.4mo Basic type IX (T)/ULR: 5.93±2.35y;R&R: 6.76±2.31y ULR: 82; RR: 98 ULR, D:22.07±2.48;N: 22.01± 3.41; R&R,D: 22.76± 2.49;N: 22.87± 4.12 ULR, O:0,S:50,U:32;R&R, O:0,S:55,U:43 Esodeviation of ≤10 PD to exodeviation of ≤10 PD at distance in primary position
Table 2 Quality appraisal of studies
N: Not addressed; U: Unclear or not reported; Y: Adequately addressed.
 Was the cohort recruited in an acceptable way (robust inclusion/exclusion criteria or consecutive recruitment)?Y Y Y Y N Y Y Y Was the study prospective? N N N N N N N N Was the intervention conducted in an explicit and standardized manner (e.g.guidelines/protocol applied)?Y U Y N Y Y Y Y Was the outcome appropriately measured to minimize bias? Y Y Y Y Y Y Y Y Did they identify important confounding factors (e.g.age at intervention, baseline angle of deviation)?Y Y Y Y Y Y Y Y Did they adjust for confounding factors in the design and/or analysis where necessary?Y N Y N N Y Y Y Were they followed-up for at least 12mo? Y Y Y Y Y Y Y Y Are the authors’ conclusions substantiated by the reported data? Y Y Y Y N Y Y Y
Was the cohort recruited in an acceptable way (robust inclusion/exclusion criteria or consecutive recruitment)?Y Y Y Y N Y Y Y Was the study prospective? N N N N N N N N Was the intervention conducted in an explicit and standardized manner (e.g.guidelines/protocol applied)?Y U Y N Y Y Y Y Was the outcome appropriately measured to minimize bias? Y Y Y Y Y Y Y Y Did they identify important confounding factors (e.g.age at intervention, baseline angle of deviation)?Y Y Y Y Y Y Y Y Did they adjust for confounding factors in the design and/or analysis where necessary?Y N Y N N Y Y Y Were they followed-up for at least 12mo? Y Y Y Y Y Y Y Y Are the authors’ conclusions substantiated by the reported data? Y Y Y Y N Y Y Y
The overcorrection rate of two kinds of surgeries: six studies compared the overcorrection rate of BLR versus R&R. In all these six papers, the success was de fined as that the alignment should be within 10 PD of exophoria/tropia and 5 PD of esophoria/tropia at distance in the primary position. Pooled results suggested that both two groups were much the same with statistically insigni ficant difference for the overcorrection(OR=0.85, 95%CI 0.41, 1.75), and with no identified heterogeneity (I2=0,P=0.97; Figure 4).
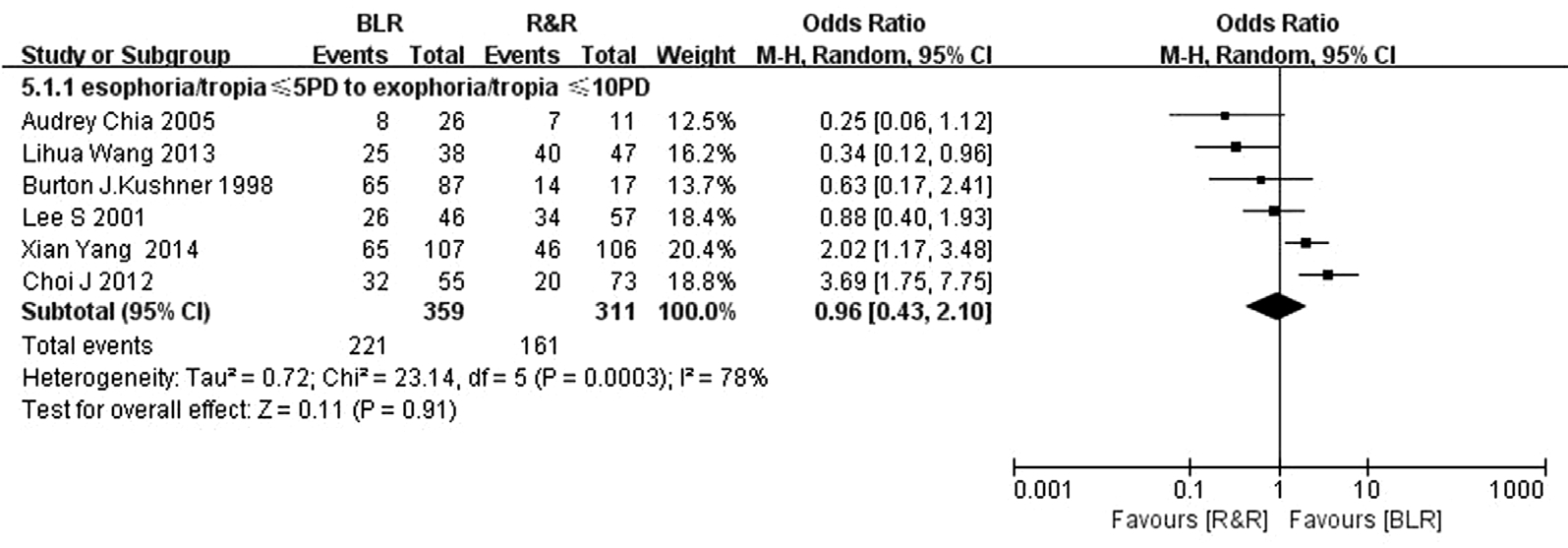
Figure 2 The rate of success comparing bilateral lateral rectus recession and unilateral lateral rectus recession and medial rectus resection.

Figure 3 Strati fied analyses of success rate comparing bilateral lateral rectus recession and unilateral lateral rectus recession and medial rectus resection according to the duration of follow-up.

Figure 4 The rate of overcorrection comparing bilateral lateral rectus recession and unilateral lateral rectus recession and medial rectus resection.
The recurrence rate of two kinds of surgeries: six studies focused on the comparison of the recurrence rate between the two groups. In all six papers, the definition of success was that the alignment should lie between 10 PD of exophoria/tropia and 5 PD of esophoria/tropia at distance in the primary position. The pooled result of two compared groups was comparable (OR=1.16, 95%CI 0.49, 2.77), however, with evident heterogeneity for the outcome (I2=77%,P<0.001;Figure 5).
To explore the study heterogeneity, a subgroup analyses covering all factors of age of surgery onset, preoperative angle of deviation and the length of follow-up was conducted. As a result, it is found that the former two factors had no effect on the reduction of heterogeneity. But when the duration of follow-up was more than 2y, the pooled result was in favor of R&R (OR=0.40, 95%CI 0.23, 0.71) with little identified heterogeneity (I2=37%,P=0.21). While, if the length of followup was less than 2y, the BLR showed better performance(OR=2.11, 95%CI 1.17, 3.81) without identi fied heterogeneity for the outcome (I2=0,P=0.41; Figure 6).
Publication bias: There was no evidence of publication bias according to inspection of the funnel plot (Figure 7).

Figure 5 The rate of recurrence comparing bilateral lateral rectus recession and unilateral lateral rectus recession and medial rectus resection.
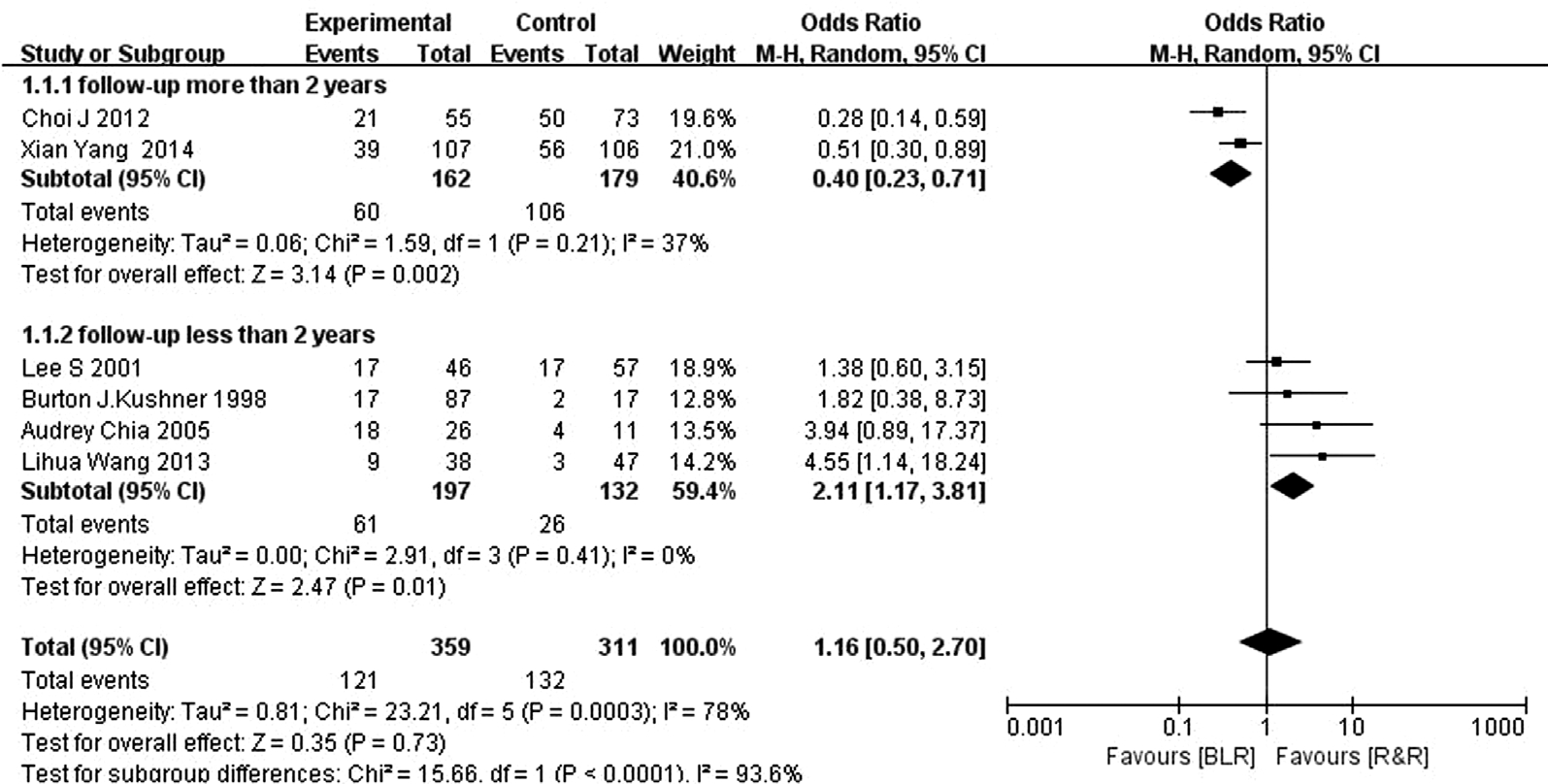
Figure 6 Strati fied analyses of undercorrection rate comparing bilateral lateral rectus recession and unilateral lateral rectus recession and medial rectus resection according to the preoperative angle of deviation.
ULR versus R&RThree trials with more than 180 participants evaluated the effectiveness between the two compared groups of ULR and R&R. In two retrospective studies of all the three trials, the success of surgery was defined as alignment between 10 PD of exophoria and 5 PD of esophoria; while for the Kimet al’s[19]study, the success of surgery was defined as the alignment within 10 PD of orthotropia. After reading the full text, it is found that no patient in either group was postoperatively overcorrected at final follow-up, so all the surgery success rate, overcorrection rate and recurrence rate can be calculated in Kimet al’s[19]study if the success of surgery was defined as an alignment between 10 PD of exophoria and 5 PD of esophoria. This ensured the consistency of success standards of surgery for all three articles.
In the two studies, the type of IX(T) included both basic and true divergence excess, of which, the later one was very little, only two true divergence excess IX(T) are in Kimet al’s[17]study.
Analysis results show that the ULR and R&R were equivalent to some extent in term of success rate (OR=0.82, 95%CI 0.36,1.89). The mean duration of follow-up of more than 2y and a same follow-up period of more than 3y are for all the 3 trials involved. In addition, it is also found that the heterogeneity of outcome is evident (I2=74%,P=0.65), and such heterogeneity was not affected by the factor of age. In the subgroup analysis concentrating on the angle of preoperative deviation, it is found that in both studies by Suhet al[18]and Kimet al[19], the preoperative angle of exodeviation was between 20 PD and 25 PD (moderate angle exotropia); moreover, the pooled result was consistent with that of previous one (OR=1.08, 95%CI 0.65, 1.79). In Kimet al’s[17]study, a total of 130 children with IX(T) of ≤20 PD (small angle exotropia) were involved, and the results indicated that R&R has a better outcome than ULR(OR=0.37, 95%CI 0.18, 0.74; Table 2).

Figure 7 Tests for publication bias of the success rate.
All three studies compared the overcorrection rate of ULR versus R&R. The difference between two compared groups(pooled OR=0.26, 95%CI 0.06, 1.12) was not found, as well as the identi fied heterogeneity (I2=0,P=0.07; Table 2).
ULR and R&R have a similar recurrence rate (pooled OR=1.40, 95%CI 0.93, 2.09) with evident heterogeneity(I2=79%,P=0.1). After stratifying included studies with regard to the preoperative angle of deviation, the pooled results of Suhet al’s[18]and Kimet al’s[19]study that with children exodeviation of 20 PD to 25 PD was consistent with previousone (OR=0.89, 95%CI 0.54, 1.48), and the Kimet al’s[17]study with children IX(T) of ≤20 PD was in favour of R&R(OR=3.50, 95%CI 1.68, 7.26; Table 3).
Table 3 Stratified analyses of success, overcorrection and recurrence rate according to preoperative angle of deviation comparing unilateral lateral rectus recession and unilateral lateral rectus recession and medial rectus resection
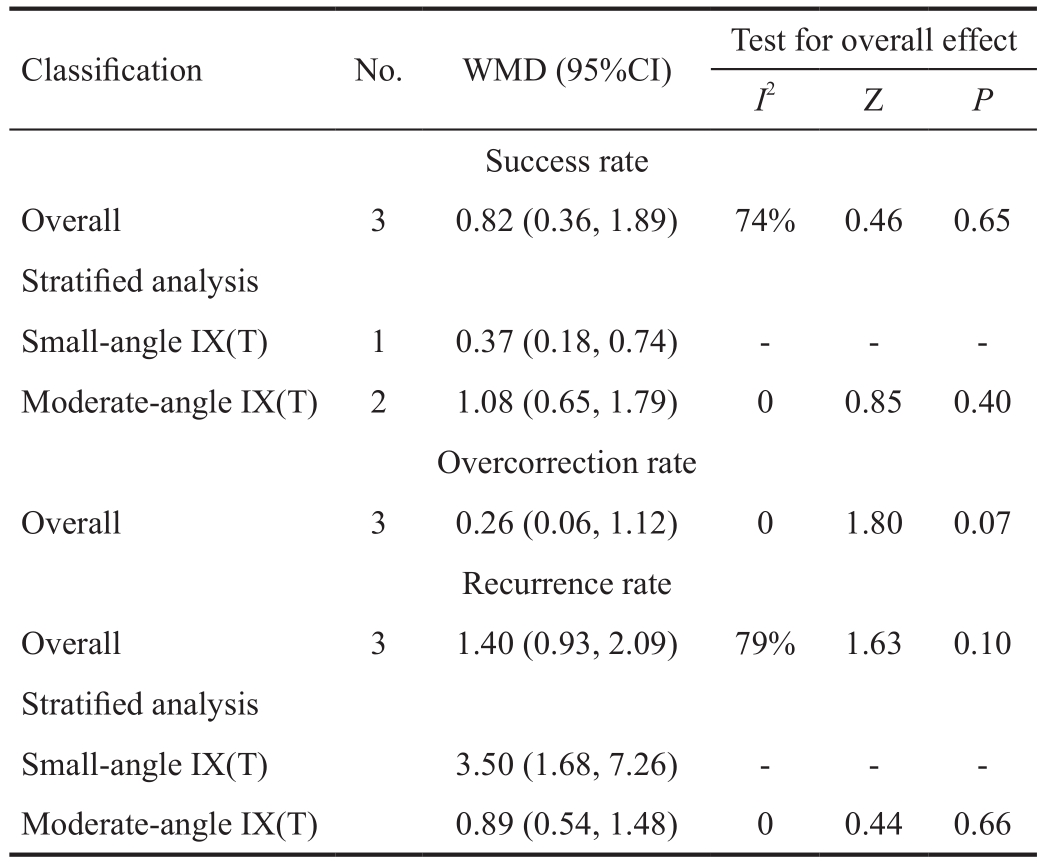
 Success rate Overall 3 0.82 (0.36, 1.89) 74% 0.46 0.65 Strati fied analysis Small-angle IX(T) 1 0.37 (0.18, 0.74) - - -Moderate-angle IX(T) 2 1.08 (0.65, 1.79) 0 0.85 0.40 Overcorrection rate Overall 3 0.26 (0.06, 1.12) 0 1.80 0.07 Recurrence rate Overall 3 1.40 (0.93, 2.09) 79% 1.63 0.10 Strati fied analysis Small-angle IX(T) 3.50 (1.68, 7.26) - - -Moderate-angle IX(T) 0.89 (0.54, 1.48) 0 0.44 0.66
Success rate Overall 3 0.82 (0.36, 1.89) 74% 0.46 0.65 Strati fied analysis Small-angle IX(T) 1 0.37 (0.18, 0.74) - - -Moderate-angle IX(T) 2 1.08 (0.65, 1.79) 0 0.85 0.40 Overcorrection rate Overall 3 0.26 (0.06, 1.12) 0 1.80 0.07 Recurrence rate Overall 3 1.40 (0.93, 2.09) 79% 1.63 0.10 Strati fied analysis Small-angle IX(T) 3.50 (1.68, 7.26) - - -Moderate-angle IX(T) 0.89 (0.54, 1.48) 0 0.44 0.66
Main FindingsTo our best knowledge, this is the first Metaanalysis of comparing three main kinds of surgeries for treating iIX(T), and found that 1) for basic type IX(T), BLR can acquire a higher success rate and lower recurrence rate when the duration of follow-up is more than 2y, while R&R has a better cure rate and lower undercorrection rate when the during of follow-up is less than 2y, and overcorrection rate is same for both; 2) for moderate angle IX(T), the ef ficacy of ULR surgery is comparable to R&R surgery (mean duration of followup >2y). For small angle IX(T), R&R has a better long-term outcome (mean duration of follow-up >3y); 3) R&R surgery show a higher exotropic drift than BLR in the long term.
BLR versus R&RLee and Choi[20]reported that the mean follow-up time point of surgical recurrence is 21.3mo. Furthermore,in another study previously conducted by Jeounget al[21], a Kaplan-Meier survival analysis showed that an estimated mean duration from surgery to failure was 23.0±1.9mo in a BLR group and 28.3±2.1mo in an R&R group. So 2y could be used as the point for stratifying follow-up time.
In order to minimize heterogeneity between articles, only studies, the success of which can be got when it was de fined as esodeviation of ≤5 PD to exodeviation of ≤10 PD at distance in primary position, were included. For comparison between BLR and R&R, only the basic type IX(T) was included. For ULR and R&R, only two studies included both basic and true divergence excess type IX(T) due to limited researches were available in this area. Actually, one of these two study only included basic type IX(T).
The success rate of BLR surgery ranged from 43% to 83%[3,13-14,16,21-28],and R&R surgery varied from 33% to 83%[3,13-14,16,26-28]. In Chiaet al’s[14]study, at the end of 1-year follow-up, R&R was more successful than BLR with success rate of 74.2% to 42.2%. In addition, Jeounget al[21]and Kushneret al’s[16]reports showed that R&R had significantly better surgical outcomes at 1.3-year and 1-year follow-up, respectively. However, a report by Maruoet al[26]stated that BLR showed a better outcome than that of R&R at the end of 4-year follow-up with success rate of 66.7% and 32.8%. In Choiet al’s[15]study, surgical outcomes by 2y after surgery for IX(T) were not different between the two compared groups. However, for the final outcomes (a mean duration of 3.8-year follow-up), the BLR group was better than the R&R group. In this study, BLR had a higher success rate and lower recurrence rate for a duration of follow up of more than 2y, by contrast, R&R showed better effects on cure rate and undercorrection rate for a duration of followup of less than 2y; while for the overcorrection rate, both two compared groups were similar, regardless of the duration of follow-up, indicating that more exotropic drift of R&R than BLR during these periods. Therefore, the hypothesis of that BLR is in possession of a better and more stable long-term surgical outcome than R&R is well justi fied. More RCTs are necessarily required to verify such hypothesis.
As already mentioned above, IX(T) could be divided into four types with respect to the different angle of deviation at distance and near fixation. Classical teaching tells that different types of IX(T) are adapted to different surgical methods. For instances,R&R is better for convergence insufficiency exotropia, BLR is better for divergence excess exotropia, and for basic-type exotropia, both BLR and R&R are recommended. However,in Kushner’s[16]study, R&R showed a better surgical outcome than BLR in basic type IX(T) at postoperative 1y, which is very different from classical theory, and a similar outcome between two compared groups at postoperative 2y was indicated by Choiet al’s[15]study; however, when the mean duration of follow up is more than 46mo, BLR achieved a higher satisfactory outcome than R&R in basic type IX(T).
Subsequent exotropic[4,29-30]shift with R&R is common, which is mainly attributed by two explanations. First, medial rectus resection may cause an immediate tethering effect, and result in initial success, but, incomitance of lateral gaze could cause a gradual loss of fusion and exotropic shift. Another possible explanation is the muscle stretching in the long-term caused by the resected medial rectus tension, which may contribute to a weakness of the tethering effect.
ULR versus R&RLeeet al[5]has reported that ULR’s success rate was 85.7% in the treatment of IX(T) under 25 PD at postoperative 1y. Wanget al[6]also stated ULR is a safe and effective surgery for small to moderate angle (15 to 35 PD)IX(T) with a minimum follow-up of 6mo (success of 76%;orthophoria or <10 PD exotropia). Dadeya and Kamlesh[7]conducted a long-term follow-up (3y), and found that patients who underwent ULR had satisfactory results (±5 PD of orthophoria) in the treatment of IX(T) with a deviation of 25 to 30 PD (success of 77.7%). In the very study, results of a Metaanalysis also indicate that ULR is an attractive alternative procedure in the treatment of IX(T) with a deviation of 25 to 30 PD, when compared with R&R.
In addition, a report by Yanget al[8]demonstrated that subjects who underwent ULR showed a significantly better outcome at a 3-year follow-up (success rate of 74.2%; esophoria/tropia≤5 PD to exophoria/tropia ≤10 PD), however a significantly more exotropic drift over time is also indicated. And predictive factors of recurrence were a larger preoperative near angle of deviation (>16 PD) and larger initial postoperative exodeviation (>5 PD) at distance. In Lyuet al’s[9]study, patients with 20-24 PD of IX(T) showed a worse prognosis compared with 15-19 PD of IX(T) (followed up >2y). For lesser preoperative angle of deviation, ULR tended to show better surgical outcome. The results of the very study do not support the hypothesis, since the ULR is found to be an effective surgical method for correcting moderate-angle exotropia with results similar to that of R&R. However, only one study involved in the Meta-analysis compared the outcome of ULR and R&R for small-angle exotropia, and more satisfactory surgical outcome was obtained in R&R. The reason of this that interpreted by author of the study is that the proportion of patients in the paper with good stereopsis (60.7% of RR, 73.9% of ULR)was lower than other studies. Since the quantity and quality of included literatures were not enough, the conclusion is not very credible, and further long-term prospective studies with sufficient number of samples are needed to verify the hypothesis.
ImplicationThe basic-type IX(T) appears to be the most common of the subtypes and is also the type for which there is the most divergences regarding the issue of which surgical approach is the best. BLR and R&R are the two most common procedures[4]. Most western clinicians prefer to use BLR, as this kind of surgery will not cause incomitance on horizontal gaze for symmetry of the surgery. However, R&R could lead to evident diplopia when the eye moves in the direction of the recession lateral muscle, the situation of which will be gradually improved over time. Some IX(T) children’s binocular vision function was severely damaged, which lead to poorer convergence ability with near point of convergence more than 10 cm. Many ophthalmologists, especially in China,think medial rectus resection could enhance the ability of convergency and prevent recurrence of IX(T), so they prefer to choose R&R for these kinds of patients. Others state that postoperative convergence capacity improvement is consistent regardless of what kind of surgical approach is applied,as long as the degree of postoperative strabismus is in the normal range and binocular vision function can be restored.The above two situations can be used as a reference for our choice of suitable surgical method, but which type of surgery is to be chosen is still depends on the long-term prognosis,including decrease of strabismus degree, improvement of stereopsis, and enhancement of control ability. The change of strabismus angle can re flect the curative effect of the operation intuitively and get the recognition of their families, therefore,most clinicians like to use it as an indicator to determine the success of surgery. In this Meta-analysis, success was de fined as esophoria/tropia ≤5 PD to exophoria/tropia ≤10 PD, and then the BLR and R&R groups were found with no signi ficant difference for surgical outcomes by 2y. However, BLR could acquire a better long-term (>2y) surgical result than R&R group, while continuous recurrence in the R&R group leads to a high failure rate. Therefore, BLR should be the better choice for the basic type of IX(T) in the long run. The main purpose of IX(T) surgery is to restore binocular function and reduce the frequency of exotropia, so measurements of preoperative and postoperative stereopsis and control are particularly important.The combination of three indicators to evaluate the ef ficacy of surgery will enable us a more comprehensive understanding of the recovery of those patients who suffered a reduced degree of strabismus, but poorer functional recovery may also require appropriate binocular vision training.
The other question is about follow-up time. Due to the lack of long-term post-operative natural history studies, it is dif ficult to know how long the time two surgical procedures will take to reach a stable period, and to check whether the two surgeries are stable at then. From this article, it is indicated that if the follow-up time is too short, it will cause a false impression of both surgical procedures have a relatively high success rate,and R&R showed a better outcome than BLR. In fact, with extending follow-up time, the success rates of both surgeries were declining, and R&R has a higher rate of recurrence, while BLR could acquire a relatively better result. So in clinical practice, postoperative follow-up should be as long as possible and at least more than 3y. Because some patients could have a good alignment in the short term, and overtime may be slowly back, if such case is found by the clinician in the follow-up process, certain preventive measures, such as binocular vision training, should be taken. Perhaps there is no need to take a second operation, but if the follow-up time is too short, the patients are highly likely to have secondary surgery.
In order to reduce postoperative complications and leave room for future re-operation, for small and moderate-angle IX(T),ULR is often recommended. Larger amount of recession of single lateral rectus may lead to complications like abduction limitation and lateral incomitance. However, according to our experience and other authors’ reports, these two cases rarely occur, and even when lateral incomitance occurred after ULR, it tends to balance out over time and is not clinically significant. This can be considered as a reference factor for the choice of procedure, but not as a determinant. Our main consideration is the long-term postoperative stability of surgery, and many clinical studies have shown that ULR surgery has a good long-term outcome. Recently, however,ULR also is reported to have a good effect on moderate-angle exotropia (20-25 PD). According to the conclusions drawn in this article, R&R is recommended for small-angle IX(T),and both ULR and R&R are proper for moderate-angle IX(T).Only three retrospective cohort studies compared R&R were included in this paper, which makes the conclusion reached hardly convincing. Actually, the paper is just to summarize the latest researches in this area and have them analyzed to derive some assumptions that may inspire later scholars to eventually address the question of the best surgical approach for treat small and/or moderate angle divergence excess and/or basic IX(T) in children, by conducting more well-designed RCTs.
LimitationThis Meta-analysis was carried out using robust methods. Of which, the search strategy was not limited by language or date, so the possibility of missing relevant studies should be very low. Moreover, the quality of selected articles was assessed by two independent researches using widely used Critical Appraisal Skills Programme (CASP) checklist. At the same time, this paper is limited in some aspects, of which, the main one is that the design of most studies incorporated in the Meta-analysis is suboptimal. The RCT is the best choice for comparing effectiveness of two kinds of interventions,however there is only one RCT was involved in the entire article, and the quality of this study is not good enough. Due to the lack of high-quality researches in this regard, a more practical approach was employed, shifting the line of sight to studies with next level evidence (retrospective cohort studies with a comparison group). Observational research has inherent design flaws, for example, the selection bias led by the absence of strict method of allocation, which increases the risk of confounding factors on the outcome, such as preoperative deviation or age[9]. Although the difference of the followup period could increase the heterogeneity between different groups, the same type of IX(T) as well as measured outcomes and the definition of success can make the Meta-analysis possible.
Foundation:Supported by Young Medical Talents Foundation of Jiangsu Province (No.QNRC2016080).
Conflicts of Interest: Song DS, None; Chen ZJ, None; Qian J, None.
1 Nusz KJ, Mohney BG, Diehl NN. The course of intermittent exotropia in a population-based cohort.Ophthalmology2006;113(7):1154-1158.
2 Buck D, Powell CJ, Rahi J, Cumberland P, Tif fin P, Taylor R, Sloper J,Davis H, Dawson E, Clarke MP. The improving outcomes in intermittent exotropia study: outcomes at 2y after diagnosis in an observational cohort.BMC Ophthalmol2012;12:1.
3 Yuksel D, Spiritus M, Vandelannoitte S. Symmetric or asymmetric surgery for basic intermittent exotropia.Bull Soc Belge Ophtalmol1998;268:195-199.
4 Burian HM. Exodeviations: their classi fication, diagnosis and treatment.Am J Ophthalmol1966;62(6):1161-1166.
5 Kim SH, Choi YJ. Effects of unilateral lateral rectus recession according to the tendon width in intermittent exotropia.Eye (Lond)2006;20(7):785-788.
6 Wang LH, Nelson LB. Outcome study of unilateral lateral rectus recession for small to moderate angle intermittent exotropia in children.J Pediat Ophthalmol Strab2010;47(4):242-247.
7 Dadeya S, Kamlesh. Long-term results of unilateral lateral rectus recession in intermittent exotropia.J Pediat Ophthalmol Strab2003;40(5):283-287.
8 Yang HK, Kim MJ, Hwang JM. Predictive factors affecting Long-term outcome of unilateral lateral rectus recession.PLoS One2015;10(9):e0137687.
9 Lyu IJ, Park KA, Oh SY. Long-term surgical outcomes and factors for recurrence after unilateral lateral rectus muscle recession.Br J Ophthalmol2016;100(10):1433-1436.
10 Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in Meta-analyses.BMJ2003;327(7414):557-560.
11 Wang LH, Wu QZ, Kong XY, Li ZW. Comparison of bilateral lateral rectus recession and unilateral recession resection for basic type intermittent exotropia in children.Br J Ophthalmol2013;97(7):870-873.
12 Yang X, Man TT, Tian QX, Zhao GQ, Kong QL, Meng Y, Gao Y,Ning MZ. Long-term postoperative outcomes of bilateral lateral rectus recession vs unilateral recession-resection for intermittent exotropia.Int J Ophthalmol2014;7(6):1043-1047.
13 Lee S, Lee YC. Relationship between motor alignment at postoperative day 1 and at year 1 after symmetric and asymmetric surgery in intermittent exotropia.Jpn J Ophthalmol2001;45(2):167-171.
14 Chia A, Seenyen L, Long QB. Surgical experiences with twomuscle surgery for the treatment of intermittent exotropia.J AAPOS2006;10(3):206-211.
15 Choi J, Chang JW, Kim SJ, Yu YS. The Long-term survival analysis of bilateral lateral rectus recession versus unilateral recession-resection for intermittent exotropia.Am J Ophthalmol2012;153(2):343-351.e1.
16 Kushner BJ. Selective surgery for intermittent exotropia based on distance/near differences.Arch Ophthalmol1998;116(3):324-328.
17 Kim H, Yang HK, Hwang JM. Comparison of long-term surgical outcomes between unilateral recession and unilateral recession-resection in small-angle exotropia.Am J Ophthalmol2016;166:141-148.
18 Suh SY, Choi J, Kim SJ. Comparative study of lateral rectus recession versus recession-resection in unilateral surgery for intermittent exotropia.J AAPOS2015;19(6):507-511.
19 Kim HJ, Kim D, Choi DG. Long-term outcomes of unilateral lateral rectus recession versus recess-resect for intermittent exotropia of 20-25 prism diopters.BMC Ophthalmol2014;14:46.
20 Lee JY, Choi DG. The clinical analysis of recurrence after surgical correction of intermittent exotropia.J Korean Ophthalmol Soc2014;43(11):2220-2226.
21 Jeoung JW, Lee MJ, Hwang JM. Bilateral lateral rectus recession versus unilateral recess-resect procedure for exotropia with a dominant eye.Am J Ophthalmol2006;141(4):683-688.
22 Hardesty HH, Boynton JR, Keenan JP. Treatment of intermittent exotropia.Arch Ophthalmol1978;96(2):268-274.
23 Richard JM, Parks MM. Intermittent exotropia. Surgical results in different age groups.Ophthalmology1983;90(10):1172-1177.
24 Stoller SH, Simon JW, Lininger LL. Bilateral lateral rectus recession for exotropia: a survival analysis.J Pediatr Ophthalmol Strabismus1994;31(2):89-92.
25 Ing MR, Nishimura J, Okino L. Outcome study of bilateral lateral rectus recession for intermittent exotropia in children.Ophthalmic Surg Lasers1999;30(2):110-117.
26 Maruo T, Kubota N, Sakaue T, Usui C. Intermittent exotropia surgery in children: long term outcome regarding changes in binocular alignment.a study of 666 cases.Binocul Vis Strabismus Q2001;16(4):265-270.
27 Fiorelli VM, Goldchmit M, Uesugui CF, Souza-Dias C. Intermittent exotropia: comparative surgical results of lateral recti-recession and monocular recess-resect.Arq Bras Oftalmol2007;70(3):429-432.
28 Ekdawi NS, Nusz KJ, Diehl NN, Mohney BG. Postoperative outcomes in children with intermittent exotropia from a population-based cohort.J AAPOS2009;13(1):4-7.
29 Koklanis K, Georgievski Z. Recurrence of intermittent exotropia: factors associated with surgical outcomes.Strabismus2009;17(1):37-40.
30 Chang YS, Baek SH, Park JM, Kwon HU, Kim YR. Effect of muscle relaxants on short-term results of exotropia surgery: a focus on resection procedures.Korean J Ophthalmol2008;22(4):246-250.